Abstract
Apixaban is effective and safe for preventing stroke, and its usage has increased exponentially in recent years. However, data concerning the therapeutic range of apixaban is limited. This study determined the trough and peak levels of apixaban-specific anti-factor Xa activity (AFXaA) in acute ischemic stroke patients with non-valvular atrial fibrillation (NVAF) in Korea. The study included 85 patients who received apixaban. Blood samples were taken to measure the trough and peak levels of AFXaA using a chromogenic anti-factor assay, as well as prothrombin time (PT) and activated partial thromboplastin time (aPTT). We also reviewed complications such as major bleeding of patients treated with apixaban. In patients given a 5.0-mg apixaban dose, the median trough and peak levels of AFXaA were 104.5 and 202.0 ng/mL. In patients given a 2.5-mg apixaban dose, the median trough and peak AFXaA levels were 76.0 and 151.0 ng/mL. The PT showed a positive correlation with increased AFXaA activity at both levels (Trough R = 0.486, Peak R = 0.592), but the aPTT had no relationship with AFXaA activity at both levels (Trough R = 0.181, Peak R = 0.129). Two cases with intracranial bleeding belonged to the highest AFXaA quartile (Trough, p = 0.176; Peak, p = 0.053). In conclusion, we determined the trough and peak levels of AFXaA in patients with NVAF while being treated with the apixaban in Korea. Our results could be used as a starting point when setting the reference ranges for laboratories using anti-Xa assay. Large-scale studies are needed to establish the reference range for AFXaA in patients with NVAF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Direct factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban, have been shown to be equivalent or superior to warfarin for the prevention of stroke or systemic embolism and have lower rates of major bleeding in patients with non-valvular atrial fibrillation (NVAF). They also have less dosing variability and a rapid onset of action, and stability without drug monitoring [1,2,3]. Because of these advantages, they are being rapidly adopted for the prevention of stroke, both locally and nationally [4].
Of the factor Xa inhibitors, apixaban has the favorable profile in terms of bleeding risk, which is a serious risk for all patients receiving anticoagulants. And it is well tolerated with pharmacokinetic variability such as fewer interactions with concomitant drugs than other direct factor Xa inhibitors [5,6,7]. Additionally, it does not require routine coagulation monitoring. However, the plasma drug concentration should be measured in patients who have some situations such as trauma, emergency surgery, bleeding or embolic events, and concomitant treatment [8, 9]. Dose monitoring is also needed to reduce side effects such as re-infarction due to failure to reach the therapeutic dose or major bleeding due to overdose. In addition, dose monitoring can be used to assess the drug compliance of patients. Therefore, laboratory dose monitoring may be essential in those special situations. However, few studies have investigated apixaban levels in the plasma of patients, and it is consequently difficult to determine the therapeutic range of apixaban.
The majority of published data on the effects of apixaban on laboratory tests of hemostasis are based on studies where the drug is added to plasma or blood in vitro. These studies showed a linear correlation between the levels of apixaban concentration and apixaban-specific anti-factor Xa activity (AFXaA) [10, 11]. However the results of global coagulation tests, such as prothrombin time (PT) or activated partial thromboplastis time (aPTT) were not sensitive enough to determine the apixaban concentration in plasma since the sensitivity mainly depends on the reagents [12,13,14,15].
There are few published data on the levels of AFXaA in the Korean population. Thus, this study aimed to determine levels of apixaban-specific AFXaA in acute ischemic patients with NVAF to assist with drug monitoring. In addition, we assessed the association between levels of AFXaA and PT/aPTT results to determine the apixaban sensitivity of our PT and aPTT tests. We also reviewed complications such as major bleeding of patients treated with apixaban in hospitalization.
Materials and methods
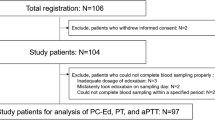
Study participants
This study included a total of 85 patients who were seen at the Gyeongsang National University Hospital from January 2016 to February 2017. All patients started to treat with apixaban immediately after admission with acute ischemic stroke to prevent secondary stroke. At that time, they were diagnosed with NVAF and belonged to a CHA2DS2-VASC score > 2 based on the anticoagulant therapy guidelines [16]. The standard recommended dose of apixaban is 5.0-mg taken orally twice daily, but is set at 2.5-mg if at least two of the following criteria are met: age ≥ 80 years, body weight ≤ 60 kg, and serum creatinine level ≥ 1.5 mg/dL [17, 18]. The main patient exclusion criteria were contraindication to anticoagulation treatment, such as active bleeding, severe thrombocytopenia, major trauma and invasive procedure. Also excluded were patients with severe hepatic impairment or renal impairment (total bilirubin > 3.0 mg/dL, serum creatinine level > 2.5 mg/dL). Before the study was initiated, all patients provided informed consent and the study received approval from the institutional review board.
