Abstract
Acromegaly is characterized by sustained elevation of circulating growth hormone (GH) and insulin-like growth factor I (IGF-I), and is clearly associated with increased morbidity and overall mortality mainly due to cardiovascular, metabolic, and respiratory diseases. Although cancer-related mortality varies widely amongst retroperspective studies, it appears to be consistently elevated mainly in patients with uncontrolled disease. We review individual tumor types including neoplasms of the colon, breast, prostate, and thyroid where in vitro, animal studies, and studies in non-acromegalic cancer patients have established a role for the GH/IGF-I axis in tumor progression and possibly initiation. We highlight deficiencies in data in acromegalic patients where the evidence is less convincing. Instead, we explore the hypothesis that acromegaly, independent of hormone secretion, is a disease that heralds genetic and/or epigenetic alterations predisposing to cancer risk elsewhere.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Cancer mortality in acromegalic patients
Retroperspective studies focusing on mortality in acromegaly have shown that 9–50% of deaths in acromegalic patients are attributable to cancer related complications (average 24% in 5,024 patients with acromegaly) (Table 1). While earlier studies by Wright et al. [1], Alexander et al. [2], Nabarro [3], Bengtsson et al. [4], and Etxabe et al. [5] demonstrated a 2–3 fold increased overall mortality for acromegalic patients, cancer related mortality rates were either not increased [6] or increased only in females (2–3 fold, [1, 3, 4] or in males (5–7 fold, [2, 5]. If the cancer entities were documented, they covered a wide array of different malignancies but cancers of the breast, colon, prostrate, and hematological system were the most frequent types. Most of the subsequent studies focusing on mortality analyzed overall rates in comparison to sex-and age-matched population based on historical controls. It is important to note that more recent studies examined mortality rates in relationship to post-treatment growth hormone (GH) and /or insulin-like growth factor I (IGF-I) levels. Such studies were able to demonstrate that mortality rates were comparable to population-based controls if post-treatment GH levels (either nadir or random) were below threshold cut-offs suggestive of “cure” or “in-remission” and were elevated in patients with persistent disease [7–14]. At least two studies also found a correlation between post treatment IGF-I levels and mortality rates [9, 13] while two others [12, 14] did not detect an effect of IGF-I levels on outcome. The authors of these studies suggest that increased mortality risk in acromegalic patients is restricted mainly to those with elevated post-treatment GH levels. It is of interest to note that the largest cohort of patients studied by Orme et al. [10] as well as those studied by Holdaway et al. [13] demonstrated increased mortality rates for all cancers only in acromegalic patients with higher post-treatment GH levels while cancer-related mortality for all acromegalic patients regardless of treatment outcome was not increased compared to population controls. Orme found a 1.8 fold increased mortality risk of all cancers, a 4.6 fold increased mortality risk of colon cancer and a 2.9 fold increased mortality risk of breast cancer if random serum GH levels were higher than 10 ng/ml. On the other hand there was no significant relationship between duration of acromegaly and cancer related mortality in these patients.
It should also be noted that many authors have argued that most deaths amongst acromegalic patients are attributable to cardiovascular disease (60%) followed by respiratory causes (25%). Correspondingly, analyses of mortality determinants in patients with persistently elevated GH levels show that hypertension and heart disease, and not cancer, are the strongest predictors of mortality [15, 16].
Cancer related mortality data, on the other hand, does not reflect cancer incidence or cancer morbidity. This along with the potential bias of cause of death reporting from autopsy examinations, we will argue that studies focusing on mortality are not likely to be helpful in answering the question of cancer risk.
2 Overall cancer incidence in acromegalic patients
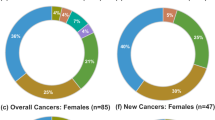
Unfortunately, studies focusing on cancer incidence or cancer prevalence in acromegaly do not provide conclusive evidence of increased cancer risk (Table 2). Most studies report a moderately (1.5 to 4-fold) increased relative risk for acromegalic patients to develop tumors, mainly of the colon/rectum, breast, prostate, thyroid, and hematological system [3–24] while other studies do not confirm increased tumor prevalence or incidence [6, 10].
The study by Mustacchi and Shimkin, for example, analyzing 223 patients treated for acromegaly from 1937 to 1955 [6] did not find an increased cancer incidence compared to population tumor incidence rates (13 vs. 10 malignancies, respectively). In 1982, Klein et al. [17] studied 44 patients and reported 11 cases of cancer 4 of which involved the colon. Although the observed rates were not compared to expected rates, the control group was comprised of 29 patients with chromophobic pituitary adenomas. Subsequently, Nabarro [3] reported in his personal series an increased cancer prevalence in women, mainly due to breast cancer (11 observed vs. 2.6 expected) while men showed no difference in cancer incidence rates. Brunner et al. [18] were able to demonstrate an increased risk only for colon cancer in 52 acromegalic patients compared to population tumor incidence rates (standardized incidence ratio, SIR, of 4.7 for colon cancer). Barzilay et al. [19], Cheung & Boyages [21], Popvich et al. [22], and Higuchi et al. [23] described an increased cancer incidence in their smaller series of acromegalic patients (with patient numbers varying between 44 and 220) compared to population tumor incidence rates (SIR 2.45, SIR 2.5, SIR 3.39, SIR3.53, respectively) but the statistical power of such studies has been questioned [10].
The studies by Ron et al. [20], Orme et al. [10], and Baris et al. [24], analyzed large retrospective epidemiological cohort data. Ron et al. reviewed hospital records of 1,041 acromegalic male patients admitted to the United States Veteran Affairs (VA) hospitals and after excluding 87 patients with a diagnosis of cancer prior to the diagnosis of acromegaly documented 116 cases of cancers (including 13 colon cancers) and an increased tumor incidence compared to tumor incidence rates from 3.7 million first admissions to VA hospitals (SIR 1.6, SIR for colon cancer 3.08). This study was criticized for the inclusion of 27 cases of pituitary tumors as cancer manifestations; also, the prevalence of acromegaly greatly out-numbered that in the general population. Instead of using population tumor incidence rates to calculate the expected numbers of tumors the authors utilized non-acromegalic hospitalized patients as controls.
The important study by Orme et al. analyzed a large cohort of 1,239 acromegalic patients, yielding 16,778 person-years at risk. After excluding 16 patients with the diagnosis of cancer before the diagnosis of acromegaly 79 cancers were observed in the patient group while 104 were expected from calculations utilizing data from the national cancer register for England and Wales (SIR 0.76). Nevertheless, sub-analysis of the incidence of different tumor types revealed a non-significant increased incidence of colon cancers in acromegalic patients (SIR 1.68).
Baris et al., on the other hand, found an increased risk for all cancers in 1,634 patients from Sweden and Denmark compared to population tumor incidence rates (SIR 1.5). Risks were increased for all gastroenteropancreatic (GEP) cancers (as wells as colon and rectum separately), kidney cancers, thyroid, and breast in females while prostate cancer was not significantly increased [24].
Epidemiologic analyses of cancer incidence/prevalence and cancer mortality in patients with acromegaly is hampered by several factors. Acromegaly is a rarely diagnosed disease with a reported prevalence of 40 to 90 cases per million population, which makes it difficult for a single center to gather sufficient numbers of patients for statistical analysis [25]; this may lead to biased reporting by specialized centers limiting generalization to the larger community. Secondly, as the main causes of death are cardiovascular and respiratory events, patients with uncontrolled acromegaly might succumb before developing recognizable cancer. Indeed, nearly 50% of patients in studies from the 1940s–1970s died before the age of 60 years. In this regard it remains to be shown conclusively if current standards will change cancer incidence in the acromegalic population.
Another important consideration is that acromegaly study patients were included in cancer incidence estimates only if they presented with an initial diagnosis of acromegaly. Patients presenting with a malignancy as the primary diagnosis have been traditionally excluded (see Table 2). In the case of the Orme et al. study 16 patients with cancer and subsequent diagnosis of acromegaly were excluded accounting for 17% of all cancer patients. Ron et al. excluded 87 patients with an initial diagnosis of a malignancy before diagnosis of acromegaly (49% of all patients with cancer). Although this exclusion is justified to evaluate the effects of increased GH and/or IGF-I levels on cancer development it may obscure the alternate hypothesis; namely that acromegaly and cancer share a common unifying non-endocrine etiology.
We conclude that the data generated from retrospective studies suggest an increased overall tumor incidence/prevalence in patients with acromegaly but additional prospective studies are required to resolve the significance of these observations.
2.1 Colorectal cancer
Colorectal tumors constitute the most frequent malignancy associated with acromegaly. The summary risk ratio for all colorectal cancer estimated from the three largest retrospective population-based studies by Ron et al. [20], Orme et al. [10], and Baris et al. [24] is 2.04 (95% CI: 1.32, 3.14) suggesting a modestly increased risk [26]. Prospective studies utilizing colonoscopy or flexible sigmoidoscopy with barium examination have been performed to evaluate the risk of colon polyps and colorectal cancer and are listed in Table 3. Most of these studies included only a small number of patients and the controls vary between in-house non-acromegalic patients, e.g. subjects with irritable bowel syndrome, and models generated from screening colonoscopy and/or autopsy studies. Three of the four larger studies including more than 100 acromegalic patients each demonstrate an increased risk of colon adenomas with an adenoma prevalence of 22 to 26% [27–29] while two of them show an increased risk for colon carcinoma with a prevalence of 4 to 5% [28, 29]. The study by Renehan et al. on the contrary, did not confirm either the increased prevalence of adenomas or carcinomas in acromegalic patients if compared to either literature data of 2,559 bowel examinations in autopsy studies or 810 bowel examinations performed in screening colonoscopy studies [30]. Overall, the data presented in colonoscopy studies are problematic mainly because of inadequate controls (e.g. autopsy studies tend to present a higher frequency of adenomas in the asymptomatic general population due to “optimal” examination conditions; predominance of males in some colonoscopy screening studies also leads to a higher incidence of adenomas/carcinomas in the general population; age and environmental influences are important factors which have not been e taken into account when comparing prevalence in acromegalic vs. controls). Therefore, the data suggesting an increased prevalence/incidence of colon adenomas in acromegalic patients have to be interpreted with caution. The available population-based data are more consistent. Renehan et al. [26] estimated in their meta-analysis that acromegaly is associated with a moderate (2-fold) increase in colorectal cancer risk. This estimate is increasingly accepted by other investigators and consensus working groups [15, 26, 31– 36].
