Abstract
Hyperkalemia is a frequent clinical abnormality in patients with chronic kidney disease, and it is associated with higher risk of mortality and malignant arrhythmias. Severe hyperkalemia is a medical emergency, which requires immediate therapies, followed by interventions aimed at preventing its recurrence. Current treatment paradigms for chronic hyperkalemia management are focused on eliminating predisposing factors, such as high potassium intake in diets or supplements, and the use of medications known to raise potassium level. Among the latter, inhibitors of the renin-angiotensin aldosterone system are some of the most commonly involved medications, and their discontinuation is often the first step taken by clinicians to prevent the recurrence of hyperkalemia. While this strategy is usually successful, it also deprives patients of the recognized benefits of this class, such as their renoprotective effects. The development of novel potassium binders has ushered in a new era of hyperkalemia management, with a focus on chronic therapy while maintaining the use of beneficial, but hyperkalemia-inducing medications such as renin-angiotensin aldosterone system inhibitors. This review article examines the incidence and clinical consequences of hyperkalemia, and its various treatment options, with special emphasis on novel therapeutic agents and the potential benefits of their application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hyperkalemia is common in patients with chronic kidney disease (CKD) and end stage renal disease (ESRD), due to the central role the kidneys play in maintaining normal potassium homeostasis. Hyperkalemia can induce or worsen cardiac arrhythmias, and it is associated with significantly increased mortality [1–4]. Besides CKD, the most common risk factors for hyperkalemia include clinical conditions such as acute kidney injury (AKI), cardiovascular disease (CVD), or diabetes mellitus (DM), and also various medications commonly used in patients with CKD [5]. The medications most commonly associated with hyperkalemia are the inhibitors of the renin-angiotensin-aldosterone system (RAASi), and hyperkalemia is one of the main reasons why they have to be discontinued in many patients with CKD, in spite of their recognized benefits in this population. This review examines the incidence of hyperkalemia, its clinical consequences and its various treatments, with a focus on novel pharmacologic agents which could be used for improved chronic management of hyperkalemia, and which hold promise to result in improved clinical outcomes.
1.1 Incidence and risk factors of hyperkalemia
Elevated serum potassium is rarely detected in the general population. In a Canadian study only 2.6 % of emergency room visits and 3.5 % of hospital admissions were associated with hyperkalemia, in a population which included 10 % of patients with CKD [6]; with similar incidences of 3.2 % [7] and 2.6 % [8] reported in two US studies. Since hyperkalemia is a transient condition, and there are no prospective studies of intra-individual frequent longitudinal monitoring of serum potassium, the true incidence of hyperkalemia remains unknown, and could be higher. The sensitivity of the ICD-10 diagnosis for hyperkalemia was found to be extremely low (14.6 %) [6], underscoring the challenge of identifying this condition from retrospective administrative databases without laboratory measurements.
CKD is the single most important condition predisposing to hyperkalemia, with both decreased GFR (lower clearance) and the presence of tubulointerstitial dysfunction (lower tubular secretion) contributing to an abnormal potassium homeostasis. Under steady state conditions the capacity of the kidneys to maintain eukalemia in the face of gradually worsening kidney function is remarkable, but their ability to handle acutely increased potassium loads diminishes [9]. There is not a single GFR inflection point for increased risk of hyperkalemia; instead, the risk of hyperkalemia increases linearly as GFR decreases with advancing CKD [8].
