Abstract
Erythropoietin (Epo) is a hematopoietic hormone produced mainly by the kidneys in response to hypoxia. Recent acquisitions in the fields of hematology, neurology, cardiology, and experimental medicine show cytoprotective, angiogenetic and antinflammatory effects of Epo. Exogenous erythroPoietin in Acute Myocardial Infarction: New Outlook aNd Dose Association Study (EPAMINONDAS, EudraCTno. 200500485386) is one of four ongoing randomized controlled trials, each testing the effects of Epo in ≥100 patients with STEMI. EPAMINONDAS is a multicenter, prospective, double-blind, placebo-controlled, dose-finding study assessing intravenous moderate doses of human recombinant Epo (epoietin-α, 100 or 200 IU/kg/die) versus placebo, given on the first 3 days, in 102 patients with first ST-segment elevation myocardial infarction. Initial dosing is within 12 h of primary percutaneous coronary revascularization. The primary endpoint is infarct size, quantified by CK-MB time–concentration curve, left ventricular wall motion score index, and pattern of contrast-enhanced magnetic resonance imaging. Secondary endpoints are ischemic recurrences, ventricular remodelling, and safety events, assessed in-hospital and at 12 months’ follow-up. The results of current phase II studies will help define the safety/efficacy profile of Epo for patients with STEMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction remains a public health problem and a main cause of death, often premature, in many developing countries [1]. Despite improved clinical outcomes by early thrombolysis and/or angioplasty, in-hospital mortality in ST-elevation myocardial infarction (STEMI) is still high, approximating 5% in the Global Registry of Acute Coronary Events [2]. Beyond the acute phase, adverse ventricular remodelling, heart failure, and mortality are directly related to infarct size and to left ventricular (LV) dysfunction [3, 4]. Thus, cardiomyocyte salvage remains a primary aim of effective treatment.
Experimental studies indicate that cardiomyocytes threatened by necrotic or apoptotic damage can be rescued by growth factors, such as erythropoietin (Epo) [5] and insulin-like growth factor-1 (IGF-1) [6, 7]. Indeed, Epo and its receptor (EpoR) exert biological functions that go beyond erythropoiesis [8, 9] and that include broad antiapoptotic actions, mediated by Bcl-2 and Bcl-XL, proangiogenetic, and antinflammatory effects [8, 9]. Moreover, the Epo–EpoR system enhances the synthesis and bioavailability of constitutive nitric oxide (NO) [10], through endothelial NO synthase transcription and activation, increases coronary flow-reserve [11], recruits bone-marrow and/or cardiac pluripotential precursor cells [12, 13], and has membrane-stabilizing and insulin-sensitizing actions [5], in synergy with IGF-1 [14]. Epo is thus emerging as a potentially important heart and vascular protective hormone [15].
EPAMINONDAS: design and end points
EPAMINONDAS (Exogenous erythroPoietin in Acute Myocardial Infarction: New Outlook aNd Dose Association Study) is a multicenter, prospective, randomized, double-bind, placebo-controlled, dose-finding, phase II trial testing the effects on infarct size of two intravenous (i.v.) doses of epoietin-α, administered on the first 3 days of hospitalization to a homogeneous group of 102 patients with a first STEMI. The first dose of drug or placebo is given within 12 hours (h) of primary percutaneous coronary intervention (PCI).
The primary end point is to assess the dose-dependent effects of Epo compared to placebo on infarct size. The latter is estimated by serum CK-MB 24 h time–concentration curves in the acute phase, and by LV wall motion score index, LV ejection fraction, and extent of “delayed enhancement” by contrast-enhanced magnetic resonance (MR), assessed at discharge and at 12 months’ follow-up.