There is furthermore evidence that colorectal neoplasia in acromegaly has different characteristics compared with that in the general population. Adenomatous lesions are more likely to be right sided (35 to 68% of the lesions) [27, 30, 34]; they tend to be larger and more dysplastic [28, 34, 35]; the adenomas are often multiple [27]. When resected there is a 25 to 41% chance of recurrence within 3 years and this seems to increase with higher GH/IGF-I levels [29, 36].
In patients with acromegaly the length of the colon and sigma is generally greater than in controls, and epithelial cells of sigmoid crypts present a slightly enhanced pattern of proliferation which is positively correlated to circulating IGF-I levels and an decreased apoptotic activity [30, 37, 38]. It has been speculated that GH/IGF-I excess in acromegaly increases epithelial cell proliferation and decreases apoptosis leading to greater susceptibility to accumulation of genetic defects resulting in colon cancer [16, 39]. Abnormalities in lymphocyte subset patterns in the colon mucosa of acromegalic patients and increased serum and intra-colonic unconjugated deoxycolic acids may represent an alternate pathophysiological mechanism of colonic neoplasia. The latter has been associated with the development of colon cancer in the general population and may also contribute to a tumor favorable environment in acromegalic patients [35, 40, 41].
2.1.1 The role of GH/IGF-I in tumor initiation and progression
Circumstantial evidence supporting a role of GH/IGF-I in the development of adenomas and cancers of the colon arises from cell and animal models and data in non-acromegalic patients with colon cancer.
The actions of GH are mediated by the GH receptor, which is ubiquitously expressed in colonic epithelium [42]. GH is mitogenic and anti-apoptotic in many tissues [43, 44], but there is relatively little data on its action in colonic tissue. Instead, IGF-I-based studies have demonstrated that both normal and tumoral colorectal cancer cell lines express the IGFI-R, and that IGF-I induces proliferation and anti-apoptotic activity in colorectal cancer cell lines [45–47].
Animal studies involving the over expression of GH or IGF-I distinguish two different murine phenotypes of hypersomatotropism [48, 49]. The selectively over expressed GH transgene is associated with both high GH and IGF-I levels while the IGF-I transgenic mouse has high IGF-I but low GH levels [48, 49]. Although both models exhibit biochemical and phenotypical features of acromegaly, the IGF-I transgenic mouse exhibits an increased bowel length with highly proliferative colonic crypt cells and decreased apoptosis, whereas no proliferative or apoptotic changes were present in the crypt cells of the GH transgenic model [48–51]. Intriguingly evidence to date suggests that IGF-I transgenic mice do not show an increased incidence of bowel cancer while GH transgenics do so [52]. A liver-specific gene-deletion of IGF-I results in reduced circulating IGF-I levels and a reduction in cancer growth and metastases in three cancer models, one for colon cancer and two for breast cancer [53]. Serum IGF-I concentrations vary between individuals across the general population, and it has been postulated that this may impact upon cancer risk [54]. A recent meta-analysis of a number of prospective studies on colon cancer risk has pooled the data and estimated a summary odds ratio of 1.58 (CI:1.11–2.27) for the association of the uppermost categories of serum IGF-I concentration compared to the lowermost categories [55].
In summary, there appears to be an increased prevalence of colorectal neoplasms in acromegaly where regular screening and polypectomy is advisable. Total colonoscopy should be performed as acromegalic patients more frequently develop cancers in the ascending and transverse colon. Predisposing features include multiple skin tags, a positive family history, increasing age, and persistently elevated GH and IGF-I levels [56].
Remaining questions include the age and frequency at which colonoscopy should be performed. As suggested by different authors we agree that colonoscopic screening is recommended to all newly diagnosed patients and that thereafter the American Cancer Society guidelines for patients with increased risk are applicable (colonoscopy every 5 years if no cancer or polyps are detected, with more frequent follow-up if any lesions are detected, depending on the number, size, and histologic features of the lesions) [33, 57–59]. While some have recommended even more intensive screening and follow-up programs [59], others have argued that acromegalic patients should not receive special screening or follow-up treatment as the modest increase in relative risk for colon cancer does not warrant special screening or surveillance measures. In fact guidelines for familial colorectal cancer screening suggest that colonoscopic surveillance is only warranted for a lifetime risk of 1 in 10 or greater [60, 61].
2.2 Breast cancer
Determining the incidence of breast cancer in women with acromegaly is even more difficult to ascertain than of other tumors as the restriction to the female sex nearly halves the number of patients at any single centre. Only one study by Nabarro [3] has reported a 4-fold higher risk for breast cancer, while subsequent studies failed to confirm a significantly increased incidence in patients with acromegaly [10, 24].
In contrast to that of colon cancer, in vitro data, animal studies, and epidemiologic studies in non-acromegalic patients have implicated the GH/IGF-I axis in the development of breast cancer. The GH-R is expressed in human mammary tumors (predominantly in the epithelial cell but also to some extent in the stromal cells) and human breast cancer cell lines [62]. The additional finding of GH protein expression in mammary tumors as well as normal tissue appears to suggest a possible autocrine/paracrine role for GH on tumor development and growth [63]. In line with this hypothesis, studies in MCF-7 mammary cancer cells have shown that blockade of GH-R by a specific GH antagonist abrogates cell proliferation [64].
The IGF-IR is also expressed on primary cultures of malignant breast epithelial cells as well as in several estrogen-dependent and, at lower levels, in estrogen-independent cell lines and IGF-I causes marked proliferation of breast cancer cells which can be inhibited by anti-IGFI-R antibody [65–67]. A paracrine as well as an autocrine IGF-I/IGF-IR loop has been demonstrated in stromal cell—breast cancer cell interactions and in breast cancer cell lines [68–70]. Early studies involving chronic administration of GH in female rats demonstrated an increased development of breast tumors over the long term [71]. In addition, transgenic mice over-expressing human GH [72] or IGF-I [73] have displayed an increased incidence of mammary tumors. Conversely, lit/lit mice with a defective GH-releasing hormone receptor and thus decreased GH/IGF-I levels show a significant growth inhibition of transplanted human breast cancer cells [74].
Furthermore, epidemiologic studies in non-acromegalic patients with breast carcinoma have suggested that these patients have significantly higher serum GH and IGF-I levels compared to individuals without carcinoma [75, 76] and that high IGF-I tertiles alone predict a 4.6 fold higher risk, and in combination with a low IGFBP3, a 7.3 fold higher risk for premenopausal but not postmenopausal breast cancer [77]. The meta-analysis by Renehan et al. [55] estimated a summary odds ratio of 1.93 (CI:1.38–2.69) for the association of the uppermost categories of serum IGF-I concentration compared to the lowermost categories in premenopausal breast cancer, but did not find an association between IGF-I levels and postmenopausal breast cancer. Unexpectedly, the authors found a positive association between IGFBP-3 and premenopausal breast cancer.
We conclude that until further studies are available to evaluate the true incidence, it is advisable to offer periodic mammography to women over the age of 50, as in the general population.
2.3 Prostate cancer
Even though acromegaly is associated with benign prostate hyperplasia as well as micro- and macro-calcifications regardless of age or gonadal status [78 79], the incidence of prostate cancer in patients with acromegaly is not significantly elevated and may even be reduced [10, 20 24]. It has been argued that this reduction may be seen because the disease is limited to elderly men and only recently men with acromegaly have survived long enough to participate in epidemiologic studies [80]. Again, in vitro, animal and non-acromegalic prostate cancer patient studies have implicated the involvement of the GH/IGF-I axis in prostate cancer.
Primary cultures of tumor prostate epithelial cells, as well as androgen sensitive and androgen insensitive prostate tumor cell lines all express significant levels of IGF-IR [81, 82]; increased expression of the IGF-IR is associated with progression of androgen-sensitive prostate cancer cells lines to androgen independence [83, 84]; treatment with IGF-I causes cell proliferation which is independent of the presence of androgens in the androgen-insensitive but dependent on androgens in the androgen-sensitive cell lines and which is inhibited by IGF-IR antisense oligonucleotide transfection [82, 85]. In concordance with these observations are the findings that injection of PA-III prostate adenocarcinoma cells transfected with an IGF-IR anti-sense construct into rats resulted in a 90% decrease in tumor growth compared to control transfected cells [86]. Not only prostate epithelial cells but also stromal cells derived from benign prostatic hyperplasia express IGF-IR mRNA and IGF-I stimulation increases stromal cell density by 80%, an effect abrogated by co-incubation with IGFI-R neutralizing antibodies providing a possible explanation for the above mentioned association of acromegaly with benign prostate hyperplasia [87].
Transgenic mice expressing human IGF-I in basal epithelial cells of prostrate demonstrate a stepwise development of prostatic adenocarcinomas [88].
Finally, in retroperspective population studies, prostate cancer is associated with IGF-I levels in the higher normal range [89, 90]. Matzoros et al. estimated an odds ratio of 1.9 for a serum IGF-I increment of 60 ng/ml and also demonstrated that in the presence of higher serum testosterone levels the relative risk for prostate cancer increased even further in regard to serum IGF-I increments [89]. A prospective study demonstrated that serum IGF-I levels in the upper quintile of the normal range were associated with a significantly increased 4-fold risk of developing prostate cancer [91] and also with a 5-fold increased risk of advanced stage prostate cancer [92]. The meta-analysis of Renehan et al. estimated a summary odds ratio of 1.83 (CI:1.03–3.26) for the association of the uppermost categories of serum IGF-I compared to the lowermost categories [55].
