Abstract
The Study on global AGEing and adult health (SAGE) aims at improving empirical understanding of the health and well-being of older adults in low- and middle-income countries. A total of 321 adults aged 50 years and older were interviewed in rural Pune district, India, in 2007. We used Structural Equation Modelling (SEM) to examine the pathways through which social factors, functional disability, risk behaviours, and chronic disease experience influence self-rated health (SRH) and quality of life (QOL) amongst older adults in India. Both SRH and QOL worsened with increased age (indirect effect) and limitations in functional ability (direct effect). QOL, socio-economic status (SES), and social networking had no significant effect on SRH. Smoking was associated with the presence of at least one chronic illness, but this did not have a statistically significant effect on SRH. Higher social networking was seen amongst the better educated and those with regular income, which in turn positively affected the QOL rating. QOL had a direct, but statistically not significant, effect on SRH. In conclusion, the indirect effects of age on SRH mediated through functional ability, and the effects of SES on QOL mediated through social networking, provide new understanding of how age and socio-economic status affect SRH and QOL. By allowing for measurement errors, solving for collinearity in predictor variables by integrating them into measurement models, and specifying causal dependencies between the underlying latent constructs, SEM provides a strong link between theory and empirics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Self-rated health (SRH) and quality of life (QOL) are complex latent constructs commonly used to assess health and well-being (Fayers and Sprangers 2002; Garrity et al. 1978; Robine and Jagger 2003; World Health Organization 1996). SRH is a widely used measure to predict health outcomes (Salomon et al. 2009). It is an useful, reliable, and all-inclusive measure that substitutes for other more specific measures of health and disability in predicting health outcomes (Lundberg and Manderbacka 1996). It is based on the individual’s evaluation of his health status using a single global health question: In general, how would you rate your health today? SRH is influenced not only by perception, experience of disease, and ability to function but also by health expectations, which in turn are influenced by a person’s psycho-social and cultural contexts (Salomon et al. 2003). Though the exact wording and response options have varied with different surveys, which makes it difficult to directly compare distributions and levels of measurement, SRH assesses the same phenomenon across different settings (Jurges et al. 2008). One theory suggests that when a person is asked to self-rate his health, he reflects upon the different components of health, including the ability to function, body feelings of pain and sensation, signs of disease, diagnosed health problems, and preventive and risk behaviours in the context of his age, sex, previous health experience, health experience of his peers, and his own health expectations. He then summarizes this information in his own meaningful way into a single rating on a scale of “very good” to “very bad” based on his emotions experienced at the time of self-rating and the cultural norms of reporting health status in his surroundings (Jylha 2009).
Quality of life is a construct that goes beyond just wealth and health. It is linked with social well-being, social belonging, employment, recreation, and leisure (Gregory et al. 2009). The relationships between QOL and SRH and the extent to which individuals distinguish quality of life from health is unclear, but it seems likely that overall health relates principally to physical health and that QOL is related more to mental health (Fayers and Sprangers 2002).
Self-rated health is known to decline as age advances, and women are more likely than men to report poor SRH (Asfar et al. 2007; Hirve et al. 2010; Ishizaki et al. 2009). The association of aging with poor SRH is possibly mediated through decreasing functional disability and pre-existing illness (Lee and Shinkai 2005; Tay et al. 2005). Limitations in functional ability, sleep, activities of daily living, mobility, and cognition are strongly associated with poor SRH (Machado et al. 2006; Benyamini et al. 2000; Mora et al. 2008). Physical functioning has a stronger association with SRH than mental or social functioning Furthermore, the association between mental or social functioning and SRH differs among individuals with depression and cognitive impairment (Mavaddat et al. 2011).
