Abstract
We evaluated whether patients who meet the survey criteria for fibromyalgia suffer from a higher rate of sexual dysfunction and sleep disorders compared to those without fibromyalgia. While 54 of the participants were patients diagnosed with fibromyalgia, the remaining 41 made up the healthy control group of the study. The patients were given four different sets of questionnaires: the Pittsburgh Sleep Quality Index (PSQI), Revised Fibromyalgia Impact Questionnaire, Beck Depression Inventory (BDI) and Female Sexual Function Index (FSFI) in order to evaluate sleep function, fibromyalgia disease severity, depression status and sexual function. We found a mean FSFI score of 19.29 ± 3.35 in the women with FMS and 25.88 ± 2.47 in the control group. The participants with FMS suffered from higher depression rates compared to participants in the healthy group. With PSQI score > 5 indicating the presence of a sleep disorder, sleep disorders were detected in 66.6% of women with FMS and 39.3% without FMS. In the Spearman correlation analysis, weak negative correlation was found between the PSQI and FSFI values (r = − 0.213; p = 0.076). In contrast, a positive correlation was detected between the FSFI and RFIQ (r = 0.578; p = < 0.001). Finally, a negative correlation was detected between FSFI and BDI values (r = − 0.509; p < 0.001). Therefore, physicians who investigate the fibromyalgia syndrome in their routine practice to take the negative effects of sexual dysfunction on female patients into consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia syndrome (FMS), which affects about 2–8% of the population, is characterized by chronic widespread pain (CWP), allodynia (a pain due to a stimulus which does not normally provoke pain), sleep disturbance, functional bladder problems and numbness [1,2,3]. A female to male incidence ratio is somewhere between 7:1 and 9:1 [1]. FMS may cause functional disability and have a significantly negative effect on quality of life [3]. The prevalence of FMS increases with age and it is especially more frequent at or near menopause.
FMS is associated with substantial physical and psychological impairment, reduced quality of life and a spectrum of sexual problems [4, 5]. In patients with chronic fatigue syndrome, Blazquez et al. reported a higher incidence of sexual dysfunction, which is defined as a change in a phase of the sexual activity that can culminate in frustration, pain and a reduction in the number of sexual intercourses. He also reported a higher number of cognitive, neurological and neurovegetative symptoms concomitant to fibromyalgia [6, 7].
Sex is a human activity that improves quality of life and has positive psychological and social effects. There are several recorded causes of sexual dysfunction, including physical and psychiatric disorders [8]. Accumulating evidence from studies with samples of fibromyalgia patients has shown the significant association between sexual dysfunction and sleep disturbance. FMS with sleep disorders and depression leads to a deterioration in the sexual life of both female and male patients, and sexual dysfunction has been shown to be more frequent in patients with FMS than in control groups [9, 10]. Based on the results of previous studies, depression, anxiety, fatigue and widespread pain are the leading causative factors of sexual dysfunction in patients with FMS [11, 12]. While the mechanisms are unclear, they appear to involve the hypothalamus–pituitary–adrenal axis, sexual hormones and cytokines. Depression affects 83.3% patients with FMS and, in Brazil, 67.2% of them have depression diagnosed as a comorbidity [13, 14]. Understanding the association between sexual dysfunction, sleep disorder, depression and FMS is of importance for the development of prevention and treatment strategies. In this context, we evaluated whether patients who meet the survey criteria for FMS suffer from a higher rate of sexual dysfunction and sleep disorders compared to healthy normals.