It is of interest to point out, that acromegaly is also associated with increased liver synthesis of IGFBP-3, which has IGF-independent (as well as IGF-dependent) pro-apoptotic and anti-tumoral effects at the local level. In non-acromegalic patients with prostate cancer, levels of IGFBP-3 are often found to be decreased in the serum and in prostatic tissue [93, 94]. Because IGFBP-3 is a substrate for PSA, a member of the kallikrein family of serine proteases, it has been postulated that rising levels of PSA during prostate cancer evolution facilitates disease progression by proteolytically cleaving IGFBP-3, thereby increasing bioavailable IGF-I at the cellular level [95]. As IGFBP-3 proteolysis is not elevated in patients with acromegaly it has been speculated that this might present a protective mechanism in these patients against the development of prostate cancer [16].
In conclusion, we suggest that men with acromegaly should be screened for prostate cancer as in the general population using serum PSA measurement, rectal examination and/or prostatic ultrasound annually. Patients with high IGF-I receiving replacement testosterone should be monitored with special attention even though the data, thus far, does not confirm an increased risk in acromegalic men.
2.4 Thyroid cancer
Acromegaly is clearly associated with diffuse and nodular goiter, the prevalence of which is dependent on the diagnostic methods ranging from 78–92% using ultrasound [96–102] and 11–87% using palpation [19, 99, 103]. Most studies show to some degree a positive relationship between GH/IGF-I levels and thyroid volume [96–98 101]. The majority of patients have normal thyroid function; hyperthyroidism ranges between 4 and 14% [100–103].
Retrospective studies focusing on overall cancer incidence thyroid cancer constitutes 3.1% of malignancies in acromegaly. Larger studies examining the relative risk for cancer subtypes demonstrate a 4.3 increased [20], 2.5 increased [10], and 3.7 increased [24] relative risk for thyroid cancer, but it has to be taken into account that the patient numbers with thyroid cancer were very low (1 to 3 patients). Retrospective studies focusing on thyroid disease in acromegaly demonstrated either no thyroid cancer in 37 to 80 acromegalic patients [97, 98, 103], or an increased thyroid cancer prevalence compared to the general population [100, 102, 104]. The study by Tita et al. [102] reported a 60-fold increased prevalence of thyroid carcinoma in patients with acromegaly (5.6% of their 125 acromegalic patients had thyroid cancer compared to 0.1% of a general control population in iodine deficient area). Reported types of thyroid cancer include papillary, follicular-variant papillary and follicular carcinomas.
In vitro studies have demonstrated not only that IGF-I increases proliferation of porcine thyroid cells and rat FRTL-5 thyroid cells but also potentiates TSH-mediated thyroid cell proliferation [105]. Furthermore, the existence of a local autocrine IGF-I loop is suggested by the increased presence of IGF-IR in follicular and papillary cancer cells and tumor specimens [106, 107] and by the synthesis of IGF-I in follicular thyroid cells [108], papillary cell lines [109], and surgical thyroid specimens [110].
In view of the high prevalence of nodular goiter in acromegaly and the potential roles of IGF-I and IGFBP3 in malignancy we suggest that thyroid nodules in acromegalic patients should be monitored in accordance with the American Thyroid Association guidelines and that special emphasis should be placed on fine-needle aspiration of all non-functioning nodules 1 cm or greater in size [111].
2.5 Other tumors
As shown in Table 2 other tumor entities have been found in acromegalic patients. Similarly scattered case reports exist describing various tumors including brain tumors [112–114], osseous tumors [115], skin epidermoid tumors and melanomas [116], adrenal tumors [117–120], and different lymphohematopietic neoplasms (lymphoma, multiple myeloma, chronic myeloid or lymphocytic leukemia) [121–123].
In the early smaller studies it was also suggested that lung tumors occurred more frequently in patients with acromegaly [3, 6, 124], but the larger studies by Ron et al. [20], Orme et al. [10], and Baris et al. [24] did not confirm an increased prevalence. On the other hand, experimental studies have shown that normal and tumoral lung tissue, as well as small cell lung cancer (SCLC) and non-SCLC express the IGF-IR and produce IGF-I in an autocrine fashion [125–129]. Stimulation with IGF-I or over expression of the IGF-IR induces cell proliferation and increases the metastatic activity of lung cancer cells [130]. Furthermore, a large-scale genome-wide association study in UK Caucasians undertaken to identify susceptibility alleles for lung cancer identified variants in the GH/IGF-I pathway associated with the inherited predisposition to this cancer [131]. Additional evidence is provided by a case-control-study in non-acromegalic lung cancer patients, which demonstrated a positive association between IGF-I levels and lung cancer risk and an inverse relationship for IGFBP3 [132]. Conversely, in the meta-analysis by Renehan et al. IGF-I was not associated with an increased risk for lung cancer [55].
3 Pathogenesis of tumor development in acromegaly
3.1 The GH/IGF-I axis (endocrine/autocrine theory)
Endocrine GH secretion occurs in a pulsatile manner from the anterior pituitary gland to mediate somatic growth through membrane bound growth hormone receptor (GHR), a member of the cytokine receptor superfamily [133] (for review see [134]). Upon binding of GH receptor dimers undergo a conformational change [135] bringing two Janus kinases 2 (JAK2) which are associated with the intracellular domain of the receptor into close association that then autophosphorylate [136]. Subsequently, these kinases phosphorylate the GHR and activate the signal transducers and activators of transcription (STAT) proteins, in particular STAT5, which translocates to the nucleus and transactivates specific genes such as c-fos, insulin, and acid-labile subunit [137]. STAT 5b binding sites have also been demonstrated in the IGF-I promoter and shown to regulate IGF-I transcription in a GH-dependent manner [138, 139]. GH receptor activation is also mediated via the phosphatidylinositol 3’-kinase (PI3K) and Ras/MAPK pathways (for review see [140, 141]).
Elevated circulating GH levels, independent of IGF-I, have mitogenic and anti-apoptotic effects in many tissues through transcriptional regulation of different signaling pathways (reviewed in [142]) including AKT [143], inhibition of the pro-apoptotic caspase-3 protein [144], and activation of nuclear factor (NF) -kappaB, PI3K [145] and p70S6K, a kinase involved in the control of cell proliferation and differentiation [146]. Negative regulators of GH signaling include suppressor of cytocine signaling (SOCS) -1, -2, -3 and CIS (cytokine inducible SH2-containing protein) [147]. Haplo-insufficiency of SOCS2 enhances the trophic actions of GH in the small intestine and promotes formation of colon polyps, thus suggesting that small variations in SOCS2 expression levels may significantly influence the impact of elevated GH in the intestine [148].
In addition to the classical endocrine actions of the GH/IGF-I axis, important paracrine and autocrine effects of locally produced GH and/or IGF-I are increasingly recognized. Autocrine GH increases MCF-7 cell proliferation, protects from apoptosis, promotes epithelial to mesenchymal transition and confers an invasive cell type [149, 150]. Forced expression of GH in MCF-10A cells, an immortalized but otherwise normal human mammary epithelial cell line, is sufficient for oncogenic transformation and tumor formation in vivo [151]. Importantly, GH administration was not transforming in this system highlighting the role of autocrine GH in this process.
The IGF system is comprised of three ligands (IGF-I, IGF-II, and insulin), multiple receptors (IGF-IR, IR, hybrids of IGF-IR and IR, and IGF-IIR), six IGF binding proteins (IGFBP), three families of IGFBP proteases, and nine growth-mediating factors (reviewed in [152]). IGF-I circulates in the serum bound to IGFBP3 and ALS as a complex, which acts both as a reservoir and regulator of local IGF-I distribution. IGF-I is released from IGFBP3 by proteolysis. The IGF-I cellular effects are achieved through the interaction of IGF-I with the IGF-IR, a transmembrane receptor tyrosine kinase. Ligand-binding to the IGF-IR results in a conformational change leading to trans-phophorylation of one receptor subunit by the other. This is followed by recruitment of specific docking intermediates, including insulin-receptor substrate-1 (IRS-1), Shc and 14–3–3 proteins [153, 154]. These molecules link the IGFI-R to diverse signaling pathways, allowing induction of growth, transformation, differentiation and protection against apoptosis. IGFI-R activation or over expression is associated with an increased propensity for invasion and metastasis. This effect is mediated by multiple signaling intermediates including of IRS-1, which can disrupt E-cadherin from the actin cytoskeleton and promote β-catenin-mediated transcriptional activity [155]. Similarly, tumor cell motility and invasive potential are influenced by crosstalk between the IGF axis and integrins [156], and by IGF induced secretion of matrix metalloproteinases [157]. The finding that IGF-IR over expression confers an invasive, metastatic phenotype in a murine model of pancreatic cancer highlights the importance of these functions [158]. Furthermore, IGF-IR inhibition is capable of inhibiting metastasis in vivo [159, 160].
We conclude that experimental and epidemiological studies provide robust evidence that elevated GH and/or IGF-I levels can contribute to tumor progression and possibly tumor initiation. However, elevated circulating levels of GH and IGF-I in acromegalic subjects may not necessarily lead to increased tumor development due to differences in the endocrine and autocrine/paracrine GH/IGF-I axis. Furthermore, elevated IGFBP3 which has pro-apoptotic and anti-proliferative effects, may alter tissue sensitivity to GH/IGF-I signaling [161]. On the other hand, a biological mechanism distinct from this frequently cited enhancement of the GH/IGF-I pathway may be operational in determining the risk of cancer in acromegaly.