Measurements of anti-factor Xa activity, PT and aPTT
Blood samples were collected in 3.2% sodium citrate tubes after 3–4 days of apixaban therapy. The peak AFXaA levels were measured 3 h after apixaban administration, and the trough levels were measured immediately prior to apixaban administration. The levels of AFXaA, PT, and aPTT were measured using a STA R Max® analyzer (Diagnostica Stago, Asnieres, France). Specifically, AFXaA levels were determined using a one-stage chromogenic assay with STA-Liquid Anti-Xa reagents (Diagnostica Stago, Asnieres, France). This assay has excellent correlation with the reference method (LC–MS) according to a comparison study [10, 11]. Additionally, we measured PT using the STA®-Neoplastine® CI Plus PT assay and aPTT using the STA®-PTT A aPTT assay (Diagnostic Stago, Asnieres-sur-Seine, France).
Renal- and liver-function assessment
For all patients, blood urea nitrogen (BUN) and creatinine were measured immediately after admission (Cobas® 8000 modular analyzer series, Roche-Diagnostics, Switzerland), and renal function was evaluated using CCr as estimated from the Cockcroft-Gault equation. Liver function tests (e.g., aspartate aminotransferase [AST], alanine aminotransferase [ALT], total bilirubin, alkaline phosphatase and PT) were also performed to assess hepatic dysfunction.
Complications such as major bleeding
Major bleeding was defined as clinically overt bleeding accompanied by one or more of the following criteria: (1) a decrease in the hemoglobin level of at least 2 g per deciliter over a 24-h period, (2) transfusion of 2 or more units of packed red cells, (3) bleeding at a critical site (i.e., intracranial, intraspinal, intraocular, pericardial, intraarticular, intramuscular with compartment syndrome, or retroperitoneal), or (4) fatal bleeding [19].
Statistical analysis
Continuous variables are presented as the median and range, and categorical variables are presented as frequencies and percentages. Because no variables satisfied the assumption of a normal distribution or equal variances by the Shapiro–Wilk test and Levene’s test, respectively, the Mann–Whitney U test was used to compare age, body weight, body mass index, and laboratory tests between the patients treated with either 5.0- or 2.5-mg of apixaban. Fisher’s exact test was used to compare the sex and medical history ratios between the groups, as well as the incidence of complications. Spearman’s correlation analysis was used to examine the association between AFXaA levels and PT/aPTT results. The AFXaA level at the trough and peak times was categorized in quartiles for both dosages. SPSS software for Windows, version 21 (SPSS Inc., Chicago, IL) was used for all statistical analysis. p value < 0.05 was considered statistically significant.
Results
Clinical characteristics of the subjects
A total of 85 patients who experienced a stroke with NVAF while under treatment with apixaban were enrolled in this study. The baseline demographic and clinical characteristics are summarized in Table 1. The median age was 74.5 years, and 43.5% of the subjects were female. A total of 12.9% of the patients had a history of stroke or transient ischemic attack (TIA), and 4.7% of the subjects had an acute myocardial infarction (AMI). The median value of the CHA2DS2-VASC score (the clinical prediction rules for estimating the risk of stroke in patients with NVAF) was 3.8.
Anti-factor Xa activity, PT, and aPTT
All of the coagulation assays, including AFXaA, PT and aPTT, were performed within 2–9 days (3.9 ± 1.6 days) after the first administration of apixaban, and the results are summarized in Table 1. In patients receiving the 5.0-mg dose, the median levels of AFXaA at the trough and peak times were 104.5 and 202.0 ng/mL, respectively. In patients receiving the 2.5-mg dose, the median levels of AFXaA at the trough and peak times were 76.0 and 151.0 ng/mL, respectively.