Materials and Methods
We performed a prospective cross-sectional study with participants who visited our orthopedic clinic. Fifty-four married and sexually active female patients with FMS [diagnosed according to the American College of Rheumatology(ACR) criteria] and more than 6 months of pain [15] were included in the study. The tender points examination was performed at the time of diagnosis on the day of the investigation, in all subjects by a single observer. All patients presented with at least 11 tender points, fulfilling the American College of Rheumatology criteria. The control group comprised 41 married couples with an active sexual life. Inclusion criteria of the control group were as follows: healthy women with no complaint of pain during the last 12 months and no use of chronic medication. All questionnaires were answered individually without intervention of the spouse. Exclusion criteria consisted of presence of pelvic trauma/surgery, urinary incontinence, lower urinary tract symptoms, cardiovascular disease, psychiatric problems, use of drugs, and alcohol abuse. We also excluded women who had endocrinological/gynecological diseases and who had taken psychotropics. Sexually inactive women were also excluded, as stated in the questionnaire (“no activity in the last 4 weeks”). The patients’ age, height, body weight, body mass index (BMI), and educational status were recorded. The patients were given four different sets of questionnaires: the Pittsburgh Sleep Quality Index (PSQI), Revised Fibromyalgia Impact Questionnaire (FIQR), Beck Depression Inventory (BDI) and Female Sexual Function Index (FSFI) in order to evaluate sleep function, FM disease severity, depression status and sexual function.
The FSFI was employed to assess sexual function and all participating women completed the FSFI form (translated into Turkish). The FSFI is divided into six main domains: desire, arousal, lubrication, orgasm, satisfaction, and pain, with each item scored with a 5- or 6-point Likert-type scale. The maximum score for each domain is 6, and total FSFI scores ranged from 2 to 36, with higher scores indicating better sexual function [16]. A cutoff total score of ≤ 26.55 on the FSFI is the current standard for diagnosing sexual dysfunction in women across a wide range of ages (18–74 years) and lifestyles [17]. Furthermore, to estimate the presence or sexual difficulty in each domain, a score of 40% or less than the maximum value of the desire subscale (≤ 2.4) and a score of less than 60% of the maximum value of the other five domain subscales (< 3.6) were selected as the cutoff, according to the previous report, respectively [18]. Prior to conducting the present study, institutional review board approval was obtained and all study participants gave informed consent.
The Revised Fibromyalgia Impact Questionnaire (FIQR) was recently developed by Bennett et al. [19] recently in an attempt to correct the limitations of the FIQ, while also retaining the essential properties of the original instrument [20, 21]. They developed an online and paper-equivalent version of the questionnaire (FIQR). The basic domain structure of the original instrument of the FIQR in terms of function, overall impact, and severity of symptoms that are characteristic of FMS are the same as in the FIQ. However, modified function questions and the questions that measure dyscognition, tenderness, balance, and environmental sensitivity, which were not part of the original FIQ, were added in the FIQR. Furthermore, some of the problems in the wording, omissions, concepts, and scoring of the original FIQ were corrected in the FIQR. All questions were graded on a 0–10 numeric scale.
For assessment of the patients’ sleep disorders, we used the PSQI, which is a scale that provides information about the type and severity of sleep disorder and sleep quality in the last 1 month. All questionnaires were completed under the supervision of a physician and 19 questions out of a total of 24 questions were answered by the patient, and the remaining 5 were answered by the partner of the patient. The total scores for the seven subdimensions give the total PSQI score. A total score of 5 and less indicates that the sleep quality is “good”. A global PSQI score > 5 is accepted as indicating poor sleep quality [22].
The Beck Depression Inventory (BDI) is a 21-item survey that measures items relating to the symptoms of depression such as hopelessness, irritability, cognitive problems, feelings of guilt or being punished, and the presence of physical symptoms, such as fatigue, weight loss, and lack of sexual desire [23]. BDI is a depression assessment questionnaire that has been validated [23] to use within the Turkish population. For this reason, we used the BDI instead of the BDI-II. The scores of the BDI range from 0 to 63; higher scores indicate more severe depression. A BDI score < 11 is consistent with the absence of depression.
SPSS version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp.) was used for data analysis in the present study. The normal distribution of data was checked using the Kolmogorov–Smirnov test and a comparison was made for each parameter. While the t test was used for normally distributed groups, and the Mann–Whitney U test was used for abnormal distribution. Chi square analyses were employed for a detailed examination of differences across groups. The one-way ANOVA test was used to compare continuous variables and regression analyses were run for comparing multiple variables. Pearson’s correlation analysis was applied as the correlation analysis. The significance of these tests, in turn, was defined as p ≤ 0.05. Also, Institutional Review Board (IRB) approval was obtained from the local committee.