The socio-economic environment shapes perceptions of health and QOL (Blazer 2008). Widowhood is strongly associated with poor SRH for both men and women independent of socio-economic status (SES) (Sudha et al. 2006). Individuals with no formal education, independent of age, report higher levels of sickness and poorer SRH (Subramanian et al. 2009; Bobak et al. 1998; Mirowsky and Ross 2008). Material deprivation and low financial security are also strongly related to poor SRH (Bobak et al. 2000). The role of social experience in predicting SRH is, however, less clear (Sen 2002). Family cohesion (type of kin rather than number of kin ties), marital stability, social class, social capital, and social networking are all associated with SRH (Vaillant and Mukamal 2001; Mansyur et al. 2008). The association between social support and social networking and SRH is, however, weaker when controlled for economic status (Tay et al. 2004), and the association between social support and SRH may also be influenced by functional abilities such as mobility and interpersonal relationships (Lee and Shinkai 2005). Visiting friends, attending social and religious functions, volunteering in community activities, and diversity of participation are all positively related to SRH independent of gender, race, or social integration (Morrow-Howell et al. 2003; Piliavin and Siegl 2007; Harris and Thoresen 2005; Young and Glasgow 1998).
The presence of modifiable healthy behaviours (smoke and alcohol abstinence, regular exercise, healthy diet, weight management, and blood pressure control) and the absence of chronic illnesses (diabetes, depression, arthritis, etc.) predict functional ability to maintain activities of daily living and contribute to good SRH and QOL in old age (Yates et al. 2008; Peel et al. 2005; Vaillant and Mukamal 2001; Gureje et al. 2008; Ishizaki et al. 2009; Collins et al. 2004; Williams et al. 2009). A physically active lifestyle in mid-life is critical for maintaining high physical function in old age independent of any long-standing illness (Hillsdon et al. 2005). Obesity strongly predicts limitation of general mobility and a larger number of chronic illnesses predicts poorer SRH outcomes (Yount et al. 2010).
Though much is known about the socio-economic and psycho-social determinants of SRH globally, the pathways through which they influence SRH are still unclear. The conventional approach has been to reduce such latent constructs to an arbitrary scale/score that is then subjected to traditional single equation regression techniques. However, such techniques do not allow for interdependencies or endogenous effects between complex constructs like SRH and QOL. Moreover, these regression techniques assume that the predictor variables are measured without any measurement error and, in fact, the measurement error of the predictor variable is attributed to the unexplained variance of the response variable. Both lead to serious bias in the regression coefficients.
In this paper we used data from a rural Indian population to test a simple conceptual model based on Jylha’s framework (Jylha 2009) of how an individual evaluates his health status based on his health experiences.
2 Methods
2.1 Ethics Statement
This study was approved by the King Edward Memorial Hospital Ethics Committee, Pune, India, and the WHO Ethics Review Committee. Respondents participated in the study after providing a written informed consent.
2.2 Sample
The Study on global AGEing and adult health (SAGE) questionnaire was administered to a rural population under demographic surveillance in Vadu area of Pune district, India, as part of a multi-country initiative of the WHO and INDEPTH—a global network of health and demographic surveillance systems in low- and middle-income countries (LMICs). The study aims to improve the empirical understanding of health and well-being of older adults aged 50 years and older in LMICs (Kowal et al. 2012). The Health and Demographic Surveillance System (HDSS), Vadu, has surveyed all individuals every 6 months in its population of about 80,000 spread over 22 villages in Pune district, India, since 2002. The SAGE was administered between December 2006 and April 2007 to a sample of 500 adults randomly selected from a list of 9,801 individuals aged 50 years and older that had been generated from the most current HDSS 2006 dataset. Nine trained graduates of both sexes interviewed the selected respondents under the supervision of a social scientist.
