Abstract
Most research on the effectiveness of prenatal care has focused on birth outcomes and has found small or no effects. It is possible, however, that prenatal care is “too little too late” to improve pregnancy outcomes in the aggregate, but that it increases the use of pediatric health care or improves maternal health-related parenting practices and, ultimately, child health. We use data from the Fragile Families and Child Wellbeing birth cohort study that have been augmented with hospital medical record data to estimate effects of prenatal care timing on pediatric health care utilization and health-related parenting behaviors during the first year of the child’s life. We focus on maternal postpartum smoking, preventive health care visits for the child, and breastfeeding. We use a multi-pronged approach to address the potential endogeneity of the timing of prenatal care. We find that first trimester prenatal care appears to decrease maternal postpartum smoking by about 5 percentage points and increase the likelihood of 4 or more well-baby visits by about 1 percentage point, and that it may also have a positive effect on breastfeeding. These findings suggest that there are benefits to standard prenatal care that are generally not considered in evaluations of prenatal care programs and interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Most research on the effectiveness of prenatal care has focused on birth outcomes, usually birthweight or infant mortality, and has found small or no effects. It is possible, however, that prenatal care during the confines of a pregnancy is often “too little too late” to improve the outcome of a given pregnancy, but that it increases the use of pediatric health care or improves maternal health-related parenting practices and, ultimately, child health. According to the Public Health Service’s Expert Panel on the Content of Prenatal Care, a broad goal of contemporary prenatal care is to promote the health of the mother, child, and family through the pregnancy, delivery, and the child’s development (USDHHS 1989).
We use survey data from the Fragile Families and Child Wellbeing birth cohort study that have been augmented with hospital medical record data to estimate effects of an important aspect of prenatal care, timing of initiation, on pediatric health care utilization and health-related parenting behaviors during the first year of the child’s life. We focus on maternal postpartum smoking, preventive health care visits for the child, and breastfeeding. We use a multi-pronged approach to address the potential endogeneity of the timing of prenatal care. This study fills a critical gap in the literature and contributes to a more complete understanding of the benefits of prenatal care.
1 Background
Prenatal care is one of the most frequently used health services in the United States, according to data from the 1995 National Medical Ambulatory Care Survey (Schappert 1997; Kogan et al. 1998b). Standard prenatal care, which involves a series of encounters during the gestational period, educates women about pregnancy, monitors medical conditions they may have, tests for gestational health problems, and refers expectant mothers to services such as support groups and social services (March of Dimes 2009). Owing largely to expansions of Medicaid for pregnant women in the late 1980s and early 1990, prenatal care has become quasi-universal, with 92–96% of mothers giving birth in the US in 2006 receiving at least some prenatal care (Martin et al. 2009). However, there is variation in the timing of initiation of that care. For example, 17% of births in 2006 occurred to mothers who initiated care after the first trimester of pregnancy. The rates of late and no care are higher among mothers who are young and poor (Lia-Hoagberg et al. 1990).
1.1 Birth outcome production functions
Economists have been studying the production of infant health for several decades. Prenatal care (usually the timing of initiation) has been a key input of interest, and the outcomes studied have typically been infant mortality, birthweight, or low birthweight. A recent study by Reichman et al. (2009) also investigated whether an infant is born with an abnormal health condition. Much of this literature is reviewed by Conway and Kutinova (2006) and Reichman et al. (2009).
Most recent studies of the effects of prenatal care on birth outcomes have found very modest or no effects. For example, Reichman et al. (2009) found that first trimester care reduces birthweight by only 20 g, and Evans and Lien (2005) found that prenatal visits do not have a significant effect on birthweight overall, but have a positive effect among mothers early in their pregnancies. The finding of a small or no overall effect of prenatal care is consistent with findings from a recent descriptive study with extremely rich data (Reichman and Teitler 2005) and a recent review in the medical literature indicating that few features of prenatal care would be expected to increase birthweight at the aggregate level (Lu et al. 2003). Overall, the evidence that early or frequent prenatal care improves birth outcomes is less than compelling.
A key methodological challenge in estimating the effect of prenatal care on birth outcomes is the potential endogeneity of prenatal care (i.e., the estimated effects of prenatal care use may reflect unobserved characteristics of mothers that are associated with both prenatal care use and the birth outcome). Many studies in the economics literature have used instrumental variables techniques, which have become increasingly sophisticated in terms of model specification and testing, with prenatal care price or availability measures as instruments. Other studies, such as Evans and Lien (2005) have exploited natural experiments (in this case, a bus strike in Pennsylvania). The latter approach, while conceptually appealing, can be applied only under special, somewhat idiosyncratic, circumstances and may not result in findings that are generalizable. Reichman et al. (2009) employed a third approach—using rich data to accurately characterize prenatal care and to proxy theoretically important but typically unobserved variables. The authors were able to assess the sensitivity to different measures, data sources, and model specifications (including instrumental variables models). For example, they found that the difference between self-reported first trimester prenatal care and that based on detailed information recorded in medical records was substantial, and that using the self-reports overestimated the effects of first trimester care on birthweight.
1.2 A broader view of the potential of prenatal care
Prenatal care may have long-term effects on mothers’ health behaviors, use of pediatric health care, and their children’s health by increasing awareness of how their behaviors and environment can impact the health of their child or by connecting mothers to the health care and social service systems, sometimes for the first time. Postnatal smoking and breastfeeding may be particularly influenced by prenatal care, as those behaviors are universally emphasized in prenatal care protocols (USDHHS 1989). Referrals to counseling or smoking cessation treatment have become typical features of contemporary prenatal care (USDHHS 1989), and there is evidence (much of it based on randomized controlled trials) that prenatal smoking interventions are effective in reducing smoking during pregnancy (Dolan-Mullen et al. 1994; Melvin et al. 2000; Klesges et al. 2001) and in reducing postpartum relapse among mothers who quit smoking during pregnancy (Fang et al. 2004). There is also evidence that prenatal breastfeeding education increases breastfeeding. For example, Kistin et al. (1989) found, in a randomized controlled trial, that prenatal breastfeeding education and counseling increased rates of breastfeeding among urban, black, low-income women.