Results
The mean ages were 32.56 ± 4.90 years and 31.53 ± 4.86 years for participants in the study and control group, respectively. No statistical differences appeared between the mean ages of the two groups (p = 0.535). BMI, duration of marriage, number of children in each group were also similar. Mean BMI level was 26.78 ± 5.10 in study group and 28.15 ± 2.06 in control group (p = 0.190). Educational status was statistically different between the two groups. Participants in the study group, appeared to have a higher educational status compared to participants in the control group. All results were shown in Table 1. Biochemical and hormonal parameters were within normal limits in the case of all subjects, and no significant difference was found between patients with fibromyalgia and healthy controls.
The present study resulted in a mean FSFI score of 19.29 ± 3.35 in women with FMS in contrast to a FSFI score of 25.88 ± 2.47 in the control group. Although this difference between the two groups is statistically significant (p < 0.001), a more detailed evaluation of the subdomains desire, arousal and lubrication domains did not reveal a statistically significant difference. Mean BDI score was 11 (4–16) in women with FMS and 4.5 (0–13) in women without FMS, respectively. Therefore, women diagnosed with FMS suffered from depression at higher rates than women in the healthy group (p < 0.001) (Table 1).
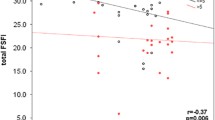
On the other hand, mean PSQI score was 9 (3–20) in study group and 4.5 (1–15) in control group, respectively (p < 0.001). A PSQI score > 5 indicating the presence of a sleep disorder, sleep disorders were detected in 66.6% of women with FMS and 39.3% of women without FMS. Also, the median total FSFI score was significantly lower in patients with sleep disorders [21.4 (18.9–25.3) vs. 23.2 (21.2–28.4), p < 0.05]. A weak negative correlation was detected between PSQI and FSFI values (r = − 0.213; p = 0.076) in the Spearman correlation analysis. In contrast, a positive correlation was found between the FSFI and RFIQ (r = 0.578; p = < 0.001) and finally, a negative correlation was determined between FSFI and BDI values (r = − 0.509; p < 0.001). Also, no correlation was observed between BMI and FSFI total score (r = − 0.067; p = 0.582).
Discussion
This study showed a significant association between sexual dysfunction, depression and sleep disorders in FMS patients. The physiopathology of fibromyalgia is very complex and possibly involves alterations in the neurotransmitters of pain modulation, thalamic perfusion dysfunction, and changes in the hypo-thalamic-pituitary-adrenal axis. While most patients with fibromyalgia complain of chronic fatigue and generalized pain, 25% also have major depression at diagnosis and 50% may have a past history of depression [24, 25]. Of note, the prevalence of depression is increased in fibromyalgia patients compared to medically healthy individuals [26, 27]. Among patients with fibromyalgia, the current and 12-month prevalence of major depression has been reported to be between 20 and 30% in various previous studies, [28, 29] but also from 30 to 80% in other studies [30]. The present study, similarly demonstrated a higher BDI score among patients with FMS. In contrast to our study, Dogan et al. [31] reported no significant difference in the BDI scores between patients with FMS and the control subjects. Depression has the effect of lowering the patient’s pain tolerance, so that a noxious stimulus that normally would cause no more than a mild discomfort gives rise to pain [24, 32, 33]. This may be related to the low levels of pain-inhibiting neurotransmitters such as serotonin, noradrenalin, and endogenous opioid peptides in patients with depression or, alternatively, as a result of their affective disorder, such patients may appear to worry that even mild pain is the harbinger of some serious illness [34]. This mechanism may, therefore, explain the greater BDI score of our patients with fibromyalgia.
