Abstract
Across four surveys (N = 6.9 million), Americans reported substantially higher levels of depressive symptoms, particularly somatic symptoms, in the 2000s–2010s compared to the 1980s–1990s. High school students in the 2010s (vs. the 1980s) reported more somatic symptoms (e.g., trouble sleeping, thinking, and remembering; shortness of breath) and were twice as likely to have seen a professional for mental issues. College students in recent years (vs. the 1980s) were more likely to report feeling overwhelmed and to believe they were below average in mental and physical health, but were less likely to say they felt depressed. Total Center for Epidemiological Studies Depression scores were higher among adults in 2000 (vs. 1988), especially somatic symptoms. Teens displayed less suicidal ideation in 2011 versus 1991 and were slightly less likely to commit suicide. Thus, more subtle symptoms of depression became more prevalent even as some overt indicators of depression became less prevalent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
American culture has changed substantially over the last few decades, with fundamental shifts in relationships, women’s roles, technology, and medicine. This cultural change has resulted in generational differences in personality traits, attitudes, and behaviors. For example, recent adolescents have more self-focused fears than their 1980s counterparts (Lindfors et al. 2012), are more likely to believe they are above average (Twenge et al. 2012) and have expectations more out of line with reality (Reynolds et al. 2006).
Several authors have speculated that these cultural trends and others might produce a higher incidence of depression and depressive symptoms (e.g., Myers 2000; Seligman 1988b). This paper tests this hypothesis. Determining time period and birth cohort differences in depressive symptoms is important for identifying the scope of mental health issues in current times. Depression is both debilitating (Mathers and Loncar 2006) and prevalent (Baumeister and Harter 2007). In addition, examining cohort differences in depressive symptoms should shed light on the cultural roots of depression. Models from cross-cultural psychology, such as the Mutual Constitution Model, posit that cultures and individuals constantly influence each other (Markus and Kitayama 2010). Cultures are continually changing, and these changes impact individual people.
Several studies have found that the prevalence of depressive symptoms has increased over years and birth cohorts (Lewinsohn et al. 1993; Robins, et al. 1984; Wickramaratne et al. 1989; for a review, see Klerman and Weissman 1989). However, most of these studies were done at one time and asked respondents to recall previous episodes of depression and were thus subject to recall bias (Patten 2003). In a meta-analysis of 26 samples of children and adolescents, Costello et al. (2006) found no evidence for a birth cohort difference in depression in concurrent reports. They concluded that the retrospective method produced the false impression of more depression in recent years. Other studies are cross-sectional (done at one time), such as the American Psychological Association’s 2012 Stress in America survey finding that Millennials (those ages 18–33 in 2012) reported more stress than older birth cohorts did (APA 2013). However, a one-time survey cannot distinguish whether differences are due to age or to birth cohort. It is possible that younger people have always been more stressed than older people, and thus that the difference is an age or developmental effect rather than a cohort or cultural trend.
The ideal design for a study examining time period and birth cohort differences in depressive symptoms is a time-lag design, which examines samples of similar age at different points in time (Schaie 1965). This design holds age constant while year varies; thus, any differences must be due to time period or cohort—and thus to cultural change. (The time-lag method is one of three methods for studying age, cohort, and time period differences. The other two are cross-sectional, a one time study that cannot distinguish between age and cohort, and a longitudinal study, which holds cohort constant while examining changes with age and time period). Several studies using time-lag designs have found that more recent years and birth cohorts experienced higher incidences of depression, hopelessness, and other mental health issues, both in the U.S. (e.g., Compton et al. 2006; Goodwin 2003; Herbst 2011; Lester 2013; Newsom et al. 2003; Swindle et al. 2000; Twenge et al. 2010) and in other Western countries such as Australia, Belgium, and the United Kingdom (Brault et al. 2012; Collishaw et al. 2009; Goldney et al. 2010). In contrast, other time-lag studies found that mental health issues did not differ or were less prevalent over time after the late 1980s to early 1990s (Achenbach et al. 2003; Costello et al. 2006; Twenge and Nolen-Hoeksema 2002).
Thus the previous research literature gives an unclear picture of time period and birth cohort differences in depression and mental health over time in the U.S., particularly after the 1980s. Very few studies have examined differences in depressive symptoms in U.S. samples from the 1990s to the 2010s. One of the few that did (Twenge et al. 2010) used the MMPI, a measure written in the 1930s. Although the MMPI was revised and renormed in 1989, it is not the most modern measure of depression. In addition, most of the MMPI respondents were college students, who might not be representative of the entire population.
If depressive symptoms evince time period or cohort differences, what are the likely mechanisms? In a recent review, Hidaka (2012) argued that the greater recent prevalence of depression is caused by social isolation, lack of exercise and sunlight, and poor diets. Paradoxically, countries with a higher GDP (“rich” countries) have a higher incidence of depression. Lower GDP countries, often those with more collectivistic cultural values, have not experienced greater depression incidence over time (Klerman and Weissman 1989). Other researchers have found that mental health issues are more prevalent when people become more focused on extrinsic values such as money, fame, and image (Kasser and Ryan 1996; Twenge et al. 2010) or speculated that the growth in expectations has led to disappointment and depression (Seligman 1988a; Twenge 2006). This suggests that as cultures become more individualistic and prosperous, depression should increase (Eckersley and Dear 2002). Most evidence suggests that American culture has continued to become more individualistic since the 1990s, both in cultural products such as song lyrics (DeWall et al. 2011) and in the traits of individual people (Twenge and Foster 2010). Based on this research, I hypothesize that depressive symptoms among Americans will be higher in recent decades (2000s–2010s) compared to previous decades (1980s–1990s).