2.3 Instruments
The SAGE questionnaire was adapted from the 2003 World Health Survey and 16 other national cross-sectional and longitudinal studies on aging. The household questionnaire included the household roster and questions on housing, family support networks and transfers, household assets, income, and expenditures. The individual questionnaire included the socio-demographic characteristics of the individual and asked about work history and benefits, social networking, social cohesion and social capital (attending social and religious events, public meetings, volunteering, visiting friends/families/co-workers, etc.), history of diagnosed chronic illnesses (diabetes, angina, hypertension, chronic lung disease, asthma, stroke, depression, cancer, arthritis, cataracts, oral health, and injuries), and risk and preventive health behaviours using the WHO STEPS questionnaire on smoking, alcohol habits, fruit and leafy vegetable consumption, and physical activity. SES was assessed based on land ownership, ownership of household appliances, regular source of income, education, spousal support, type of toilet, cooking fuel used, and the presence of electricity in house. The ability to function in eight domains—mobility, self-care, pain and discomfort, cognition, inter-personal relationships, affect, sleep/energy, and vision—was self-assessed by the respondent on a 5-point Likert scale ranging from ‘no difficulty’ to ‘extreme difficulty’. QOL was assessed using several questions drawn from the WHOQOL–BREF questionnaire. The questions covered respondents’ satisfaction with their health, personal relationships, ability to perform activities of daily living, living conditions, money needs, and energy levels. SRH was self-assessed on a 5-point Likert scale using a single global health question (In general, how would you rate your health today?) with ratings ranging from ‘very good’ to ‘very poor’. All variables with self-ratings (e.g. SRH, functional ability, QOL, etc.) were labelled such that low values indicated ‘good’ and higher values indicated ‘poor’ status (see Appendix).
2.4 Statistical Methods
2.4.1 Structural Equation Modelling (SEM)
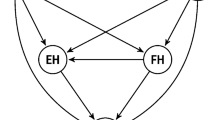
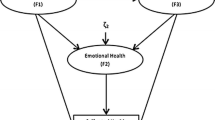
We used SEM in our analysis, and this method is increasingly being used in the social sciences, medicine, and public health (Catalano et al. 2011; Folmer et al. 2010; Hendrie et al. 2011; Scott-Parker et al. 2013; Chen et al. 2013) because it allows both latent and observed indicators to be used within a single framework (Greene 2000; Theil 1971). In the SEM model, we considered SRH and QOL as the main outcomes; limitations in functional ability, social cohesion, and chronic illness as intermediate predictors; and individual characteristics such as age, sex, SES (education, income, land ownership, etc.), and risk behaviours as the more distant predictors of SRH and QOL. We hypothesized that age had an indirect effect on QOL and SRH mediated through ability to function while sex had a direct effect on QOL that in turn affected SRH. We also hypothesized that SES had direct and indirect effects on SRH and QOL that were mediated through social networking. Risk behaviour was hypothesized to have an indirect effect on QOL and SRH that was mediated through the presence of known chronic illness (Peel et al. 2005; Yates et al. 2008). Finally, we hypothesized that QOL had a direct effect on SRH but not vice versa.
We used LISREL v8.8 software to estimate the SEM parameters. We evaluated each of the measurement models (confirmatory factor models) before evaluating the structural model part. First, we specified and tested the validity of the observed indicators for the latent constructs of QOL, FUNCTION (ability to function in the eight domains), NETWORK (social participation, networking, cohesion, and social capital), SES (education, regular income, presence of living spouse, land ownership, material assets, etc.), and RISK (risk behaviours—tobacco and alcohol consumption, physical inactivity, and dietary habits).
In the measurement model, we checked the significance of the unstandardized and standardized factor loadings (λx, λy), and we calculated the correlations between the latent variables in the SEM before testing the model (results not shown). In the structural model, we evaluated the significance of regression coefficients, squared multiple correlations, residuals, and modification indices (Joreskog and Sorbom 2001; Hair et al. 1998; Rothenberg 1971). We calculated the direct, indirect, and total effects associated with each independent variable as in path analysis (Wright 1934). The SEM model was evaluated for goodness of fit by normal theory weighted least squares χ2 and the root mean square error of approximation (RMSEA).