In a previous study, researchers showed that the women with depression have high prevalence of sexual dysfunction in the reproductive age group [35]. Therefore, sexual dysfunction may be one of the considerations during the assessment of depression. In our study, we similarly found a negative correlation between FSFI score and the BDI score, demonstrating once again that women with depression with or without fibromyalgia have more sexual dysfunction. In a few studies researchers reported a significant association between FMS and FSD. However, these studies rely on very small samples and fail to include standardized and validated questionnaires. Unlike these studies, in the present study, we applied The Revised Fibromyalgia Impact Questionnaire (FIQR), which was developed by Bennett et al. [19] recently in an attempt to correct the limitations of the FIQ and is fully validated. Overall, most of the studies suggest that especially arousal levels and orgasmic function seem to be decreased in women with FMS. The studies further provide evidence for significantly more pain during intercourse in women with FMS [36,37,38]. In one of these studies, Shaver and colleagues found women with FMS to report significantly more negative changes in sexual functioning, including fewer orgasms, decreased arousal and excitement, and more pain during intercourse. Interestingly, no differences in desire levels between women with FMS and healthy women were observed. Similarly, Aydin and colleagues also found more pain complaints during sexual intercourse in FMS patients compared with controls (50 vs. 16.7%), and several pieces of evidence suggest a higher prevalence of yeast infections and vulvodynia (both of which have been suggested as risk factors for sexual pain disorders) in women with FMS. [10, 21, 37,38,39]. In another study, Yilmaz et al. reported that the mean total FSFI scores and all subgroup scores were significantly lower in patients with fibromyalgia compared with the scores of patients without FMS [40]. However not all domains were lower in women with FMS. In our recent published meta-analysis, we found a clear association between FMS and the overall femal sexual dysfunction score as well as sexual function domains including arousal, desire, lubrication, pain, orgasm, and satisfaction were demonstrated [41]. In our present study, we found that total FSFI scores, orgasm, satisfaction and pain domains were lower in women with FMS (p < 0.01). But, we did not find statistical difference between the desire, arousal and lubrication domains within the groups.
As we know, the pathophysiology of FMS includes alterations in ascending and descending central nervous and peripheral nerve pathways, which lead to increased pain and sensitivity. Some researchers have supported the opinion that several genetic predispositions, stress and poor sleep are the risk factors for FMS [42]. In a recent study, poor sleep is reported by almost 80% of patients with fibromyalgia [43]. Epidemiological studies indicate that lower sleep quality is a risk factor for fibromyalgia; poor sleep is strongly and dose-dependently associated with symptom severity [44] in the fibromyalgia population. Clinical trials of pharmacological therapies have shown that these therapies improve the sleep quality and reduced pain in patients with fibromyalgia [45, 46]. We used PSQI for assessment of sleep disorders. The PSQI includes seven components; however, only the global score can be used to differentiate poor sleepers from good sleepers, with the global PSQI score of > 5 being a sensitive and specific measure of lower sleep quality. In the present study, the mean PSQI scores were 9 (3–20) in individuals with fibromyalgia and 4.5 (1–15) in healthy controls. Similarly to our study, a recent meta analysis showed that individuals with fibromyalgia perceived lower sleep quality [47].
The main cause of sexual dysfunction in patients with FMS is unknown. However, similar to the findings of the present study, many studies found that anxiety, depression and sleep impairment, were frequently found among FMS patients. Therefore, is possible to conclude that all these conditions may be in response to sexual dysfunction [48]. A recent study evaluating sexual dysfunction in women with FMS and sleep disorder and FMS alone, demonstrated that sleep disorder have a negative impact on sexual function in women with FMS. They found that the median FSFI scores were 21.4 (18.9–25.3) in patients with sleep disorder and 29.2 (27.2–32.4) in patients without sleep disorder [49]. Similarly, we found median FSFI scores were 21.4 (18.9–25.3) in patients with sleep disorder and 23.2 (21.2–28.4) in patients without sleep disorder. In an other study similar to the present one, which was performed by Koca et al., a positive correlation was observed between the patients with PSQI score > 5 (poor sleep quality) and sexual dysfunction [50]. They also found poor sleep quality to be markedly associated with the pain score, severity of disease, and sexual dysfunction.
When interpreting the results of the present study, it is important for some potential limitations to be taken into consideration. The results are not generalizable to other scenarios since it was conducted in a single centre. The implementation of Islamic morality in Turkey makes sexuality a subject that is scarcely addressed in healthcare services. The inclusion of participants of other ethnicities or sexual tendencies in the study, could have cast different results. In addition, the present study does not include an analysis of the smoking history or the insulin resistance status of the participant with FMS. Finally, this study only includes Turkish males and the results may not be generalized to males from other racial or ethnic backgrounds.