This hypothesis is tested in four large time-lag surveys (N = 6.9 million) examining like-aged samples at different points in time; thus, they hold age constant while time period and birth cohort vary. Three of the four surveys are nationally representative. They provide a view of time period and cohort differences in depressive symptoms among four generations: Silent (born 1925–1945), Boomer (1946–1960), GenX (1961–1981), and Millennials (1982–1999). (Note that a generation refers to those born in a somewhat arbitrarily defined period, and birth cohort to those born in a specific year; I will use the two terms fairly interchangeably as both refer to time of birth).
Few studies collect data over time, so the ideal data are not always available. The ideal study would have administered a standard measure of depressive symptoms such as the Center for Epidemiological Studies Depression (CES-D) scale and other measures of anxiety, suicidal ideation, and mental health issues to a nationally representative sample with the same average age over several decades. To my knowledge, such a study does not exist. Thus I draw from four surveys that include at least one characteristic of the ideal study and include different measures of depressive symptoms.
Study 1 analyzes differences in somatic symptoms of depression in a nationally representative sample of American 12th graders between 1982 and 2012. Study 2 examines differences in responses to mental health items among a nationally representative sample of entering college students between 1985 and 2013. Study 3 examines adults in the Longitudinal Study of Generations, one of the few time-lag surveys to include the CES-D, in 1988 and 2000. Finally, Study 4 analyzes trends in suicidal ideation among a nationally representative sample of high school students (9th–12th graders) between 1991 and 2011 and trends in completed suicides over the same time.
2 Study 1: Psychosomatic Symptoms Among 12th Graders 1982–2012
The Monitoring the Future (MtF) survey has collected a nationally representative sample of U.S. 12th graders every year since 1976. As respondents are the same age, the survey uses the time-lag design useful for identifying time period and cohort differences separated from age differences. MtF does not include the CES-D or any other standard measure of anxiety or depressive symptoms. However, since 1982, MtF has included items about physical and psychosomatic symptoms that overlap considerably with the somatic symptoms assessed in the CES-D and other depression scales (see Table 1). Studying somatic symptoms is especially important as they are independent predictors of outcomes of major depression (Hung et al. 2010) and are closely associated with depression as both causes and consequences of the disorder (Lopresti et al. 2013).
MtF also includes items assessing physical illness, allowing a view of whether all symptom reporting has increased. In addition, it asks participants if they have sought treatment for physical or mental health issues, allowing an assessment of treatment-seeking. I also examined whether sex, race, or socioeconomic status (SES) moderated the effects.
2.1 Method
MtF samples high schools across the United States chosen to represent a cross-section of the U.S. population on variables such as region, race, gender, and socioeconomic status (see http://www.monitoringthefuture.org). The survey uses a multi-stage random sampling procedure to select high schools and then students to complete the survey. The participation rate of schools is between 66 and 80 %, and the student participation rate is between 79 and 83 % (Johnston et al. 2013). About 15,000 high school seniors are sampled each year in the spring. The sample is divided into subsamples of about 2,500 people, and each subsample is asked a different set of questions, called a “Form.” The current project used items from Form 1 beginning in 1982 when the health items were first introduced. I analyzed all of the MtF datasets available online at the time analysis began; this included data files for all years 1982–2012 (N = 70,838). As the survey administrators recommend, all analyses were weighted by the sampling weight to make them nationally representative.
The relevant section of Form 1 begins, “These next questions concern your health. During the LAST 30 DAYS, on how many days (if any) did you have the following problems or symptoms?” with the following items: “Headache,” “Sore throat or hoarse voice,” “Trouble with sinus congestion, runny nose, or sneezing,” “Coughing spells,” “Chest colds,” “Coughing up phlegm or blood,” “Shortness of breath when you were not exercising,” “Wheezing or gasping,” “Trouble remembering things,” “Difficulty thinking or concentrating,” “Trouble learning new things,” “Trouble sleeping,” “Trouble getting started in the morning,” “Stayed home most or all of a day because you were not feeling well.” For each item, response choices were 1 = None, 2 = 1 day, 3 = 2 days, 4 = 3–5 days, 5 = 6–9 days, 6 = 10–19 days, 7 = 20+ days.
Factor analysis yielded three factors with Eigenvalues greater than 1: mental issues (alpha = .77), breathing issues (alpha = .72), and physical ailments (alpha = .79). Table 2 shows which items were included on which subscales. The mental issues subscale items are very similar to those assessing somatic symptoms on the CES-D.
The next section begins, “In the LAST 12 MONTHS, how many times (if any) have you seen a doctor or other professional for each of the following?” with the following items: “For a routine physical check-up,” “For an injury suffered in a fight, assault, or auto accident,” “For any other accidental injury,” “For some physical illness or symptom.” Response choices were 1 = None, 2 = Once, 3 = Twice, 4 = 3–5 times, 5 = 6–9 times, 6 = 10+ times.
