Abstract
Diabetes has been shown to be associated with worse survival and repeat revascularization (TVR) after primary angioplasty. Drug-eluting stent (DES) may offer benefits in terms of TVR, that may be counterbalanced by an higher risk of stent thrombosis, especially among STEMI patients. Aim of the current study was to evaluate the impact of diabetes on 5-year outcome in patients undergoing primary angioplasty with Glycoprotein IIb–IIIa inhibitors in the era of DES. Our population is represented by STEMI patients undergoing primary angioplasty and stent implantation at a tertiary center with 24-h primary PCI capability within 12 h of symptom onset. All patients received glycoprotein IIb–IIIa inhibitors. No patient was lost to follow up. From 2003 to 2005, 270 STEMI patients were treated with DES (n = 180), or BMS (n = 90). A total of 69 patients had history of diabetes at admission (25.5%). At a follow-up of 1510 ± 406 days, diabetes was associated with a higher rate of death (29.5 vs. 5.1%, P < 0.0001), reinfarction (24.1 vs. 9.1%, P < 0.0001), TVR (19.1 vs. 13.1%, P = 0.052), IST (17.2 vs. 6.8%, P < 0.001) and MACE (51.9 vs. 25.1%, P < 0.001). These results were confirmed in both patients receiving BMS or DES, except for TVR, where no difference was observed between diabetic and non-diabetic patients. This study shows that among STEMI patients undergoing primary angioplasty with Gp IIb–IIIa inhibitors, diabetes is associated with worse long-term mortality, reinfarction, and IST, even with DES implantation, that, however, were able to equalize the outcome in terms of TVR as compared to non diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Several randomized trials and meta-analyses have shown that primary angioplasty is superior to thrombolytic therapy in the treatment of patients with ST-segment elevation myocardial infarction (STEMI) [1]. Stent implantation has further improved the outcome by reducing the occurrence of restenosis as compared to balloon angioplasty in selected STEMI patients [2, 3]. However, the outcome of bare metal stents seems to be worse in unselected patients with a rate of TVR up to 20% [4, 5], especially among diabetic patients [6–8]. Drug-eluting stents (DES) have been shown in several randomized trials to reduce restenosis and TVR in both elective [9–13] or STEMI patients [14–18] as compared to bare-metal stents (BMS). However, concerns have emerged on the potential higher risk of stent thrombosis and death with DES [19–22], that might be even more pronounced among STEMI patients, as suggested by a prospective registry [23]. In the PaclitAxel or Sirolimus-Eluting Stent vs Bare Metal Stent in primary angioplasty (PASEO) randomized trial 270 STEMI patients were randomized to SES, PES or BMS (1:1:1) [24, 25]. The aim of the current study was to evaluate the impact of diabetes on 5-year outcome in patients undergoing primary angioplasty with Glycoprotein IIb–IIIa inhibitors with or without DES.
Methods
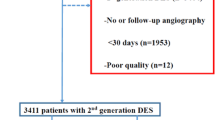
Our population is represented by STEMI patients undergoing primary angioplasty and randomized to BMS (n = 90), SES (n = 90) or PES (n = 90). Details on study design have already been reported [24, 25]. Briefly, individuals eligible for enrolment were consecutive patients presenting with STEMI who fulfilled all the following inclusion criteria: (1) chest pain for more than 30 min; (2) ST-segment elevation of 1 mm or more in 2 or more contiguous electrocardiograph leads or with presumably new left bundle-branch block; (3) Hospital admission within 12 h from symptoms onset. Exclusion criteria included: (1) Active internal bleeding or a history of bleeding diathesis within the previous 30 days; (2) A history of intracranial hemorrhage, intracranial neoplasm, arteriovenous malformation or aneurysm; (3) Known allergy to sirolimus, paclitaxel, heparin, aspirin, or clopidogrel; (4) A history of stroke within 30 days or any history of hemorrhagic stroke; (5) Major surgical procedure or severe physical trauma within the previous month; (6) History, symptoms, or findings suggestive of aortic dissection; (7) Thrombolytic/fibrinolytic therapy within 24 h; (8) History of thrombocytopenia; (9) Hemorrhagic retinopathy; (10) Patients on warfarin or acenocoumarol with INR ≥ 2; 11) Pregnancy. A vessel size <2.25 mm was the only exclusion angiographic criteria.