Data from the 2002 Prenatal Risk Assessment Monitoring System (PRAMS) Surveillance Report indicate that, in the 27 PRAMS states combined, over 70% of mothers reported that, during the course of their prenatal care, a health care provider or worker counseled them (beyond offering printed materials) on the harmful effects of smoking during pregnancy, and that over 80% reported that their prenatal care counseling included a discussion of breastfeeding (Williams et al. 2006). Postnatal smoking and breastfeeding are important behavioral outcomes because children who are exposed to second-hand tobacco smoke are at increased risk for sudden infant death syndrome, acute respiratory infections, asthma, and ear infections (USDHHS 2006), and human milk decreases the incidence and/or severity of a wide range of infectious diseases and appears to be protective against many other health conditions, including sudden infant death syndrome, diabetes, obesity, hypercholesterolemia, asthma, and neurodevelopmental delays (AAP 2005).
Connection and exposure to the health care system through prenatal care may also encourage the use of pediatric care. Descriptive studies have found that children whose mothers have less than adequate prenatal care utilization (based on an index that takes into consideration the month care began and the number of prenatal care visits given gestational age) have significantly fewer well-child visits by age 6 months and are significantly less likely to have adequate immunizations than children of mothers who have adequate prenatal care (Kogan et al. 1998a), and that early prenatal care is positively associated with the number of well-child visits in the first two years of life (Freed et al. 1998). Of course, these associations cannot be interpreted as causal effects. The American Academy of Pediatrics (AAP) recommends eight routine visits to a pediatrician during the first year of life, with a set schedule of assessments for various developmental milestones, screenings, and immunizations (AAP 2008).
As far as we know, no previous studies in the economics literature have examined the effects of prenatal care on pediatric health care utilization or parenting practices that could affect children’s health and development. In fact, very few studies (in any literature) have considered potential broader impacts (beyond the birth outcome) of prenatal care. One exception is a recent study by Conway and Kutinova that used data from the National Maternal and Infant Health Survey to examine the effects of prenatal care on women’s health. The authors found that receiving early and adequate prenatal care leads mothers to maintain a healthy weight and may reduce lengthy maternal hospitalizations (Conway and Kutinova 2006).
2 Conceptual framework
We consider three maternal postnatal behaviors that are directly relevant to the child’s health: postpartum cigarette smoking, taking the infant for well-baby visits, and breastfeeding. We would not expect visits to a pediatrician to affect the health of the mother, at least directly. However, two of our outcomes have direct effects not only on child health, but also on maternal health. Breastfeeding imparts health benefits to women in the form of reduced risk for diabetes, breast, and ovarian cancers (Ip et al. 2007), and the adverse health effects from smoking cigarettes are well known. In specifying a conceptual framework, we begin with a simple model for well-baby visits (which do not have direct effects on the mother’s health) and then move to more complicated models wherein behaviors can affect both the infant’s and the mother’s health.
2.1 Demand for child inputs with no maternal health production
Following Corman et al. (1987) and the theoretical literature on which they build, we assume that the mother’s utility is a function of consumption goods (C), child health (CH), and tastes as follows:
Child health is a function of prenatal care (PC), other prenatal inputs (PrI), postnatal inputs (PoI) such as the use of pediatric care, the health endowment of the mother (HE), and other characteristics of the mother (E) such as education that act as efficiency parameters in the structural child health production function that follows:
The demand for each input is a function of the price and availability of that input, the prices and availability of substitute and complementary inputs, income (Y), child health, and tastes. The demand for a given postnatal input can be expressed as follows:
The determinants of child health (from Eq. 2) can be substituted for child health in Eq. 3 to derive a quasi-reduced-form demand function for a given postnatal input, as follows:
Equation 4 can be used to estimate the demand for well-baby health care, which does not directly affect the mother’s health. As discussed earlier, prenatal care may affect input price/availability (e.g., by directing women to convenient locations for pediatric care) or tastes (e.g., by educating women about the negative health effects of smoking). Therefore, prenatal care may affect child health not only through direct impacts on the neonate, but also through the use of health inputs.
2.2 Demand for inputs with joint health production
We can re-express Eqs. 1 and 2, as follows, to incorporate the possibility that the mother herself may derive utility from a given behavior (maternal behavior, MB), and that the behavior may affect not only the infant’s health, but also her own health (maternal health, MH).Footnote 1 This would be the case for two of the postnatal inputs of interest, postpartum smoking and breastfeeding.
The child’s health production function (Eq. 2a*) is similar to the one expressed in Eq. 2a with the exception that the mother’s health during the pregnancy (and not a static health endowment) affects the health of the child. The mother’s health is produced as follows, where her health depends on her endowment plus pre-and postnatal child health inputs that might also affect her own health:
Utility maximization yields a demand for postnatal behaviors that may contain factors related to consumption. For example, mothers may derive pleasure from the bonding experience of breastfeeding or simply enjoy smoking cigarettes. These behaviors are also inputs into both maternal and infant health. The structural demand function for a given postnatal input (behavior) can be expressed as follows, where Y is income and μ represents unobservable factors such as tastes and other unobserved factors:
A quasi-reduced form demand function for a given postnatal input, netting out measures of child health, leads to:
We can further net out maternal health, resulting in the following quasi reduced-form demand function for a given postnatal input (breastfeeding or smoking) as a function of the price/availability of that and other postnatal inputs and of the mother’s endowed health (HE), as well as prenatal inputs, including prenatal care:
Since Eq. (4b*) is identical to Eq. (4), we can estimate the effects of prenatal care on all three of our postnatal outcomes (well-baby care, smoking, and breastfeeding) using the same right-hand-side variables.