Relationship between anti-factor Xa activity and PT/aPTT
The relationship between AFXaA and PT/aPTT is presented in Fig. 1. The PT showed a positive correlation with increased AFXaA activity at both levels (Trough R = 0.486, Peak R = 0.592, p < 0.001), but the aPTT had no relationship with AFXaA activity at both levels (Trough R = 0.181, p = 0.112 Peak R = 0.129, p = 0.262). Based on our laboratory’s own reference values, 30.0 and 81.9% of the samples had a normal PT and aPTT, respectively (data not shown) (Fig. 2).
Case presentation
During the course of this study, two patients experienced major bleeding in hospitalization. These two patients were under apixaban treatment at 2.5 mg twice daily and suddenly presented clinical signs of hemorrhage as intracranial bleeding. At that time, the levels of PT were slightly increased (14.5 and 13.7 s at the trough, 15.2 and 14.5 s at the peak, reference range 11.9–14.3 s), but the levels of aPTT were within the reference range (30.1 and 32.6 s at the trough, 31.4 and 32.7 s at the peak, reference range 29.1–43.5 s). It is notable that the levels of AFXaA activity were markedly higher in these cases (270 and 387 ng/mL at the trough and 450 and 491 ng/mL at the peak) than in the other cases. When the 85 patients were divided into quartiles based on AFXaA levels, the cases with complications belonged to fourth quartile for both dosages (Table 2).
Discussion
The present study determined for the first time the median trough and peak levels of AFXaA in NVAF patients treated with apixaban in Korea. The median trough and peak levels of AFXaA were 104.5 and 202.0 ng/mL, respectively, at the 5.0-mg dose and 76.0 and 151.0 ng/mL, respectively, at the 2.5-mg dose. Compared with previous studies, the median level of AFXaA at the peak was significantly higher than the level of apxiaban concentration in previous studies. (5.0-mg p = 0.01, 2.5-mg p = 0.015) [5]. Frost et al. reported the median trough and peak levels of apixaban on treatment day seven, which they predicted to be steady-state concentrations, for a total of 11 healthy subjects in the USA (5.0-mg 49.6 and 128.5 ng/ml, 2.5-mg 21.0 and 62.3 ng/ml, respectively) [5]. Data from the manufacturer showed the predicted apixaban steady-state exposure and reported that the median trough and peak levels of apixaban were 103.0 and 171.0 ng/mL, respectively, for the 5-mg dose and 79.0 and 123.0 ng/mL, respectively, for the 2.5-mg dose in NVAF [20]. One source of this variation may be due to the methodology implemented in each study. Ethnic, geographical and environmental elements may also contribute to this variation. Drug distribution also has the potential for variability related to ethnic differences [21]. Among the characteristics of our clinical patients, one of several factors may have led to the high levels of AFXaA. These findings suggest that the trough and peak reference levels of AFXaA should be calibrated independently in each hospital’s laboratory. However, our results could be used as a starting point when setting the reference ranges for other laboratories using AFXaA, not LC–MS method. Further clinical studies are necessary to determine an appropriate fixed dose of apixaban (as proposed by the manufacturer).
Chromogenic anti-factor Xa assays could be useful for the assessment of apixaban; however, laboratory monitoring techniques lag behind new drug development, specifically regarding factor Xa inhibitors. Knowing the association between routine coagulation tests, such as PT and aPTT, and AFXaA levels is helpful to manage patient care in emergency situations. PT and aPTT are not sensitive enough for quantitative measurement of apixaban concentrations at the plasma level. However, some earlier studies demonstrated that, depending on the specific reagent used, PT was modestly prolonged by factor Xa inhibitors [8, 9, 15]. Our results also showed that increased PT was associated with increased AFXaA, but aPTT was insufficient to accurately determine the level of AFXaA. Even though PT was associated with AFXaA, there was very little evidence that the AFXaA could be quantitatively estimated using the PT. Moreover, some patients under apixaban therapy still had normal PTs. Therefore, PT and aPTT results can be easily misinterpreted if the results are not fully understood, which could have clinical implications. Additionally, clinicians should also consider the possibility of factitious reporting of other coagulation assays in the presence of factor Xa inhibitors, which may lead to incorrect result interpretation and improper diagnosis and management.