The secondary endpoints are to assess the effects of two doses of Epo versus placebo on the incidence of major adverse events and on LV remodelling at 12 months’ follow-up. The incidence of major adverse events [defined as cardiovascular death, death from other cause, nonfatal myocardial infarction, nonfatal ischemic stroke, cardiogenic shock, rehospitalization for recurrent ischemia, heart failure, pulmonary embolism or other life-threatening conditions, sustained ventricular arrhythmias, atrial fibrillation, major bleeds (including intracranial), deep vein thrombosis, new onset hemodialysis or ultrafiltration, mechanical ventilation, uncontrolled hypertension] is recorded by 3-monthly interviews, hospital records, and clinical visits with 12-lead ECGs at follow-up. LV remodelling is assessed by echocardiography and cardiac MR, based on global and regional changes in geometry and function from discharge to follow-up.
Methods
Patients
Consecutive patients with diagnostic signs and symptoms of STEMI, satisfying the study criteria (Fig. 1), and with a Thrombolysis In Myocardial Infarction (TIMI) flow grade 0-1 in the infarct-related artery on initial angiography are eligible. Immediately after successful PCI, patients are asked for written informed consent and, if they agree, are assigned—according to a pre-defined randomization scheme—to receive Epo or placebo on top of optimal standard medical care. Neither the patient, nor the attending physician, nor the staff performing echocardiography, MR, or the clinical follow-up are aware of the assigned treatment. A total of 102 patients are scheduled.
Treatment
Prior to or at the time of primary PCI, standard antithrombotic treatment for STEMI is administered, consisting of aspirin, heparin, clopidogrel, and abciximab [1]. On arrival into the coronary care unit and within 12 h of PCI, enrolled patients are randomly assigned to placebo or one of two Epo doses (100 or 200 IU/kg/day). Active drug or placebo are diluted in 100 ml of saline and administered i.v. over 30 min for the first 3 days, under regular blood pressure and continuous ECG monitoring. The double-blind administration is ensured by a treatment code unknown to physicians, nurses and patients. Drug or placebo is prepared, under medical supervision, by nurses not involved in the study, according to instructions contained in predefined packages provided by the Pharmacy. Standard treatment, including β-blockade, lipid-lowering therapy, and angiotensin-converting enzyme inhibition or angiotensin-II receptor blockade, is additionally prescribed [1].
Clinical and laboratory measures
Blood pressure, heart rate, and ECG are monitored in the coronary care unit and then at regular time points until discharge. Major adverse events (as defined above) are recorded during hospitalization and up to 12 months’ thereafter. Before discharge and at 12 months, the following are also performed and recorded: physical exam, 12-lead ECG, 2-D echocardiogram, and cardiac MR.
LV remodelling is defined as a >20% change in end-diastolic volume at follow-up compared to pre-discharge values. Absolute changes in LV ejection fraction, contractility by wall motion score index, and MR contrast-enhanced first-pass and delayed enhancement perfusion imaging at follow-up versus pre-discharge are also recorded. During follow-up, patients are assessed every 3 months, either as out-patients or by telephone call. An independent data safety monitoring board receives real-time clinical information, performs interim safety analyses at 25, 50, 75 and 100% recruitment, and provides regular feedback to the investigators.
Biochemical measurements
Six-hourly serial blood samples are drawn from the time of enrolment up to 24 h, for the serum determination of creatine-kinase (CK)-MB. Full blood cell and reticulocyte count, AST and ALT are measured daily during the first 3 days, and before discharge. A venous blood sample for future determinations is also taken, processed, and stored, at baseline, discharge and follow-up.
Statistical analysis
The sample size of 102 patients has been selected to detect differences in the primary endpoint variables (expressed as means and standard deviations and estimated according to current literature) with a power of 0.8 and an alfa value of 0.01. Bonferroni’s correction is applied to repeated comparisons. Comparisons are made between Epo and placebo-treated patients, and among the three different treatment arms. Statistical analyses are performed using the SPSS program (version 11).