The institutional review board of the Ospedale “S.G. Moscati” (Avellino, Italy) approved the protocol in 2003, and all patients gave written informed consent.
Medications
All patients received in the coronary care unit 70U/Kg i.v. bolus of unfractionated heparin (UFH) plus 1000U/h infusion (to maintain an activated clotting time of at least 200 s), aspirin intravenously (500 mg) and clopidogrel (300 mg loading dose). All patients received upstream Gp IIb–IIIa inhibitors administration as a routine adjunctive therapy before primary PCI. Postinterventional antiplatelet therapy for all patients included in the three study group, consisted of aspirin (100 mg) indefinitely and clopidogrel (75 mg for 6 months).
Angioplasty procedure
Stenting procedures were performed according to standard techniques. The number and length of stents, and the type of BMS to be implanted, were left to the operator’s discretion. The operator was allowed to implant DES to cover the entire length of the lesion with coverage of the entire stented segment and of 5 mm proximal and distal segments. The use of IVUS, adjunctive thrombectomy devices, distal protection devices and IABP were left to the operator’s discretion.
Angiographic analysis
Thrombolysis in Myocardial Infarction (TIMI) grade 3 coronary flow in the treated vessel and a residual stenosis less than 30% were the criteria used to define a successful PCI. Quantitative angiographic analyses (Integris Allura, Philips, The Netherlands) were performed on line and off line by two experienced technicians who were unaware of treatment assignment with the averaging scores if they were non in agreement.
Data collection and follow-up
As per protocol, patients were reviewed at our outpatient clinic or by telephone interview at 6, 12, 24, 36, and between 48 and 72 months. For patients who died during follow up, hospital records and necropsy data were reviewed, when possible. No patient was lost to follow up.
Study end points and definitions
End points of this study were: Death, reinfarction (reMI), combined death/reMI, target-vessel revascularization (TVR), in-stent thrombosis (IST) and Major Adverse Cardiac Events (MACE) at 5-year follow-up.
All deaths were considered cardiac unless an unequivocal noncardiac cause could be identified. Recurrent MI was defined as recurrence on anginal symptoms with typical ECG changes and increase above upper limit of normal of CKMB or troponin. The indication for a second intervention had to be substantiated by symptoms or by ECG or scintigraphic evidence of ischaemia at rest or during exercise. Subsequent revascularisation of other coronary arteries did not constitute an end point.
Statistical analysis
Continuous data were expressed as median (25–75th percentiles) and categorical data as percentages. The analysis of variance was appropriately used for continuous variables. The χ2 test or the Fisher’s exact test was used for categorical variables. The difference in event rates between groups during the follow up period was assessed by the Kaplan–Meier method with the log rank test. A probability value of P < 0.05 was considered significant. Statistical analysis was performed using SPSS 15.0.
Results
Patient population
Our population is represented by 270 patients with STEMI. Diabetes was observed in 69 patients (34.1%). As shown in Table 1, no difference in demographic and clinical characteristics was observed between the two groups. As shown in Table 2, no difference was observed in terms of angiographic and procedural characteristics. Almost 50% of patients underwent PCI of left anterior descending artery. All patients received upstream glycoprotein IIb–IIIa inhibitors. Procedural success was obtained in 93–95% of patients. A direct stenting strategy was adopted in 24–29% of patients. As reported in Table 3, no difference was observed in terms of clopidogrel prescription between the two groups, with almost all patients stopping clopidogrel therapy at 6 months follow-up.