Besides a low GFR, patients with CKD often have characteristics which conspire with low clearance to induce an elevated serum potassium level (Fig. 1). The variable combination of predisposing factors, and the variable definitions used for hyperkalemia explains why the incidence of hyperkalemia in patients with CKD has varied widely, ranging from as low as 7.7 % to as high as 73 % [3, 7, 10, 11]. In terms of mechanism of action, the predisposing factors for hyperkalemia in CKD involve increased potassium intake/load, abnormal cellular redistribution, worsening of the already decreased ability to excrete potassium, or often a combination of these. Patients with CKD are often instructed to consume a low sodium diet. Such heart-healthy diets contain much more potassium, a generally beneficial feature in patients with normal kidney function, but a risk factor for hyperkalemia in those with CKD. Furthermore, the prohibition of table salt is often compensated by some patients by the addition of salt substitutes without the realization of their high potassium content. Other conditions resulting in an acute potassium load in CKD could include acute conditions with tissue breakdown (e.g. rhabdomyolysis), gastrointestinal bleeding or blood transfusion using outdated blood [12]. Metabolic acidosis is another condition that could occur in the context of CKD, and facilitate the shift of potassium from the intracellular to the extracellular space [13]. These conditions often occur in the context of acute kidney injury superimposed on CKD, which further lowers the kidneys’ ability to excrete potassium, and which often results in the rapid development of severe and life-threatening hyperkalemia. Kidney transplants can have normal or decreased GFR, and can result in hyperkalemia through specific mechanisms including the use of anti-rejection medications [14].
Mechanisms of action of the development of hyperkalemia in patients with chronic kidney disease and associated comorbid conditions. AKI, acute kidney injury; CKD, chronic kidney disease; CVD, cardiovascular disease; DM, diabetes mellitus; GFR, glomerular filtration rate; RAAS, renin-angiotensin-aldosterone system. Reprinted with permission from Kovesdy CP, Am J Med 128:1281–1287, 2015 [60]
Two other major comorbidities that directly or indirectly cause hyperkalemia are diabetes mellitus and cardiovascular disease (Fig. 1). These conditions often cluster with CKD, and hence their concomitant presence contributes to the higher incidence of hyperkalemia seen in this patient population. Type II diabetes is characterized by insulin deficiency, and uncontrolled diabetes results in hypertonicity; both of these conditions can lead to a diminished ability to shift potassium to the intracellular space [15]. Furthermore, diabetes mellitus can be associated with hyporeninemic hypoaldosteronism, resulting in decreased tubular potassium secretion [16, 17].
Cardiovascular disease includes disease states such as acute myocardial infarction, left ventricular hypertrophy and congestive heart failure. Besides a direct pathophysiologic effect on potassium homeostasis (e.g. decreased tubular sodium flow in CHF), these conditions require numerous therapeutic interventions which are proven to improve outcomes in these patients; yet they also induce or worsen hyperkalemia (Fig. 1). The use of these medication classes has become one of the major causes of hyperkalemia in clinical practice, and has resulted in a therapeutic conundrum because of the uncertain risk-benefit ratio once hyperkalemia ensues as a result of their application. Among the relevant cardiovascular medications beta-2 receptor blockers inhibit renin production and hampers potassium redistribution to the intracellular space [18]; heparin inhibits aldosterone production [19]; and digitalis glycosides block Na-K-ATPase and hence impair collecting duct potassium secretion [20]. Notwithstanding these pathophysiologic links, the independent practical significance of these drug classes for hyperkalemia is limited, as the magnitude of the increase in serum potassium attributable to them is typically in ~0.2–0.5 mEq/l [21, 22]. A much more practically relevant class of drugs involved in hyperkalemia are the RAASi, e.g. angiotensin converting enzyme inhibitors, angiotensin receptor blockers, direct renin inhibitors and mineralocorticoid receptor antagonists [7]. Hyperkalemia attributable to these medications is uncommon in patients without CKD (typically <2 %), but the incidence increases to 5 % with dual RAASi therapy, and rises to up to 10 % in patients with CKD. [5, 23–26] Interestingly, RAASi therapy can lead to hyperkalemia even in anuric dialysis patients [27], probably because of inhibition of gastrointestinal potassium secretion. Hyperkalemia has become a thorn in the side of Cardiologists, Endocrinologists and Nephrologists, as it is one of the main reasons why patients with strong medical indications for RAASi cannot tolerate this therapy. The discontinuation rate of RAASi for reasons such as hyperkalemia in early clinical trials was low (1.2–1.6 %23), and contributed to the marked increase in the prescription of these agents to patients with CKD in the wake of trials showing benefits associated with them. The deceptive nature of the low discontinuation rate of RAASi in trials that enrolled select groups of patients who were at low risk of hyperkalemia became evident once a marked increase in hyperkalemia incidence was reported after the publication of some landmark clinical trials, which also showed an increase in hyperkalemia-related morbidity and mortality [28]. Furthermore, the intolerance of RAASi appears to be much higher among patients at high risk for hyperkalemia such as unselect CKD populations. Among patients included in a recent large cohort study of >650,000 patients with prevalent CKD, only 8 % of patients newly started on a RAASi remained on this treatment for the entire duration of their follow-up, with 66 % receiving it during >50 % of their follow-up [29]. Since RAASi are essentially the only medication class with proven renoprotective properties independent of their blood pressure lowering effects, the inability of their clinical use due to hyperkalemia has become a serious therapeutic barrier in patients with CKD.
