Abstract
Severe sepsis and multiple organ distress syndrome remain a diagnostic and therapeutic challenge for intensive therapy. Platelet activating factor forms a bridge between inflammation and clot formation. Our study surveys the effect of severe sepsis on platelet function and focuses on spontaneous aggregation in severely ill patients. Daily arterial blood samples were collected from 45 patients (average age of 60.7 ± 13) for five consecutive days following admission and 30 healthy controls. Platelet aggregation was measured using adrenaline (ADR), adenosine diphosphate (ADP), collagen (COL) and normal saline (SAL). Clinical status was observed using Multiple Organ Dysfunction Score (MODS) and Sequential Organ Failure Assessment (SOFA) score systems. Inducible aggregation deteriorated in septic patients in all 5 days with ADR, ADP and COL (P < 0.05) while SAL aggregation was increased during intensive care. Low platelet patients showed weak inducible aggregation with ADP throughout, with ADR on the 2nd, 3rd, 4th and 5th days and with COL on the 1st, 2nd and 3rd days. SAL aggregation showed no significance. No significant difference was seen between platelet functions comparing survivors and non-survivors. In the spontaneous aggregative group, platelet count was insignificantly higher, while procalcitonin levels were lower in 1st, 3rd and 4th days and no significant difference was observed in lactate levels. We demonstrated the presence of spontaneous platelet activity while overall inducible platelet aggregation is significantly deteriorated in septic patients. There were significant differences in inducible aggregation between normal and low platelet count groups. Inducible platelet function had no predictive value in the outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe sepsis and septic shock are still a great challenge for intensive care units (ICU) as they are the leading cause of ICU admissions with 11.9% [1]. According to recent cohort multi-central studies the incidence of sepsis accounts for 19.6–59% among patients treated on the ICU accounting for 40–47% mortality based on clinical results [2, 3]. One prominent factor in the estimation of outcome in sepsis is the number of organs affected by the multiple organ dysfunction syndrome [4]. During the development of multiple organ dysfunction syndrome there is not only a hyperactivation of the innate immune system characterized by the elevated serum levels of tumor necrosis factor alpha (TNF-a), interleukin 1b (IL-1b), interleukin 6 (IL-6) and platelet activating factor (PAF) but also periods of immunosuppression along with existing hypodynamic states [5, 6]. During the “cytokine storm” PAF form a bridge between inflammation and clot formation [7], thus activating platelets and inducing aggregate formation in the circulatory system. The PAF mediated pathway is also responsible for the elevated production of inflammatory eicosanoids and suspected to be one of the main mediators of acute lung injury [7]. The decline of normal endothelial function also has a procoagulant effect [8]. The alteration of platelet function and count can be observed in septic patients affected by microvascular insufficiency [9, 10]. According to Lee et al. about 58% of patients may develop thrombocytopenia during severe sepsis while recent studies have not found a connection between the actual platelet count and function [11, 12]. Platelet functions measured by aggregation agonists are also altered during critical illnesses. Previous investigations show significantly deteriorated inducible aggregability in severe septic patients [12, 13]. The aim of our present prospective study was to evaluate the platelet function alteration characteristics among severe septic patients. The early impairment of the microvascular flow is formerly described in severe septic patients [14, 15]. Our hypothesis elucidated whether the microvascular flow deterioration is a result of the increased inducible platelet aggregability. Furthermore we tried to asses the connection between reduced platelet count and platelet function. Our focus was the evaluation of the spontaneous thrombocyte aggregation in septic patients.
Methods
Patients
Our study was carried out in accordance with the ethical guidelines of the 2003 Declaration of Helsinki and we obtained the permission of the Regional Research Ethical Committee of University of Pécs (2406/2005). Forty-five patients were included in our study. We had 30 healthy volunteers in our control group for ophthalmological ambulatory procedures. All patients provided a written informed consent following detailed information regarding the study and blood sampling. In the case of a consciousness disorder we obtained consent from the next of kin as per national law.