Diabetes and long-term outcome
Follow-up data were available in all patients at 1510 ± 406 days. As reported in Table 4, at long-term follow-up diabetes was associated with a significantly higher rate of death (29.5 vs. 5.1%, HR [95% CI] = 9.75 [4.11–23.1], P < 0.0001) (Fig. 1), reinfarction (24.1 vs. 9.1% HR [95% CI] = 3.42 [1.66–7.01], P < 0.0001) (Fig. 2), death/reMI (44.8 vs. 13.7%, HR [95% CI] = 5.17 [2.98–8.98], P < 0.001) (Fig. 3), IST (17.2 vs. 6.8%, HR [95% CI] = 6.3 [2.33–17.1], P < 0.001) (Fig. 4) and MACE (51.9 vs. 25.1%, HR [95% CI] = 3.24 [2.06–5.08], P < 0.001) (Fig. 6). These results were confirmed in both patients receiving BMS or DES, except for TVR, where no difference was observed between diabetes and non-diabetic patients. In the analysis restricted to diabetic patients, DES, as compared to BMS, were associated with a significant reduction in TVR (14.3 vs. 27.3%, HR [95% CI] = 0.13 [0.034–0.46], P = 0.002) (Fig. 5) and MACE (38.4 vs. 88.3%, HR [95% CI] = 0.34 [0.17–0.66], P = 0.002) (Fig. 6), and slightly benefits in terms of death (25.1 vs. 39.1%, HR [95% CI] = 0.54 [0.22–1.31], P = 0.17) (Fig. 1), reinfarction (17.8 vs. 38.3%, HR [95% CI] = 0.43 [0.15–1.24], P = 0.12) (Fig. 2) and in-stent thrombosis (27.7 vs. 14.3%, HR [95% CI] = 0.55 [0.17–1.8], P = 0.32) (Fig. 4).
Discussion
The main finding of the present study is that diabetes was associated with a significantly higher mortality, reinfarction, TVR and IST. These results were similarly observed among patients treated with BMS or DES, except for TVR, where no difference was observed among patients treated with DES. Among diabetic patients, the use of DES was safe, with a non significant reduction in death and reinfarction and IST but a significant reduction in TVR and overall MACE, as compared to BMS.
Several studies have demonstrated that hyperglycemia at admission is associated with larger infarct size and higher mortality in patients with STEMI [26–31]. In fact, several in vitro and in vivo experiments have shown that hyperglycemia may be involved in the reperfusion injury. Acute hyperglycemia increases intercellular adhesion molecule-1 levels [32], which would augment plugging of leukocytes in the capillaries [33]. Furthermore, leukocytes trapped in the coronary capillaries and venules early after coronary reperfusion are much more frequently observed in the diabetic rat heart than in the nondiabetic heart [34]. Plugging of enhanced leukocytes in the microcirculation may further contribute to the impaired myocardial perfusion [35]. Hyperglycaemia may also augment thrombus formation. Blood glucose has been demonstrated to be an independent predictor of platelet-dependent thrombosis, even in the normal range [36]. A recent study suggested that a microthrombus in the capillaries play a crucial role in the no-reflow phenomenon after STEMI [37]. Finally, diabetes has also been associated with abnormal coronary endothelial function, diminished coronary flow reserve, and impaired ischemic preconditioning [38–40], all of which may result in abnormal myocardial perfusion.
In a recent report, De Luca et al. [41] found among patients treated with Gp IIb–IIIa inhibitors that diabetes was associated with higher occurrence of distal embolization, impaired myocardial reperfusion, and higher mortality.
However, diabetes is associated with a significantly higher rates of restenosis [6–8]. In a previous report, De Luca et al. [42], found that BMS did not provide significant benefits in outcome as compared to balloon angioplasty in unselected diabetic patients undergoing primary angioplasty. The recent introduction of DES, has certainly reduced the risk of restenosis, that may be counterbalanced by an higher rate of late in-stent thrombosis, especially among STEMI. A recent individual patients’ data meta-analysis showed that, among STEMI diabetic patients undergoing primary angioplasty, the use of DES was safe, and associated with a significant reduction in TVR at 1-year follow-up. However, it has been described a late catch-up phenomenon in terms of restenosis, with a potential risk of late in-stent thrombosis.
Our study is the first one evaluating the impact of diabetes on 5-year outcome among STEMI patients undergoing primary angioplasty in the era of DES. Diabetes was associated with a significantly higher mortality, reinfarction, TVR and IST, irrespective of DES or BMS, except than for TVR. In fact, among patients treated with DES, no difference was observed between diabetic and non-diabetic patients. Furthermore, among diabetic patients, the use of DES was safe, with a non significant reduction in death and reinfarction, similar rates of IST but a significant reduction in TVR and overall MACE, as compared to BMS.