1.2 Outcomes associated with hyperkalemia
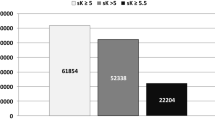
Serum potassium concentration, and the balance of between intra- and extracellular potassium concentration plays an important role in normal cell membrane electrophysiology. Hyperkalemia therefore results in electrophysiologic perturbations, with the most important effect on cardiac electrophysiology, including a decrease in myocardial resting membrane potential, increased cardiac depolarization, myocardial excitability, cardiac instability and conduction system abnormalities, which ultimately lead to arrhythmias progressing to ventricular fibrillation and asystole [30, 31]. It is thus not surprising that elevated serum potassium concentrations have been associated with higher mortality rates in numerous observational studies, irrespective of the clinical characteristics of the studied population. The typical pattern is that of a U-shaped association, with both high and low serum potassium concentrations associated with higher mortality (Fig. 2). Such a U-shaped association was present in patients without CKD hospitalized with acute myocardial infarction (ideal serum potassium ~4 mEq/l) [32], and in patients with non-dialysis dependent CKD [3, 33], and those receiving chronic hemodialysis (ideal serum potassium ~4.0–4.5 mEq/l) [1, 2, 4]. Importantly, many of these observational studies have examined long term all-cause mortality, whereas the putative pathophysiology of hyperkalemia suggests that adverse effects would be exerted immediately or shortly after the development of the abnormality, and would manifest itself primarily as malignant arrhythmias and sudden cardiac death [34–36]. Supporting this hypothesis, a study performed in patients receiving peritoneal dialysis reported an association between hyperkalemia with increased 1-year mortality, but not with longer-term mortality [37]. More direct evidence was provided by the above mentioned study in hospitalized patients with myocardial infarction, who experienced higher risk of ventricular fibrillation associated with serum potassium levels >5.0 mEq/l [32], and by a study of 245,808 hospitalized US veterans describing significantly increased 1-day mortality associated with serum potassium levels >5.5 mEq/l [7]. The latter study also reported that the risk associated with comparable levels of hyperkalemia was substantially higher in individuals with normal kidney function compared to those with increasingly severe CKD (odds ratios for serum potassium >6.0 vs. <5.5 mEq/l in those with normal eGFR and CKD stages 3, 4 and 5: 31.64, 19.52, 11.56 and 8.02, respectively). The reason for the seemingly lesser risk in patients with more advanced CKD is unclear, but may be due to the higher activation of adaptive mechanisms in individuals who are exposed to more frequent episodes of hyperkalemia.
Association of serum potassium level with all-cause mortality. Reprinted with permission from Hayes J et al., Nephron Clin Pract 120:c8–16, 2012 [3]
1.3 Treatment of hyperkalemia
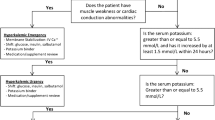
Severe hyperkalemia (variably defined, but typically representing serum potassium >6.0–6.5 mEq/l) is regarded as a clinical emergency, mandating cardiac monitoring in a controlled setting and immediate medical interventions. A detailed review of the various treatments applied in the context of acute management of hyperkalemia [5] is beyond the scope of this review. Once a patient is diagnosed with clinically relevant hyperkalemia, and once this is acutely treated, the goal becomes to prevent the future development of recurrent hyperkalemia. To this effect, our current paradigm is centered on identifying and eliminating the risk factors of hyperkalemia. Most often the first action consist of eliminating modifiable causes, e.g. lowering dietary potassium intake, correcting metabolic acidosis, and/or discontinuing or lowering the dose of hyperkalemia-inducing medications [11]. As discussed above, some of these measures involve therapeutic compromises, in that the cessation of a heart-healthy diet or a RAASi deprives patients of their beneficial cardiovascular effects. Therefore, an ideal approach would favor alternative interventions to allow the continuation of beneficial cardiovascular interventions while correcting hyperkalemia, e.g. the use of diuretics and correction of metabolic acidosis. However, the latter may not be feasible (e.g. in volume depleted patients, or those with no metabolic acidosis) or may not be effective enough, in which case the next step would involve treatment with a potassium binding agent.