3.2 The genetic/epigenetic theory
It is conceivable that factors that predispose to a GH-secreting pituitary tumor may also predispose to the development of different cancers. In this regard, a recent study utilizing the nationwide Swedish Family-Cancer Database to analyze familial risks for pituitary adenomas and associated tumors through parental and sibling probands is of interest [162]. While familial pituitary tumor syndromes were seldom (only three offspring-parent pairs showed concordant pituitary tumors), the results suggested an association between pituitary adenomas in the offspring and parental skin cancer (SIR 1.60; CI:1.13–2.21), leukemia (SIR 1.90; CI:1.31–2.66), and nervous system hemangiopericytomas (SIR 182, CI not listed). Among siblings there was a significant association between pituitary tumors and breast cancer (SIR 1.46; CI:1.02–2.01), while the risk of pituitary adenoma was marginally increased in individuals whose siblings were diagnosed with colorectal cancer (SIR 1.53; CI:0.69–2.92). The same authors reported earlier that pituitary tumors (SIR 2.2; CI:1.5–3.1) as well as other endocrine tumors (SIR 3.2; CI:1.82–4.96) were increased in patients first diagnosed with colorectal cancer [163, 164]. Similarly, the authors described an increased rate of second primary endocrine tumors but also non-endocrine neoplasia (including breast, renal, liver, nervous system cancers) after first endocrine tumors, even though the authors acknowledge, that some of these tumors occur in the setting of familial tumor syndromes, such as multiple endocrine neoplasia (MEN) 1/2, Neurofibromatosis, von-Hippel-Lindau disease [165].
The larger studies analyzing cancer incidence in acromegalic patients listed in Table 2 typically excluded patients in their analysis with a first primary non-pituitary tumor followed by a second primary somatotroph adenoma. Ron et al. [20] excluded 87 patients in whom a non-pituitary tumor preceded the diagnosis of acromegaly accounting for nearly 50% of patients with acromegaly and tumors. Similarly, Orme et al. [10] excluded 16 patients with primary non-pituitary tumors while many of the other studies did not list the number of patients excluded. If a common genetic-epigenetic susceptibility is significant in the development of malignant tumors as well as pituitary somatotroph adenomas these previously excluded patients should be included in the analysis. It is tempting to speculate that if all patients were to be included into the statistical analysis the risk of malignant tumors in patients with acromegaly (occurring before or after the diagnosis of acromegaly) is remarkably higher than the estimated SIRs listed in Table 2.
The data supporting second primary tumors after first primary pituitary adenomas is of a much smaller size compared to the data on first and second non-endocrine cancers (see overview [166]). Indeed the latter category predicts that heritable factors and environmental influences may be responsible for the increased occurrence of second primary tumors following primary pituitary adenomas. Thus, we will next discuss potential common genetic events that might predispose to the development of a pituitary somatotroph adenoma as well as other neoplasms.
The first potential candidate gene is the recently described aryl hydrocarbon receptor interacting protein (AIP) gene. AIP interacts with the aryl hydrocarbon receptor and heat shock protein 90 dimer where it is involved in mediating cellular responses to environmental toxins, such as dioxin [167]. Vierimaa et al. [168] identified germline mutations in this gene in 16% of all patients diagnosed with pituitary adenomas in a population-based series from Northern Finland. Many patients lacked a strong family history of pituitary adenomas, thus suggesting that AIP is a low penetrance tumor susceptibility gene. The prevalence of AIP germ-line mutations also varies in different clinical settings. In unselected sporadic pituitary tumors, the overall prevalence seems to be low as shown by studies in patients from the US [169], from Japan [170], and in a patient cohort from France, Belgium, and Italy [171]. In familial isolated pituitary adenomas AIP mutations occur more frequently (up to 15%) [172, 173]. While the numbers of patients with AIP mutation are too small to evaluate the risk of developing other tumors, the incidence of somatic AIP mutations was analyzed in a Finnish series of 373 colorectal cancers, 82 breast cancers, and 44 prostate cancers [174]. Only two missense mutations were identified in colorectal cancer but not in healthy controls and the authors suggested that somatic AIP mutations are not common in these tumor entities. To prove this hypothesis, germline AIP mutations will have to be examined in the context of additional common somatic changes in the pituitary and other affected organs.
Finally, in common with multiple other tumors, epigenetic modification is a feature of pituitary tumorigenesis and methylation-associated silencing of cell cycle regulators have been reported by different groups (reviewed in [175]). For example, the p16 member of the INK4 family blocks cell cycle progression in the G1 phase by specific binding to cyclin-dependant kinase 4 and 6 (CDK 4/6). If p16 is inactivated CDK4/6 binds to cyclin D and phophorylates Rb, which stimulates entry into the S phase and activates cell proliferation [176, 177]. Sporadic pituitary adenomas frequently show loss of p16 due to promoter hypermethylation [178–180]. Loss of p16 by aberrant promoter methylation is also a frequent event in many other tumors, including breast, prostate, colon, liver, and lung [181–184]. Epigenetic events targeting p16 promoter in acromegaly and a wide range of tumors raise the interesting possibility that common environmental factors, such as folate deficiency, may contribute to acromegaly and other tumors. Folate deficiency appears to increase the risk of developing several malignancies including colorectal cancer [185], and changes in folate metabolism have also been implicated in pituitary adenoma formation [186]. Folate deficiency has been associated with overall DNA hypomethylation but with promoter DNA hypermethylation, especially of the p16 gene promoter thus potentially leading to decreased p16 levels and enhanced cell proliferation [187, 118].
Although the epigenetic mechanisms discussed here are speculative it presents an alternative integrated approach of how environmental factors may impose on genetic events thus endangering one individual to multiple neoplastic diseases including pituitary adenomas.
4 Conclusions
While the majority of epidemiologic studies in acromegalic patients indicate a modest increase of cancer risk, other studies clearly do not support this notion. The true incidence and prevalence of neoplasia in patients with acromegaly is, therefore, difficult to determine on the basis of currently published studies. Deficiencies in these studies include patient numbers, inclusion criteria, selected control populations, and statistical methodologies.
Increasing evidence from in vitro data, animal studies and studies in non-acromegalic patients continue to strengthen the role of the GH/IGF-I axis in tumor development. Such evidence should provide the impetus for more data gathering from large prospective and even retrospective studies relying on tumor registries. Given the increasingly recognized risk of secondary tumors in patients with primary neoplasia, the search for common early genetic and/or epigenetic changes in acromegaly will prove critical in examining cancer risk. Until firmer evidence proves otherwise, acromegalic patients should receive tumor-screening programs for patients at increased risk of cancer. Maximal and sustained GH and IGF-I normalization should be sought to prevent and reduce co-morbidities and normalize life expectancy.
5 Key unanswered questions
The main question if acromegaly is associated with an increased cancer risk still remains controversial. Therefore, it is also currently disputable, if and how patients with acromegaly should be screened for secondary neoplasia. Large scale epidemiologic studies are still required to answer this question. Prospective evaluation of patients with pre-existing conditions should be considered.
The endocrine as well as non-endocrine mechanisms responsible for increased cancer risk deserve a more balanced evaluation. In particular, further studies examining possible epigenetic and genetic variations including multiple tumors from the same patients are required to support the contribution of non-endocrine mechanisms in cancer risk.
References
Wright AD, Hill DM, Lowy C, Fraser TR. Mortality in acromegaly. Q J Med 1970;39(153):1–16.
Alexander L, Appleton D, Hall R, Ross WM, Wilkinson R. Epidemiology of acromegaly in the Newcastle region. Clin Endocrinol (Oxf) 1980;12:71–9.
Nabarro JDN. Acromegaly. Clin Endocrinol (Oxf) 1987;26:481–512.
Bengtsson BA, Eden S, Ernest I, Oden A, Sjogren B. Epidemiology and long-term survival in acromegaly. A study of 166 cases diagnosed between 1955 and 1984. Acta Med Scand 1988;223(4):327–35.
Etxabe J, Gaztambide P, Latorre P, Vazquez JA. Acromegaly: an epidemilogical study. J Endocrinol Invest 1993;16:181–7.
Mustacchi P, Shimkin MB. Occurrence of cancer in acromegaly and in hypopituitarism. Cancer 1957;10(1):100–4.
Bates AS, Van't Hoff W, Jones JM, Clayton RN. An audit of outcome of treatment in acromegaly. Q J Med 1993;86:293–9.
Rajasoorya C, Holdaway IM, Wrightson P, Scott DJ, Ibbertson HK. Determinants of clinical outcome and survivial in acromegaly. Clin Endocrinol (Oxf) 1994;41:95–102.
Swearingen B, Barker FG, Katznelson L, Biller BM, Grinspoon S, Klibanski A, et al. Long-term mortality after transsphenoidal surgery and adjunctive therapy for acromegaly. J Clin Endocrinol Metab 1998;83(10):3419–26.
Orme SM, McNally RJ, Cartwright RA, Belchetz PE. Mortality and cancer incidence in acromegaly: a retrospective cohort study. United Kingdom Acromegaly Study Group. J Clin Endocrinol Metab 1998;83(8):2730–4.
Beauregard C, Truong U, Hardy J, Serri O. Long-term outcome and mortality after transsphenoidal adenomectomy for acromegaly. Clin Endocrinol (Oxf) 2003;58(1):86–91.
Ayuk J, Clayton RN, Holder G, Sheppard MC, Stewart PM, Bates AS. Growth hormone and pituitary radiotherapy, but not serum insulin-like growth factor-I concentrations, predict excess mortality in patients with acromegaly. J Clin Endocrinol Metab 2004;89(4):1613–7.
Holdaway IM, Rajasoorya RC, Gamble GD. Factors influencing mortality in acromegaly. J Clin Endocrinol Metab 2004;89(2):667–74.
Kauppinen-Makelin R, Sane T, Reunanen A, Valimaki MJ, Niskanen L, Markkanen H, et al. A nationwide survey of mortality in acromegaly. J Clin Endocrinol Metab 2005;90(7):4081–6.
Melmed S. Acromegaly and cancer: not a problem? J Clin Endocrinol Metab 2001;86(7):2929–34.
Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 2004;25(1):102–52.
Klein I, Parveen G, Gavaler JS, Vanthiel DH. Colonic polyps in patients with acromegaly. Ann Intern Med 1982;97(1):27–30.