A final item asks, “Overall, relative to other people your age, do you think your physical health over the past year has been …” with response choices of 1 = Much poorer than average, 2 = Somewhat poorer than average, 3 = About average, 4 = Somewhat better than average, 5 = Much better than average.
2.2 Results and Discussion
High school students in the 2010s reported more somatic symptoms of depression than those in the 1980s, including trouble remembering things, difficulty thinking or concentrating, and trouble sleeping. They also reported more breathing issues and were more likely to report that they felt their physical health was below average. However, they did not report significantly more physical ailments such as colds or coughing spells (see Table 1), suggesting that the differences are not caused by greater reporting of symptoms in general.
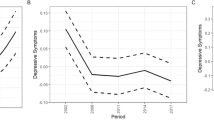
For some symptoms, reports in the 2010s are slightly less than in the late 2000s (see Table 1; Fig. 1). Thus Table 1 reports the d comparing the earliest years (1982–1984) to both the most recent years (2010–2012) and the second most recent years (2005–2009).
The modest though significant shifts at the mean mask larger changes in the percentage of teens experiencing somatic symptoms. For example, 36 % of students in 2010–2012 reported having trouble remembering at least once in the previous month, up from 26 % in 1982–1984, a 38 % increase. In 2010–2012, 23 % of students reported shortness of breath, compared to 14 % in 1982–1984, a 64 % increase. 23 % reported having trouble sleeping six or more days a month in 2010–2012, up from 13 % in 1982–1984, a 73 % increase. More than twice as many 2010–2012 teens (8 %) reported having trouble sleeping on 20 or more days a month compared to 1982–1984 (3 %). Similarly, more than twice as many 2010–2012 teens (5 %) as those in 1982–1984 (2 %) reported having trouble thinking clearly on 20 or more days a month.
Recent high school students were more likely to have undergone a routine physical check-up (52 % in 1982–1984 compared to 62 % in 2010–2012, a 19 % increase). Recent students were also twice as likely to have seen a doctor or other professional for emotional or psychological issues (4.3 % did so in 1982–1984, compared to 9.3 % in 2010–2012). However, recent students were no more likely to have seen a doctor or other professional for a physical injury or symptom.
Thus, compared to GenX’ers (born 1961–1981) in the 1980s and 1990s, Millennials (born 1982–1999) were more likely to experience somatic symptoms of depression and were more likely to seek treatment for emotional or psychological issues. This trend has leveled off in recent years; oddly, somatic symptoms decreased during the recession years 2008–2012. However, somatic symptoms in 2010–2012 were still significantly higher than in the early 1980s.
I also examined if sex, race, or socioeconomic status (SES) moderated the effects. The cohort difference in mental issues was more pronounced among girls (comparing 1982–1984 to 2010–2012, d = .21) than among boys (d = .09). Thus the tendency of more recent generations to report more mental issues was largely driven by girls. Sex did not moderate cohort differences in the other variables. Race and SES (measured by father’s education) did not significantly moderate the effects. Sex, race and SES also had significant main effects, with female, white, and high SES individuals more likely to report mental issues and seek professional help for them.
3 Study 2: Mental Health Issues Among Entering College Students, 1985–2013
The American Freshman survey has collected a nationally representative sample of incoming college students every year since 1966 (N = 6.7 million). Since 1985, it has asked three questions relevant to mental health, including whether respondents felt overwhelmed or depressed and whether they believe their physical or emotional health to be below average compared to their peers.
3.1 Method
The American Freshman project, part of the Cooperative Institutional Research Program (CIRP) administered by the Higher Education Research Institute (HERI), has surveyed a nationwide sample of about 200,000 first-year students at U.S. 4-year colleges or universities in the fall every year since 1966 (Pryor et al. 2007). Originally, some 2-year colleges participated, but the data—including that for past years—are now reported only for students at 4-year colleges or universities (N = 6.7 million from 1,201 college campuses). Most respondents are 18 years old. Data for campuses are included only if more than 75 % of first-time full-time freshman students participated. The survey weights its results to be demographically representative of all first-year students at 4-year colleges and universities in the U.S. The weighting is done in a two-step procedure: first to correct for nonparticipation within campuses, and second to ensure that the campuses included are representative of 4-year colleges and universities in the U.S. I obtained the aggregated data from HERI’s publicly available research reports (e.g., Pryor et al. 2007). The available data are broken down by sex but not by other demographic variables.
The AF survey asked four questions relevant for depression in two sections of the questionnaire. One section begins “For the activities below, indicate which ones you did during the past year. If you engaged in the activity frequently, mark F. If you engaged in the activity one or more times, but not frequently, mark O (Occasionally). Mark N (Not at all) if you have not performed the activity during the past year. Mark one for each item.” Two items in this section were “Felt overwhelmed by all I have to do” and “Felt depressed.” Another section began: “Rate yourself on each of the following traits as compared with the average person your age. We want the most accurate estimate of how you see yourself.” Two items on this list were “emotional health” and “physical health.” Response choices were “highest 10 %,” “above average,” “average,” “below average,” and “lowest 10 %.”