Limitations
Despite long-term follow-up data, due to the relatively small sample size, this study can not provide definite conclusions on DES safety in terms of death and reinfarction in diabetic patients, that will hopefully be provided by large randomized trials.
The relatively high rate of cardiogenic shock observed in our study may be due to the fact that in peripheral hospitals of our province lysis still represents, if not contraindicated, the initial preferred strategy, whereas primary angioplasty is preferred in patients with haemodynamic compromise that are therefore transferred to our hospital to undergo mechanical reperfusion.
Conclusions
This study shows that among STEMI patients undergoing primary angioplasty with Gp IIb–IIIa inhibitors, diabetes is associated with worse long-term mortality, reinfarction, and IST, even with DES implantation, that, however, were able to equalize the outcome in terms of TVR as compared to non diabetic patients.
References
Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361:13–20
Stone GW, Grines CL, Cox DA, Garcia E, Tcheng JE, Griffin JJ, Guagliumi G, Stuckey T, Turco M, Carroll JD, Rutherford BD, Lansky AJ (2002) Controlled abciximab and device investigation to lower late angioplasty complications (CADILLAC) investigators. Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction. N Engl J Med 346:957–966
De Luca G, Suryapranata H, Stone GW, Antoniucci D, Biondi-Zoccai G, Kastrati A, Chiariello M, Marino P (2008) Coronary stenting versus balloon angioplasty for acute myocardial infarction: a meta-regression analysis of randomized trials. Int J Cardiol 126:37–44
Antoniucci D, Migliorini A, Parodi G, Valenti R, Rodriguez A, Hempel A, Memisha G, Santoro GM (2004) Abciximab-supported infarct artery stent implantation for acute myocardial infarction and long-term survival: a prospective, multicenter, randomized trial comparing infarct artery stenting plus abciximab with stenting alone. Circulation 109:1704–1706
Suryapranata H, De Luca G, van’t Hof AW, Ottervanger JP, Hoorntje JC, Dambrink JH, Gosselink AT, Zijlstra F, de Boer MJ (2005) Is routine stenting for acute myocardial infarction superior to balloon angioplasty? A randomised comparison in a large cohort of unselected patients. Heart 91:641–645
Elezi S, Kastrati A, Pache J, Wehinger A, Hadamitzky M, Dirschinger J, Neumann FJ, Schomig A (1998) Diabetes mellitus and the clinical and angiographic outcome after coronary stent placement. J Am Coll Cardiol 32:1866–1873
Kornowski R, Mintz GS, Kent KM, Pichard AD, Satler LF, Bucher TA, Hong MK, Popma JJ, Leon MB (1997) Increased restenosis in diabetes mellitus after coronary interventions is due to exaggerated intimal hyperplasia: a serial intravascular ultrasound study. Circulation 95:1366–1369
Bolognese L, Carrabba N, Santoro GM, Valenti R, Buonamici P, Antoniucci D (2003) Angiographic findings, time course of regional and global left ventricular function, and clinical outcome in diabetic patients with acute myocardial infarction treated with primary percutaneous transluminal coronary angioplasty. Am J Cardiol 91:544–549
Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C et al (2003) SIRIUS investigators. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 349:1315–1323
Stone GW, Ellis SG, Cox DA, Hermiller J, O’Shaughnessy C, Mann JT et al (2004) TAXUS-IV Investigators; TAXUS-IV Investigators. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med 350:221–231
Ardissino D, Cavallini C, Bramucci E, Indolfi C, Marzocchi A, Manari A et al (2004) SES-SMART investigators. Sirolimus-eluting vs uncoated stents for prevention of restenosis in small coronary arteries: a randomized trial. JAMA 292:2727–2734
Colombo A, Moses JW, Morice MC, Ludwig J, Holmes DR Jr, Spanos V et al (2004) Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation 109:1244–1249