Centers and financial support
EPAMINONDAS involves three clinical centers located in Rome (Italy), each enrolling 34 patients and performing/recording clinical and laboratory exams, as per protocol. The scientific coordinator of the investigation and head of the research unit within the Department of Cardiovascular Medicine of the “Gemelli” University Hospital is Dr. F. Andreotti. This center acts as core laboratory for randomization and for the centralized biochemical analyses. Head of the research unit within the Department of Cardiology of the Sant’Andrea Hospital of the 2nd Faculty of the University “La Sapienza” is Dr. C. Autore. This center acts as core laboratory for cardiac MR, in collaboration with the “Gemelli” Radiology department. Head of the research unit within the Department of Cardiology of the Umberto I Hospital of the 1st Faculty of the University “La Sapienza” is Prof. L. Agati. This center acts as echocardiographic core laboratory. EPAMINONDAS is funded by the Italian “Ministero dell’Istruzione, dell’Università e della Ricerca” (PRIN 2006_6063891).
Discussion
Non-hematopoietic effects of Epo
Epo’s predominant role is red cell production through prevention of erythroid precursor cell apoptosis and by promoting proliferation and maturation of erythroid progenitor cells [14]. Non-hematopoietic effects of Epo, however, have been recently described [15, 16], consistent with the discovery of Epo receptors on the same cells that synthesize Epo, as well as on cardiomyocytes, cardiac fibroblasts, and endothelial, retinal, gastric, prostate and vascular smooth muscle cells [15]. Epo production occurs mainly in peritubular kidney cells under the control of hypoxia inducible factor-1 [17], but Epo mRNA has recently been found also in extrarenal tissues, including liver, spleen, brain, lung, bone marrow, and reproductive organs [15].
Potential cardioprotective effects of Epo
Reasons to believe that Epo may improve cardiac function in patients with acute myocardial infarction are based on a large body of evidence [16]. Initial experiments in rats showed consistent cardioprotection by Epo following ischemia-reperfusion or permanent coronary artery ligation [18–20], through multiple antiapoptotic pathways, independent of increases in hematocrit. High doses given intraperitoneally (i.p., 5,000 IU/kg/day) for seven consecutive days, starting before or after transient (30 min) coronary artery occlusion, compared with saline, reduced cardiomyocyte loss by 50% [19]. Even a single i.p. dose (3,000 IU/kg), compared with saline, decreased apoptosis and reduced infarct size to approximately 1/3 when given immediately after permanent coronary artery occlusion [20]. In contrast, subcutaneous injections (5,000 IU/kg/day) starting 24 h before, at the time of, and for 5 days after permanent left anterior descending coronary artery ligation, did not improve long-term cardiac function in the same animal species [21]. In a similar model, a single i.v. dose (3,000 IU/kg), compared with saline, decreased apoptosis and reduced infarct size when given immediately or 4, 8, or 12 h after infarction, but not after 24 h [22]. On balance, these data suggest that Epo administration in rats is effective when given i.p. or i.v. (but not subcutaneously) and when started within a day after infarction. For a broad review of animal and clinical studies investigating the effects of Epo on myocardial necrosis and/or apoptosis, see Riksen et al. [16]. Benefits of Epo on ischemic myocardium have been reported to occur in rats, mice, rabbits and dogs, but not in pigs or sheep [16].
To date, studies investigating the potential protective effects of Epo in human cardiac ischemia are extremely limited. Accordingly, several trials are being performed in the attempt to translate the cardioprotection found in experimental models to patients with acute myocardial infarction.
Safety of Epo in cardiac patients
Epo has been administered to heart failure patients with or without diabetes, anemia or renal failure [23, 24]. In these trials, subcutaneous doses, ranging from 15,000–30,000 IU/week for 3 months to 4,000 IU/week for 1 year, showed benefits, in terms of reduced length and rate of hospitalizations, reduced progression of renal impairment, increased LV ejection fraction, and improved exercise tolerance, in the absence of Epo-related complications [23, 24].
