Abstract
To describe the development of a pharmacy driven off-label recombinant factor seven (rFVIIa) protocol by a multi-disciplinary team for critical bleeding. A multi-disciplinary team made up of members from several critical care and surgical departments within the hospital were formed and charged with developing a standardized approach to how rFVIIa would be used for critical bleeding in an academic medical center. Groups represented on the multi-disciplinary team included clinical pharmacy, emergency medicine, pulmonary, hematology, cardiothoracic surgery, trauma, neurosurgery, and vascular surgery physicians. A pharmacist driven off-label rFVIIa protocol was developed and implemented for the use in those patients with critical bleeding. The protocol was based on the available literature and local expert opinion. Through the use of this protocol a significantly smaller average dose of rFVIIa is now being used when compared to those patients treated prior to the new protocol (47.5 vs. 62.2 mcg/kg, p = 0.036) while all-cause mortality was not significantly altered (35 vs. 48.8 %, p = 0.057). An effective and safe pharmacy driven protocol was implemented by a multi-disciplinary team for rFVIIa as seen by providing a significantly lower average dose of rFVIIa while not sacrificing for overall patient mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive bleeding, especially in the perioperative period, remains a major complication following surgery. This potential refractory hemorrhage is a major contributor to morbidity and mortality in a variety of patient populations. This is especially true in cardiac surgery where severe bleeding occurs in slightly under 10 % of cases and accrues almost a 20 % mortality in elective vascular cases [1–4]. In trauma cases 30–40 % of all deaths can be attributed to uncontrolled bleeding [5]. The principle cause for most refractory hemorrhage is multi-factoral but is usually a combination of several pathologies. Causes for bleeding can usually be broken down into a pre-existing undetected bleeding disorder, a complication secondary to the surgical operation itself or an abnormality from blood loss [6]. Whether or not these coagulopathies are drug related or physiologic in nature they must be controlled in order to prevent further complications or ultimately death. The treatment for most coagulopathies is primarily based on source control, fluid management, and blood product utilization (platelets, packed red blood cells, plasma, and cryoprecipitate). At times these treatments are not adequate to control a patient’s coagulopathy and the need for additional support is needed. Commonly used agents are three and four factor prothrombin complex concentrates (PCCs), desmopressin, and activated recombinant factor seven (rFVIIa). With the limited availability of the three and four factor PCC products within the United States, lack of clinical experience and limited therapeutic indications for desmopressin, the use of rFVIIa continues to increase.
Recombinant factor VIIa is a prothrombotic agent that binds to tissue factor when exposed to circulating blood following tissue injury [7]. This tissue factor-rFVIIa interaction leads to thrombin generation via the extrinsic clotting pathway. In addition, rFVIIa activates factor X on the surface of activated platelets, which further leads to enhanced thrombin release at the site of injury [8]. This large production of thrombin by rFVIIa is commonly termed as a thrombin ‘burst’. Currently rFVIIa has FDA approval for hemophilia A or B with inhibitors to Factor VIII or Factor IX, acquired hemophilia, and congenital factor VII deficiency, but due to the high rate of thrombin generation rFVIIa has been commonly used for many “off-label” indications [9–11]. While many other factor products will eventually lead to increased levels of thrombin the fact that rFVIIa is administered in an activated state also contributes to a faster and more profound response which would theoretically make it more effective in situations of critical bleeding. These “off-label” indications are becoming more popular and rFVIIa seems to be highly effective, however, the appropriate dosing scheme for off-label indications is not well understood.
The current FDA approved dose for patients with hemophilia is 90 micrograms per kg (mcg/kg) to be given every 2 h until hemostasis is reached. However, rFVIIa dosing ranges from 10 to 400 mcg/kg have been reported in the literature depending on hematologist preference, or clinical experience. The largest dosing study in the hemophilia population included 78 patients being treated with either 35 or 70 mcg/kg per dose. The average number of doses in this study required to achieve hemostasis was 2.8 and 3.2 for the 35 and 70 mcg/kg doses respectively [12]. These doses have been translated to off-label indications due to lack of overall published data. Currently most data suggest that doses of 40–90 mcg/kg can be appropriately utilized for most off-label indications [13–15]. Doses higher than this only increase the risk for thrombotic events (i.e. myocardial infarction, deep venous thrombosis, pulmonary embolism) [15]. As in the phase one trial described above the use of sequential, spaced out dosing schemes have also been suggested for patients with no response to initial doses in off-label indications [15, 16].