Brunner JE, Johnson CC, Zafar S, Peterson EL, Brunner JF, Mellinger RC. Colon cancer and polyps in acromegaly: increased risk associated with family history of colon cancer. Clin Endocrinol (Oxf) 1990;32(1):65–71.
Barzilay J, Heatley GJ, Cushing GW. Benign and malignant tumors in patients with acromegaly. Arch Intern Med 1991;151(8):1629–32.
Ron E, Gridley G, Hrubec Z, Page W, Arora S, Fraumeni JF Jr. Acromegaly and gastrointestinal cancer. Cancer 1991;68(8):1673–7.
Cheung NW, Boyages SC. Increased incidence of neoplasia in females with acromegaly. Clin Endocrinol (Oxf) 1997;47(3):323–7.
Popovic V, Damjanovic S, Micic D, Nesovic M, Djurovic M, Petakov M, et al. Increased incidence of neoplasia in patients with pituitary adenomas. The Pituitary Study Group. Clin Endocrinol (Oxf) 1998;49(4):441–5.
Higuchi Y, Saeki N, Iuchi T, Uchino Y, Tatsuno I, Uchida D, et al. Incidence of malignant tumors in patients with acromegaly. Endocr J 2000;47(Suppl):S57–60.
Baris D, Gridley G, Ron E, Weiderpass E, Mellemkjaer L, Ekbom A, et al. Acromegaly and cancer risk: a cohort study in Sweden and Denmark. Cancer Causes Control 2002;13(5):395–400.
Holdaway IM, Rajasoorya C. Epidemiology of acromegaly. Pituitary 1999;2(1):29–41.
Renehan AG, O'Connell J, O'Halloran D, Shanahan F, Potten CS, O'Dwyer ST, et al. Acromegaly and colorectal cancer: a comprehensive review of epidemiology, biological mechanisms, and clinical implications. Horm Metab Res 2003;35(11–12):712–25.
Delhougne B, Deneux C, Abs R, Chanson P, Fierens H, Laurent-Puig P, et al. The prevalence of colonic polyps in acromegaly: a colonoscopic and pathological study in 103 patients. J Clin Endocrinol Metab 1995;80(11):3223–6.
Jenkins PJ, Fairclough PD, Richards T, Lowe DG, Monson J, Grossman A, et al. Acromegaly, colonic polyps and carcinoma. Clin Endocrinol (Oxf) 1997;47(1):17–22.
Terzolo M, Reimondo G, Gasperi M, Cozzi R, Pivonello R, Vitale G, et al. Colonoscopic screening and follow-up in patients with acromegaly: a multicenter study in Italy. J Clin Endocrinol Metab 2005;90(1):84–90.
Renehan AG, Bhaskar P, Painter JE, O'Dwyer ST, Haboubi N, Varma J, et al. The prevalence and characteristics of colorectal neoplasia in acromegaly. J Clin Endocrinol Metab 2000;85(9):3417–24.
Ezzat S, Melmed S. Are patients with acromegaly at increased risk for neoplasia? J Clin Endocrinol Metab 1991;72:245–9.
Melmed S, Casanueva FF, Cavagnini F, Chanson P, Frohman L, Grossman A, et al. Guidelines for acromegaly management. J Clin Endocrinol Metab 2002;87(9):4054–8.
Ezzat S, Serri O, Chik CL, Johnson MD, Beauregard H, Marcovitz S, et al. Canadian consensus guidelines for the diagnosis and management of acromegaly. Clin Invest Med 2006;29(1):29–39.
Vasen HF, van Erpecum KJ, Roelfsema F, Raue F, Koppeschaar H, Griffioen G, et al. Increased prevalence of colonic adenomas in patients with acromegaly. Eur J Endocrinol 1994;131(3):235–7.
Colao A, Balzano A, Ferone D, Panza N, Grande G, Marzullo P, et al. Increased prevalence of colonic polyps and altered lymphocyte subset pattern in the colonic lamina propria in acromegaly. Clin Endocrinol (Oxf) 1997;47(1):23–8.
Jenkins PJ, Frajese V, Jones AM, Camacho-Hubner C, Lowe DG, Fairclough PD, et al. Insulin-like growth factor I and the development of colorectal neoplasia in acromegaly. J Clin Endocrinol Metab 2000;85(9):3218–21.
Cats A, Dullaart RP, Kleibeuker JH, Kuipers F, Sluiter WJ, Hardonk MJ, et al. Increased epithelial cell proliferation in the colon of patients with acromegaly. Cancer Res 1996;56(3):523–6.
Bogazzi F, Russo D, Locci MT, Chifenti B, Ultimieri F, Raggi F, et al. Apoptosis is reduced in the colonic mucosa of patients with acromegaly. Clin Endocrinol (Oxf) 2005;63(6):683–8.
Jenkins PJ, Mukherjee A, Shalet SM. Does growth hormone cause cancer? Clin Endocrinol (Oxf) 2006;64(2):115–21.
Ochsenkuhn T, Bayerdorffer E, Meining A, Schinkel M, Thiede C, Nussler V, et al. Colonic mucosal proliferation is related to serum deoxycholic acid levels. Cancer 1999;85(8):1664–9.
Veysey MJ, Thomas LA, Mallet AI, Jenkins PJ, Besser GM, Wass JA, et al. Prolonged large bowel transit increases serum deoxycholic acid: a risk factor for octreotide induced gallstones. Gut 1999;44(5):675–81.
Lincoln DT, Kaiser HE, Raju GP, Waters MJ. Growth hormone and colorectal carcinoma: localization of receptors. In Vivo 2000;14(1):41–9.
Thomas MJ. The molecular basis of growth hormone action. Growth Horm IGF Res 1998;8(1):3–11.
Ross RJ. The GH receptor and GH insensitivity. Growth Horm IGF Res 1999;9(Suppl B):42–5.
Singh P, Rubin N. Insulinlike growth factors and binding proteins in colon cancer. Gastroenterology 1993;105(4):1218–37.
Garrouste FL, Remacle-Bonnet MM, Lehmann MM, Marvaldi JL, Pommier GJ. Up-regulation of insulin/insulin-like growth factor-I hybrid receptors during differentiation of HT29-D4 human colonic carcinoma cells. Endocrinology 1997;138(5):2021–32.
Sekharam M, Zhao H, Sun M, Fang Q, Zhang Q, Yuan Z, et al. Insulin-like growth factor 1 receptor enhances invasion and induces resistance to apoptosis of colon cancer cells through the Akt/Bcl-x(L) pathway. Cancer Res 2003;63(22):7708–16.
Mathews LS, Hammer RE, Behringer RR, D'Ercole AJ, Bell GI, Brinster RL, et al. Growth enhancement of transgenic mice expressing human insulin-like growth factor I. Endocrinology 1988;123(6):2827–33.
Quaife CJ, Mathews LS, Pinkert CA, Hammer RE, Brinster RL, Palmiter RD. Histopathology associated with elevated levels of growth hormone and insulin-like growth factor I in transgenic mice. Endocrinology 1989;124(1):40–8.
Ulshen MH, Dowling RH, Fuller CR, Zimmermann EM, Lund PK. Enhanced growth of small bowel in transgenic mice overexpressing bovine growth hormone. Gastroenterology 1993;104(4):973–80.
Ohneda K, Ulshen MH, Fuller CR, D'Ercole AJ, Lund PK. Enhanced growth of small bowel in transgenic mice expressing human insulin-like growth factor I. Gastroenterology 1997;112(2):444–54.
Lund PK. IGFs and the digestive tract. In: Roberts CT, Rosenfeld RG, editors. The IGF system molecular biology, physiology, and clinical applications. Totowa, NJ: Humana; 1999. p. 517–44.
Yakar S, Pennisi P, Kim CH, Zhao H, Toyoshima Y, Gavrilova O, et al. Studies involving the GH-IGF axis: Lessons from IGF-I and IGF-I receptor gene targeting mouse models. J Endocrinol Invest 2005;28(5 Suppl):19–22.
Pollak M. Insulin-like growth factor physiology and cancer risk. Eur J Cancer 2000;36(10):1224–8.
Renehan AG, Zwahlen M, Minder C, O'Dwyer ST, Shalet SM, Egger M. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 2004;363(9418):1346–53.
Jenkins PJ. Cancers associated with acromegaly. Neuroendocrinology 2006;83(3–4):218–23.
American Cancer Society. Cancer reference information. Atlanta: American Cancer Society; 2007.
AACE Acromegaly Guidelines Task Force. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Diagnosis and Treatment of Acromegaly. Endocr Pract 2004;10(3):213–25.
Jenkins PJ, Fairclough PD. Screening guidelines for colorectal cancer and polyps in patients with acromegaly. Gut 2002;51(Suppl 5):V13–4.
Renehan AG, O'Dwyer ST, Shalet SM. Guidelines for colonoscopic screening in acromegaly are inconsistent with those for other high risk groups. Gut 2003;52(7):1071–2.
Perry I, Stewart PM, Kane K. Colorectal screening guidelines in acromegaly. Gut 2003;52(9):1387.
Mertani HC, Garcia-Caballero T, Lambert A, Gerard F, Palayer C, Boutin JM, et al. Cellular expression of growth hormone and prolactin receptors in human breast disorders. Int J Cancer 1998;79(2):202–11.
Wennbo H, Tornell J. The role of prolactin and growth hormone in breast cancer. Oncogene 2000;19(8):1072–6.
Kaulsay KK, Zhu T, Bennett W, Lee KO, Lobie PE. The effects of autocrine human growth hormone (hGH) on human mammary carcinoma cell behavior are mediated via the hGH receptor. Endocrinology 2001;142(2):767–77.
Pollak MN, Perdue JF, Margolese RG, Baer K, Richard M. Presence of somatomedin receptors on primary human breast and colon carcinomas. Cancer Lett 1987;38(1–2):223–30.
Pollak MN. Endocrine effects of IGF-I on normal and transformed breast epithelial cells: potential relevance to strategies for breast cancer treatment and prevention. Breast Cancer Res Treat 1998;47(3):209–17.