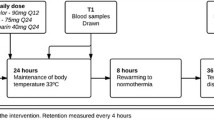
Our inclusion criteria were recently discovered severe sepsis (within 24 h) with two or more organ dysfunctions. Sepsis criteria included: fever >38°C, hypothermia <36°C, tachycardia >90/min, tachypnoe, altered state of consciousness, positive fluid imbalance, hyperglycemia, leukocyte count >12 g/l or <4 g/l, elevated C-reactive protein (CRP) >10 mg/l, serum procalcitonin (PCT) level >2 ng/ml [16–18]. Patients in moribund state or with any kind of hematological baseline disease such as myeloproliferative disorders like lymphoma or leukaemia were excluded. The endpoint was either the 5th day of inclusion or the death of the patient. Supportive therapy was performed according to the recent sepsis management guidelines [19]: fluid resuscitation with crystalloids and colloids, early broad spectrum antibiotic treatment (most commonly carbapenems with or without aminoglycosides), in case of hemodynamic shock norepinephrine with or without dobutamine, for control of glucose levels controlled infusion of actrapid, in oliguria/anuria furosemide with hemodialysis, stress ulcer prophylaxis with pantoprazole or famotidine, thrombosis prophylaxis by enoxaparine or fraxiparine, morphine and propofol were used for analgesia and sedation respectively during mechanical ventilation at appropriate doses. None of the patients received drotrecogin alfa and antiplatelet drugs and 17 patients received cortisteroids. We compared our patient data with healthy volunteers as controls. The data was further evaluated between survivors and non-survivors. The diagnosis and follow up of severe sepsis were scored according to the Sequential Organ Failure Assessment (SOFA) [20] and Multiple Organ Dysfunction Score (MODS) [21].
Blood samples
Daily arterial blood samples were collected once upon admission and once for the following four consecutive days. Venous blood samples were collected from healthy controls. We avoided arterial blood sampling due to possible bleeding complications. Furthermore, a pilot study showed that platelet aggregation of venous and arterial origin provided no statistical significant difference [22]. Routine laboratory parameters (arterial blood gas, renal and hepatic markers, full blood count, etc.) and other parameters (CRP, PCT, D-dimer, lactate, fibrinogen) were measured from the blood samples. The laboratory tests were carried out by the Institute of Laboratory Medicine, University of Pécs.
Platelet aggregometry
The measurement of platelet aggregation levels was carried out using the Carat TX4® aggregometer (Entec-Medical) based on Born’s optical system. Sodium-citrate anticoagulated blood samples were centrifuged with 600 rpm for 5 min and platelet rich plasma was separated into four vials (450 μl). The remaining material was centrifuged for 10 min with 5000 rpm to obtain platelet poor plasma (500 μl). Aggregation agonists and saline were introduced separately into the platelet rich plasma samples. We used 50 μl of 0.9% NaCl solution (SAL) to measure the spontaneous and the same amount of 10 μM adenosine diphosphate (ADP), 2 μg/ml collagen (COL), 10 μM adrenaline (ADR) (Theracont TA-3 inductor kit, CARAT Diagnostica Ltd., Budapest, Hungary) to evaluate the inducible aggregation [22]. We assumed spontaneous platelet aggregation to be higher than 10%. Our opinion suggests that 1–3% aggregation could be an artefact. If the spontaneous aggregation is higher and consecutive in the series of measurements in one patient, it has to be analysed as an objective result. This is why we chose the 10% value as a reference due to the absence of data from literature. The inducible platelet aggregation was chosen >60% as measured by Carat TX4® platelet aggregometer. This value was verified in a study which was performed in our University [23].
Based on the criteria of thrombocytopenia defined by the Surviving Sepsis Campaign 2008 guidelines (100000/μl) we divided our patients into a normal platelet count group and a low platelet count group [19]. The severity of sepsis and platelet function evaluations were carried out with a separation based on the number of affected organs. According to sepsis epidemiology studies we chose three or more organ failures as separation criteria based on the 50% mortality during ICU care [1]. High severity (more than three affected organs) and mild severity (less than three affected organs) patient groups were formed according to the admission status. We also measured the change of aggregability between survivors and non-survivors.
Statistics
Our data is presented with mean ± standard deviation of the mean. Kruskal–Wallis-test was used with P < 0.05 considered significant. The number of patients required was calculated by power analysis according to spontaneous and non-spontaneous platelet aggregation results from our previous pilot studies performed on similar population. Therefore, with type I α = 5% and type II (power) of 90% we needed 40 patients.
Results
The main demographical data, MODS and SOFA scores calculated on the first, third and fifth admission day and the most commonly occurring organ failures of our study population are discussed in Table 1.
The evaluation of platelet aggregation in septic patients compared to healthy controls revealed a significant deterioration in the inducible aggregation among septic patients. The ADP, ADR and COL induced function measurements resulted in significantly lower levels for all the five study days (P < 0.05) while the SAL based aggregation showed a significant increase in the platelet function of septic patients (P < 0.001) (Fig. 1).