3 Results
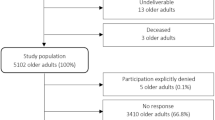
The SAGE questionnaire was administered to 321 individuals (response rate 64 %) aged 50 years and older. The non-respondents—125 (25 %) due to out-migrations or incorrect address and 54 (11 %) due to refusal or inability to comprehend—did not differ significantly in terms of age, sex, education, or other socio-demographic characteristics. The proportion of missing information was less than 2 % for any given variable. Table 1 compares the socio-demographic characteristics of the general population and the study sample. There was no significant difference in age (mean age of 61.2 and 62.2 years, respectively), sex distribution (males—about 51 %), or marital status (about 75 % with spousal support) between the SAGE sample and the overall population. The SAGE sample was better educated (8 % with higher education compared to 5 % for the general population) and had a higher standard of living (50 % had access to a private drinking water source and 25 % owned a refrigerator) compared to the general population (43 and 10 %, respectively).
Table 2 shows the unstandardized and standardized factor loadings of the significant observed indicators. It also lists the indicators dropped from the final measurement model due to weak association with their latent construct. All observed indicators retained in the final measurement model had significant loadings, and the results indicated that the latent constructs FUNCTION, NETWORK, and QOL were well represented by their observed indicators. The presence of a living spouse indicated both FUNCTION and SES. The item “How often have you worked with your neighbourhood to fix or improve something?” indicated both NETWORK and QOL with a stronger loading on NETWORK. A comparison of the standardized factor loadings showed that all latent constructs (QOL, NETWORK, FUNCTION, SES, and SRH) were strongly related to their respective indicators.
Figure 1 shows the final structural model for the tested theory. The final model had a χ2/df ratio of less than 2 (χ2 = 409.87; df = 271), and together with a RMSEA of 0.041 (an RMSEA of < 0.05 indicates close fit) this suggested an acceptable fit to the data. An examination of the Q-plot (results not shown) revealed that there were no standardized residual outliers or modification indices greater than 7.882. SRH was indirectly influenced by age and mediated through functional ability (standardized β = 0.90). Higher SES and higher QOL were associated with better SRH but these relationships lacked statistical significance.
Women rated their QOL more poorly compared to men (standardized γ = 2.61). QOL was worse among older respondents and this was mediated through limitations in functional ability (standardized β = 0.33). A higher level of social networking was seen amongst the better educated and those with regular income, which in turn was associated with a better QOL (standardized β = 0.34).
Smoking or consumption of tobacco was associated with the presence of at least one chronic illness, which in turn was associated with poor SRH and QOL. However the association between chronic illness and SRH or QOL lacked statistical significance. The standardized coefficients revealed that age and limitation in functional ability had large effects on SRH.
4 Discussion
Our study provides new understanding of the complex pathways through which social environment, functional limitation, chronic disease experience, and other factors influence SRH and QOL. The indirect effect of age on SRH was mediated through functional ability, and the indirect effects of SES and education on QOL were mediated through social networking. This furthers our understanding of how age influences SRH and how education and social networking influence QOL, which have been observed in other studies (Harris and Thoresen 2005; Morrow-Howell et al. 2003; Piliavin and Siegl 2007; Young and Glasgow 1998). The effect of low education and material deprivation on poor SRH has been seen in both Western and Post-communist populations, and a lack of perceived control appears to mediate some of the effects of material deprivation (Bobak et al. 2000). The lack of statistical significance of a direct effect of SES on SRH in our study could be explained by a stronger indirect effect of SES on SRH mediated through social networking. It is also possible that individuals perceive their social capital and social cohesion to be as important as, or more important than, their economic status for rating their health and well-being. The view that socially disadvantaged individuals may not perceive or report illness because their assessment of their own health is directly contingent on their social experience was not seen in our study (Subramanian et al. 2009). Our finding that the presence of a living spouse was an indicator for functional ability that in turn influenced SRH is consistent with a study amongst elderly people in South India. This highlights the importance of being married and the availability of kin for providing both emotional and economic support in improving SRH and health outcomes (Sudha et al. 2006).