Arteaga CL, Osborne CK. Growth inhibition of human breast cancer cells in vitro with an antibody against the type I somatomedin receptor. Cancer Res 1989;49(22):6237–41.
Yee D, Paik S, Lebovic GS, Marcus RR, Favoni RE, Cullen KJ, et al. Analysis of insulin-like growth factor I gene expression in malignancy: evidence for a paracrine role in human breast cancer. Mol Endocrinol 1989;3(3):509–17.
Paik S. Expression of IGF-I and IGF-II mRNA in breast tissue. Breast Cancer Res Treat 1992;22(1):31–8.
Huff KK, Kaufman D, Gabbay KH, Spencer EM, Lippman ME, Dickson RB. Secretion of an insulin-like growth factor-I-related protein by human breast cancer cells. Cancer Res 1986;46(9):4613–9.
Moon HD, Simpson ME, Li CH, Evans HM. Neoplasms in rats treated with pituitary growth hormone; pulmonary and lymphatic tissues. Cancer Res 1950;10(5):297–308.
Tornell J, Carlsson B, Pohjanen P, Wennbo H, Rymo L, Isaksson O. High frequency of mammary adenocarcinomas in metallothionein promoter-human growth hormone transgenic mice created from two different strains of mice. J Steroid Biochem Mol Biol 1992;43(1–3):237–42.
Hadsell DL, Murphy KL, Bonnette SG, Reece N, Laucirica R, Rosen JM. Cooperative interaction between mutant p53 and des(1–3)IGF-I accelerates mammary tumorigenesis. Oncogene 2000;19(7):889–98.
Yang XF, Beamer WG, Huynh H, Pollak M. Reduced growth of human breast cancer xenografts in hosts homozygous for the lit mutation. Cancer Res 1996;56(7):1509–11.
Emerman JT, Leahy M, Gout PW, Bruchovsky N. Elevated growth hormone levels in sera from breast cancer patients. Horm Metab Res 1985;17(8):421–4.
Peyrat JP, Bonneterre J, Hecquet B, Vennin P, Louchez MM, Fournier C, et al. Plasma insulin-like growth factor-1 (IGF-1) concentrations in human breast cancer. Eur J Cancer 1993;29A(4):492–7.
Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B, et al. Circulating concentrations of insulin-like growth factor-I and risk of breast cancer. Lancet 1998;351(9113):1393–6.
Colao A, Marzullo P, Ferone D, Spiezia S, Cerbone G, Marino V, et al. Prostatic hyperplasia: an unknown feature of acromegaly. J Clin Endocrinol Metab 1998;83(3):775–9.
Colao A, Marzullo P, Spiezia S, Ferone D, Giaccio A, Cerbone G, et al. Effect of growth hormone (GH) and insulin-like growth factor I on prostate diseases: an ultrasonographic and endocrine study in acromegaly, GH deficiency, and healthy subjects. J Clin Endocrinol Metab 1999;84(6):1986–91.
Jenkins PJ, Besser M. Clinical perspective: acromegaly and cancer: a problem. J Clin Endocrinol Metab 2001;86(7):2935–41.
Cohen P, Peehl DM, Lamson G, Rosenfeld RG. Insulin-like growth factors (IGFs), IGF receptors, and IGF-binding proteins in primary cultures of prostate epithelial cells. J Clin Endocrinol Metab 1991;73(2):401–7.
Iwamura M, Sluss PM, Casamento JB, Cockett AT. Insulin-like growth factor I: action and receptor characterization in human prostate cancer cell lines. Prostate 1993;22(3):243–52.
Kaplan PJ, Mohan S, Cohen P, Foster BA, Greenberg NM. The insulin-like growth factor axis and prostate cancer: lessons from the transgenic adenocarcinoma of mouse prostate (TRAMP) model. Cancer Res 1999;59(9):2203–9.
Nickerson T, Chang F, Lorimer D, Smeekens SP, Sawyers CL, Pollak M. In vivo progression of LAPC-9 and LNCaP prostate cancer models to androgen independence is associated with increased expression of insulin-like growth factor I (IGF-I) and IGF-I receptor (IGF-IR). Cancer Res 2001;61(16):6276–80.
Pietrzkowski Z, Wernicke D, Porcu P, Jameson BA, Baserga R. Inhibition of cellular proliferation by peptide analogues of insulin-like growth factor 1. Cancer Res 1992;52(23):6447–51.
Burfeind P, Chernicky CL, Rininsland F, Ilan J, Ilan J. Antisense RNA to the type I insulin-like growth factor receptor suppresses tumor growth and prevents invasion by rat prostate cancer cells in vivo. Proc Natl Acad Sci U S A 1996;93(14):7263–8.
Grant ES, Ross MB, Ballard S, Naylor A, Habib FK. The insulin-like growth factor type I receptor stimulates growth and suppresses apoptosis in prostatic stromal cells. J Clin Endocrinol Metab 1998;83(9):3252–7.
DiGiovanni J, Kiguchi K, Frijhoff A, Wilker E, Bol DK, Beltran L, et al. Deregulated expression of insulin-like growth factor 1 in prostate epithelium leads to neoplasia in transgenic mice. Proc Natl Acad Sci U S A 2000;97(7):3455–60.
Mantzoros CS, Tzonou A, Signorello LB, Stampfer M, Trichopoulos D, Adami HO. Insulin-like growth factor 1 in relation to prostate cancer and benign prostatic hyperplasia. Br J Cancer 1997;76(9):1115–8.
Wolk A, Mantzoros CS, Andersson SO, Bergstrom R, Signorello LB, Lagiou P, et al. Insulin-like growth factor 1 and prostate cancer risk: a population-based, case-control study. J Natl Cancer Inst 1998;90(12):911–5.
Chan JM, Stampfer MJ, Giovannucci E, Gann PH, Ma J, Wilkinson P, et al. Plasma insulin-like growth factor-I and prostate cancer risk: a prospective study. Science 1998;279(5350):563–6.
Chan JM, Stampfer MJ, Ma J, Gann P, Gaziano JM, Pollak M, et al. Insulin-like growth factor-I (IGF-I) and IGF binding protein-3 as predictors of advanced-stage prostate cancer. J Natl Cancer Inst 2002;94(14):1099–106.
Tennant MK, Thrasher JB, Twomey PA, Birnbaum RS, Plymate SR. Insulin-like growth factor-binding protein-2 and -3 expression in benign human prostate epithelium, prostate intraepithelial neoplasia, and adenocarcinoma of the prostate. J Clin Endocrinol Metab 1996;81(1):411–20.
Kanety H, Madjar Y, Dagan Y, Levi J, Papa MZ, Pariente C, et al. Serum insulin-like growth factor-binding protein-2 (IGFBP-2) is increased and IGFBP-3 is decreased in patients with prostate cancer: correlation with serum prostate-specific antigen. J Clin Endocrinol Metab 1993;77(1):229–33.
Cohen P, Peehl DM, Graves HC, Rosenfeld RG. Biological effects of prostate specific antigen as an insulin-like growth factor binding protein-3 protease. J Endocrinol 1994;142(3):407–15.
Miyakawa M, Saji M, Tsushima T, Wakai K, Shizume K. Thyroid volume and serum thyroglobulin levels in patients with acromegaly: correlation with plasma insulin-like growth factor I levels. J Clin Endocrinol Metab 1988;67(5):973–8.
Cheung NW, Boyages SC. The thyroid gland in acromegaly: an ultrasonographic study. Clin Endocrinol (Oxf) 1997;46(5):545–9.
Junik R, Sawicka J, Kozak W, Gembicki M. Thyroid volume and function in patients with acromegaly living in iodine deficient areas. J Endocrinol Invest 1997;20(3):134–7.
Kasagi K, Shimatsu A, Miyamoto S, Misaki T, Sakahara H, Konishi J. Goiter associated with acromegaly: sonographic and scintigraphic findings of the thyroid gland. Thyroid 1999;9(8):791–6.
Gasperi M, Martino E, Manetti L, Arosio M, Porretti S, Faglia G, et al. Prevalence of thyroid diseases in patients with acromegaly: results of an Italian multi-center study. J Endocrinol Invest 2002;25(3):240–5.
Herrmann BL, Baumann H, Janssen OE, Gorges R, Schmid KW, Mann K. Impact of disease activity on thyroid diseases in patients with acromegaly: basal evaluation and follow-up. Exp Clin Endocrinol Diabetes 2004;112(5):225–30.
Tita P, Ambrosio MR, Scollo C, Carta A, Gangemi P, Bondanelli M, et al. High prevalence of differentiated thyroid carcinoma in acromegaly. Clin Endocrinol (Oxf) 2005;63(2):161–7.
Wuster C, Steger G, Schmelzle A, Gottswinter J, Minne HW, Ziegler R. Increased incidence of euthyroid and hyperthyroid goiters independently of thyrotropin in patients with acromegaly. Horm Metab Res 1991;23(3):131–4.
Balkany C, Cushing GW. An association between acromegaly and thyroid carcinoma. Thyroid 1995;5(1):47–50.
Tramontano D, Cushing GW, Moses AC, Ingbar SH. Insulin-like growth factor-I stimulates the growth of rat thyroid cells in culture and synergizes the stimulation of DNA synthesis induced by TSH and Graves’-IgG. Endocrinology 1986;119(2):940–2.
Maiorano E, Ciampolillo A, Viale G, Maisonneuve P, Ambrosi A, Triggiani V, et al. Insulin-like growth factor 1 expression in thyroid tumors. Appl Immunohistochem Mol Morphol 2000;8(2):110–9.
Vella V, Sciacca L, Pandini G, Mineo R, Squatrito S, Vigneri R, et al. The IGF system in thyroid cancer: new concepts. Mol Pathol 2001;54(3):121–4.
Tode B, Serio M, Rotella CM, Galli G, Franceschelli F, Tanini A, et al. Insulin-like growth factor-I: Autocrine secretion by human thyroid follicular cells in primary culture. J Clin Endocrinol Metab 1989;69:639–47.