3 Data
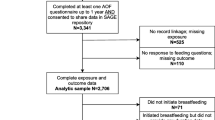
The Fragile Families and Child Wellbeing (FFCWB) study is an ongoing longitudinal birth cohort study. Between the spring of 1998 and the fall of 2000, parents were interviewed in 75 hospitals in 20 large US cities (in 15 states) shortly after their children were born. Cities were selected from all 77 cities in the US with over 200,000 people, using a stratified random sample. Within each hospital, births were randomly sampled from birth logs. Non-marital births were oversampled (see Reichman et al. 2001 for more information about the research design). Both parents were re-interviewed approximately 1 year later. A total of 4,898 mothers (86% of those who were eligible) were interviewed after they gave birth (the “baseline” interview); of those, 4,365 (89%) completed follow-up interviews 12–18 months later (the “1 year follow-up” interview). The survey data are rich in sociodemographic characteristics of both mothers and fathers, and include information on the parents’ relationship status and living arrangements.
As part of an “add on” study to the core survey, the following were collected and attached to the survey records: (1) data from medical records (from the birth hospitalization) of the mother and child, and (2) spatial (geographic) coordinates of the mother’s address at the time of the birth and of the hospital in which she gave birth. The medical records data were collected using a detailed standardized instrument. The availability of medical record data depended, for the most part, on administrative processes of hospitals rather than decisions on the part of survey respondents to make their records available. Medical record data, which were needed for the analyses, were available for 3,684 (75%) of the 4,898 births in the FFCWB sample. The geographic coordinates were used to append measures of prenatal care availability and census tract level poverty, which are used in certain analyses as described later.
The enhanced FFCWB data are well suited for analyzing the effects of the timing of prenatal care on maternal postnatal behaviors because they were collected as part of a longitudinal birth cohort study and include: (1) detailed data on prenatal care that were recorded in the subjects’ obstetrical charts; (2) information about the mother’s postnatal behaviors; (3) detailed information on the mother’s health that was documented in prenatal medical records; (4) data on the fathers regardless of whether they ever lived with their children; and (5) spatial coordinates that allow us to append geographic data.
4 Descriptive analysis
Below we describe the measures we use in our analyses, present summary statistics, and point out many salient characteristics of the sample. Unless indicated otherwise, all covariates are measured at the time of the birth (baseline). In general, we rely on mothers’ reports. However, when the mother’s responses on specific items were missing, we use the father’s reports if those are available. Additionally, paternal reports are the primary source of information on paternal education. We restrict the sample to cases with non-missing data on the maternal postnatal behaviors, prenatal care from the medical records, and covariates, resulting in a sample size of 2,283. Descriptive statistics are presented in Table 1.
4.1 Timing of prenatal care
The key measure of prenatal care timing, based on information from the hospital medical records, is a dichotomous indicator for first trimester prenatal care (before week 14 of the pregnancy). We are assuming that earlier care results in increased exposure to health education and referrals to other services that take place as part of prenatal care. In our sample, over half (58%) of the mothers received first trimester care. In almost all cases (95%), the week prenatal care began was indicated directly in the records. When that was not the case, we calculated the number of days between the date of the last menstrual period (LMP) and the date prenatal care began, and divided by 7. If both week care began and LMP were unavailable (<1% of cases), we imputed LMP by subtracting 280 from the estimated date of confinement.
4.2 Postnatal behaviors
Our three main outcome measures are whether the mother smoked cigarettes at the time of her 1 year follow-up interview, whether the child had at least 4 well-baby visits between the mother’s baseline and follow-up interviews, and whether the mother breastfed the child for at least 6 months. In the 1 year follow-up interview, the mother was asked if she had smoked cigarettes within the past month. If she responded affirmatively to that question, she was coded as smoking at follow-up. Over one quarter (27%) of the mothers in the sample reported smoking in the past month in their follow-up interviews (22% of those who received first trimester care, 33% of those with late care). These rates are in line with figures reported by Colman et al. (2003), based on 1993–1999 PRAMS data from ten states, indicating that about 22% of mothers smoked cigarettes 2–6 months postpartum.
The mother was also asked in the 1 year follow-up interview how many times (0, 1–3, or 4 or more times) the child had been seen by a doctor, nurse or other health care professional for a regular check-up or well-baby visit since the birth. Due to the wording of the question, we were not able to assess whether the infant had the 8 visits recommended by the AAP. Instead, we constructed a variable for 4 or more well-baby visits (vs. <4). The majority of the infants (94%) had at least four well-baby visits by the time of the mother’s follow-up interview. This figure, although not entirely comparable, appears consistent with PRAMS data for 19 reporting states in 2000 indicating that between 75 and 90% of infants received a “sufficient” number of well-baby visits.Footnote 2
Finally, the mother was asked in the 1 year follow-up interview if she ever breastfed the child and if so, for how long. The AAP recommends exclusive breastfeeding for the first 6 months of the child’s life (AAP 2005). We use that threshold to define our outcome—breastfed for at least 6 months. Less than one quarter (21%) of the mothers in the sample breastfed for that long. This figure compares unfavorably with national statistics, which indicate that in 1999 almost one-third of women breastfed for 6 or more months,Footnote 3 and likely reflects the unique characteristics of the FFCWB sample (see sociodemographic profile below).
4.3 Covariates
We include an extensive set of sociodemographic characteristics in our models, all from the baseline survey. These include maternal age (<20 years, 20–34 years, and 35 or more years, with 20–34 years as the reference category), marital status (married, cohabiting but not married, and neither married nor cohabiting, with the last as the reference category), race/ethnicity (non-Hispanic white, Hispanic, non-Hispanic black, and other, with non-Hispanic black as the reference category), education (less than high school graduate, high school graduate, some college, and college graduate, with less than high school graduate as the reference category), nativity (whether the mother was born outside of the United States), employment (whether the mother had been employed at all during the 2 years prior to the birth), health insurance status (whether the birth was covered by Medicaid or other public health insurance), parity (whether this was the mother’s first birth), and the father’s education (whether the father had less than a high school education). We also control for length of time (in years) between the mother’s baseline and follow-up interviews.