With the only absolute contraindications to rFVIIa therapy being drug hypersensitivity or to mouse, bovine, or hamster proteins the use of rFVIIa in the treatment of refractory critical bleeding is very appealing. However, the incidence of thromboembolic events must be seriously considered with rates significantly higher when compared to placebo (5.5 vs. 3.2 %, p = 0.003) [17].
The high potential for harm to the patient and uncertainty within the published literature regarding appropriate dosing strategy led to the development of a specific dosing protocol at our institution. Here we report our experience and process by which we developed and implemented a low and sequential dosing treatment scheme using rFVIIa at an academic medical center.
Problem
In our medical center we commonly interact with patients with varying ailments. We are a level 1 trauma and cardiac center that performs many surgeries from mechanical circulatory support (left and right ventricular support devices) to the typical neurological and trauma cases from our region. For these cases and many others the development of critical bleeding that is refractory to standard management can be relatively frequent. In these circumstances it was common to use rFVIIa for bleeding control. The problem with its use as outlined above is the lack of standardized dosing regimens as it is being used for off-label indications. Our process for ordering at this time was mainly a phone call or order placed into the system to pharmacy for a particular dose of rFVIIa. For “off-label” indications any physician was allowed to order rFVIIa with no need for co-signature by hematology or the pharmacy department. This lack of specific privileging was likely one of the major causes for the wide dosing ranges and frequent use. For patients with hemophilia orders were usually written by a hematologist as they typically guided their factor replacement. Once an order for rFVIIa was received the pharmacy would prepare the dose and send to the patient via pharmacy technician as a part of the normal work flow. This presented several problems to our institution including highly variable dosing by the physicians, lag time in time from order to dose administration, and no oversight to what other therapies were being implemented before rFVIIa’s use. In an effort to come up with a more standardized, consistent, and efficient process the decision was made to develop an institutional specific protocol.
Protocol development and implementation
Once the decision was made to develop a protocol a multi-disciplinary team consisting of members from cardio-thoracic surgery, neurosurgery, emergency medicine, pulmonary, hematology, trauma/surgery, and pharmacy were put together. It was from this team that our protocol was designed and the role pharmacy would play within it was developed. After several meetings and revisions a protocol was developed covering the following major points.
Other management strategies
The typical management strategy for critical bleeding revolves around site stabilization, fluid therapy, and replacement of lost coagulation factors through blood product administration. For the body to be able to appropriately form clots it must have the frame work for which to build it. This idea is similar to why these agents must be used prior to rFVIIa. While rFVIIa does provide some clotting factor (activated factor VII) it is imperative that other resources be available for the body to get the best response from the rFVIIa (i.e. platelets, fresh frozen plasma for other clotting factors missed with rFVIIa, and cryoprecipitate for fibrinogen). In addition to these factors acid/base status should be analyzed as one study demonstrated that a drop in pH from 7.4 to 7.0 nearly abolished all of the activity (>90 %) of rFVIIa secondary to the reduced activity of the FXa/FVa complex thus decreasing the conversion of prothrombin to thrombin [18]. If all of these factors have been recognized and addressed than the patient could then be considered a candidate for rFVIIa.
Pharmacists’ role
Pharmacists at The University of Kentucky Medical Center (UKMC) provide clinical services in most areas of practice within the hospital including cardiology, pulmonary/critical care, vascular, cardiothoracic, trauma, and neurosurgery. The large pharmacy residency program at UKMC allows for many great educational opportunities including 24 h on-call shifts. The details of the residency on call program have been previously published [19, 20]. Having a clinical pharmacist at the hospital 24 h a day allows for several unique clinical pharmacy services to be offered including Crofab® initiation and administration, code sepsis, code blue, and stroke alert response, anticoagulation and antibiotic management. It also allowed for the potential for increased involvement in the rFVIIa process. Pharmacy was already in a great position for increased visibility in the process since rFVIIa was already housed within the pharmacy budget and the ability to have consistent support for its use was apparently needed.
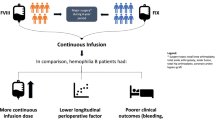
Therefore, the multidisciplinary team agreed to change rFVIIa ordering from a specific dose to a pharmacy to dose order. This would trigger the response by the pharmacy resident on-call bringing them to the patient bedside for a “STAT” consult. Once the appropriateness of the rFVIIa had been established by the resident, other management strategies implemented, and clinical team in agreement the pharmacist would decide on a dose for the patient and administer rFVIIa at the patient’s bedside. To speed up the process of admixing and administration the resident on-call would bring several vials and strengths of rFVIIa with them to each rFVIIa pharmacy to dose call in case administration would be warranted.