1.4 Use of potassium binders for chronic management of hyperkalemia: Something old, something new
For over 50 years the only potassium binder that was available in the US was sodium-polystyrene sulfonate (with calcium-polystyrene sulfonate available in some other countries), and it was mainly used in the context of acute hyperkalemia [38]. The approval of sodium-polystyrene sulfonate in 1961 for treatment of hyperkalemia was based on a clinical trial involving 32 azotemic patients, and showing a significant decrease of 0.9 mEq/l in serum potassium over 24 h [39]. A clinical trial of this size and duration would hardly be deemed fit to serve as the basis of a clinical indication in today’s day and age; but the lack of alternative methods to treat hyperkalemia (dialysis was not yet available, and there were no other medications of similar scope) meant that sodium-polystyrene sulfonate became widely used in clinical practice. The efficacy of sodium polystyrene sulfonate as an acute intervention for hyperkalemia has also been shown in a small retrospective analysis of 154 hyperkalemic patients with mean serum potassium of 5.9 mEq/l, in whom serum potassium decreased by 0.7–1.1 mEq/l in response to the binder therapy [38]. N.B., while sodium polystyrene sulfonate is used as an acute intervention, it should not be considered an emergency intervention, as its onset of action is after several hours following oral administration [40]; hence it should only be used in emergency situations in conjunction with other interventions with shorter onset of action.
The use of sodium polystyrene sulfonate as a chronic intervention for hyperkalemia has never been approved, although off label application in everyday clinical practice is probably common. In an observational study of 14 patients treated with sodium polystyrene sulfonate daily, hyperkalemia was successfully corrected and controlled [41]. Notwithstanding the lack of larger clinical trials, the effectiveness of sodium polystyrene sulfonate towards hyperkalemia management is in general accepted among clinicians, even though the proportional effects of the resin itself vs. the sorbitol used to alleviate its constipating effects [42] continue to be debated [43–46]. What is sorely missing is the systematic evaluation of its safety, due to the lack of clinical trial data providing long term prospective monitoring and recording of adverse events while using the drug. Concerns about the safety of sodium polystyrene sulfonate were raised by case reports describing severe upper and lower gastrointestinal injuries following its administration [47, 48], with 62 % of the colonic injuries exhibiting transmural necrosis and a mortality rate of 33 % [49]. In a systematic evaluation examining patients receiving sodium polystyrene sulfonate, the incidence of colonic necrosis was 0.3 % overall, but higher (1.8 %) in post-surgical patients [50]. A similarly low incidence of colonic necrosis was described in another retrospective cohort (0.14 %, vs. 0.07 % in those not exposed to this drug) [51]. Notwithstanding the relative rarity of these severe injuries, the absolute number of patients affected is not trivial, due to the frequency with which sodium polystyrene sulfonate continues to be used [38]. Following a black box warning by the US Food and Drug Administration (FDA) the mixture of sodium-polystyrene sulfonate with 70 % sorbitol has been banned [52], but versions without sorbitol or with sorbitol added at a 33 % concentration remain in use.