By design, only one quarter (23%) of the mothers were married at the time of the birth. Forty percent of the mothers in the sample were cohabiting with, but not married to, the biological father of the child at the time of the birth and over one-third (37%) were neither married nor cohabiting. The oversampling of non-marital births resulted in a sample that is largely minority and poor. About half (45%) of the mothers were non-Hispanic black and 30% were Hispanic. The education levels were low—over one-third (35%) of the mothers had not completed high school and another third (30%) had only a high school education. Most of the mothers worked at some time during the 2-year period preceding the child’s birth (81%). About two-thirds (64%) of the births were covered by public insurance, reflecting the fact that a large proportion of the sample is poor or near poor.
We include prenatal smoking in our models, but later assess the sensitivity of our results to the inclusion of that variable. Eighteen percent of the mothers reported in their baseline interviews that they had smoked cigarettes at all during the pregnancy. Most mothers (1,621 mothers, or 71% of the sample) reported not smoking both at baseline (pertaining to the prenatal period) and at the 1 year follow-up. Of the mothers who did smoke, 367 (16% of the sample) reported smoking in both time periods, 245 (11%) reported smoking at 1 year but not during pregnancy, and 50 (2%) reported smoking during pregnancy but not at 1 year (not shown in tables). Our measure of prenatal smoking is similar to national estimates, which indicate that 19% of pregnant women report smoking in the past month.Footnote 4
The maternal health endowment (HE in Eq. 4b*) is a theoretically important (but frequently unobserved) variable, as it may affect both the timing of prenatal care initiation and the decision to engage in postnatal health promoting (or reducing) behaviors vis-à-vis the child. With the medical record data, we were able to characterize the maternal health endowment with three different variables: The first is whether the mother had documentation of any pre-existing (prior to the first prenatal visit) physical health condition (including chronic lung disease, cardiac problems, chronic diabetes, and pre-existing hypertension) in her hospital medical record (22% of the sample). The second is whether the mother had a diagnosed mental illness prior to the first prenatal visit (11% of the sample). Specifically, the mother was coded as having a pre-existing mental illness if there was any documentation of a diagnosed mental disorder (e.g., depression, anxiety, bipolar disorder, schizophrenia, anorexia, suicidality, or mental retardation). Having any diagnosis may be related to health care use, and recent research indicates that individuals with mental health conditions are more likely to smoke and less likely to quit than those who do not have mental health problems (Lasser et al. 2000). As such, mental illness is a particularly important covariate in our models. The third measure of maternal health endowment, also taken from the mother’s hospital medical record, is whether the mother had previously delivered a preterm, low birthweight, or small-for-gestational age infant (9% of the sample).
Another variable that both economic theory and past research suggest would affect both prenatal care timing and postnatal health behaviors is the wantedness of the child. This variable is generally unobserved and would therefore be in the error term, μ, of the postnatal input model. Some studies have attempted to measure wantedness and assess its effect on prenatal input use. Joyce and Grossman (1990), Joyce et al. (2002) and Reichman et al. (2009) all found significant effects of wantedness, as they characterized it, in hypothesized directions.Footnote 5 Wantedness may also affect postnatal infant health promotion. During the baseline FFCWB interview, the mother was asked if she had considered having an abortion rather than carrying the pregnancy to term. Over one quarter (29%) of the mothers reported that they had considered having an abortion. We created a variable for whether the mother considered abortion as our measure of wantedness, but recognize that it may in fact reflect a different sentiment. For example, it is possible that women who consider having an abortion are particularly thoughtful about the pregnancy and its implications and that their children end up being as wanted as those to mothers who did not consider abortion. That said, past research using this same measure indicates that women who considered abortion were more likely to use negative prenatal inputs (cigarettes and illicit drugs) and initiate prenatal care late in the pregnancy than those who did not consider abortion (Reichman et al. 2009). Thus, prior research is consistent with the notion that having considered an abortion indicates, in general, a lower willingness to invest in the child.
Compared to mothers who initiated prenatal care after the first trimester of pregnancy, mothers who received first trimester care were less likely to be teenagers (15 vs. 23%), more likely to be married (30 vs. 15%), more likely to have attended or completed college (41 vs. 28%), less likely to have publicly insured births (57 vs. 73%), and much less likely to have considered abortion (22 vs. 38%) and to have smoked during pregnancy (15 vs. 23%). They also lived closer, on average, to the hospitals in which they gave birth and had a slightly higher average income eligibility threshold for pregnant women in their state’s Medicaid program (these two measures will be discussed later in the context of our bivariate probit models).
In supplemental analyses, we included several measures of non-health related parenting behavior, measured at 1 year. Positive parenting behaviors included whether the mother reported that she engages in the following activities with the child every day: playing games, singing, reading, telling stories, playing with toys, and hugging. We also included a negative parenting behavior—whether the mother reported that she spanked the child in the past month.
5 Multivariate analysis
We apply a multi-pronged approach with the goal of obtaining unbiased estimates of the effects of first trimester care on maternal postpartum behaviors. First, we rely on rich and well-measured data and conduct numerous robustness checks. We control for factors that few studies have been able to incorporate directly and which both economic theory and empirical research suggest are potential sources of unobserved heterogeneity (e.g., maternal health endowment and wantedness of the child). We use a measure of first trimester prenatal care that was constructed from information in the mother’s obstetrical records, which are designed to collect this information; our models are therefore not subject to biases stemming from the overreporting of first trimester prenatal care (Reichman et al. 2009). We assess sensitivity of the estimates to variable construction, model specification, and sample composition. Second, we conduct a series of “falsification tests” by estimating the effects of prenatal care on non-health related parenting behaviors, such as reading to the child and spanking, that prenatal care is not designed to affect. Our third approach, described in more detail later, is to estimate bivariate probit models to test for the potential endogeneity of prenatal care.