3.2 Results and Discussion
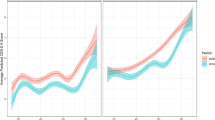
Entering U.S. college students in the 2010s (vs. the 1980s) were more likely to feel overwhelmed and to say they believed their emotional health and physical health was below average (see Table 2). For example, 50 % more students reported feeling overwhelmed between 1985–1989 and 2010–2013, and 24 % more felt below average in emotional health. These decreases in rating emotional health below average occurred despite an increase in rating oneself above average on most other traits (Twenge et al. 2012). However, 22 % fewer entering college students said they felt depressed. Unlike the results for the high school students, college students’ mental health issues continued to increase during the recession years.
The difference in feeling overwhelmed was primarily driven by women (d = .31 for 1985–1989 vs. 2010–2013, compared to d = .11 for 1985–1989 vs. 2010–2013 for men). The difference in feeling below average in emotional health was also driven more by women (d = .20 vs. d = .15 for men). Effect sizes for the time difference for physical health and depression were similar for women and men. There was also a main effect for sex on all variables, with college women reporting more mental health issues than college men. For example, 44 % of 2013 women said they felt overwhelmed, versus 20 % of men.
4 Study 3: The CES-D in the Longitudinal Study of Generations
Although MtF and AF are nationally representative, they do not include a standard measure of depressive symptoms such as the CES-D. In addition, both MtF and AF include only young respondents (12th graders and entering college students); thus, it is unclear if the rise in some depressive symptoms also appears among adults. One of the few time-lag surveys of adults to include the CES-D is the Longitudinal Study of Generations, which included the CES-D with consistent response choices between 1988 and 2000. The first wave included young adults and their parents and grandparents; later waves followed the initial sample and added the children of the original young adults, which kept the mean age of the sample relatively constant over time, allowing time-lag analysis. Because the respondents were from the same families, this dataset also rules out alternative explanations for time period differences such as shifts in ethnic, cultural, or class composition in the U.S. population over time.
4.1 Method
In 1971, researchers contacted the members of a health maintenance organization, Kaiser Permanente, in Southern California, surveying three generations in the same families (grandparents, parents, and teen to young adult children). In later waves, a fourth generation—the children of the original young adults—were included as they reached adolescence. The sample was 95 % white and the participants were primarily working to middle class. In later waves, more than half of the sample had moved from Southern California to other parts of the state, the U.S., or even abroad (Bengtson et al. 2002). The LSG datafile covering the years 1971–2000 is available online.
All 20 CES-D items were included beginning in 1985, but the response labels were changed beginning in 1988. Since 1988, the response labels were “1 = Rarely or none of the time,” “2 = Some of the time,” “3 = A moderate amount of the time,” and “4 = Most or all of the time.” Thus I compared the responses from 1988 to those from 2000.
A principal components factor analysis with varimax rotation of the CES-D items in this sample yielded four factors with Eigenvalues greater than 1: Negative affect (7 items; alpha = .86), somatic symptoms (7 items; alpha = .76), positive affect (4 items; alpha = .77), and relations with others (2 items; alpha = .65). Negative affect items included “I felt that I could not shake the blues even with help from my family or friends;” “I felt depressed;” “I thought my life had been a failure;” “I felt fearful;” “I felt lonely;” “I had crying spells;” and “I felt sad.” Somatic symptoms items included “I did not feel like eating; my appetite was poor;” “I was bothered by things that don’t usually bother me,” “I had trouble keeping my mine on what I was doing;” “I felt that everything I did was an effort;” “My sleep was restless;” “I talked less than usual;” and “I could not ‘get going.’” Positive affect items included “I felt that I was just as good as other people;” “I felt hopeful about the future;” “I was happy;” and “I enjoyed life.” Relations with others items included “People were unfriendly;” and “I felt that people disliked me.” These subscales have also been found in previous research (e.g., Gatz and Hurwicz 1990; Shafer 2006). The LSG survey also included the Bradburn affect scale, which asks respondents to say “yes” or “no” to whether they felt certain ways during the past few weeks. One of the items is “depressed or very unhappy.”
In total, 1,425 respondents completed at least one of the CES-D items in 1988, and 1,781 in 2000 (the tables show the total number who responded to all items in the subscales). All 1988 participants were 19 years of age or older, so we excluded the 6.5 % of participants in 2000 who were 18 or under. The mean age of the samples was similar in 1988 (M = 50.13, SD = 16.12) and 2000 (M = 47.92, SD = 19.01). To insure that changes over time were not due to aging, we also examined differences among respondents in their 30 s (the age group with the largest n) in 1988 versus those in their 30 s in 2000. Since 12 years passed between these two assessments, these are two different groups of people and thus different in birth cohort as well as time period.
4.2 Results and Discussion
Adult respondents in 2000 reported more depressive symptoms on the CES-D than respondents in 1988. Somatic symptoms, including having a poor appetite, having difficulty concentrating, and feeling that everything was an effort, increased the most. The trends were similar among respondents in their 30 s (see Table 3). Effect sizes were small to moderate; however, given that the time period was only 12 years, they are in the same range as many other studies finding increases in mental health issues over time (between d = .01 and .02 a year; Twenge 2000; Twenge and Foster 2010). These changes at the mean also led to larger changes at the top and bottom of the distribution. In 1988, 18 % of respondents scored a 16 or above (a common cutoff for depression) on the CES-D; in 2000, 25 % did, a 39 % increase. Individual items showed similar trends; for example, 42 % agreed that “I felt everything I did was an effort” at least a little of the time in 1988, which jumped to 55 % in 2000, a 31 % increase.