Roiron C, Sanchez P, Bouzamondo A, Lechat P, Montalescot G (2006) Drug eluting stents: an updated meta-analysis of randomised controlled trials. Heart 92:641–649
Valgimigli M, Bolognese L, Anselmi M, Campo G, Rodriguez AE, de Cesare N et al (2005) Tirofiban and sirolimus-eluting stent vs. abciximab and bare-metal stent for acute myocardial infarction: a randomized trial. JAMA 293:2109–2117
Spaulding C, Henry P, Teiger E, Beatt K, Bramucci E, Carrié D et al (2006) TYPHOON investigators. Sirolimus-eluting versus uncoated stents in acute myocardial infarction. N Engl J Med 355:1093–1104
Menichelli M, Parma A, Pucci E, Fiorilli R, De Felice F, Nazzaro M et al (2007) Randomized trial of sirolimus-eluting stent versus bare-metal stent in acute myocardial infarction (SESAMI). J Am Coll Cardiol 49:1924–1930
van der Hoeven BL, Liem SS, Jukema JW, Suraphakdee N, Putter H, Dijkstra J, Atsma DE, Bootsma M, Zeppenfeld K, Oemrawsingh PV, van der Wall EE, Schalij MJ (2008) Sirolimus-eluting stents versus bare-metal stents in patients with ST-segment elevation myocardial infarction: 9-month angiographic and intravascular ultrasound results and 12-month clinical outcome results from the MISSION! Intervention study. J Am Coll Cardiol 51:618–626
Valgimigli M, Campo G, Percoco G, Bolognese L, Vassanelli C, Colangelo S, de Cesare N, Rodriguez AE, Ferrario M, Moreno R, Piva T, Sheiban I, Pasquetto G, Prati F, Nazzaro MS, Parrinello G, Ferrari R (2008) Multicentre evaluation of single high-dose bolus tirofiban vs abciximab with sirolimus-eluting stent or bare metal stent in acute myocardial infarction study (MULTISTRATEGY) investigators. Comparison of angioplasty with infusion of tirofiban or abciximab and with implantation of sirolimus-eluting or uncoated stents for acute myocardial infarction: the MULTISTRATEGY randomized trial. JAMA 299:1788–1799
McFadden EP, Stabile E, Regar E, Cheneau E, Ong AT, Kinnaird T et al (2004) Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet 364:1519–1521
Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G et al (2005) Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293:2126–2130
Lagerqvist B, James SK, Stenestrand U, Lindbäck J, Nilsson T, Wallentin L, SCAAR Study Group (2007) Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med 356:1009–1019
Kernis SJ, Cohen D, Rein K (2005) Clinical outcome associated with use of drug-eluting stents compared with bare metal stent for primary percutaneous intervention. Am J Cardiol 96(suppl 7A):47H
Spertus JA, Kettelkamp R, Vance C, Decker C, Jones PG, Rumsfeld JS et al (2006) Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation 113:2803–2809
Di Lorenzo E, De Luca G, Sauro R et al (2009) PaclitAxel or Sirolimus-Eluting Stent vs Bare Metal Stent in primary angioplasty (PASEO) randomized trial. JACC Cardiovasc Interv 2:515–523
Di Lorenzo E, Sauro R, Varricchio A et al (2009) Long-term outcome of drug-eluting stents compared with bare metal stents in ST-segment elevation myocardial infarction: results of the paclitaxel- or sirolimus-eluting stent versus bare metal stent in Primary Angioplasty (PASEO) randomized trial. Circulation 120:964–972
Capes SE, Hunt D, Malmberg K, Gerstein HC (2000) Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355:773–778
Bolk J, van der Ploeg T, Cornel JH, Arnold AE, Sepers J, Umans VA (2001) Impaired glucose metabolism predicts mortality after a myocardial infarction. Int J Cardiol 79:207–214
Porter A, Assali AR, Zahalka A, Iakobishvili Z, Brosh D, Lev EI, Mager A, Battler A, Kornowski R, Hasdai D (2008) Impaired fasting glucose and outcomes of ST-elevation acute coronary syndrome treated with primary percutaneous intervention among patients without previously known diabetes mellitus. Am Heart J 155(2):284–289