On admission 19 patients were in the low platelet count range and 26 patients were in the normal platelet count group. The ADP induced platelet aggregation was significantly deteriorated in patients with low platelet count in all 5 days (P < 0.05) while adrenaline caused aggregations were lower in the 2nd, 3rd, 4th and 5th consecutive day (P < 0.05). Collagen induced aggregation was significantly lower on the 1st, 2nd, 3rd days following admission (P < 0.05). There was no difference between the two groups based on the saline aggregation (Fig. 2). Compared to our control group most of the aggregations measured in the normal platelet group were significantly lower than the control results with the exception of the adrenaline inducible aggregation on the 3rd, 4th, 5th days and ADP induced aggregation on the 5th day (P < 0.05). The low platelet group had significantly deteriorated aggregation levels with all inductors in all cases (P < 0.001) compared to controls.
Fourteen patients deceased during our study and 31 patients built up the survival group. Non-survivors showed no significant deterioration in platelet count. All induced and saline aggregation measurement results when compared to survivors were not significantly different in non-survivors (Fig. 3). In the survivor group we found four patients with notable aggregation levels (>50%) during the saline based aggregation tests. The spontaneous aggregation group (14 patients) revealed a non-significant difference in platelet counts compared to the non-spontaneous aggregation group. The non-spontaneous aggregation group showed a significantly higher PCT levels on the 1st, 3rd, 4th consecutive days. Lactate levels were also lower in the spontaneous aggregative patients during our study (Fig. 4).
Discussion
Platelet count disorders have been already described in sepsis however the exact mechanism behind the development of thrombocytopenia requires further investigation [24]. The primary objective of our study was to evaluate the alterations of inducible aggregation in severely septic patients and determine its usefulness as a predictor of mortality. Platelet function tests using flow cytometry protocol presented the loss of platelet function in patients developing multiple organ dysfunction syndrome [25, 26]. In patients who received corticosteroids, we did not find significant variations either in the inducible platelet aggregation values or spontaneous aggregation values. Homogenously, all patients received low molecular weight heparin treatment which could slightly decrease platelet aggregation values but we analysed the changes of the inducible aggregation. Due to ethical concerns, the other recommended and regular treatments (vasopressor and inotropic agents, infusions for fluid replacement, insulin, stress ulcer prophylaxis, analgesics, sedatives, antibiotics etc.) were not investigated in drug free patient subgroups.
According to Lundhal et al.’s [25] theory more active platelets are activated and consumed in the early stage of sepsis therefore platelet activity should decrease during critical illness. Our data shows a significant deterioration in ADR, ADP, and COL induced aggregation compared to the control group but no change was observed during the 5-day period. Yaguchi et al. showed a loss of platelet aggregative function in patients with severe sepsis in contrast with other studies suggesting increased platelet function in trauma based septic shock patients [13, 27]. In concordance with Yaguchi’s findings [13], our study found a similar decrease in aggregation amongst severe septic patients.
Our measurements using Born’s optical method and saline as “inducer” showed significant aggregate formation in a group of severely septic patients compared to healthy controls. According to our current knowledge until now spontaneous platelet aggregation has never been measured using our technique with 0.9% saline, without inducers. In our previous pulmonary embolism studies [9] we did not verify any spontaneous aggregation values. It is known that platelets do not form aggregates in healthy individuals. Eto et al. [28] presented aggregates containing less than 100 platelets in patients with acute coronary syndrome using the high sensibility laser aggregometry light scattering method. Also patients with acute myocardial infarction have shown increased aggregation levels which correlate with the size of the necrotic tissue [29]. Until now studies have not reflected the use of saline as an alternative to inductors used for the measurement of spontaneous aggregation in severely septic patients.
Limitations
Due to the relatively small sample size, our investigation can be elucidated as a pilot study. Unfortunately, similar studies regarding spontaneous platelet aggregation in sepsis have not been performed to date to compare our data from the literature. This is truly a major limitation but at the same time of prime scientific value concerning our study. According to the current sepsis guidelines followed in intensive therapy, we were limited in our approach to create several separate drug free control groups.
Conclusion
Our hypothesis about the key role of highly inducible platelet aggregation in the development of microvascular flow insufficiency could not be confirmed. Our results proved that platelet aggregation can be altered by the actual platelet count. Concerning aggregability we found no significant difference between survival and non-survival patients therefore we cannot recommend this test as a mortality predictor.
Our main finding in this study is the spontaneous aggregation in septic patients. Spontaneous aggregation may cause microcirculatory disturbances therefore further investigations in the field are required.