However, respondents in 2000 were no more likely than those in 1988 to describe themselves as depressed when asked directly. There was also no change in the single CES-D item “I felt depressed” (d = .01 among all respondents age 19 and over; d = .03 among respondents in their 30 s). This replicates Study 2, which found no differences in the percentage of college students saying they were depressed. Overall, this study replicates the time period and cohort differences found in Study 1 and Study 2 in a sample of adults, with increases in psychosomatic symptoms but little change in overt admissions of depression.
5 Study 4: Suicidal Ideation Among High School Students, 1991–2011
Thus far, we have examined depressive symptoms using the CES-D, somatic symptoms, treatment-seeking, and items about feeling overwhelmed and below average in emotional health. These surveys did not include questions about suicidal ideation or suicide rate, two of the most troubling outcomes of depression (Hawton et al. 2013). The Youth Risk Behavior Surveillance System administered by the U.S. Centers for Disease Control and Prevention (CDC) surveyed a nationally representative sample of U.S. 9th through 12th graders every other year, 1991–2011. It included four questions about suicidal ideation and action (considering suicide, making a plan to commit suicide, attempting to commit suicide, and being medically treated after a suicide attempt). Sex and race can also be examined as moderators. The rate of completed suicide is also available from U.S. Census records.
5.1 Method
The Youth Risk Behavior Surveillance System surveyed a nationally representative sample of 9th through 12 graders every other year between 1991 and 2011 (N = 159,691). The aggregated data are available on the CDC website. The relevant section begins “The next five questions ask about sad feelings and attempted suicide. Sometimes people feel so depressed about the future that they may consider attempting suicide, that is, taking some action to end their own life.” Questions included, “During the past 12 months, did you ever feel so sad and hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities?” (asked in 1999 and later years) “During the past 12 months, did you ever seriously consider attempting suicide?” “During the past 12 months, did you make a plan about how you would attempt suicide?” Response choices were “A. Yes B. No.” The last question was “If you attempted suicide during the past 12 months, did any attempt result in an injury, poisoning, or overdose that had to be treated by a doctor or nurse?” Response choices were “A. I did not attempt suicide during the past 12 months. B. Yes C. No.” The survey also breaks down data by respondent sex and race and ethnicity (with white, Black, and Hispanic the only groups large enough to have enough data in across all years). We also gathered the actual suicide rate for the comparable age group (ages 15–24) from the Statistical Abstract of the United States (U.S. Census 2012).
5.2 Results and Discussion
Between 1991 and 2011, U.S. teens were increasingly less likely to say they considered suicide or made a plan to commit suicide. For example, the number who considered suicide decreased 40 % from 1991–1994 to 2011, and the number who made a plan to commit suicide decreased 32 %. There was no significant change in the number of teens who attempted to commit suicide or were medically treated for such an attempt or in those who said they felt sad or hopeless for two weeks or more (see Table 4).
Sex of respondent moderated several of these effects. Most notably, the number of boys who reported attempting suicide was higher in 2011 than in 1991 (d = .09), whereas slightly fewer girls reported a suicide attempt in 2011 than in 1991 (d = −.03). The time period/cohort difference in considering a suicide attempt and making a suicide plan was larger among girls than among boys (considering an attempt: boys d = −.22, girls d = −.40; making a plan: boys d = −.05, girls d = −.25).
Race and ethnicity were also moderators. The time period/cohort difference for considering suicide was larger among White teens (d = −.35) than among Black (d = −.24) and Hispanic teens (d = −.25). The difference by year in making a suicide plan was also larger among White teens (d = −.19) than among Black (d = −.11) or Hispanic teens (d = −.04). And although about the same number of White teens in 2011 (vs. 1991) reported attempting suicide (d = −.02), slightly more Black (d = .06) and Hispanic teens (d = .08) reported a suicide attempt in 2011 compared to 1991. Thus, the lower prevalence of suicidal ideation in recent years was primarily driven by White girls and was not present or even reversed among other populations on some items.
Americans aged 15–24 were also less likely to actually commit suicide over this time period, although the decline was small in terms of effect size (see Table 4). Suicidal ideation and completed suicides were slightly higher during the recession years, in contrast to the lower somatic symptoms during the recession years found in MtF.
6 General Discussion
Across four large surveys, Americans in the 2000s–2010s (vs. the 1980s–1990s) were more likely to report depressive symptoms, especially psychosomatic symptoms, but were less likely to overtly admit to depression or report suicidal ideation. This pattern of findings replicated across three age groups (adolescents, young adults, and adults), two sampling methods (nationally representative and members of the same families), and several methods of measurement (individual items, symptom reports, suicidal behavior, and the CES-D). This pattern of findings was most pronounced among girls and women. Study 1 also found that twice as many high school students now seek treatment for mental and emotional issues. As Hidaka (2012), theorized, something in modern life is undermining mental health. Fortunately, the increased prevalence of mental health issues has not extended to more severe outcomes such as suicide, perhaps due to the increased use of therapy and anti-depressant medications (Pratt et al. 2011).