By setting the protocol up this way the multi-disciplinary team was hoping to implement some consistency within the process, provide better overall patient care and management of critical bleeding, and improve time between ordering the rFVIIa and patient administration.
Dosing
For dosing, our protocol was based on the literature demonstrating doses of around 90 mcg/kg to be a soft maximum for rFVIIa in the balance of efficacy and thrombotic risk and the use of a sequence of doses based on the patient specific efficacy. Therefore, the total dose of 90 mcg/kg was divided into three equal 30 mcg/kg doses to be given up to three times if needed (Fig. 1). Prior to the protocols implementation physicians decided what dose they wanted to give and administered it on their own. Doses in this setting had a very wide range, but were mainly higher single one time doses. The negative to using this method is the chance that by giving a one-time dose you could miss the amount of rFVIIa needed to reverse the coagulopathy and perhaps give too much pushing the patient into more of a pro-thrombotic state. By giving smaller doses and waiting to see the effect you allow the patient to dictate the dose needed and potentially minimize the amount of unnecessary drug and potential for side effects caused by the rFVIIa and drug overdosing.
Education
In order for this new protocol to work effectively a large education initiative was undertaken. For the physician staff a change in culture from just ordering rFVIIa like every other medication to a consult for pharmacy had to be done. This process was already precedented by other similar processes already in place like Crofab and Xigris administration which were both based on STAT pharmacy to dose orders. Since pharmacy would be playing such an integral role in this process extensive pharmacy education was needed. For the central operating staff recognizing the rFVIIa pharmacy to dose order and knowing whom to contact about it, and for the clinical staff what to do once this order was placed. Reinforcement of this process for the clinical staff is currently done every year with each incoming residency class and each event is reviewed for accuracy and consistency to the protocol based on the daily on-call reports published each day by the on-call resident to the entire pharmacy staff. Furthermore, any additional training needed for staff, nursing, pharmacy, or physician is done as needed on a case by case basis.
Experience with protocol
The hospital’s pharmacy and therapeutics committee approved the protocols use by the clinical pharmacy staff and the new protocol was implemented in July 2008. To analyze our new protocol a retrospective, cohort review was done comparing rFVIIa treatment using the new dosing protocol to a historic patient population treated with the non-protocolized approach to rFVIIa administration for the management of critical bleeding. The review received expedited IRB approval in October 2012.
Data was included on all patients aged 18 years or older, admitted between January 2003 and June 2008 for the pre-protocol population and January 2009–October 2012 for the post-protocol group, and whom received rFVIIa for an off-label indication. Baseline characteristics were comparable between each group with only the home medications warfarin and low dose aspirin being significantly higher in the post protocol population (Table 1). The post-protocol population included one hundred and seventeen patients while the pre-protocol population included a total of eighty patients. Overall it was found that a majority of the use of rFVIIa in our institution was for off-label indications.
The average administered dose was significantly smaller in the post-protocol population (47.5 vs. 62.2 mcg/kg, p 0.036) when compared to the pre-protocol population (Table 2). While a formal cost analysis was not been performed, this difference of almost 15 mcg/kg translates to a dose of around 1,250 mcg rFVIIa (average weight of 85 kg of patients in study) less than what our patients were receiving on average. If we assume that 1 mg of rFVII cost around $1,500, then based on the average reduction in dose one could expect an average cost savings of almost $1,900 per patient. While the number of patients that received rFVIIa actually increased after the protocol was implemented the total amount of rFVIIa given over those time spans did decrease.
All-cause mortality was not significantly different between the post and pre protocol groups (35 vs. 48.8 %, p 0.057). However, this was an improvement in absolute risk of 13.8 % and relative risk of 28 %. The rate of thrombotic events has been reported to be as high as 9 % in patients treated with rFVIIa for off label indications [17]. In our analysis the combination of the adverse events stroke, deep venous thrombosis, and pulmonary embolism were similar between the post and pre-protocol groups (6 vs. 5 %, p 0.769) with very few events occurring in either group (6 vs. 4). Specific blood products utilized was not significantly different between the groups except for the use of cryoprecipitate. The amount of cryoprecipitate went down to 1.23 for the post population from 2.27 in the pre-protocol population (p 0.045).
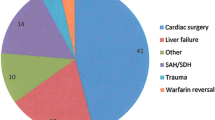
Even when the patients were divided based on their clinical service, under whose care the patients were when they received rFVIIa (pulmonary, cardiothoracic, trauma, vascular, and neurosurgery), no differences were seen in patient outcomes (mortality, blood product utilization, or adverse events) from rFVIIa administration (Fig. 2).