Table 2 presents estimates from probit models of the effects of first trimester prenatal care on the postnatal behaviors of interest—cigarette smoking at 1 year, 4 or more well-baby visits, and breastfeeding for 6 months or more. Each cell contains the probit coefficient on top, the marginal effect in brackets, and the standard error of the probit coefficient, which is corrected for city clustering of observations using the Huber–White method, in parentheses. The estimates for first trimester prenatal care suggest that early initiation of prenatal care confers postnatal benefits to children. We find that mothers who begin prenatal care in the first trimester of pregnancy are 5 percentage points less likely than mothers who initiate care later to smoke 12–18 months after the birth, all else equal. This translates to a postpartum smoking reduction of 19% relative to the sample mean. In addition, mothers who initiate prenatal care in the first trimester are 1 percentage point more likely to take their infant for 4 or more well-baby visits. We find no significant association between first trimester prenatal care and breastfeeding for 6 months or more. In supplementary models (results not shown in tables), we assessed the sensitivity of the results to the 6 month cutoff for our breastfeeding outcome. We estimated models with the following alternative outcomes: breastfeeding for at least 1 month, for at least 2 months, for at least 3 months, for at least 4 months, and ever, as well as the number of weeks the baby was breastfed. No matter how breastfeeding was defined, it was never significantly associated with first trimester prenatal care in our single-equation probit models.
There are strong racial and ethnic differences in smoking, with non-Hispanic black and Hispanic mothers being much less likely than their non-Hispanic white counterparts to smoke at 1 year. As expected, marital status and maternal education are strong predictors of postnatal health-promoting behaviors. Compared to mothers who were neither married to nor cohabiting with the father of their child at the time of the birth, those who were married were 8 percentage points less likely to smoke at 1 year and 10 percentage points more likely to breastfeed the child for at least 6 months. Mothers who were college graduates were 15 percentage points less likely to smoke, 3 percentage points more likely to take the infant for 4 or more well-baby visits, and 21 percentage points more likely to breastfeed their infant for 6 months or more, compared to mothers with less than a high school education. With each defined increment of education, the likelihood that the mother engaged in each of the three health-promoting behaviors increased.
As expected, prenatal smoking is a very strong predictor of postnatal smoking. Mothers who smoked during pregnancy were 70 percentage points more likely than those who did not smoke during pregnancy to smoke at follow-up. Another significant predictor of postnatal smoking is pre-existing mental illness. This result is unsurprising, given the findings of Lasser et al. (2000) referenced earlier. Although mothers with a history of mental illness are more likely to smoke, we find no evidence that they are less likely to take their child to the doctor or to breastfeed.
5.1 Specification checks
We conducted supplemental analyses to assess the robustness of our estimates to alternative measures of key analysis variables.Footnote 6 First, compared to the other two outcomes, breastfeeding is less conceptually linked to early prenatal care. For example, breastfeeding discussions may be most effective late in the pregnancy, as the birth becomes more imminent. In contrast, smoking cessation efforts are likely to commence as soon as the mother shows up for care, and the habit of using health care may become more engrained the earlier one starts. We thus re-explored the lack of effects on breastfeeding by estimating models (corresponding to those in Table 2) using first or second trimester care (92% of the sample), versus third trimester or no care, instead of first trimester care.Footnote 7 The effects remained insignificant. Second, we estimated models predicting postnatal smoking, well-baby visits and breastfeeding that used an alternative measure of prenatal smoking—whether the mother smoked one pack or more of cigarettes per day (rather than whether she smoked cigarettes at all). The effects of first trimester prenatal care on whether the infant had four or more well-baby visits and was breastfed for at least 6 months did not change, but the effect of first trimester prenatal care on postpartum smoking increased in magnitude and was highly significant. Third, we estimated models using alternative measures of prenatal care—weeks of prenatal care delay, the Adequacy of Prenatal Care Utilization Index, and the Graduated Index-Revised. The latter two measures, which take into consideration not only the timing of prenatal care initiation, but also the number of prenatal visits given the gestational age of the infant at birth, are described in detail in Alexander and Kotelchuck (1996). For postnatal smoking, we found that both the magnitude and the significance of the prenatal care variables were consistent with those when we used first trimester care as our prenatal care variable. For well-baby visits, the alternative measures of prenatal care had the correct sign, but both the magnitude and significance were lower than when using first trimester care. For breastfeeding, prenatal care remained insignificant when using the alternative measures.
We estimated another set of supplemental models to assess the robustness of our estimates to the selection of covariates. First, we ran parsimonious models that included only variables typically found in nationally representative data sets (mother’s age, marital status, race/ethnicity, education, employment, and nativity, as well as first birth and time between baseline and follow-up interviews). For postpartum smoking and well-baby visits, first trimester prenatal care was significant and of the expected sign. The magnitude of the effect for well-baby visits was similar to the corresponding estimate in Table 2, but that for smoking was much greater than the corresponding Table 2 estimate. For breastfeeding, the effect of prenatal care remained insignificant. Second, we estimated models with all of the covariates from Table 2 except prenatal smoking. Again, there was no significant effect of prenatal care on breastfeeding. The estimate for well-baby visits was similar to the corresponding estimate in Table 2, but that for postpartum smoking was much greater than the corresponding Table 2 estimate. Third, we estimated models with all covariates from Table 2 plus the following variables, all measured at baseline: the infant’s gender, whether the mother lived with both of her parents when she was 15 years old, whether the mother regularly attended religious services, whether the mother was obese prior to pregnancy, whether the infant was born weighing less than 2,500 g, the father’s age, whether the father smoked cigarettes, and state indicators. Maternal obesity was derived from the hospital medical records; all other supplementary variables were from the baseline interview. The estimated effects of first trimester prenatal care on maternal postpartum behaviors were very similar to the corresponding estimates in Table 2. Finally, because wantedness of the child is very difficult to characterize (as discussed previously), we estimated models that excluded the “considered abortion” measure and found no changes in the estimated effects of prenatal care on maternal behaviors.
We also restricted the sample to the 1,866 mothers who reported that they did not smoke during pregnancy. The effect of prenatal care on breastfeeding remained insignificant and the effect of first trimester prenatal care on four or more well-baby visits had the same magnitude as in Table 2 and was statistically significant. For postnatal smoking, the effect of first trimester prenatal care was negative and significant, but the magnitude was reduced, from 5 to 3 percentage points. The latter result is not surprising, since most prenatal non-smokers are unlikely to take up smoking. However, some of the mothers who did not smoke during pregnancy did subsequently initiate or resume smoking after they gave birth, and we found evidence that early prenatal care made this less likely.