The results may help explain why some studies (such as Twenge et al. 2010 of the MMPI) have shown greater prevalence of mental health issues in the 2000s compared to the 1980s while others (Costello et al. 2006) have not. The MMPI scales focus on somatic symptoms, and the current studies find that most of the cohort difference in depressive symptoms is due to somatic symptoms rather than negative affect or direct reports of depression. Somatic symptoms are potentially more worrisome than negative affect alone, as some studies have found that they are more predictive of mortality than cognitive or affective symptoms (Roest et al. 2011). Apparently, the pressures, lifestyles, and social forces of modern life have led people to experience more psychosomatic issues such as sleeping issues and difficulty concentrating. However, they have not led to greater overt reports of depression, nor to greater suicidal ideation.
The results suggest that the younger generation may be more in need of mental health treatment. Although no more of these patients may describe themselves as depressed than during previous years, more may manifest somatic symptoms of depression or describe feeling overwhelmed. Despite the increased awareness of mental health issues, depressive symptoms may still present themselves as psychosomatic symptoms such as difficulty focusing, sleeping, and eating or as feeling “stressed” or overwhelmed.
The introduction of selective serotonin reuptake inhibitor medications (SSRIs) in the late 1980s to early 1990s may have had a suppressor effect on changes in depressive symptoms in the U.S. With more people taking SSRIs (Pratt et al. 2011)—especially those with high levels of depressive symptoms—mean levels of depressive symptoms should decrease. The increase in the number of high school students seeking psychological therapy during this time may also have suppressed any increase in depressive symptoms or suicidal ideation that might otherwise be caused by cultural factors. Thus it is possible that the higher recent prevalence of depressive symptoms might have been even higher if SSRIs and other professional help for mental health issues were not in greater use. It is also possible that the greater use of SSRIs may be the reason for the lower prevalence of suicide and suicidal ideation among teens. SSRIs became prominent during the 1990s, just as the suicide rate declined, so may have prevented some suicides and suicidal ideation. However, it cannot be determined if one caused the other.
Analyses of moderators suggest that both the greater recent prevalence of depressive and anxious symptoms and the lesser recent prevalence of suicidal ideation are most pronounced in female samples. The lesser prevalence of suicidal ideation is most pronounced among Whites. This suggests that interventions and medications aimed to decrease suicidal ideation have been most effective among White girls, but that this same population has become even more likely to suffer from psychosomatic symptoms and feelings of being overwhelmed. The smaller cohort decline (or even small increase) in suicidal ideation among Black and Hispanic teens suggests that these populations may still lack access to sufficient mental health resources and treatment.
6.1 Limitations
Data collected over time is rare, and a nationally representative, time-lag survey administering a standard measure of depressive symptoms to same-aged respondents since the 1980s has, to my knowledge, not been conducted. Taken together, these studies each fills part of the picture, but none are ideal. The high school sample in Study 1 is nationally representative, but does not include other age groups or a standard measure of depressive symptoms. The college sample in Study 2, although nationally representative of entering college students, excludes those in the cohort who are not attending a 4-year college. In addition, this survey relies on one-item measures, which may compromise reliability. Study 3 of adults used the reliable, valid, multi-item CES-D, but was not nationally representative and may be confounded by other variables if the respondents in 2000 were different in some systematic way from the respondents in 1988. The sample in Study 4 is nationally representative, but again relied on one-item measures.
One strength of these studies is that they hold age constant as time varies, so any differences cannot be due to age or development. However, like any time-lag study holding age constant, these studies cannot separate the effects of birth cohort and time period. We cannot tell if Americans of all ages experienced more depressive symptoms over time, or if each successive birth cohort experienced more symptoms. Both explanations indicate that cultural change has occurred, but a birth cohort difference would suggest a more stable and perhaps more permanent trend.
As with any correlational study, it is difficult to prove what caused these trends. For example, it is possible that the increase in self-reported depressive symptoms is due to the decreased stigmatization of depression and mental health issues in general. However, the data argue against this explanation. Outright admissions of depression (such as the single items in Studies 2, 3, and 4) are similar across the decades or less prevalent in recent years, whereas more subtle indicators of depression such as psychosomatic symptoms are more prevalent in recent years. In addition, two studies have found that socially desirable and defensive responding did not differ between the 1980s and the 2000s (Twenge and Im 2007; Twenge et al. 2010). The latter study found that the greater recent prevalence of mental health issues on the MMPI remained after scores on the L and K scales were controlled.
Decreased stigmatization is, however, a possible explanation for the twofold increase in high school students seeing mental health professionals. On the other hand, a recent study found that college students’ willingness to seek help for mental health issues was lower in 2008 than in 1968 (Mackenzie et al. 2014). This suggests that more young people are seeking help because they are experiencing symptoms, not because they are more positive toward mental health treatment.