In SEM, the statistical significance (or lack thereof) of pathways is partly dependent on how well the observed variables indicate their latent constructs. It is possible that some indicators (e.g. vegetable and fruit intake for the “RISK” construct and the abridged WHO–QOL questions for the “QOL” construct) may not adequately capture the various dimensions and meanings of their constructs. This may also explain why the intuitive relationship between SRH and QOL, though in the expected direction, was not significant in our model. This could also be a result of our poor understanding of how the elderly in India perceive and distinguish QOL from SRH or simply because the sample size was not adequate for the effect, which may not have been strong enough for the above reasons. The lack of statistical significance of the relationship between known or diagnosed chronic illness and SRH seen in other studies (Collins et al. 2004; Gureje et al. 2008; Williams et al. 2009; Tay et al. 2005) could be because most chronic illnesses like depression, diabetes, etc. often exist undiagnosed in the population thereby raising the concern of using ‘known chronic disease’ as a predictor for SRH. Alternately, it could also result from older adults considering health experiences of their peers as more important than their own previous experiences of health when rating their own health. The lack of a significant association between known chronic illness and SRH needs to be studied in-depth, possibly with bio-markers. Both age-comparative and time-comparative SRH measures have been shown to be significantly correlated with each other and are associated with physical health problems (Li et al. 2006). The need for a time reference for the SRH question has been debated as a means to distinguish between ‘perceived general health’ and ‘perceived current health’, which is a stronger predictor of health care utilization and medication use (Fielding and Li 1997). It was beyond the scope of this paper, however, to distinguish between ‘perceived general health’ and ‘perceived current health’.
Structural Equation Modelling is never able to prove causality. However, it can test causal relationships with cross-sectional data, though less convincingly than with longitudinal data. Our study was limited by the conceptual theory we tested and the constraints on relationships that we imposed on our theory. A potential shortcoming was that our conceptual model hypothesized unidirectional causality, e.g. between SRH and QOL, but there could also be reverse causality and it is not possible to determine causality or reverse causality from a cross-sectional dataset. In order to achieve identification of the model, we specified the relationship between FUNCTION and age as well as chronic illness and RISK as being without error but this might not have empirical support.
Structural Equation Modelling is an empirical-based technique to test or confirm a theory and is not to be used as an exploratory tool. In this paper, we postulated a simple theory based on existing evidence that could be easily identified by SEM. As an example, in the theory we tested sex had an indirect effect on SRH mediated through QOL. In other words, we constrained the direct effect of sex on SRH. It is possible to test alternate and more complex theories with more determinants and more complex pathways for a better understanding of SRH and QOL and their linkages. The pathways (or lack thereof) through which functional ability, disease experience, social factors, and other factors influence SRH and QOL are a function of both the data and theoretical meaningfulness. Further research is needed to cross-validate against similar datasets from different cultural settings and population sub-groups or within the same population over time.
In accordance with global trends in population aging, many countries are developing healthy aging policies to promote quality as well as years of healthy life. Our study provides evidence for policy interventions aimed to increase social networking and social participation among older adults with lower SES in order to improve their QOL as well as to increase functional ability among older adults to improve their health and health outcomes.
References
Asfar, T., Ahmad, B., Rastam, S., Mulloli, T. P., Ward, K. D., & Maziak, W. (2007). Self-rated health and its determinants among adults in Syria: A model from the Middle East. BMC Public Health, 7, 177.
Benyamini, Y., Idler, E. L., Leventhal, H., & Leventhal, E. A. (2000). Positive affect and function as influences on self-assessments of health: Expanding our view beyond illness and disability. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 55(2), P107–P116.
Blazer, D. G. (2008). How do you feel about…? Health outcomes in late life and self-perceptions of health and well-being. [Review]. Gerontologist, 48(4), 415–422.