Finally, we performed auxiliary models for specific subgroups of women to further explore the robustness of the estimated effect (zero) of first trimester care on breastfeeding. Because the WIC program subsidizes infant formula, it may be difficult to persuade poor women to breastfeed. If education allows women to better understand the benefits of breastfeeding, then prenatal breastfeeding education might be effective only for more highly educated women. Breastfeeding can be difficult and may depend on having social support. Finally, breastfeeding might be more difficult for women who work, and low-income women have faced substantial pressures to work since welfare reform.Footnote 8 In that sense, breastfeeding may be less of a choice variable for poor women. To explore these issues, we estimated models for women who participated in WIC after the birth, lived in poor census tracts (less than 30% poor) at baseline, had at least some college education at the time of the birth, worked (at all) during the first year of the baby’s life, and had private insurance at the time of the birth. As indicated earlier, we also ran models that included baseline religious attendance, which may be a proxy for social support. In all cases, we found no effect of first trimester prenatal care on breastfeeding.
5.2 Falsification tests
To investigate a competing explanation for our findings—that mothers who are the most interested in their children’s well-being will both get early prenatal care and engage in favorable parenting practices, we estimated the effects of first trimester prenatal care on parenting behaviors that prenatal care was not designed to affect. If the mother’s dedication to parenting is an important unobserved confounder, we would expect early prenatal care to predict non-health related parenting behaviors, such as reading to the child and spanking. As indicated earlier, at 1 year the mothers were asked how often they engaged in each of the following positive parenting behaviors with their child each week: playing games, singing, reading stories, telling stories, playing with toys, and hugging. In addition, they were asked how often they spanked the child. We estimated models corresponding to those in Table 2 for each of these parenting behaviors, characterized a number of different ways including in combinations. In both linear regressions and probit models, we found that first trimester prenatal care was never a significant predictor of any of the non-health related parenting behaviors.Footnote 9 The contrast in findings for the non-health related parenting behaviors (which are not focuses of prenatal care) and the health related parenting behaviors (which are specific focuses of prenatal care) adds to the evidence that our findings vis-à-vis the health behaviors represent causal effects.Footnote 10
5.3 Bivariate probit models
To test whether the observed associations between timing of prenatal care initiation and maternal behaviors represent unbiased estimates, we ran bivariate probit models. Distance (in kilometers) from the mother’s residence at the time of the birth to the hospital in which she gave birth (calculated using the spatial coordinates in the data)Footnote 11 and the state Medicaid income eligibility threshold for pregnant women as a percentage of the federal poverty line (National Governors Association 1997) were used as identifiers for first trimester prenatal care. Both represent access to prenatal care.Footnote 12
The test results, shown with the full bivariate probit results in the “Appendix”, reveal that (1) the two identifiers are jointly significant predictors of first trimester care for all outcomes, (2) the two identifiers are excludable from the behavioral outcome equations, and (3) the error terms in the prenatal care equation are not significantly correlated with the error terms in either the smoking or well-baby visits equations.Footnote 13 These results suggest that our single equation estimates of the effects of prenatal care on postpartum smoking and well-baby visits are not biased.Footnote 14 However, the situation for breastfeeding is more complicated. While the single equation estimates were extremely robust (indicating no association between prenatal care and breastfeeding), the bivariate probit estimates indicate some unobserved heterogeneity (rho is negative and significant) and that first trimester care has a positive effect on breastfeeding. This finding is robust to the definition of prenatal care and to the inclusion of alternative sets of covariates and identifiers.Footnote 15 In other words, there appear to be unobserved factors that are positively correlated with breastfeeding but negatively correlated with early prenatal care. However, it is not obvious what those factors might be, and the bivariate probit estimate of the effect of first trimester care on breastfeeding is not estimated with precision. For these reasons, we are cautious in our inferences about the effects of prenatal care on breastfeeding. There may be a positive effect, but it is only apparent in bivariate probit specifications.
5.4 Recap
The estimated effects of first trimester prenatal care on maternal postpartum smoking and well-baby visits are extremely robust. Not surprisingly, the effects of prenatal care on postnatal smoking are larger when the baseline control is smoking a least a pack a day (instead of at all) and when prenatal smoking is not included in the model at all, and smallest when restricting the sample to mothers who did not smoke at all during pregnancy. Bivariate probit models indicate that the single-equation estimates of the effects of prenatal care on maternal postpartum smoking and well-baby visits are unbiased. Single-equation probit estimates of the effects of prenatal care on breastfeeding are very robust and show no association between the two behaviors, but bivariate probit models suggest that there is unobserved heterogeneity and a positive (although imprecisely estimated) effect of prenatal care.
6 Conclusion
As far as we know, this is the first study in the economics literature to investigate the effects of prenatal care on maternal postpartum parenting behaviors. We used population-based data from a national birth cohort study and found that early prenatal care appears to have favorable effects on maternal postpartum behaviors that are directly relevant to children’s health. Specifically, first trimester prenatal care appears to decrease the likelihood that a mother smokes cigarettes 12–18 months after giving birth, by about 5 percentage points, and increase the likelihood that the infant receives at least four well-baby visits, by about 1 percentage point. The effects on breastfeeding are more ambiguous. We addressed the potential endogeneity of prenatal care in a number of different ways, none of which is perfect but that together paint a robust and consistent picture for postpartum smoking and well-baby visits. More research needs to be done to explore the sources of unobserved heterogeneity vis-à-vis prenatal care and breastfeeding.