It is possible that the direct questions about feeling depressed show no differences due to shifting interpretations of the word “depressed,” which may have once meant sad, but may have acquired a more precise definition during the 1990s. A search of the American English corpus of the Google Books database (which includes the full text of 5 million books) shows an increase in the use of the word “depressed” beginning in the 1970s, peaking in the late 1980s and early 1990s, and remaining at historically high levels in the 2000s. This suggests more discussion of depression in the culture during this time period, perhaps resulting in differences in how the word is interpreted. However, word interpretation is unlikely to explain the differences in reports of somatic symptoms, as they occurred across several domains and do not include the word “depressed.”
As with most studies, our conclusions are limited by the samples involved. These studies examined U.S. populations and cannot be generalized to other countries. Three of the studies included nationally representative samples, suggesting that the results should generalize to the U.S. population of those ages. Our conclusions for teens and early young adults are more certain than those for adults, as only one study sampled adults and it was not nationally representative.
6.2 Conclusions
American teens and adults are manifesting more somatic symptoms of depression even as suicidal ideation and overt admissions of depression have stayed constant or declined. Overall, the rate of depressive symptoms among Americans remains unacceptably high.
References
Achenbach, T. M., Dumenci, L., & Rescorla, L. A. (2003). Are American children’s problems still getting worse? Journal of Abnormal Child Psychology, 31, 1–11.
American Psychological Association. (2013). Stress in America: Missing the health care connection. http://www.apa.org/news/press/releases/stress/2012/full-report.pdf.
Baumeister, H., & Harter, M. (2007). Prevalence of mental disorders based on general population surveys. Social Psychiatry and Psychiatric Epidemiology, 42, 537–546.
Bengtson, V. L., Biblarz, T. J., & Roberts, R. E. L. (2002). How families still matter: A longitudinal study of youth in two generations. Cambridge: Cambridge University Press.
Brault, M.-C., Meuleman, B., & Bracke, P. (2012). Depressive symptoms in the Belgian population: Disentangling age and cohort effects. Social Psychiatry and Psychiatric Epidemiology, 47, 903–915.
Collishaw, S., Maughan, B., Natarajan, L., & Pickles, A. (2009). Trends in adolescent emotional problems in England: A comparison of two national cohorts twenty years apart. Journal of Child Psychology and Psychiatry, 51, 885–894.
Compton, W. M., Conway, K. P., Stinson, F. S., & Grant, B. F. (2006). Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. American Journal of Psychiatry, 163, 2141–2147.
Costello, J., Erkanli, A., & Angold, A. (2006). Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry, 47, 1263–1271.
DeWall, C. N., Pond, R. S., Campbell, W. K., & Twenge, J. M. (2011). Tuning in to psychological change: Linguistic markers of psychological traits and emotions over time in popular U.S. song lyrics. Psychology of Aesthetics, Creativity, and the Arts, 5, 200–207.
Eckersley, R., & Dear, K. (2002). Cultural correlates of youth suicide. Social Science and Medicine, 55, 1891–1904.
Gatz, M., & Hurwicz, M.-L. (1990). Are old people more depressed? Cross-sectional data on Center for Epidemiological Studies Depression Scale factors. Psychology and Aging, 5, 284–290.
Goldney, R. D., Eckert, K. A., Hawthorne, G., & Taylor, A. W. (2010). Changes in the prevalence of major depression in an Australian community sample between 1998 and 2008. Australian and New Zealand Journal of Psychiatry, 44, 901–910.
Goodwin, R. D. (2003). The prevalence of panic attacks in the United States: 1980 to 1995. Journal of Clinical Epidemiology, 56, 914–916.
Hawton, K., Cornabella, C. C., Haw, C., & Saunders, K. (2013). Risk factors for suicide in individuals with depression: A systematic review. Journal of Affective Disorders, 147, 17–28.
Herbst, C. M. (2011). ‘Paradoxical’ decline? Another look at the relative reduction in female happiness. Journal of Economic Psychology, 32, 773–788.
Hidaka, B. H. (2012). Depression as a disease of modernity: Explanations for increasing prevalence. Journal of Affective Disorders, 140, 205–214.
Hung, C.-I., Liu, C.-Y., Wang, S.-J., & Juang, Y–. Y. (2010). Somatic symptoms: An important index in predicting the outcome of depression at six-month and two-year follow-up points among outpatients with major depressive disorder. Journal of Affective Disorders, 125, 134–140.
Johnston, L. D., Bachman, J. G., O’Malley, P. M., & Schulenberg, J. E. (2013). Monitoring the future: A continuing study of American youth (12th-grade survey), 1976–2010; (8th- and 10th-grade survey), 1991–2010 [Computer files and codebook]. ICPSR25382-v2. Ann Arbor, MI: Inter-university Consortium for Political and Social Research.
Kasser, T., & Ryan, R. M. (1996). Further examining the American dream: Differential correlates of intrinsic and extrinsic goals. Personality and Social Psychology Bulletin, 22, 280–287.
Klerman, G. L., & Weissman, M. M. (1989). Increasing rates of depression. Journal of the American Medical Association, 261, 2229–2235.
Lester, D. (2013). Hopelessness in undergraduate students around the world: A review. Journal of Affective Disorders, 150, 1204–1208.
Lewinsohn, P. M., Rohde, P., Seeley, J. R., & Fischer, S. A. (1993). Age-cohort changes in lifetime occurrence of depression and other mental disorders. Journal of Abnormal Psychology, 102, 110–120.