Onoda N, Ohmura E, Tsushima T, Ohba Y, Emoto N, Isozaki O, et al. Autocrine role of insulin-like growth factor (IGF)-I in a human thyroid cancer cell line. Eur J Cancer 1992;28A(11):1904–9.
Minuto F, Barreca A, del Monte P, Cariola G, Torre GC, Giordano G. Immunoreactive insulin-like growth factor I (IGF-I) and IGF-I-binding protein content in human thyroid tissue. J Clin Endocrinol Metab 1989;68:621–6.
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16(2):109–42.
Cannavo S, Curto L, Fazio R, Paterniti S, Blandino A, Marafioti T, et al. Coexistence of growth hormone-secreting pituitary adenoma and intracranial meningioma: a case report and review of the literature. J Endocrinol Invest 1993;16(9):703–8.
De Menis E, Tulipano G, Villa S, Billeci D, Bonfanti C, Pollara P, et al. Development of a meningioma in a patient with acromegaly during octreotide treatment: are there any causal relationships? J Endocrinol Invest 2003;26(4):359–63.
Curto L, Squadrito S, Almoto B, Longo M, Granata F, Salpietro F, et al. MRI finding of simultaneous coexistence of growth hormone-secreting pituitary adenoma with intracranial meningioma and carotid artery aneurysms: report of a case. Pituitary 2007;10:299–305.
Lima GA, Gomes EM, Nunes RC, Vieira NL, Sieiro AP, Brabo EP, et al. Osteosarcoma and acromegaly: a case report and review of the literature. J Endocrinol Invest 2006;29(11):1006–11.
Corcuff JB, Ogor C, Kerlan V, Rougier MB, Bercovichi M, Roger P. Ocular naevus and melanoma in acromegaly. Clin Endocrinol (Oxf) 1997;47(1):119–21.
Breckenridge SM, Hamrahian AH, Faiman C, Suh J, Prayson R, Mayberg M. Coexistence of a pituitary macroadenoma and pheochromocytoma—a case report and review of the literature. Pituitary 2003;6(4):221–5.
Sleilati GG, Kovacs KT, Honasoge M. Acromegaly and pheochromocytoma: report of a rare coexistence. Endocr Pract 2002;8(1):54–60.
Baughan J, de Gara C, Morrish D. A rare association between acromegaly and pheochromocytoma. Am J Surg 2001;182(2):185–7.
Nasushita R, Watanobe H, Goto T, Tando Y, Tanosaki M, Shiroto T, et al. A case of acromegaly accompanied by adrenal preclinical Cushing's syndrome. Endocr J 1999;46(1):133–7.
Hagg E, Asplund K, Holm J. Acromegaly and multiple myeloma. Ann Intern Med 1988;109(5):437–8.
Alves RH, Vaisman M, Brasil RR, Gadelha MR. Acromegaly and non-Hodgkin's lymphoma. Endocr Pract 1998;4(5):279–81.
Au WY, Chow WS, Lam KS, Ko GT, Cockram CS, Kwong YL. Acute leukaemia in acromegaly patients. Br J Haematol 2000;110(4):871–3.
Ritchie CM, Atkinson AB, Kennedy AL, Lyons AR, Gordon DS, Fannin T, et al. Ascertainment and natural history of treated acromegaly in Northern Ireland. Ulster Med J 1990;59(1):55–62.
Minuto F, del Monte P, Barreca A, Fortini P, Cariola G, Catrambone G, et al. Evidence for an increased somatomedin-C/insulin-like growth factor I content in primary human lung tumors. Cancer Res 1986;46(2):985–8.
Macauly VM, Teale JD, Everard MJ, Joshi GP, Smith IE, Millar JL. Somatomedin-C/insulin-like growth factor-I is a mitogen for human small cell lung cancer. Br J Cancer 1988;57(1):91–3.
Jaques G, Rotsch M, Wegmann C, Worsch U, Maasberg M, Havemann K. Production of immunoreactive insulin-like growth factor I and response to exogenous IGF-I in small cell lung cancer cell lines. Exp Cell Res 1988;176(2):336–43.
Rotsch M, Maasberg M, Erbil C, Jaques G, Worsch U, Havemann K. Characterization of insulin-like growth factor I receptors and growth effects in human lung cancer cell lines. J Cancer Res Clin Oncol 1992;118(7):502–8.
Favoni RE, de Cupis A, Ravera F, Cantoni C, Pirani P, Ardizzoni A, et al. Expression and function of the insulin-like growth factor I system in human non-small-cell lung cancer and normal lung cell lines. Int J Cancer 1994;56(6):858–66.
Nakanishi Y, Mulshine JL, Kasprzyk PG, Natale RB, Maneckjee R, Avis I, et al. Insulin-like growth factor-I can mediate autocrine proliferation of human small cell lung cancer cell lines in vitro. J Clin Invest 1988;82(1):354–9.
Rudd MF, Webb EL, Matakidou A, Sellick GS, Williams RD, Bridle H, et al. Variants in the GH-IGF axis confer susceptibility to lung cancer. Genome Res 2006;16(6):693–701.
Yu H, Spitz MR, Mistry J, Gu J, Hong WK, Wu X. Plasma levels of insulin-like growth factor-I and lung cancer risk: a case-control analysis. J Natl Cancer Inst 1999;91(2):151–6.
Cosman D, Lyman SD, Idzerda RL, Beckmann MP, Park LS, Goodwin RG, et al. A new cytokine receptor superfamily. Trends Biochem Sci 1990;15(7):265–70.
Lanning NJ, Carter-Su C. Recent advances in growth hormone signaling. Rev Endocr Metab Disord 2006;7(4):225–35.
Brown RJ, Adams JJ, Pelekanos RA, Wan Y, McKinstry WJ, Palethorpe K, et al. Model for growth hormone receptor activation based on subunit rotation within a receptor dimer. Nat Struct Mol Biol 2005;12(9):814–21.
Argetsinger LS, Campbell GS, Yang X, Witthuhn BA, Silvennoinen O, Ihle JN, et al. Identification of JAK2 as a growth hormone receptor-associated tyrosine kinase. Cell 1993;74(2):237–44.
Herrington J, Smit LS, Schwartz J, Carter-Su C. The role of STAT proteins in growth hormone signaling. Oncogene 2000;19(21):2585–97.
Woelfle J, Chia DJ, Rotwein P. Mechanisms of growth hormone (GH) action. Identification of conserved Stat5 binding sites that mediate GH-induced insulin-like growth factor-I gene activation. J Biol Chem 2003;278(51):51261–6.
Chia DJ, Ono M, Woelfle J, Schlesinger-Massart M, Jiang H, Rotwein P. Characterization of distinct Stat5b binding sites that mediate growth hormone-stimulated IGF-I gene transcription. J Biol Chem 2006;281(6):3190–7.
Cesena TI, Cui TX, Piwien-Pilipuk G, Kaplani J, Calinescu AA, Huo JS, et al. Multiple mechanisms of growth hormone-regulated gene transcription. Mol Genet Metab 2007;90(2):126–33.
Zhu T, Goh EL, Graichen R, Ling L, Lobie PE. Signal transduction via the growth hormone receptor. Cell Signal 2001;13(9):599–616.
Perry JK, Emerald BS, Mertani HC, Lobie PE. The oncogenic potential of growth hormone. Growth Horm IGF Res 2006;16(5–6):277–89.
Costoya JA, Finidori J, Moutoussamy S, Searis R, Devesa J, Arce VM. Activation of growth hormone receptor delivers an antiapoptotic signal: evidence for a role of Akt in this pathway. Endocrinology 1999;140(12):5937–43.
Sanders EJ, Parker E, Harvey S. Retinal ganglion cell survival in development: mechanisms of retinal growth hormone action. Exp Eye Res 2006;83(5):1205–14.
Jeay S, Sonenshein GE, Kelly PA, Postel-Vinay MC, Baixeras E. Growth hormone exerts antiapoptotic and proliferative effects through two different pathways involving nuclear factor-kappaB and phosphatidylinositol 3-kinase. Endocrinology 2001;142(1):147–56.
MacKenzie SJ, Yarwood SJ, Peden AH, Bolger GB, Vernon RG, Houslay MD. Stimulation of p70S6 kinase via a growth hormone-controlled phosphatidylinositol 3-kinase pathway leads to the activation of a PDE4A cyclic AMP-specific phosphodiesterase in 3T3-F442A preadipocytes. Proc Natl Acad Sci U S A 1998;95(7):3549–54.
Adams TE, Hansen JA, Starr R, Nicola NA, Hilton DJ, Billestrup N. Growth hormone preferentially induces the rapid, transient expression of SOCS-3, a novel inhibitor of cytokine receptor signaling. J Biol Chem 1998;273(3):1285–7.
Michaylira CZ, Ramocki NM, Simmons JG, Tanner CK, McNaughton KK, Woosley JT, et al. Haplotype insufficiency for suppressor of cytokine signaling-2 enhances intestinal growth and promotes polyp formation in growth hormone-transgenic mice. Endocrinology 2006;147(4):1632–41.
Kaulsay KK, Mertani HC, Tornell J, Morel G, Lee KO, Lobie PE. Autocrine stimulation of human mammary carcinoma cell proliferation by human growth hormone. Exp Cell Res 1999;250(1):35–50.
Mukhina S, Mertani HC, Guo K, Lee KO, Gluckman PD, Lobie PE. Phenotypic conversion of human mammary carcinoma cells by autocrine human growth hormone. Proc Natl Acad Sci U S A 2004;101(42):15166–71.
Zhu T, Starling-Emerald B, Zhang X, Lee KO, Gluckman PD, Mertani HC, et al. Oncogenic transformation of human mammary epithelial cells by autocrine human growth hormone. Cancer Res 2005;65(1):317–24.
Riedemann J, Macaulay VM. IGF1R signalling and its inhibition. Endocr Relat Cancer 2006;13(Suppl 1):S33–43.