Marso SP, Miller T, Rutherford BD, Gibbons RJ, Qureshi M, Kalynych A, Turco M, Schultheiss HP, Mehran R, Krucoff MW, Lansky AJ, Stone GW (2007) Comparison of myocardial reperfusion in patients undergoing percutaneous coronary intervention in ST-segment elevation acute myocardial infarction with versus without diabetes mellitus (from the EMERALD Trial). Am J Cardiol 100(2):206–210
Ishihara M, Kagawa E, Inoue I, Kawagoe T, Shimatani Y, Kurisu S, Nakama Y, Maruhashi T, Ookawa K, Dai K, Aokage Y (2007) Impact of admission hyperglycemia and diabetes mellitus on short- and long-term mortality after acute myocardial infarction in the coronary intervention era. Am J Cardiol 99(12):1674–1679
Timmer JR, van der Horst IC, de Luca G, Ottervanger JP, Hoorntje JC, de Boer MJ, Suryapranata H, Dambrink JH, Gosselink M, Zijlstra F, van’t Hof AW, Zwolle Myocardial Infarction Study Group (2005) Comparison of myocardial perfusion after successful primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction with versus without diabetes mellitus. Am J Cardiol 95(11):1375–1377
Marfella R, Esposito K, Giunta R, Coppola G, De Angelis L, Farzati B, Paolisso G, Giugliano D (2000) Circulating adhesion molecules in humans: role of hyperglycemia and hyperinsulinemia. Circulation 101:2247–2251
Booth G, Stalker TJ, Lefer AM, Scalia R (2001) Elevated ambient glucose induces acute inflammatory events in the microvasculature: effects of insulin. Am J Physiol Endocrinol Metab 280:E848–E856
Hokama JY, Ritter LS, Davis-Gorman G, Cimetta AD, Copeland JG, McDonagh PF (2000) Diabetes enhances leukocyte accumulation in the coronary microcirculation early in reperfusion following ischemia. J Diabetes Complications 14:96–107
Engler RL, Dahlgren MD, Morris DD, Peterson MA, Schmid-Schonbein GW (1986) Role of leukocytes in response to acute myocardial ischemia and reflow in dogs. Am J Physiol 251:H314–H323
Shechter M, Merz CN, Paul-Labrador MJ, Kaul S (2000) Blood glucose and platelet-dependent thrombosis in patients with coronary artery disease. J Am Coll Cardiol 35:300–307
Sakuma T, Leong-Poi H, Fisher NG, Goodman NC, Kaul S (2003) Further insights into the no-reflow phenomenon after primary angioplasty in acute myocardial infarction: the role of microthromboemboli. J Am Soc Echocardiogr 16:15–21
Nitenberg A, Valensi P, Sachs R, Dali M, Aptecar E, Attali J-R (1993) Impairment of coronary vascular reserve and ACh-induced coronary vasodilation in diabetic patients with angiographically normal coronary arteries and normal left ventricular systolic function. Diabetes 42:1017–1025
Nahser PJ Jr, Brown RE, Oskarsson H, Winniford MD, Rossen JD (1995) Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. Circulation 91:635–640
Ishihara M, Inoue I, Kawagoe T, Shimatani Y, Kurisu S, Nishioka K, Kouno Y, Umemura T, Nakamura S, Sato H (2001) Diabetes mellitus prevents ischemic preconditioning in patients with a first acute anterior wall myocardial infarction. J Am Coll Cardiol 38:1007–1011
De Luca G, Michael Gibson C, Bellandi F, Murphy S, Maioli M, Noc M, Zeymer U, Dudek D, Arntz HR, Zorman S, Gabriel HM, Emre A, Cutlip D, Rakowski T, Gyongyosi M, Huber K, Van’t Hof AW (2009) Benefits of pharmacological facilitation with glycoprotein IIb-IIIa inhibitors in diabetic patients undergoing primary angioplasty for STEMI. A subanalysis of the EGYPT cooperation. J Thromb Thrombolysis 28(3):288–298
De Luca G, Suryapranata H, Timmer J, Ottervanger JP, van’t Hof AW, Hoorntje JC, Dambrink JH, Gosselink AT, de Boer MJ (2006) Impact of routine stenting on clinical outcome in diabetic patients undergoing primary angioplasty for ST-segment elevation myocardial infarction. Diabetes Care 29:920–923
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Luca, G., Sauro, R., Varricchio, A. et al. Impact of diabetes on long-term outcome in STEMI patients undergoing primary angioplasty with glycoprotein IIb–IIIa inhibitors and BMS or DES. J Thromb Thrombolysis 30, 133–141 (2010). https://doi.org/10.1007/s11239-009-0420-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-009-0420-5