Lindfors, P., Solantaus, T., & Rimpela, A. (2012). Fears for the future among Finnish adolescents in 1983–2007: From global concerns to ill health and loneliness. Journal of Adolescence, 35, 991–999.
Lopresti, A. L., Hood, S. D., & Drummond, P. D. (2013). A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep, and exercise. Journal of Affective Disorders, 148, 12–27.
Mackenzie, C. S., Erickson, J., Deane, F., & Wright, M. (2014). Changes in attitudes toward seeking mental health services: A 40-year cross-temporal meta-analysis. Clinical Psychology Review, 34, 99–106.
Markus, H. R., & Kitayama, S. (2010). Cultures and selves: A cycle of mutual constitution. Perspectives on Psychological Science, 5, 420–430.
Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine, 3, 2011–2030.
Myers, D. G. (2000). The American paradox: Spiritual hunger in an age of plenty. New Haven, CT: Yale University Press.
Newsom, C. R., Archer, R. P., Trumbetta, S., & Gottesman, I. I. (2003). Changes in adolescent response patterns on the MMPI/MMPI-A across four decades. Journal of Personality Assessment, 81, 74–84.
Patten, S. B. (2003). Recall bias and major depression lifetime prevalence. Social Psychiatry and Epidemiology, 38, 290–296.
Pratt, L. A., Brody, D. J., & Gu, Q. (2011). Antidepressant use in persons aged 12 and over: United States, 2005–2008. National Center for Health Statistics Data Brief 76.
Pryor, J. H., Hurtado, S., Saenz, V. B., Santos, J. L., & Korn, W. S. (2007). The American freshman: Forty-year trends, 1966–2006. Los Angeles: Higher Education Research Institute.
Reynolds, J., Stewart, M., MacDonald, R., & Sischo, L. (2006). Have adolescents become too ambitious? High school seniors’ educational and occupational plans, 1976 to 2000. Social Problems, 53, 186–206.
Robins, L. N., Helzer, J. E., Weissman, M. M., Orvaschel, H., Gruenbreg, E., Burke, J. D., et al. (1984). Lifetime prevalence of specific psychiatric disorders in three sites. Archives of General Psychiatry, 41, 949–958.
Roest, A. M., Thombs, B. D., Grace, S. L., Stewart, D. E., Abbey, S. E., & de Jonge, P. (2011). Somatic/affective symptoms, but not cognitive/affective symptoms, of depression after acute cardiac syndrome are associated with 12-month all-cause mortality. Journal of Affective Disorders, 131, 158–163.
Schaie, K. W. (1965). A general model for the study of developmental problems. Psychological Bulletin, 64, 92–107.
Seligman, M. E. P. (1988a). Boomer blues. Psychology Today, 22, 50–53.
Seligman, M. E. P. (1988b). Why is there so much depression today? The waxing of the individual and the waning of the commons. In. R. E. Ingram (Ed.), Contemporary psychological approaches to depression (pp. 1–9). New York, NY: Plenum.
Shafer, A. B. (2006). Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. Journal of Clinical Psychology, 62, 123–146.
Swindle, R., Heller, K., Pescosolido, B., & Kikuzawa, S. (2000). Responses to nervous breakdowns in America over a 40-year period. American Psychologist, 55, 740–749.
Twenge, J. M. (2000). The age of anxiety? Birth cohort change in anxiety and neuroticism, 1952-1993. Journal of Personality and Social Psychology, 79, 1007–1021.
Twenge, J. M. (2006). Generation me: Why today’s young Americans are more confident, assertive, entitled–and more miserable than ever before. New York: Free Press.
Twenge, J. M., & Foster, J. D. (2010). Birth cohort increases in narcissistic personality traits among American college students, 1982–2009. Social Psychological and Personality Science, 1, 99–106.
Twenge, J. M., & Im, C. (2007). Changes in the need for social approval, 1958–2001. Journal of Research in Personality, 41, 171–189.
Twenge, J. M., & Nolen-Hoeksema, S. (2002). Age, gender, race, socioeconomic status, and birth cohort differences on the Children’s Depression Inventory: A meta-analysis. Journal of Abnormal Psychology, 111, 578–588.
Twenge, J. M., Campbell, W. K., & Gentile, B. (2012). Generational increases in agentic self-evaluations among American college students, 1966–2009. Self and Identity, 11, 409–427.
Twenge, J. M., Gentile, B., DeWall, C. N., Ma, D. S., Lacefield, K., & Schurtz, D. R. (2010). Birth cohort increases in psychopathology among young Americans, 1938–2007: A cross-temporal meta-analysis of the MMPI. Clinical Psychology Review, 30, 145–154.
U.S. Census. (2012). Statistical abstract of the United States. Washington, DC: U.S. Government Printing Office.
Wickramaratne, P. J., Weissman, M. M., Leaf, P. J., & Holford, T. R. (1989). Age, period, and cohort effects on the risk of major depression: Results from five United States communities. Journal of Clinical Epidemiology, 42, 333–343.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Twenge, J.M. Time Period and Birth Cohort Differences in Depressive Symptoms in the U.S., 1982–2013. Soc Indic Res 121, 437–454 (2015). https://doi.org/10.1007/s11205-014-0647-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-014-0647-1