Baserga R, Resnicoff M, Dews M. The IGF-I receptor and cancer. Endocrine 1997;7(1):99–102.
Pollak MN, Schernhammer ES, Hankinson SE. Insulin-like growth factors and neoplasia. Nat Rev Cancer 2004;4(7):505–18.
Playford MP, Bicknell D, Bodmer WF, Macaulay VM. Insulin-like growth factor 1 regulates the location, stability, and transcriptional activity of beta-catenin. Proc Natl Acad Sci U S A 2000;97(22):12103–8.
Shen MR, Hsu YM, Hsu KF, Chen YF, Tang MJ, Chou CY. Insulin-like growth factor 1 is a potent stimulator of cervical cancer cell invasiveness and proliferation that is modulated by alphavbeta3 integrin signaling. Carcinogenesis 2006;27(5):962–71.
Zhang D, Samani AA, Brodt P. The role of the IGF-I receptor in the regulation of matrix metalloproteinases, tumor invasion and metastasis. Horm Metab Res 2003;35(11–12):802–8.
Lopez T, Hanahan D. Elevated levels of IGF-1 receptor convey invasive and metastatic capability in a mouse model of pancreatic islet tumorigenesis. Cancer Cell 2002;1(4):339–53.
Dunn SE, Ehrlich M, Sharp NJ, Reiss K, Solomon G, Hawkins R, et al. A dominant negative mutant of the insulin-like growth factor-I receptor inhibits the adhesion, invasion, and metastasis of breast cancer. Cancer Res 1998;58(15):3353–61.
Samani AA, Fallavollita L, Jaalouk DE, Galipeau J, Brodt P. Inhibition of carcinoma cell growth and metastasis by a vesicular stomatitis virus G-pseudotyped retrovector expressing type I insulin-like growth factor receptor antisense. Hum Gene Ther 2001;12(16):1969–77.
Burger AM, Leyland-Jones B, Banerjee K, Spyropoulos DD, Seth AK. Essential roles of IGFBP-3 and IGFBP-rP1 in breast cancer. Eur J Cancer 2005;41(11):1515–27.
Hemminki K, Forsti A, Ji J. Incidence and familial risks in pituitary adenoma and associated tumors. Endocr Relat Cancer 2007;14(1):103–9.
Hemminki K, Forsti A, Ji J. Pituitary adenoma predisposition. J Clin Endocrinol Metab 2007 (in press).
Hemminki K, Li X, Dong C. Second primary cancers after sporadic and familial colorectal cancer. Cancer Epidemiol Biomarkers Prev 2001;10(7):793–8.
Hemminki K, Jiang Y. Second primary neoplasms after 19281 endocrine gland tumours: aetiological links? Eur J Cancer 2001;37(15):1886–94.
Vogel VG. Identifying and screening patients at risk of second cancers. Cancer Epidemiol Biomarkers Prev 2006;15(11):2027–32.
Harper PA, Riddick DS, Okey AB. Regulating the regulator: factors that control levels and activity of the aryl hydrocarbon receptor. Biochem Pharmacol 2006;72(3):267–79.
Vierimaa O, Georgitsi M, Lehtonen R, Vahteristo P, Kokko A, Raitila A, et al. Pituitary adenoma predisposition caused by germline mutations in the AIP gene. Science 2006;312(5777):1228–30.
Yu R, Bonert V, Saporta I, Raffel LJ, Melmed S. Aryl hydrocarbon receptor interacting protein variants in sporadic pituitary adenomas. J Clin Endocrinol Metab 2006;91(12):5126–9.
Iwata T, Yamada S, Mizusawa N, Golam HM, Sano T, Yoshimoto K. The aryl hydrocarbon receptor-interacting protein gene is rarely mutated in sporadic GH-secreting adenomas. Clin Endocrinol (Oxf) 2007;66(4):499–502.
Barlier A, Vanbellinghen JF, Daly AF, Silvy M, Jaffrain-Rea ML, Trouillas J, et al. Mutations in the aryl hydrocarbon receptor interacting protein gene are not highly prevalent among subjects with sporadic pituitary adenomas. J Clin Endocrinol Metab 2007;92(5):1952–5.
Daly AF, Vanbellinghen JF, Khoo SK, Jaffrain-Rea ML, Naves LA, Guitelman MA, et al. Aryl hydrocarbon receptor-interacting protein gene mutations in familial isolated pituitary adenomas: analysis in 73 families. J Clin Endocrinol Metab 2007;92(5):1891–6.
Toledo RA, Lourenco DM Jr., Liberman B, Cunha-Neto MB, Cavalcanti MG, Moyses CB, et al. Germline mutation in the aryl hydrocarbon receptor interacting protein gene in familial somatotropinoma. J Clin Endocrinol Metab 2007;92(5):1934–7.
Georgitsi M, Karhu A, Winqvist R, Visakorpi T, Waltering K, Vahteristo P, et al. Mutation analysis of aryl hydrocarbon receptor interacting protein (AIP) gene in colorectal, breast, and prostate cancers. Br J Cancer 2007;96(2):352–6.
Farrell WE. Epigenetic mechanisms of tumorigenesis. Horm Metab Res 2005;37(6):361–8.
Jeffrey PD, Tong L, Pavletich NP. Structural basis of inhibition of CDK-cyclin complexes by INK4 inhibitors. Genes Dev 2000;14(24):3115–25.
Obaya AJ, Sedivy JM. Regulation of cyclin-Cdk activity in mammalian cells. Cell Mol Life Sci 2002;59(1):126–42.
Woloschak M, Yu A, Post KD. Frequent inactivation of the p16 gene in human pituitary tumors by gene methylation. Mol Carcinog 1997;19(4):221–4.
Jaffrain-Rea ML, Ferretti E, Toniato E, Cannita K, Santoro A, Di Stefano D, et al. p16 (INK4a, MTS-1) gene polymorphism and methylation status in human pituitary tumours. Clin Endocrinol (Oxf) 1999;51(3):317–25.
Ogino A, Yoshino A, Katayama Y, Watanabe T, Ota T, Komine C, et al. The p15(INK4b)/p16(INK4a)/RB1 pathway is frequently deregulated in human pituitary adenomas. J Neuropathol Exp Neurol 2005;64(5):398–403.
Herman JG, Merlo A, Mao L, Lapidus RG, Issa JP, Davidson NE, et al. Inactivation of the CDKN2/p16/MTS1 gene is frequently associated with aberrant DNA methylation in all common human cancers. Cancer Res 1995;55(20):4525–30.
Gonzalez-Zulueta M, Bender CM, Yang AS, Nguyen T, Beart RW, Van Tornout JM, et al. Methylation of the 5’′ CpG island of the p16/CDKN2 tumor suppressor gene in normal and transformed human tissues correlates with gene silencing. Cancer Res 1995;55(20):4531–5.
Jin M, Piao Z, Kim NG, Park C, Shin EC, Park JH, et al. p16 is a major inactivation target in hepatocellular carcinoma. Cancer 2000;89(1):60–8.
Kurakawa E, Shimamoto T, Utsumi K, Hirano T, Kato H, Ohyashiki K. Hypermethylation of p16(INK4a) and p15(INK4b) genes in non-small cell lung cancer. Int J Oncol 2001;19(2):277–81.
Kim YI. Folate and DNA methylation: a mechanistic link between folate deficiency and colorectal cancer? Cancer Epidemiol Biomarkers Prev 2004;13(4):511–9.
Evans CO, Reddy P, Brat DJ, O'Neill EB, Craige B, Stevens VL, et al. Differential expression of folate receptor in pituitary adenomas. Cancer Res 2003;63(14):4218–24.
Pogribny IP, James SJ. De novo methylation of the p16INK4A gene in early preneoplastic liver and tumors induced by folate/methyl deficiency in rats. Cancer Lett 2002;187(1–2):69–75.
van Engeland M, Weijenberg MP, Roemen GM, Brink M, de Bruine AP, Goldbohm RA, et al. Effects of dietary folate and alcohol intake on promoter methylation in sporadic colorectal cancer: the Netherlands cohort study on diet and cancer. Cancer Res 2003;63(12):3133–7.
Drange MR, Fram NR, Herman-Bonert V, Melmed S. Pituitary tumor registry: a novel clinical resource. J Clin Endocrinol Metab 2000;85(1):168–74.
Mestron A, Webb SM, Astorga R, Benito P, Catala M, Gaztambide S, et al. Epidemiology, clinical characteristics, outcome, morbidity and mortality in acromegaly based on the Spanish Acromegaly Registry (Registro Espanol de Acromegalia, REA). Eur J Endocrinol 2004;151(4):439–46.
Ituarte EA, Petrini J, Hershman JM. Acromegaly and colon cancer. Ann Intern Med 1984;101(5):627–8.
Pines A, Rozen P, Ron E, Gilat T. Gastrointestinal tumors in acromegalic patients. Am J Gastroenterol 1985;80(4):266–9.
Ezzat S, Strom C, Melmed S. Colon polyps in acromegaly. Ann Intern Med 1991;114:754–5.
Ladas SD, Thalassinos NC, Ioannides G, Raptis SA. Does acromegaly really predispose to an increased prevalence of gastrointestinal tumours? Clin Endocrinol (Oxf) 1994;41(5):597–601.
Matano Y, Okada T, Suzuki A, Yoneda T, Takeda Y, Mabuchi H. Risk of colorectal neoplasm in patients with acromegaly and its relationship with serum growth hormone levels. Am J Gastroenterol 2005;100(5):1154–60.
Acknowledgements
SL holds personnel support from the Deutsche Forschungsgemeinschaft (LO 1178/1-1). SE is supported by operating grant funding from the Canadian Institutes of Health Research (CIHR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loeper, S., Ezzat, S. Acromegaly: Re-thinking the cancer risk. Rev Endocr Metab Disord 9, 41–58 (2008). https://doi.org/10.1007/s11154-007-9063-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-007-9063-z