The administration of Epo to patients with acute cardiovascular diseases may raise concerns stemming from potential prothrombotic effects, increased hematocrit, and hypertension [25]. Initial data reporting an increased frequency of thrombotic events came from retrospective non-randomized studies [26, 27] or from prospective randomized studies conducted in chronically diseased populations receiving prolonged Epo dosings (>400 IU/kg/week for months or years) [28]. Increased hematocrits have been observed particularly with simultaneous iron administration. Among 40 acute ischemic stroke patients, i.v. epoietin (33,000 IU/day) for the first 3 days compared to saline resulted in significantly improved neurological outcomes and no safety concerns at 30 days [29]. Another investigation assessed the effects of relatively high doses of epoietin α (40,000 IU/week for up to 3 weeks compared to placebo) in 1,460 critically ill medical, surgical or trauma patients [30]. Among those receiving Epo, there was no effect on transfusion rates, with an increased rate of thrombotic vascular events at 140 days (16.5 vs. 11.5%, P = 0.008) [30]. However, Epo was associated with a striking and significant reduction of mortality at 29 and 140 days among the prespecified group of trauma patients who, on average, were 20 years younger than the other patient groups [30]. Thus, Epo may exert beneficial effects in specific groups, but high total doses may cause thrombotic complications, especially in older patients not receiving antithrombotic therapy.
Phase II studies of Epo in STEMI patients
Currently, at least four randomized controlled trials, each of ≥100 patients with STEMI, are testing the effects of i.v. Epo administration on infarct size. An initial single-center, open-label pilot investigation evaluated the safety and tolerability in 22 non-anemic patients with acute STEMI randomized to a single bolus of 300 μg of darbepoetin alfa (~60,000 IU of epoietin α) or to no additional medication before primary PCI [31]. Adverse events were not observed during a 30-day follow-up. LV ejection fraction did not differ significantly at 4 months (52 ± 3% for darbepoetin vs. 48 ± 5% for controls) [31]. An ongoing multicenter, randomized, open-label trial is enrolling 466 patients with STEMI within 3 h after successful primary PCI to receive a single 60,000 IU bolus of epoietin (unspecified) on top of standard medical care vs. only standard medical care. The effect of Epo on LV ejection fraction is assessed by planar radionuclide ventriculography after 6 weeks from the acute event [32].
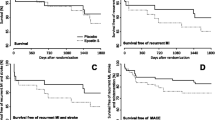
REVEAL (Reduction of infarct Expansion and Ventricular remodelling with Erythropoietin After Large myocardial infarction) is a double-blind, randomized, placebo-controlled, dose-finding, parallel-phase II study coordinated by the Duke University Medical Center, enrolling 210 patients with first STEMI, within 8 h from the onset of symptoms and treated by successful primary or rescue PCI. The primary aim is to evaluate the effects of a single administration of epoietin α (15,000, 30,000 or 60,000 IU in a dose-escalation safety phase followed by an efficacy phase) on infarct size and LV remodelling. Infarct size is assessed by cardiac MR within 2–6 days of the study medication, and again approximately 3 months later [33]. REVIVAL-3 (Regeneration of Vital Myocardium in ST-Segment Elevation Myocardial Infarction by Erythropoietin) is a German double-blind, placebo-controlled, randomized trial that has recently reported results on 138 patients with a first STEMI undergoing primary PCI. Immediately after balloon inflation and after 24 and 48 h, 68 patients received epoietin β (33,000 IU/dose) and 70 received placebo. The primary end point was LV ejection fraction at 6 months’ follow-up measured by MR. LV function and infarct size were not significantly different at discharge in the two groups. There was a trend towards a higher rate of adverse events at 6 months’ follow-up in the Epo treated group [34]. A recent pilot study administered a single i.v. dose of 40,000 IU of Epo to patients presenting with non-ST segment elevation acute coronary syndromes: plasma levels of troponin I and creatine kinase were not reduced by Epo [35]. The main characteristics of all these studies are shown in Table 1.