1.4.1 Novel potassium binders
Insufficient data about the efficacy and safety of sodium-polystyrene sulfonate, the lack of an indication for its use in chronic hyperkalemia management, and the poor tolerance of this medication has led to the development of two new potassium binders for chronic hyperkalemia therapy. Patiromer (Veltassa®) is a non-absorbable polymer which exchanges potassium with calcium, and which was recently approved by the FDA for treatment of hyperkalemia. The randomized controlled clinical trials which tested the efficacy and safety of patiromer have enrolled in excess of 500 patients total, and have shown that elevated serum potassium levels were lowered effectively and normokalemia was achieved over extended periods of time (up to 52 weeks) even while RAASi therapy was maintained [53–56]. The mean decrease in serum potassium with patiromer in the different studies was ~0.5–1 mEq/l (with larger decreases seen in patients with higher starting serum potassium levels). The most common adverse events associated with patiromer administration were constipation, hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. Serious adverse events were rare, and the rare observed fatalities were reportedly unrelated to patiromer use.
The second new potassium binder still under development is sodium zirconium cyclosilicate (ZS-9), a selective cation which exchanges potassium for sodium and hydrogen. The efficacy and safety of zirconium cyclosilicate has been tested in randomized controlled clinical trials which enrolled in excess of 1000 patients total [57, 58]. In these clinical trials zirconium cyclosilicate lowered elevated serum potassium acutely by 0.5–1 mEq/l in a dose dependent manner, with more substantial decrease seen in patients with higher starting potassium levels. Normokalemia was maintained on zirconium cyclosilicate during chronic administration over up 28 days, even in patients treated with RAASi. Adverse events reported in these trials included edema, and hypokalemia, both seen mostly in patients taking higher doses of the drug.
In summary, both patiromer and zirconium cyclosilicate appear to be effective and safe treatments of hyperkalemia, and seem to control serum potassium levels over extended periods of time even when patients are maintained on RAASi therapy. Patiromer is already approved for clinical use; remaining concerns include a boxed warning in the FDA label that it cannot be administered concomitantly with other drugs, and hypothetical questions about its long term safety. Patiromer exchanges potassium for calcium, hence its effects on soft tissue and vascular calcification in patients with advanced CKD may be of concern when used over longer periods of time. Zirconium cyclosilicate’s approval by the FDA was delayed by concerns regarding manufacturing processes, and to date it remains unclear when an approval will be granted. Based on analysis of available evidence from completed clinical trials (new ones were not requested by the FDA) concerns for zirconium cyclosilicate’s long term use relate to sodium absorption and edema, which could pose a problem in patients with CHF or advanced CKD.
Assuming no major safety problems with ongoing long term use of the novel potassium binders, an intriguing question will be their clinical impact. Currently available data focuses on efficacy and safety in the context of correcting a biochemical end point (hyperkalemia). Their effects on clinical outcomes such as hospitalizations, cardiac arrhythmias, or other cardiovascular events remains unknown. Preemption of hyperkalemia could plausibly improve clinical outcomes especially in patient groups that are prone to arrhythmias (e.g. patients with pre-existing cardiovascular disease, or patients with advanced CKD and ESRD), but this would have to be proven in properly powered clinical trials.
2 Conclusions
The evidence from observational studies regarding the higher risk of mortality and arrhythmias associated with hyperkalemia is convincing; yet it remains uncertain whether or not the correction of hyperkalemia can result in better clinical outcomes. Hypothetically, the prevention and/or correction of hyperkalemia could be beneficial by preventing malignant arrhythmias, but this would have to be proven in prospective, randomized, controlled clinical trials. Furthermore, the manner by which hyperkalemia is controlled may also be important. One of the most common interventions used to address an elevated serum potassium is the discontinuation of exacerbating factors such as hyperkalemia-inducing medications. Some of these are agents that have proven independent benefits, such as RAASi. It remains unclear if being on a RAASi, or normokalemia provides better comparative outcomes in patients with CKD. Ideally one should prefer the achievement of both, and hence therapeutic interventions that control hyperkalemia without the discontinuation of hyperkalemia-inducing but otherwise beneficial interventions (which include not only medications such as RAASi, but also heart-healthy diets [59]) may offer additional benefits. The advent of new potassium-lowering medications may result in a change in our therapeutic paradigm, by favoring the chronic use of a binder medication over the discontinuation of RAASi therapy or restriction of dietary potassium. Future studies should continue to scrutinize the effects of such a novel strategy on long term clinical outcomes.
Reference
Lowrie EG, Lew NL. Death risk in hemodialysis patients: The predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am J Kidney Dis. 1990;15:458–82.