Conclusion
The potential benefits of rFVIIa use in non-hemophilia patients remains under studied. Most of the current data demonstrates no significant impact on mortality or thromboembolic outcomes with the use of rFVIIa. Our analysis demonstrates that by using rFVIIa only as a rescue therapy when absolutely necessary a positive effect can be seen with critical bleeding. Despite lower doses being administered mortality did not statistically increase in our patient population. In fact the absolute and relative risk reductions demonstrate potential clinical benefit. The decrease in mortality in the post protocol population was likely multi-factorial and not solely a result of the protocol itself. However, by implementing a rFVIIa protocol designed by a multi-disciplinary team and bringing the pharmacist to the patient bedside to help in the management of critical bleeding more appropriate, consistent, and safer doses of rFVIIa were administered to our patients.
References
Shander A (2007) Financial and clinical outcomes associated with surgical bleeding complications. Surgery 142(4 Suppl):S20–S25
Rady M, Ryan T, Starr N (1998) Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med 26(2):225–235
Marietta M, Facchini L, Pedrazzi P, Busani S, Torelli G (2006) Pathophysiology of bleeding in surgery. Transplant Proc 38(3):812–814
Wąsowicz M, Meineri M, McCluskey SM, Mitsakakis N, Karkouti K (2009) The utility of thromboelastography for guiding recombinant activated factor VII therapy for refractory hemorrhage after cardiac surgery. J Cardiothorac Vasc Anesth 23(6):828–834
Spahn D, Cerny V, Coats T et al (2007) Management of bleeding following major trauma: a European guideline. Crit Care 11(1):R17
Koh M, Hunt BJ (2003) The management of perioperative bleeding. Blood Rev 17(3):179–185
Hedner U, Erhardtsen E (2002) Potential role for rFVIIa in transfusion medicine. Transfusions 42(1):114–124
Hoffman M (2001) III, DMM: a cell-based model of hemostasis. Thromb Haemost 85:958–968
Hedner U, Erhardtsen E (2000) Recombinant coagulation factor VIIa: from the concept to clinical application in hemophilia treatment in 2000. Semin Thromb Hemost 26:363–369
Friederich P, Geerdink M, Spataro M (2000) The effect of the administration of recombinant activated factor VII (NovoSeven) on perioperative blood loss in patients under undergoing transabdominal retropubic prostatectomy: the PROSE study. Blood Coagul Fibrinolysis 11(Suppl 1):S129–S132
Levi M, Peters M, Buller H (2005) Efficacy and safety of recombinant factor VIIa for treatment of severe bleeding: a systematic review. Crit Care Med 33:883–890
Macik BG, Lindley CM, Lusher J et al (1993) Safety and initial clinical efficacy of three dose levels of recombinant activated factor VII (rFVIIa): results of a phase I study. Blood Coagul Fibrinolysis 4(4):521–528
Shander A, Goodnough L, Ratko T (2005) Consensus recommendations for the off-label use of recombinant human factor VIIa (NovoSeven) therapy. P and T 30:644–658
Goodnough L, Lublin D, Zhang L (2007) Transfusion medicine service policies for recombinant factor VIIa administration. Transfusion 44:1325–1331
Warren O, Mandal K, Hadjianastassiou V (2007) Recombinant activated factor VII in cardiac surgery: a systematic review. Ann Thorac Surg 83:707–714
O’Connell K, Wood J, Wise R, Lozier J, Braun M (2006) Thromboembolic adverse events after use of recombinant human coagulation factor VIIa. JAMA 295:293–298
Levi M, Levy JH, Andersen HF, Truloff D (2010) Safety of recombinant activated factor VII in randomized clinical trials. N Engl J Med 363(19):1791–1800
Martinoqitz U, Kenet G, Segal E, Luboshitz J, Lubetsky A et al (2001) Recombinant activated factor VII for adjunctive hemorrhage control in trauma. J Trauma 51:431–439
Smith K, Hecht K, Armistead A, Davis G (2003) Evolution and operation of a pharmacy residency on-call program. Am J Health Syst Pharm 60:2236–2241
Mcconeghy KW, Winstead PS, Cook AM, Martin CA, Weant KA, Flynn JD (2012) Benefits of a 24-h inhouse on-call program for pharmacy residents. Am J Health Syst Pharm 69(24):2160–2164
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bain, J., Lewis, D., Bernard, A. et al. Implementation of an off-label recombinant factor VIIa protocol for patients with critical bleeding at an academic medical center. J Thromb Thrombolysis 38, 447–452 (2014). https://doi.org/10.1007/s11239-014-1107-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-014-1107-0