The insignificant associations between prenatal care and breastfeeding found in the single equation models should not be interpreted to mean that prenatal interventions have no effects on breastfeeding. First, the bivariate probit estimates suggest that there are suppressed effects in the probit models. Second, we focused on timing of prenatal care as it is practiced at the population level rather than on the specific content of that care. Indeed, Lu et al. (2001) found that mothers who reported that their physicians and nurses encouraged them to breastfeed were significantly more likely to initiate breastfeeding, and as reported earlier, Kistin et al. (1989) found, in a randomized controlled trial, that prenatal breastfeeding education and counseling increased rates of breastfeeding among urban, black low-income women—a group very similar to the population we studied. Thus, it is certainly possible that the mothers in our sample who were most encouraged by their prenatal care providers to breastfeed (and we cannot measure this) were more likely than the others to engage in that behavior.
The findings from this study suggest that there are benefits to standard prenatal care that are generally not considered in evaluations of prenatal care programs and interventions—that earlier care increases the likelihood that mothers will engage in health-promoting behaviors and refrain from health-compromising behaviors during the first year of their child’s life. These behaviors are important investments in the health and development of children and have life course implications. For example, recent work by Chay et al. (2009) highlights the importance of health care for post-neonates, demonstrating that better early health care leads to higher achievement levels into adulthood.
This study broke new ground by being the first on the topic, but it is important that the findings be replicated and further explored. That said, the results underscore both the potentially important opportunity that prenatal care presents for providing parenting and health education and the need for additional research on the effects of prenatal care on maternal behaviors and child health.
Notes
That is, we allow maternal health (and its effects) to vary over time. For example, a maternal behavior during the pregnancy, such as smoking, could have an impact on the health of the fetus (above and beyond the impact of the mother’s initial health endowment) plus it could also impact the current health of the mother.
"Sufficient" visits are defined as 2 or more checkups by 2–3 months (60–122 days) of age; 3 or more checkups by 4–5 months (123–183 days) of age; or 4 or more checkups by 6–9 months (184–274 days) of age. Data reported at: http://www.cdc.gov/PRAMS/2002PRAMSSurvReport/MultiStateExhibits/Multistates17.htm.
National data are based on the Center for Disease Control’s National Immunization Survey, reported at: http://www.cdc.gov/breastfeeding/data/NIS_data/index.htm.
Source: National Household Survey on Drug Abuse, 2000. http://www.oas.samhsa.gov/nhsda/2kdetailedtabs/Vol_1_Part_4/sect6v1.htm#6.23b.
These studies measured wantedness in different ways, but in all cases it is possible that the measures used reflect factors other than intended investment in the child (for example, Joyce and Grossman (1990) discuss the possibility that their measure may reflect, in part, the cost of contraception). In addition, wantedness may not be a fixed sentiment, but may vary over time, as discussed by Joyce et al. (2002).
Results from supplemental analyses are not shown, but are available upon request.
There were too few cases of no prenatal care (14) to analyze the effects of any prenatal care.
Kimbro (2006) found that low-income women have substantial difficulty combining work and breastfeeding in the post-welfare reform era.
Sample sizes were smaller than those in Table 1 when including telling stories, playing with toys, and hugging, which were assessed in only 18 of the 20 FFCWB cities. For the continuous regressions, the value varied from 0 to 7 days per week. For the dichotomous variables, we set the dependent variable equal to 1 if the mother engaged in the activities daily. These results are available upon request.
We also estimated models that included the non-health related parenting measures on the right hand side in addition to all of the other covariates, as those factors might account for some of the potential unobserved heterogeneity across mothers vis-à-vis parenting and health behaviors. We found that including non-health related parenting behaviors affected the estimates of prenatal care on health-related parenting behaviors in only one case--when combining the former into a measure of activities that enhance the child's cognitive development (singing, telling stories, reading stories and playing with toys) and predicting four or more well-baby visits. In that case, the estimated effect of prenatal care became insignificant. However, we cannot rule out a scenario in which mothers are encouraged in the course of pediatric care to engage in those activities (reverse causality).
To test for the possibility that proximity to hospital is an important choice variable rather than exogeneous source of prenatal care availability, we predicted distance to birth hospital as a function of the right-hand side variables from Table 2 (other than first trimester prenatal care) plus state indicators. The only variables that significantly predicted distance to hospital at conventional levels were the state indicators. These estimates suggest that proximity to a hospital is not an important factor in women’s residential location decisions.
The Wald test of the hypothesis that rho = 0 yields chi-square statistics of .37 for smoking and .07 for well-baby visits, which are statistically insignificant. Thus, for these outcomes we cannot reject the null hypothesis of zero correlation between the error terms in the prenatal care and outcome equations.
As an alternate specification, we estimated linear probability models, which produced results similar to those of the probit models.
All bivariate probit estimates were insensitive to alternative identifiers (e.g., state Medicaid to Medicare fee ratios for obstetric services or Medicaid fees for vaginal deliveries instead of Medicaid eligibility thresholds). Data were obtained from Norton (1999).
References
Alexander, G., & Kotelchuck, M. (1996). Quantifying the adequacy of prenatal care: A comparison of indices. Public Health Reports, 111, 408–418.
American Academy of Pediatrics. (2005). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506.
American Academy of Pediatrics. (2008). Recommendations for pediatric health care. http://pediatrics.aappublications.org/cgi/data/120/6/1376/DC1/1.
Chay, K. Y., Guryan, J., & Mazumder, B. (2009). Birth cohort and the black-white achievement gap: The roles of access and health soon after birth. National Bureau of Economic Research working paper 15078.
Colman, G., Grossman, M., & Joyce, T. (2003). The effect of cigarette excise taxes on smoking before, during and after pregnancy. Journal of Health Economics, 22(6), 1053–1072.
Conway, K. S., & Kutinova, A. (2006). Maternal health: Does prenatal care make a difference? Health Economics, 15(5), 461–488.
Corman, H., Joyce, T. J., & Grossman, M. (1987). Birth outcome production function in the United States. Journal of Human Resources, 22(3), 339–360.
Currie, J., & Reagan, P. B. (2003). Distance to hospital and children’s use of preventive care: Is being closer better, and for whom? Economic Inquiry, 41(3), 378–391.
Dolan-Mullen, P., Ramirez, G., & Groff, J. Y. (1994). A meta-analysis of randomized trials of prenatal smoking cessation interventions. American Journal of Obstetrics and Gynecology, 171, 1328–1334.