In conclusion, the present study demonstrates that women with fibromyalgia, have more sexual dysfunction, sleep disorders and depression. Also, a correlation was found between FSFI, BDI and PSIQ scores. Therefore, physicians who investigate the fibromyalgia syndrome in routine practice, should take the negative effects of sexual dysfunction on female patients into consideration. It is concluded that reductions in generalized pain, severity of disease, depression and sleep disorder may also reduce sexual problems in patients. Additional studies involving greater numbers of patients are necessary to evaluate the effect of fibromyalgia on sexual dysfunction and determine pathophysiological mechanisms of this disorder.
References
Brummett, C.M., Goesling, J., Tsodikov, A., Meraj, T.S., Wasserman, R.A., Clauw, D.J., Hassett, A.L.: Prevalence of the fibromyalgia phenotype in patients with spine pain presenting to a tertiary care pain clinic and the potential treatment implications. Arthritis Rheum. 65(12), 3285–3292 (2013)
Silver, D.S., Wallace, D.J.: The management of fibromyalgia-associated syndromes. Rheum. Dis. Clin. North Am. 28(2), 405–417 (2002)
Wolfe, F., Anderson, J., Harkness, D., Bennett, R.M., Caro, X.J., Goldenberg, D.L., et al.: Work and disability status of persons with fibromyalgia. J. Rheumatol. 24, 1171–1178 (1997)
Tutoglu, A., Boyaci, A., Koca, I., Celen, E., Korkmaz, N.: Quality of life, depression, and sexual dysfunction in spouses of female patients with fibromyalgia. Rheumatol. Int. 34(8), 1079–1084 (2014)
Matarín Jiménez, T.M., Fernández-Sola, C., Hernández-Padilla, J.M., Correa Casado, M., Antequera Raynal, L.H., Granero-Molina, J.: Perceptions about the sexuality of women with fibromyalgia syndrome: a phenomenological study. J. Adv. Nurs. 73(7), 1646–1656 (2017)
Ferreira Cde, C., da Mota, L.M., Oliveira, A.C., de Carvalho, J.F., Lima, R.A., Simaan, C.K., et al.: Frequency of sexual dysfunction in women with rheumatic diseases. Rev. Bras. Reumatol. 53(1), 35–46 (2013)
Blazquez, A., Ruiz, E., Aliste, L., García-Quintana, A., Alegre, J.: The effect of fatigue and fibromyalgia on sexual dysfunction in women with chronic fatigue syndrome. J. Sex Marital Ther. 41(1), 1–10 (2015)
Rico-Villademoros, F., Calandre, E.P., Rodriguez-Lopez, C.M., Garcia-Carrillo, J., Ballesteros, J., Hidalgo-Tallon, J., et al.: Sexual functioning in women and men with fibromyalgia. J. Sex Med. 9(2), 542–549 (2012)
Batmaz, I., Sariyildiz, M.A., Dilek, B., Inanir, A., Demircan, Z., Hatipoglu, N., et al.: Sexuality of men with fibromyalgia: what are the factors that cause sexual dysfunction? Rheumatol. Int. 33(5), 1265–1270 (2013)
Aydin, G., Basar, M.M., Keles, I., Ergun, G., Orkun, S., Batislam, E.: Relationship between sexual dysfunction and psychiatric status in premenopausal women with fibromyalgia. Urology 67(1), 156–161 (2006)
Kool, M.B., Woertman, L., Prins, M.A., Van Middendorp, H., Geenen, R.: Low relationship satisfaction and high partner involvement predict sexual problems of women with fibromyalgia. J. Sex Marital Ther. 32(5), 409–423 (2006)
Orellana, C., Casado, E., Masip, M., Galisteo, C., Gratacos, J., Larrosa, M.: Sexual dysfunction in fibromyalgia patients. Clin. Exp. Rheumatol. 26(4), 663–666 (2008)
Lange, M., Petermann, F.: Influence of depression on fibromyalgia: a systematic review. Schmerz 24(4), 326–333 (2010). https://doi.org/10.1007/s00482-010-0937-8. (in German)