Iseki K, Uehara H, Nishime K, Tokuyama K, Yoshihara K, Kinjo K, Shiohira Y, Fukiyama K. Impact of the initial levels of laboratory variables on survival in chronic dialysis patients. Am J Kidney Dis. 1996;28:541–8.
Hayes J, Kalantar-Zadeh K, Lu JL, Turban S, Anderson JE, Kovesdy CP. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: The role of race. Nephron Clin Pract. 2012;120:c8–16.
Kovesdy CP, Regidor DL, Mehrotra R, Jing J, McAllister CJ, Greenland S, Kopple JD, Kalantar-Zadeh K. Serum and dialysate potassium concentrations and survival in hemodialysis patients. Clin J Am Soc Nephrol. 2007;2:999–1007.
Kovesdy CP. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014;10:653–62.
Fleet JL, Shariff SZ, Gandhi S, Weir MA, Jain AK, Garg AX. Validity of the international classification of diseases 10th revision code for hyperkalaemia in elderly patients at presentation to an emergency department and at hospital admission. BMJ Open. 2012;2.
Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, Weir MR, Fink JC. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169:1156–62.
Drawz PE, Babineau DC, Rahman M. Metabolic complications in elderly adults with chronic kidney disease. J Am Geriatr Soc. 2012;60:310–5.
Bourgoignie JJ, Kaplan M, Pincus J, Gavellas G, Rabinovitch A. Renal handling of potassium in dogs with chronic renal insufficiency. Kidney Int. 1981;20:482–90.
Sarafidis PA, Blacklock R, Wood E, Rumjon A, Simmonds S, Fletcher-Rogers J, Ariyanayagam R, Al-Yassin A, Sharpe C, Vinen K. Prevalence and factors associated with hyperkalemia in predialysis patients followed in a low-clearance clinic. Clin J Am Soc Nephrol. 2012;7:1234–41.
Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med. 2004;351:585–92.
Michael JM, Dorner I, Bruns D, Ladenson JH, Sherman LA. Potassium load in CPD-preserved whole blood and two types of packed red blood cells. Transfusion. 1975;15:144–9.
Simmons DH, Avedon M. Acid-base alterations and plasma potassium concentration. Am J Phys. 1959;197:319–26.
DeFronzo RA, Goldberg M, Cooke CR, Barker C, Grossman RA, Agus ZS. Investigations into the mechanisms of hyperkalemia following renal transplantation. Kidney Int. 1977;11:357–65.
DeFronzo RA, Sherwin RS, Felig P, Bia M. Nonuremic diabetic hyperkalemia. Possible role of insulin deficiency. Arch Intern Med. 1977;137:842–3.
Glassock RJ, Goldstein DA, Goldstone R, Hsueh WA. Diabetes mellitus, moderate renal insufficiency and hyperkalemia. Am J Nephrol. 1983;3:233–40.
Tuck ML, Sambhi MP, Levin L. Hyporeninemic hypoaldosteronism in diabetes mellitus. Studies of the autonomic nervous system's control of renin release. Diabetes. 1979;28:237–41.
Arrizabalaga P, Montoliu J, Martinez VA, Andreu L, Lopez PJ, Revert L. Increase in serum potassium caused by beta-2 adrenergic blockade in terminal renal failure: Absence of mediation by insulin or aldosterone. Proc Eur Dial Transplant Assoc. 1983;20:572–6.
Edes TE, Sunderrajan EV. Heparin-induced hyperkalemia. Arch Intern Med. 1985;145:1070–2.
Bismuth C, Gaultier M, Conso F, Efthymiou ML. Hyperkalemia in acute digitalis poisoning: Prognostic significance and therapeutic implications. Clin Toxicol. 1973;6:153–62.
Buhler FR, Burkart F, Lutold BE, Kung M, Marbet G, Pfisterer M. Antihypertensive beta blocking action as related to renin and age: A pharmacologic tool to identify pathogenetic mechanisms in essential hypertension. Am J Cardiol. 1975;36:653–69.
Pedersen EB, Kornerup HJ. Relationship between plasma aldosterone concentration and plasma potassium in patients with essential hypertension during alprenolol treatment. Acta Med Scand. 1976;200:263–7.