A previous study reported that frequent monitoring of anticoagulation in patients treated with apixaban is unnecessary and that apixaban measurement is particularly useful in some clinical situations including cases of stroke recurrence, urgent surgery, bleeding events, and suspected overdose [8, 9]. In this study, there were two cases with complications, specifically major bleeding, which were associated with high AFXaA. In two cases in which patients received 2.5 mg of apixaban twice daily, cerebral hemorrhage suddenly appeared. At that time, the AFXaA levels were two to three times higher than the average in both cases. It should be noted that in these two cases the PT and aPTT were never higher than the study average. However, despite the overall higher AFXaA levels in this study compared to previous studies, the majority of the cases did not present with any side effects, highlighting the difficulty in using AFXaA as a predictor for overdose. Further studies are needed to define the relationship between AFXaA and clinical outcomes.
There remains a need for an apixaban antidote for emergency situations. In the absence of a specific antidote, clinicians typically use prothrombin complex concentrates in emergency apixaban-overdose situations. Currently, apixaban antidotes are undergoing clinical trials [22].
This study has several limitations. First, it was conducted at a single center with a small number of enrolled patients. Second, the investigation period and the number of cases with side effects were insufficient for a detailed study on the relationship between AFXaA and re-infarction or bleeding. Finally, we did not use the gold standard method, LC–MS, to measure the plasma levels of apixaban, because of its difficult accessibility.
In conclusion, we determined the trough and peak levels of AFXaA in patients who had experienced a stroke with NVAF while being treated with the apixaban. Our results could be used as a starting point when setting the reference ranges for laboratories using AFXaA. Large-scale studies are needed to establish the reference range for AFXaA in patients with NVAF.
References
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, ARISTOTLE Committees and Investigators (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365 (11):981–992. https://doi.org/10.1056/NEJMoa1107039
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, Investigators RA (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891. https://doi.org/10.1056/NEJMoa1009638
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Spinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM, Investigators EA-T (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369(22):2093–2104. https://doi.org/10.1056/NEJMoa1310907
Baker D, Wilsmore B, Narasimhan S (2016) Adoption of direct oral anticoagulants for stroke prevention in atrial fibrillation. Intern Med J 46(7):792–797. https://doi.org/10.1111/imj.13088
Frost C, Wang J, Nepal S, Schuster A, Barrett YC, Mosqueda-Garcia R, Reeves RA, LaCreta F (2013) Apixaban, an oral, direct factor xa inhibitor: single dose safety, pharmacokinetics, pharmacodynamics and food effect in healthy subjects. Br J Clin Pharm 75(2):476–487. https://doi.org/10.1111/j.1365-2125.2012.04369.x
Di Minno A, Frigerio B, Spadarella G, Ravani A, Sansaro D, Amato M, Kitzmiller JP, Pepi M, Tremoli E, Baldassarre D (2017) Old and new oral anticoagulants: food, herbal medicines and drug interactions. Blood Rev 31(4):193–203. https://doi.org/10.1016/j.blre.2017.02.001
Cohen AT, Hamilton M, Bird A, Mitchell SA, Li S, Horblyuk R, Batson S (2016) Comparison of the Non-VKA oral anticoagulants apixaban, dabigatran, and rivaroxaban in the extended treatment and prevention of venous thromboembolism: systematic review and network meta-analysis. PloS ONE 11(8):e0160064. https://doi.org/10.1371/journal.pone.0160064
Douxfils J, Mani H, Minet V, Devalet B, Chatelain B, Dogne JM, Mullier F (2015) Non-VKA oral anticoagulants: accurate measurement of plasma drug concentrations. BioMed Res Int 2015:345138. https://doi.org/10.1155/2015/345138
Reiffel JA, Weitz JI, Reilly P, Kaminskas E, Sarich T, Sager P, Seltzer J, Cardiac Safety Research Consortium p, participants (2016) NOAC monitoring, reversal agents, and post-approval safety and effectiveness evaluation: a cardiac safety research consortium think tank. Am Heart J 177:74–86. https://doi.org/10.1016/j.ahj.2016.04.010