Berber, J.S.S., Kupek, E., Berber, S.C.: Prevalence of depression and its correlation with quality of life in patients with fibromyalgia syndrome. Rev. Bras. Reumatol. 45, 47–54 (2005). https://doi.org/10.1590/s0482-50042005000200002. (in Portuguese)
Wolfe, F., Smythe, H.A., Yunus, M.B., Bennett, R.M., Bombardier, C., Goldenberg, D.L., et al.: The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum. 33(2), 160–172 (1990)
Rosen, R., Brown, C., Leiblum, S., Meston, C., Shabsigh, R., Ferguson, D., D’Agostino Jr., R.: The Female Sexual Function Index (FSFI): a multidimensional self-reported instrument for the assessment of female sexual function. J. Sex Marital Ther. 26, 191–208 (2000)
Wiegel, M., Meston, C., Rosen, R.: The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J. Sex Marital Ther. 31, 1–20 (2005)
Jiann, B.P., Su, C.C., Yu, C.C., Wu, T.T., Huang, J.K.: Risk factors for individual domains of female sexual function. J. Sex. Med. 6, 3364–3375 (2009)
Bennett, R.M., Friend, R., Jones, K.D., Ward, R., Han, B.K., Ross, R.L.: The revised fibromyalgia impact questionnaire (FIQR): validation and psychometric properties. Arthritis Res. Ther. 11, R120 (2009)
Burckhardt, C.S., Clark, S.R., Bennett, R.M.: The fibromyalgia impact questionnaire: development and validation. J. Rheumatol. 18, 728–733 (1991)
Bennett, R.: The fibromyalgia impact questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin. Exp. Rheumatol. 23, 154–162 (2005)
Buysse, D.J., Reynolds III, C.F., Monk, T.H., Berman, S.R., Kupfer, D.J.: The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989)
Hisli, N.: A study on the validity of Beck depression inventory. Psychol. J. 22, 118–126 (1988). (in Turkish)
Campbell, S.M.: Regional myofascial pain syndromes. Rheum. Dis. Clin. North Am. 15, 31–44 (1989)
De Costa, E.D., Kneubil, M.C., Leao, W.C., The, K.B.: Assessment of sexual satisfaction in fibromyalgia patients. Einstein 2, 177–181 (2004)
Rapphael, K.G., Janal, M.N., Nayak, S., Schwartz, J.E., Gallagher, R.M.: Psychiatric comorbidities in a community sample of women with fibromyalgia. Pain 124, 117–125 (2006)
Martinez, J.E., Ferraz, M.B., Fontana, A.M., Atra, E.: Psychological aspects of Brazilian women with fibromyalgia. J. Psychosom. Res. 39, 167–174 (1995)
Russell, A.S., Hui, B.K.: The use of PRIME-MD questionnaire in a rheumatology clinic. Rheumatol. Int. 25, 292–295 (2005)
Kassam, A., Patten, S.B.: Major depression, fibromyalgia and labour force participation: a population-based cross-sectional study. BMC Musculoskelet. Disord. 7, 4 (2006)
Fietta, P., Manganelli, P.: Fibromyalgia and psychiatric disorders. Acta Biomed. 78, 88–95 (2007)
Dogan, S.K., Aytur, Y.K., Atbasoglu, C.: Assessment of the relatives or spouses cohabiting with the fibromyalgia patients: is there a link regarding fibromyalgia symptoms, quality of life, general health and psychologic status? Rheumatol. Int. 31(9), 1137–1142 (2011)
Yunus, M.B., Inanıcı, F.: Fibromyalgia syndrome: clinical features, diagnosis, and biopathophysiologic mechanisms. In: Rachlin, E.S., Rachlin, I. (eds.) Myofascial Pain and Fibro Myalgia: Trigger Point Management, pp. 3–31. Mosby, Philadelphia (2002)
Hudson, J.I., Hudson, M.S., Pliner, L.F., Goldenberg, D.L., Pope Jr., H.G.: Fibromyalgia and major affective disorder: a controlled phenomenology and family history study. Am. J. Psychiatry 142, 441–446 (1985)