EPAMINONDAS is the 4th large phase II study of Epo in STEMI patients, contributing to the search of novel treatments aimed at reducing early mortality and late heart failure. It has the following distinctive features: it is double-bind and dose-finding; the first administration occurs after successful PCI, with three consecutive dosings; the total Epo dose (for body weights of 70 kg) is moderate (<50,000 IU), rather than high (>60,000 IU); the dose of active drug is weight-adjusted; finally, the extent of follow-up is 12 months. EPAMINONDAS will contribute to define Epo’s safety and potential efficacy (or lack thereof) in reducing infarct size in STEMI patients. To date, among the 68 enrolled patients, the rate of adverse events at follow-up has been low with no significant differences among the three treatment arms [36].
In conclusion, Epo is a hematopoietic hormone found to have potential cardioprotective effects against prolonged ischemia through antiapoptotic properties, promotion of neovascularization, and stem cell-mediated repair. Although animal studies have shown protection against infarcted myocardium, initial clinical testing has failed to show striking benefits. The conclusion of current phase II, randomized, placebo-controlled trials is awaited to more fully assess the cardiac effects of Epo administered at different doses and times, and to carefully monitor its safety profile in patients with STEMI.
References
Van de Werf F, Bax J, Betriu A et al (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation. Eur Heart J 29(23):2909–2945
Fox KAA, Steg GP, Eagle KA et al (2007) Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA 297(17):1892–1900
Biagini E, van Geuns RJ, Baks T et al (2006) Comparison between contrast echocardiography and magnetic resonance imaging to predict improvement of myocardial function after primary coronary intervention. Am J Cardiol 97(3):361–366
Takemura G, Nakagawa M, Kanamori H, et al (2009) Benefits of reperfusion beyond infarct size limitation. Cardiovasc Res, Feb 18 (Epub ahead of print)
Andreotti F, Crea F, Conti E (2004) Heart-kidney interactions in ischemic syndromes. Circulation 109(5):e31–e32
Conti E, Carrozza C, Capoluongo E et al (2004) Insulin-like growth factor-1 as a vascular protective factor. Circulation 110(15):2260–2265
Conti E, Musumeci MB, Assenza GE et al (2008) Recombinant human insulin-like growth factor-1: a new cardiovascular disease treatment option? Cardiovasc Hematol Agents Med Chem 6(4):258–271
Maiese K, Li F, Chong ZZ (2005) New avenues of exploration for erythropoietin. JAMA 293(1):90–95
Bogoyevitch MA (2004) An update on the cardiac effects of erythropoietin and the lessons learnt from studies in neuroprotection. Cardiovasc Res 63(2):208–216
Cai Z, Semenza GL (2004) Phosphatidylinositol-3-kinase signaling is required for erythropoietin-mediated acute protection against myocardial ischemia/reperfusion injury. Circulation 109(17):2050–2053
van de Meer P, Lipsic E, Henning RH et al (2004) Erythropoietin improves left ventricular function and coronary flow in an experimental model of ischemia-reperfusion injury. Eur J Heart Failure 6(7):853–859
Heeschen C, Aicher A, Lehmann R et al (2003) Erythropoietin is a potent physiologic stimulus for endothelial progenitor cell mobilization. Blood 102(4):1340–1346
Messina E, De Angelis L, Frati G et al (2004) Isolation and expansion of adult cardiac stem cells from human and murine heart. Circ Res 95:852–854
Fisher JW (2003) Erythropoietin: physiology and pharmacology update. Exp Biol Med 228(1):1–14
Marzo F, Lavorgna A, Coluzzi G et al (2008) Erythropoietin in heart and vessels: focus on transcription and signalling pathways. J Thromb Thrombolysis 26(3):183–187
Riksen NP, Hausenloy DJ, Yellon DM (2008) Erythropoietin: ready for prime-time cardioprotection. Trends Pharmacol Sci 29(5):258–267
Fandrey J (2004) Oxygen-dependent and tissue-specific regulation of erythropoietin gene expression. Am J Physiol Regul Integr Comp Physiol 286(6):R977–R988