Bobak, M., Pikhart, H., Hertzman, C., Rose, R., & Marmot, M. (1998). Socioeconomic factors, perceived control and self-reported health in Russia: A cross-sectional survey. Social Science and Medicine, 47(2), 269–279.
Bobak, M., Pikhart, H., Rose, R., Hertzman, C., & Marmot, M. (2000). Socioeconomic factors, material inequalities, and perceived control in self-rated health: Cross-sectional data from seven post-communist countries. Social Science and Medicine, 51(9), 1343–1350.
Catalano, D., Chan, F., Wilson, L., Chiu, C. Y., & Muller, V. R. (2011). The buffering effect of resilience on depression among individuals with spinal cord injury: A structural equation model. Rehabilitation Psychology, 56(3), 200–211.
Chen, Y.-C., Li, R.-H., & Chen, S.-H. (2013). Relationships among adolescents’ leisure motivation, leisure involvement, and leisure satisfaction: A Structural Equation Model. Social Indicators Research, 110(3), 1187–1199.
Collins, K., Rooney, B. L., Smalley, K. J., & Havens, S. (2004). Functional fitness, disease and independence in community-dwelling older adults in western Wisconsin. WMJ-MADISON, 103(1), 42–48.
Fayers, P. M., & Sprangers, M. A. (2002). Understanding self-rated health. The Lancet, 359(9302), 187–188.
Fielding, R., & Li, J. (1997). A validation of the concept of current perceived health and the Current Perceived Health-42 (CPH-42) questionnaire. Quality of Life Research, 6(1), 35–42.
Folmer, H., Dutta, S., & Oud, H. (2010). Determinants of rural industrial entrepreneurship of farmers in West Bengal: A structural equation approach. International Regional Science Review, 33(4), 367–396.
Garrity, T. F., Somes, G. W., & Marx, M. B. (1978). Factors influencing self-assessment of health. Social Science and Medicine, 12(2A), 77–81.
Greene, W. H. (2000). Econometric analysis. London: Prentice Hall.
Gregory, D., Johnston, R., Pratt, G., Watts, M., & Whatmore, S. (2009). Dictionary of human geography (5th ed., p. 1070). Hoboken, NJ, USA: Wiley.
Gureje, O., Ademola, A., & Olley, B. O. (2008). Depression and disability: Comparisons with common physical conditions in the Ibadan study of aging. Journal of the American Geriatrics Society, 56(11), 2033–2038.
Hair, J. F., Andersen, R. E., Tatham, R. L., & Black, W. C. (1998). Multivariate data analysis (5th ed.). Upper Saddle River: Prentice-Hall, NJ.
Harris, A. H., & Thoresen, C. E. (2005). Volunteering is associated with delayed mortality in older people: Analysis of the longitudinal study of aging. Journal of Health Psychology, 10(6), 739–752.
Hendrie, G. A., Coveney, J., & Cox, D. N. (2011). Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutrition, 2, 1–10.
Hillsdon, M. M., Brunner, E. J., Guralnik, J. M., & Marmot, M. G. (2005). Prospective study of physical activity and physical function in early old age. American Journal of Preventive Medicine, 28(3), 245–250.
Hirve, S., Juvekar, S., Lele, P., & Agarwal, D. (2010). Social gradients in self-reported health and well-being among adults aged 50 and over in Pune District, India. Glob Health Action, 3, doi:10.3402/gha.v3i0.2128.
Ishizaki, T., Yoshida, H., Suzuki, T., & Shibata, H. (2009). The association between self-rated health status and increasing age among older Japanese living in a rural community over a 6-year period: A longitudinal data analysis. Gerontology, 55(3), 344–352.
Joreskog, K., & Sorbom, D. (2001). LISREL 8: Structural Equation modelling with the SIMPLIS command language. Chicago, IL: Scientific Software International, Inc.
Jurges, H., Avendano, M., & Mackenbach, J. P. (2008). Are different measures of self-rated health comparable? An assessment in five European countries. European Journal of Epidemiology, 23(12), 773–781.