References
Blanco J, Muriel-Bombín A, Sagredo V et al (2008) Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care 12:R158
Linde-Zwirble WT, Angus DC (2004) Severe sepsis epidemiology: sampling, selection, and society. Crit Care 8:222–226
Vincent J, Sakr Y, Sprung CL et al (2006) Sepsis in European intensive care units: results of the soap study. Crit Care Med 34:344–353
Barriere SL, Lowry SF (1995) An overview of mortality risk prediction in sepsis. Crit Care Med 23:376–393
Nguyen HB, Rivers EP, Abrahamian FM et al (2006) Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med 48:28–54
Gogos CA, Drosou E, Bassaris HP, Skoutelis A (2000) Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis 181:176–180
Zimmerman GA, McIntyre TM, Prescott SM, Stafforini DM (2002) The platelet-activating factor signaling system and its regulators in syndromes of inflammation and thrombosis. Crit Care Med 30:S294–S301
Schouten M, Wiersinga WJ, Levi M, Poll T (2008) Inflammation, endothelium, and coagulation in sepsis. J Leukoc Biol 83:536–545
Mühl D, Füredi R, Gecse K et al (2007) Time course of platelet aggregation during thrombolytic treatment of massive pulmonary embolism. Blood Coagul Fibrinolysis 18(7):661–667
Winning J, Reichel J, Eisenhut Y et al (2009) Anti-platelet drugs and outcome in severe infection: clinical impact and underlying mechanisms. Platelets 20(1):50–57
Lee KH, Hui KP, Tan WC (1993) Thrombocytopenia in sepsis: a predictor of mortality in the intensive care unit. Singapore Med J 34:245–246
Boldt J, Menges T, Wollbrück M et al (1994) Platelet function in critically ill patients. Chest 106:899–903
Yaguchi A, Lobo FL, Vincent JL, Pradier O (2004) Platelet function in sepsis. J Thromb Haemost 2:2096–2102
DeBacker D, Creteur J, Preiser JC et al (2002) Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 166:98–104
Spanos A, Jhanji S, Vivan-Smith A et al (2009) Early microvascular changes in sepsis and severe sepsis. Shock [Epub ahead of print]
Levy MM, Fink MP, Marshall JC et al (2001) SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31(4):1250–1256
Canan BI, Hülya S, Ercan G et al (2003) Usefulness of procalcitonin for diagnosis of sepsis in the intensive care unit. Crit Care 7(1):85–90
Müller B, Becker KL, Schächinger H et al (2000) Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med 28(4):977–983
Dellinger RP, Levy MM, Carlet JM et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36:296–327
Vincent JL, Moreno R, Takala J et al (1996) The sofa (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med 22:707–710
Marshall JC, Cook DJ, Christou NV et al (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652
Levi M, Löwenberg EC (2008) Thrombocytopenia in critically ill patients. Semin Thromb Hemost 34(5):417–424
Papp E, Havasi V, Bene J et al (2007) Does glycoprotein IIIa gene (Pl(A)) polymorphism influence clopidogrel resistance?: a study in older patients. Drugs Aging 24(4):345–350
Levi M, Opal SM (2006) Coagulation abnormalities in critically ill patients. Crit Care 10:222
Lundahl TH, Petersson J, Fagerberg IH et al (1998) Impaired platelet function correlates with multi-organ dysfunction. A study of patients with sepsis. Platelets 9:223–225
Alt E, Amann-Vesti BR, Madl C et al (2004) Platelet aggregation and blood rheology in severe sepsis/septic shock: relation to the sepsis-related organ failure assessment (sofa) score. Clin Hemorheol Microcirc 30:107–115
Davenport RA, Brohi K (2009) Coagulopathy in trauma patients: importance of thrombocyte function? Curr Opin Anaesthesiol 22:261–266
Eto K, Takeshita S, Ochiai M et al (1998) Platelet aggregation in acute coronary syndromes: use of a new aggregometer with laser light scattering to assess platelet aggregability. Cardiovasc Res 40:223–229
Spiel AO, Frossard M, Mayr FB et al (2009) Pronounced platelet hyperfunction in patients with cardiac arrest achieving restoration of spontaneous circulation. Crit Care Med 37:975–979
Acknowledgements
The authors would like to express their gratitude to Professor Samuel Z. Goldhaber for giving inspiration to this work. The authors also would like to thank the laboratory assistants and the nurses of the intensive care unit at the department of Anaesthesia and Intensive Therapy for their enormous contribution. This work was supported by the Hungarian Scientific Research Fund OTKA K060227 grant.
Conflict of interest statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woth, G., Varga, A., Ghosh, S. et al. Platelet aggregation in severe sepsis. J Thromb Thrombolysis 31, 6–12 (2011). https://doi.org/10.1007/s11239-010-0486-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-010-0486-0