Parsa CJ, Matsumoto A, Kim J et al (2003) A novel protective effect of erythropoietin in the infarcted heart. J Clin Invest 112(7):999–1007
Calvillo L, Latini R, Kajstura J et al (2003) Recombinant human erythropoietin protects the myocardium from ischemia-reperfusion injury and promotes beneficial remodeling. PNAS 100(8):4802–4806
Moon C, Krawczyk M, Ahn D et al (2003) Erythropoietin reduces myocardial infarction and left ventricular functional decline after coronary artery ligation in rats. PNAS 100(20):11612–11617
Hale SL, Sesti C, Kloner RA (2005) Administration of erythropoietin fails to improve long-term healing or cardiac function after myocardial infarction in the rat. J Cardiovasc Pharmacol 46(2):211–215
Moon C, Krawczyk M, Ahn D et al (2005) Cardioprotection by recombinant human erythropoietin following acute experimental myocardial infarction: dose response and therapeutic window. Cardiovasc Drug Ther 19(4):243–250
Mancini DM, Katz SD, Lang CC et al (2003) Effect of erythropoietin on exercise capacity in patients with moderate to severe chronic heart failure. Circulation 107(2):294–299
Silverberg DS, Wexler D, Sheps D et al (2001) The effect of correction of mild anemia in severe, resistant congestive heart failure using subcutaneous erythropoietin and intravenous iron: a randomized controlled study. JACC 37(7):1775–1780
Bohlius J, Langensiepen S, Schwarzer G et al (2005) Recombinant human erythropoietin and overall survival in cancer patients: results of a comprehensive meta-analysis. J Natl Cancer Inst 97(7):489–498
Iseki K, Nishime K, Uehara H et al (1996) Increased risk of cardiovascular disease with erythropoietin in chronic dialysis patients. Nephron 72(1):3036
Wakeen M, Zimmerman SW (1998) Association between human recombinant EPO and peripheral vascular disease in diabetic patients receiving peritoneal dialysis. Am J Kidney Dis 32(3):488–493
Besarab A, Bolton WK, Browne JK et al (1998) The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 339(9):584–590
Ehrenreich H, Hasselblatt M, Dembowsky C et al (2002) Erythropoietin for acute stroke is both safe and beneficial. Mol Med 8(8):495–505
Corwin HL, Gettinger A, Fabian TC et al (2007) Efficacy and safety of epoietin alfa in critically ill patients. N Engl J Med 357:965–976
Lipsic E, van der Meer P, Voors AA et al (2006) A single bolus of a long-acting erythropoietin analogue darbepoetin alfa in patients with acute myocardial infarction: a randomized feasibility and safety study. Cardiovasc Drugs Ther 20(2):135–141
Belonje AM, Voors AA, van Gilst WH et al (2008) Effects of erythropoietin after an acute myocardial infarction: rationale and study design of a prospective, randomized, clinical trial (HEBE III). Am Heart J 155(5):817–822
www.ClinicalTrial.gov Identifier: NCT 00378352
Ott I, Schulz S, Mehilli J, et al (2009) Prospective, randomized, double-blind, placebo-controlled trial of erythropoietin in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention (REVIVAL-3). Am Coll Cardiol Scientific Sessions 2009, Orlando, Fla (www.ClinicalTrial.gov Identifier: NCT00390832)
Liem A, van de Woestijne AP, Bruijns E et al (2009) Effect of EPO administration on myocardial infarct size in patients with non-STE acute coronary syndromes; results from a pilot study. Int J Cardiol 131(2):285–287
Andreotti F, Autore C, Conti E et al (2008) Safety and feasibility of erythropoietin administration in patients with acute ST-elevation myocardial infarction. Circulation 118:S876–S877
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andreotti, F., Agati, L., Conti, E. et al. Update on phase II studies of erythropoietin in acute myocardial infarction. Rationale and design of Exogenous erythroPoietin in Acute Myocardial Infarction: New Outlook aNd Dose Association Study (EPAMINONDAS). J Thromb Thrombolysis 28, 489–495 (2009). https://doi.org/10.1007/s11239-009-0363-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-009-0363-x