Jylha, M. (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science and Medicine, 69(3), 307–316.
Kowal, P., Chatterji, S., Naidoo, N., Biritwum, R., Fan, W., Lopez Ridaura, R., et al. (2012). Data resource profile: The World Health Organization Study on global AGEing and adult health (SAGE). International Journal of Epidemiology, 41(6), 1639–1649.
Lee, Y., & Shinkai, S. (2005). Correlates of cognitive impairment and depressive symptoms among older adults in Korea and Japan. International Journal of Geriatric Psychiatry, 20(6), 576–586.
Li, Z. B., Lam, T. H., Ho, S. Y., Chan, W. M., Ho, K. S., Li, M. P., et al. (2006). Age- versus time-comparative self-rated health in Hong Kong Chinese older adults. International Journal of Geriatric Psychiatry, 21(8), 729–739.
Lundberg, O., & Manderbacka, K. (1996). Assessing reliability of a measure of self-rated health. Scandinavian Journal of Social Medicine, 24(3), 218–224.
Machado, G. M., Barreto, S. M., Passos, V. M., & Lima-Costa, M. F. (2006). Health status indicators among community-dwelling elders with arthritis: The Bambui health and aging study. Journal of Rheumatology, 33(2), 342–347.
Mansyur, C., Amick, B. C., Harrist, R. B., & Franzini, L. (2008). Social capital, income inequality, and self-rated health in 45 countries. Social Science and Medicine, 66(1), 43–56.
Mavaddat, N., Kinmonth, A. L., Sanderson, S., Surtees, P., Bingham, S., & Khaw, K. T. (2011). What determines Self-Rated Health (SRH)? A cross-sectional study of SF-36 health domains in the EPIC-Norfolk cohort. Journal of Epidemiology and Community Health, 65(9), 800–806.
Mirowsky, J., & Ross, C. E. (2008). Education and self-rated health: Cummulative advantage and its rising importance. Research on Aging, 30(1), 93–122.
Mora, P. A., DiBonaventura, M. D., Idler, E., Leventhal, E. A., & Leventhal, H. (2008). Psychological factors influencing self-assessments of health: Toward an understanding of the mechanisms underlying how people rate their own health. Annals of Behavioral Medicine, 36(3), 292–303.
Morrow-Howell, N., Hinterlong, J., Rozario, P. A., & Tang, F. (2003). Effects of volunteering on the well-being of older adults. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58(3), S137–S145.
Peel, N. M., McClure, R. J., & Bartlett, H. P. (2005). Behavioral determinants of healthy aging. American Journal of Preventive Medicine, 28(3), 298–304.
Piliavin, J. A., & Siegl, E. (2007). Health benefits of volunteering in the Wisconsin longitudinal study. Journal of Health and Social Behavior, 48(4), 450–464.
Robine, J. M., & Jagger, C. (2003). Creating a coherent set of indicators to monitor health across Europe: The Euro-REVES 2 project. The European Journal of Public Health, 13(3 Suppl), 6–14.
Rothenberg, T. J. (1971). Identification in parametric models. Econometrica, 39, 577–591.
Salomon, J. A., Mathers, C. D., Chatterji, S., Sadana, R., Ustun, T. B., & Murray, C. J. (2003). Quantifying individual levels of health: Definitions, concepts and measurement issues. In C. J. Murray & D. B. Evans (Eds.), Health systems performance assessment: Debates, methods and empiricism (pp. 301–318). Geneva: World Health Organization.
Salomon, J. A., Nordhagen, S., Oza, S., & Murray, C. J. (2009). Are Americans feeling less healthy? The puzzle of trends in self-rated health. American Journal of Epidemiology, 170(3), 343–351.
Scott-Parker, B., Watson, B., King, M. J., & Hyde, M. K. (2013). A further exploration of sensation seeking propensity, reward sensitivity, depression, anxiety, and the risky behaviour of young novice drivers in a structural equation model. Accident Analysis and Prevention, 50, 465–471.