Evans, W. N., & Lien, D. S. (2005). The benefits of prenatal care: Evidence from the PAT bus strike. Journal of Econometrics, 125, 207–239.
Fang, W., Goldstein, A., Butzen, A., Hartsock, S., Hartmann, K., Helton, M., et al. (2004). Smoking cessation in pregnancy: A review of postpartum relapse prevention strategies. Journal of the American Board of Family Practice, 17, 264–275.
Freed, G., Clark, S., Pathman, D., & Schectman, R. (1998). Influences on the receipt of well-child visits in the first two years of life. Pediatrics, 103, 864–869.
Gray, B. (2001). Do Medicaid physician fees for prenatal services affect birth outcomes? Journal of Health Economics, 20(4), 571–590.
Ip, S., Chung, M., Raman, G., Chew P., Magula, N., DeVine, D., et al. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evidence report/technology assessment report 153, US Department of Health and Human Services, agency for healthcare research and quality; 2007. Available at http://www.ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf.
Joyce, T. J., & Grossman, M. (1990). Pregnancy wantedness and the early initiation of prenatal care. Demography, 27(1), 1–17.
Joyce, T. J., Kaestner, R., & Korenman, S. (2002). On the validity of retrospective assessments of pregnancy intention. Demography, 39(1), 199–213.
Kimbro, R. T. (2006). On the job moms: Work and breastfeeding initiation and duration for a sample of low-income women. Maternal and Child Health Journal, 10(1), 19–26.
Kistin, N., Benton, D., Rao, S., & Sullivan, M. (1989). Breast-feeding rates among black urban low-income women: Effect of prenatal education. Pediatrics, 86, 741–746.
Klesges, L. M., Johnson, K. C., Ward, K. D., & Bernard, M. (2001). Smoking cessation in pregnant women. Obstetrics and Gynecology Clinics of North America, 28, 269–282.
Kogan, M., Alexander, G., Jack, B., & Allen, M. (1998a). The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United States. Pediatrics, 102, 25–30.
Kogan, M. D., Martin, J. A., Alexander, G. R., Kotelchuck, M., Ventura, S. J., & Frigoletto, F. D. (1998b). The changing pattern of prenatal care utilization in the United States, 1981–1995, using different prenatal care indices. Journal of the American Medical Association, 279, 1623–1628.
Lasser, K., Boyd, J. W., Woolhandler, S., Himmelstein, D. U., McCormick, D., & Bor, D. H. (2000). Smoking and mental illness a population-based prevalence study. Journal of the American Medical Association, 284(20), 2606–2610.
Lia-Hoagberg, B., Rode, P., Skovholt, C. J., Oberg, C. N., Berg, C., Mullett, S., et al. (1990). Barriers and motivators to prenatal care among low-income women. Social Science and Medicine, 30(4), 487–495.
Lu, M., Lange, L., Slusser, W., Hamilton, J., & Halfon, N. (2001). Provider encouragement of breast-feeding: Evidence from a national survey. Obstetrics and Gynecology, 97(2), 290–295.
Lu, M., Tache, V., Alexander, G., Kotelchuck, M., & Halfon, N. (2003). Preventing low birth weight: Is prenatal care the answer? Journal of Maternal and Fetal Neonatal Medicine, 13, 362–380.
March of Dimes. (2009). During your pregnancy: Prenatal care. Pregnancy and newborn health education center. http://www.marchofdimes.com/pnhec/159_513.asp.
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Menacker, F., & Kirmeyer, S. (2009). Births: Final data for 2006. National Vital Statistics Reports, 57(7). National center for health statistics. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_07.pdf.
Melvin, C., Dolan Mullen, P., Windsor, R. A., Whiteside, H. P., & Goldenberg, R. L. (2000). Recommended cessation counseling for pregnant women who smoke: A review of the evidence. Tob Control, 9, III80–III84.
National Governors Association, Health Policy Studies Division, NGA Center for Best Practices. (1997). MCH Update: State Medicaid coverage of pregnant women and children. Available at: http://www.nga.org/cda/files/MCHUPDATE0997.pdf.
Norton, S. (1999). Recent trends in Medicaid physician fees 1993–1998. Urban institute discussion paper. Available at: http://www.urban.org/url.cfm?ID=409113.
Reichman, N. E., Corman, H., Noonan, K., & Dave, D. (2009). Infant health production functions: What a difference the data make. Health Economics, 18(7), 761–782.
Reichman, N. E., & Teitler, J. O. (2005). Timing of enhanced prenatal care and birth outcomes in New Jersey’s HealthStart program. Maternal and Child Health Journal, 9(2), 151–158.
Reichman, N. E., Teitler, J. O., Garfinkel, I., & McLanahan, S. (2001). Fragile families: Sample and design. Children and Youth Services Review, 23, 303–326.
Schappert, S. M. (1997). Ambulatory care visits to physician’s offices, hospital outpatient departments, and emergency departments: United States, 1996. Vital Health Stat, 13, 1–37.
US Department of Health, Human Services. (1989). Caring for our future: The content of prenatal care, a report of the public health service expert panel on the content of prenatal care. Washington, DC: US Public Health Service, Dept of Health and Human Services.
US Department of Health, Human Services. (2006). The health consequences of involuntary exposure to tobacco smoke: A report of the surgeon general. Atlanta Georgia: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Williams, L., Morrow, B., Shulman, H., Stephens, R., D’Angelo, D., & Fowler, C. I. (2006). PRAMS 2002 surveillance report. Atlanta, GA: Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention.
Acknowledgements
This research was supported by grants R03HD057230 and R01HD45630 from the National Institute of Child Health and Human Development. The authors are grateful to Shin-Yi Chou for helpful comments and Prisca Figaro for research assistance.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Reichman, N.E., Corman, H., Noonan, K. et al. Effects of prenatal care on maternal postpartum behaviors. Rev Econ Household 8, 171–197 (2010). https://doi.org/10.1007/s11150-009-9074-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11150-009-9074-5