Bakris GL, Siomos M, Richardson D, Janssen I, Bolton WK, Hebert L, Agarwal R, Catanzaro D. ACE inhibition or angiotensin receptor blockade: Impact on potassium in renal failure. VAL-K study group. Kidney Int. 2000;58:2084–92.
Weir MR, Rolfe M. Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin J Am Soc Nephrol. 2010;5:531–48.
Makani H, Bangalore S, Desouza KA, Shah A, Messerli FH. Efficacy and safety of dual blockade of the renin-angiotensin system: Meta-analysis of randomised trials. BMJ. 2013;346:f360.
Susantitaphong P, Sewaralthahab K, Balk EM, Eiam-ong S, Madias NE, Jaber BL. Efficacy and safety of combined vs. single renin-angiotensin-aldosterone system blockade in chronic kidney disease: A meta-analysis. Am J Hypertens. 2013;26:424–41.
Knoll GA, Sahgal A, Nair RC, Graham J, Van WC, Burns KD. Renin-angiotensin system blockade and the risk of hyperkalemia in chronic hemodialysis patients. Am J Med. 2002;112:110–4.
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA. Rates of hyperkalemia after publication of the randomized Aldactone evaluation study. N Engl J Med. 2004;351:543–51.
Molnar MZ, Kalantar-Zadeh K, Lott EH, Lu JL, Malakauskas SM, Ma JZ, Quarles DL, Kovesdy CP: ACE Inhibitor and Angiotensin Receptor Blocker Use and Mortality in Patients with Chronic Kidney Disease. J Am Coll Cardiol 2013.
Dittrich KL, Walls RM. Hyperkalemia: ECG manifestations and clinical considerations. J Emerg Med. 1986;4:449–55.
Parham WA, Mehdirad AA, Biermann KM, Fredman CS. Hyperkalemia revisited. Tex Heart Inst J. 2006;33:40–7.
Goyal A, Spertus JA, Gosch K, Venkitachalam L, Jones PG, Van den Berghe G, Kosiborod M. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307:157–64.
Korgaonkar S, Tilea A, Gillespie BW, Kiser M, Eisele G, Finkelstein F, Kotanko P, Pitt B, Saran R. Serum potassium and outcomes in CKD: insights from the RRI-CKD cohort study. Clin J Am Soc Nephrol. 2010;5:762–9.
Epstein FH. Signs and symptoms of electrolyte disorders. In: Maxwell MH, Kleeman CR, editors. Clinical disorders of fluid and electrolyte metabolism. 3rd ed. New York: McGraw-Hill; 1980. p. 499–516.
Fisch C. Electrolytes and the heart. In: Hurst JW, editor. The heart. New York: McGraw-Hill; 1982. p. 1599.
Kleeman K, Singh BN. Serum electrolytes and the heart. In: Maxwell MH, Kleeman CR, editors. Clinical disorders of fluid and electrolyte metabolism. 3rd ed. New York: McGraw-Hill; 1980. p. 145–80.
Xu Q, Xu F, Fan L, Xiong L, Li H, Cao S, Lin X, Zheng Z, Yu X, Mao H. Serum potassium levels and its variability in incident peritoneal dialysis patients: Associations with mortality. PLoS One. 2014;9:e86750.
Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. Am J Med Sci. 2014;347:93–100.
Scherr L, Ogden DA, Mead AW, Spritz N, Rubin AL. Management of hyperkalemia with a cation-exchange resin. N Engl J Med. 1961;264:115–9.
Emmett M, Hootkins RE, Fine KD, Santa Ana CA, Porter JL, Fordtran JS. Effect of three laxatives and a cation exchange resin on fecal sodium and potassium excretion. Gastroenterology. 1995;108:752–60.
Chernin G, Gal-Oz A, Ben-Assa E, Schwartz IF, Weinstein T, Schwartz D, Silverberg DS. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35:32–6.
Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol; a preliminary report. N Engl J Med. 1961;264:111–5.
Kamel KS, Wei C. Controversial issues in the treatment of hyperkalaemia. Nephrol Dial Transplant. 2003;18:2215–8.