Baldry, P.: The emotional aspects of pain. In: Baldry, P. (ed.) Myofascial Pain and Fibromyalgia Syndromes: A Clinical Guide to Diagnosis and Management, pp. 45–55. Churchill Livingstone, Edinburgh (2001)
Sreelakshmy, K., Velayudhan, R., Kuriakose, D., Nair, R.: Sexual dysfunction in females with depression: a cross-sectional study. Trends Psychiatry Psychother. 39(2), 106–109 (2017)
Prins, M.A., Woertman, L., Kool, M.B., Geenen, R.: Sexual functioning of women with fibromyalgia. Clin. Exp. Rheumatol. 24, 555–556 (2006)
Shaver, J.L., Wilbur, J., Robinson, F.P., Wang, E., Buntin, M.S.: Women’s health issues with fibromyalgia syndrome. J. Womens Health (Larchmt) 15, 1035–1045 (2006)
Gordon, A.S., Panahian-Jand, M., McComb, F., Melegari, C., Sharp, S.: Characteristics of women with vulvar pain disorders: responses to a web-based survey. J. Sex Marital Ther. 29(suppl 1), 45–58 (2003)
Ghizzani, A., Orlandini, C., Bernardi, M.G., Cevenini, G., Luisi, S.: Sexual pain in women: quality of sex life and marital relations. Minerva Ginecol. 69(4), 381–389 (2017)
Yilmaz, H., Yilmaz, S.D., Polat, H.A., Salli, A., Erkin, G., Ugurlu, H.: The effects of fibromyalgia syndrome on female sexuality: a controlled study. J. Sex Med. 9, 779–785 (2012)
Besiroglu, H., Dursun, M.: The association between fibromyalgia and female sexual dysfunction: a systematic review and meta-analysis of observational studies. Int. J. Impot. Res. 31, 288–297 (2019). https://doi.org/10.1038/s41443-018-0098-3
Chinn, S., Caldwell, W., Gritsenko, K.: Fibromyalgia pathogenesis and treatment options update. Curr. Pain Headache Rep. 20, 25 (2016)
Jacobson, S.A., Simpson, R.G., Lubahn, C., Hu, C., Belden, C.M., Davis, K.J., et al.: Characterization of fibromyalgia symptoms in patients 55–95 years old: a longitudinal study showing symptom persistence with suboptimal treatment. Aging Clin. Exp. Res. 27(1), 75–82 (2014)
Choy, E.H.: The role of sleep in pain and fibromyalgia. Nat. Rev. Rheumatol. 11, 513–520 (2015)
Straube, S., Derry, S., Moore, R.A., McQuay, H.J.: Pregabalin in fibromyalgia: meta-analysis of efficacy and safety from company clinical trial reports. Rheumatology 49(4), 706–715 (2010)
Spaeth, M., Rizzi, M., Sarzi-Puttini, P.: Fibromyalgia and sleep. Best Pract. Res. Clin. Rheumatol. 25(2), 227–239 (2011)
Wu, Y.L., Chang, L.Y., Lee, H.C., Fang, S.C., Tsai, P.S.: Sleep disturbances in fibromyalgia: a meta-analysis of case–control studies. J. Psychosom. Res. 96, 89–97 (2017)
Bazzichi, L., Giacomelli, C., Rossi, A., Sernissi, F., Scarpellini, P., Consensi, A., et al.: Fibromyalgia and sexual problems. Reumatismo 64, 261–267 (2012)
Amasyali, A.S., Taştaban, E., Amasyali, S.Y., Turan, Y., Kazan, E., Sari, E., et al.: Effects of low sleep quality on sexual function, in women with fibromyalgia. Int. J. Impot. Res. 28(2), 46–49 (2016)
Koca, T.T., Karaca Acet, G., Tanrıkut, E., Talu, B.: Evaluation of sleep disorder and its effect on sexual dysfunction in patients with fibromyalgia syndrome. Turk. J. Obstet. Gynecol. 13(4), 167–171 (2016)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dursun, M., Besiroglu, H., Tellioglu, E. et al. Association Between Sexual Dysfunction, Sleep Impairment and Depression in Women with Fibromyalgia. Sex Disabil 38, 261–269 (2020). https://doi.org/10.1007/s11195-019-09592-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11195-019-09592-5