Gouin-Thibault I, Flaujac C, Delavenne X, Quenet S, Horellou MH, Laporte S, Siguret V, Lecompte T (2014) Assessment of apixaban plasma levels by laboratory tests: suitability of three anti-Xa assays. A multicentre French GEHT study. Thromb Haemost 111(2):240–248. https://doi.org/10.1160/TH13-06-0470
Becker RC, Yang H, Barrett Y, Mohan P, Wang J, Wallentin L, Alexander JH (2011) Chromogenic laboratory assays to measure the factor Xa-inhibiting properties of apixaban–an oral, direct and selective factor Xa inhibitor. J Thromb Thrombolysis 32(2):183–187. https://doi.org/10.1007/s11239-011-0591-8
Schmitz EM, Boonen K, van den Heuvel DJ, van Dongen JL, Schellings MW, Emmen JM, van der Graaf F, Brunsveld L, van de Kerkhof D (2014) Determination of dabigatran, rivaroxaban and apixaban by ultra-performance liquid chromatography–tandem mass spectrometry (UPLC–MS/MS) and coagulation assays for therapy monitoring of novel direct oral anticoagulants. J Thromb Haemost JTH 12(10):1636–1646. https://doi.org/10.1111/jth.12702
Dale BJ, Chan NC, Eikelboom JW (2016) Laboratory measurement of the direct oral anticoagulants. Br J Haematol 172(3):315–336. https://doi.org/10.1111/bjh.13810
Hillarp A, Gustafsson KM, Faxalv L, Strandberg K, Baghaei F, Fagerberg Blixter I, Berndtsson M, Lindahl TL (2014) Effects of the oral, direct factor Xa inhibitor apixaban on routine coagulation assays and anti-FXa assays. J Thromb Haemost JTH 12(9):1545–1553. https://doi.org/10.1111/jth.12649
Gosselin R, Grant RP, Adcock DM (2016) Comparison of the effect of the anti-Xa direct oral anticoagulants apixaban, edoxaban, and rivaroxaban on coagulation assays. Int J Lab Hematol 38(5):505–513. https://doi.org/10.1111/ijlh.12528
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, Members AATF. (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 130(23):2071–2104. https://doi.org/10.1161/CIR.0000000000000040
Alexander JH, Andersson U, Lopes RD, Hijazi Z, Hohnloser SH, Ezekowitz JA, Halvorsen S, Hanna M, Commerford P, Ruzyllo W, Huber K, Al-Khatib SM, Granger CB, Wallentin L (2016) Apixaban for reduction of S, other thromboembolic complications in atrial fibrillation. Apixaban 5 mg twice daily and clinical outcomes in patients with atrial fibrillation and advanced age, low body weight, or high creatinine: a secondary analysis of a randomized clinical trial. JAMA Cardiol 1(6):673–681. https://doi.org/10.1001/jamacardio.2016.1829.
van Es N, Coppens M, Schulman S, Middeldorp S, Buller HR (2014) Direct oral anticoagulants compared with vitamin k antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 124(12):1968–1975. https://doi.org/10.1182/blood-2014-04-571232
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the S, Standardization Committee of the International Society on T, Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost JTH 3 (4):692–694. https://doi.org/10.1111/j.1538-7836.2005.01204.x
Bristol-Myers Squibb-Pfizer. https://www.medicines.org.uk/emc/medicine/27220. Accessed 21 Feb-2017
Yasuda SU, Zhang L, Huang SM (2008) The role of ethnicity in variability in response to drugs: focus on clinical pharmacology studies. Clin Pharmacol Ther 84(3):417–423. https://doi.org/10.1038/clpt.2008.141
Rogers KC, Shelton MP, Finks SW (2016) Reversal agents for direct oral anticoagulants: understanding new and upcoming options. Cardiol Rev 24(6):310–315. https://doi.org/10.1097/CRD.0000000000000118
Acknowledgements
This work was supported by the Fund of Research Promotion Program, Gyeongsang National University, 2016.
Author information
Authors and Affiliations
Contributions
E.K. was responsible for the study concept and design. H.S., C.K. and N.C. and S.K. acquired the data. R.K. analysed the data. H.S. drafted the manuscript. E.K., M.C. and S.K. critically revised the manuscript for important intellectual content. All authors gave approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
Ethical approval has been granted by the Institutional Review Board of Gyeongsang National University Hospital. The reference number is 6079/448/10-6-13.
Rights and permissions
About this article
Cite this article
Shin, H., Cho, MC., Kim, R.B. et al. Laboratory measurement of apixaban using anti-factor Xa assays in acute ischemic stroke patients with non-valvular atrial fibrillation. J Thromb Thrombolysis 45, 250–256 (2018). https://doi.org/10.1007/s11239-017-1590-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1590-1