Kamel KS, Schreiber M. Asking the question again: Are cation exchange resins effective for the treatment of hyperkalemia? Nephrol Dial Transplant. 2012;27:4294–7.
Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: Are they safe and effective? J Am Soc Nephrol. 2010;21:733–5.
Gruy-Kapral C, Emmett M, Santa Ana CA, Porter JL, Fordtran JS, Fine KD. Effect of single dose resin-cathartic therapy on serum potassium concentration in patients with end-stage renal disease. J Am Soc Nephrol. 1998;9:1924–30.
Chelcun JL, Sable RA, Friedman K. Colonic ulceration in a patient with renal disease and hyperkalemia. JAAPA. 2012;25:34 .37-34, 38
Gorospe EC, Lewis JT, Bruining DH. Kayexalate-induced esophageal ulcer in a patient with gastroparesis. Clin Gastroenterol Hepatol. 2012;10:A28.
Harel Z, Harel S, Shah PS, Wald R, Perl J, Bell CM. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: A systematic review. Am J Med. 2013;126:264–24.
Gerstman BB, Kirkman R, Platt R. Intestinal necrosis associated with postoperative orally administered sodium polystyrene sulfonate in sorbitol. Am J Kidney Dis. 1992;20:159–61.
Watson MA, Baker TP, Nguyen A, Sebastianelli ME, Stewart HL, Oliver DK, Abbott KC, Yuan CM. Association of prescription of oral sodium polystyrene sulfonate with sorbitol in an inpatient setting with colonic necrosis: A retrospective cohort study. Am J Kidney Dis. 2012;60:409–16.
US Food and Drug Administration: Kayexalate (sodium polystyrene sulfonate) powder. Safety labeling changes approved by FDA Center for Drug Evaluation and Research (CDER)-September 2009. Available at http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed 30 July 2016.
Pitt B, Anker SD, Bushinsky DA, Kitzman DW, Zannad F, Huang IZ. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32:820–8.
Buysse JM, Huang IZ, Pitt B. PEARL-HF: Prevention of hyperkalemia in patients with heart failure using a novel polymeric potassium binder, RLY5016. Futur Cardiol. 2012;8:17–28.
Weir MR, Bakris GL, Bushinsky DA, Mayo MR, Garza D, Stasiv Y, Wittes J, Christ-Schmidt H, Berman L, Pitt B. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med. 2015;372:211–21.
Bakris GL, Pitt B, Weir MR, Freeman MW, Mayo MR, Garza D, Stasiv Y, Zawadzki R, Berman L, Bushinsky DA. Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease: The AMETHYST-DN randomized clinical trial. JAMA. 2015;314:151–61.
Packham DK, Rasmussen HS, Lavin PT, El-Shahawy MA, Roger SD, Block G, Qunibi W, Pergola P, Singh B. Sodium zirconium cyclosilicate in hyperkalemia. N Engl J Med. 2015;372:222–31.
Kosiborod M, Rasmussen HS, Lavin P, Qunibi WY, Spinowitz B, Packham D, Roger SD, Yang A, Lerma E, Singh B. Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia: The HARMONIZE randomized clinical trial. JAMA. 2014;312:2223–33.
Palmer BF, Clegg DJ. Achieving the benefits of a high-potassium, Paleolithic diet, without the toxicity. Mayo Clin Proc. 2016;91:496–508.
Kovesdy CP. Management of Hyperkalemia: An update for the internist. Am J Med. 2015;128:1281–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Dr. Kovesdy is an employee of the US Department of Veterans Affairs. Opinions expressed in this paper are those of the author’s and do not represent the opinion of the US Department of Veterans Affairs.
Conflicts of interest
Dr. Kovesdy received consultant fees from Relypsa (manufacturer of Patiromer) and ZS Pharma (manufacturer of zirconium cyclosilicate).
Rights and permissions
About this article
Cite this article
Kovesdy, C.P. Updates in hyperkalemia: Outcomes and therapeutic strategies. Rev Endocr Metab Disord 18, 41–47 (2017). https://doi.org/10.1007/s11154-016-9384-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-016-9384-x