Sen, A. (2002). Health: Perception versus observation. [Editorial]. BMJ, 324(7342), 860–861.
Subramanian, S. V., Subramanyam, M. A., Selvaraj, S., & Kawachi, I. (2009). Are self-reports of health and morbidities in developing countries misleading? Evidence from India. Social Science and Medicine, 68(2), 260–265.
Sudha, S., Suchindran, C., Mutran, E. J., Rajan, S. I., & Sarma, P. S. (2006). Marital status, family ties, and self-rated health among elders in South India. Journal of Cross-Cultural Gerontology, 21(3–4), 103–120.
Tay, J. B., Kelleher, C. C., Hope, A., Barry, M., Gabhainn, S. N., & Sixsmith, J. (2004). Influence of sociodemographic and neighbourhood factors on self rated health and quality of life in rural communities: Findings from the Agriproject in the Republic of Ireland. Journal of Epidemiology and Community Health, 58(11), 904–911.
Tay, T., Wang, J. J., Rochtchina, E., & Mitchell, P. (2005). Vision and self-rated health: Longitudinal findings from an older Australian population. Ophthalmic Epidemiology, 12(3), 179–184.
Theil, H. (1971). Principles of econometrics. New York: Wiley.
Vaillant, G. E., & Mukamal, K. (2001). Successful aging. American Journal of Psychiatry, 158(6), 839–847.
Williams, S. R., Pham-Kanter, G., & Leitsch, S. A. (2009). Measures of chronic conditions and diseases associated with aging in the national social life, health, and aging project. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 64(Suppl 1), i67–i75.
World Health Organization. (1996). Health interview surveys: Towards international harmonization of methods and instruments. Copenhagen: World Health Organization, European Regional Office.
Wright, S. (1934). The method of path coefficients. The Annals of Mathematical Statistics, 5(3), 161–215.
Yates, L. B., Djousse, L., Kurth, T., Buring, J. E., & Gaziano, J. M. (2008). Exceptional longevity in men: Modifiable factors associated with survival and function to age 90 years. Archives of Internal Medicine, 168(3), 284–290.
Young, F. W., & Glasgow, N. (1998). Voluntary social participation and health. Research on Aging, 20(3), 339–362.
Yount, K. M., Hoddinott, J., & Stein, A. D. (2010). Disability and self-rated health among older women and men in rural Guatemala: The role of obesity and chronic conditions. Social Science and Medicine, 71(8), 1418–1427.
Acknowledgments
This paper uses data from the World Health Organization Study on Global AGEing (SAGE). SAGE is supported by the US National Institute on Aging through Interagency Agreements (OGHA 04034785; YA1323-08-CN-0020; Y1-AG-1005-01) and through a research grant (R01-AG034479). Health and Demographic Surveillance System, Vadu, is a member of the International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH Network). The analyses and writing of this paper has been financed by the Umeå Centre for Global Health Research, Umeå University, with support from FAS, the Swedish Council for Working Life and Social Research (Grant No. 2006-1512) through its Ph.D. fellowship to the first author. We acknowledge the support of Kathy Kahn from INDEPTH Network and Somnath Chatterjee, Paul Kowal, and Nirmala Naidoo from WHO, Geneva, for coordinating this multi-country study. Thanks are due to Pallavi Lele and the Vadu HDSS team for their quality work and the older adult population of the Vadu Demographic Surveillance Area for their willingness to contribute their knowledge to this study.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 3.
Rights and permissions
About this article
Cite this article
Hirve, S., Oud, J.H.L., Sambhudas, S. et al. Unpacking Self-Rated Health and Quality of Life in Older Adults and Elderly in India: A Structural Equation Modelling Approach. Soc Indic Res 117, 105–119 (2014). https://doi.org/10.1007/s11205-013-0334-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-013-0334-7