Abstract
Purpose
Psychosexual distress is known to be a common complication of treatment for gynaecological cancer (GC), affecting the sexual quality of life (SQoL) for an increasing number of young gynaecological cancer survivors (YGCS). The SQoL in YGCS study aimed to identify strategies that are acceptable and helpful to YGCS in protecting and improving SQoL, using a salutogenic approach.
Methods
A qualitative study was undertaken with young women aged 18–45 and pre- or perimenopausal at diagnosis. Semi-structured interviews were conducted on Zoom and a thematic analysis of transcripts was completed in NVivo.
Results
Fifteen interviews with YGCS revealed three themes for strategy development: psychosexual education, psychosocial support, and healthcare policy and strategy to establish SQoL as standard care in gynaecologic oncology.
Conclusion
The strategies put forward by YGCS showed the need for a holistic, patient-centric, and multidisciplinary approach to SQoL. A better understanding of the strategies acceptable to YGCS, including the importance of using a trauma-informed approach to communication and care, can help healthcare providers play a vital role in protecting and improving SQoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
After going through treatment for gynaecological cancer, many younger survivors face emotional challenges related to their sexuality. This can have a big impact on their overall sexual well-being. In this study, we talked to fifteen young gynaecological cancer survivors to find out what could help them feel better about their sexual lives. They shared three important ideas: giving patients more information, having a support system of friends and family, and making sure that sexual well-being is a regular part of gynaecological cancer care. These suggestions from survivors show that healthcare experts should work together to support every aspect of a person’s journey through cancer, from diagnosis to treatment and beyond. By recognising the difficult experiences that come with cancer and its treatment, healthcare providers can play a crucial role in helping survivors feel better about their sexual well-being.
Introduction
All cancers may lead to psychological and interpersonal issues, yet cancers of the female reproductive system often also interfere with women’s fertility, sexuality, body image and identity [1,2,3]. Despite the high prevalence of post-treatment sexual complaints and increasing evidence for the need to integrate sexuality into standard care [4,5,6,7], sexual quality of life (SQoL) continues to be inadequately addressed in gynaecologic oncology. The literature on SQoL interventions for gynaecological cancer survivors (GCS) is scarce. In fact, a recent systematic review [8] found gaps in the evidence for psychosexual interventions specific to gynaecological cancer (GC). In their study, Beesley and colleagues [8] supported earlier findings from Flynn, Kew, and Kisely [9], who found that the literature on interventions for psychosexual dysfunction in women treated for gynaecological malignancy is limited, and existing studies are often of poor methodological quality.
Psychosexual distress is particularly common among younger gynaecological cancer survivors [7, 10, 11], yet we do not know how to intervene. The lack of evidence on what strategies might work with the younger GCS community is significant because the types and levels of needs vary across age, with younger individuals reporting greater unmet needs and poorer adaptation to cancer [2, 12]. Furthermore, YGCS want help dealing with sexual and psychological difficulties [13, 14] but report practical and emotional concerns as barriers to receiving help [15].
Understanding the lived experiences and recommendations of YGCS may help deliver cancer care and support services that are relevant to them. The aim of the Sexual Quality of Life in Young Gynaecological Cancer Survivors research was twofold: 1) to understand the lived experience of YGCS and 2) to identify strategies for protecting and improving SQoL that are acceptable and helpful to YGCS. A previously published article [7] reported on the first aim; understanding the lived experience of YGCS, and this article reports on the strategies identified.
Methods
Study design
We conducted a qualitative study of young adult women living in Australia who had been diagnosed with GC. Young age was defined as, at the time of diagnosis, 1) being aged 18–45 years old and 2) being pre- or peri-menopausal (i.e., at least 2 menstrual periods within 6 months of diagnosis). Exclusion criteria were recurrence of GC, inability to participate in an online interview due to a medical condition, insufficient English, or lack of access to a smartphone or computer with a reliable internet connection. Before conducting individual semi-structured interviews on Zoom, we carried out three pilot interviews with YGCS. Although the data from these pilot interviews was not incorporated into the final dataset, they played a crucial role in a) refining the interview schedule, b) establishing that an online interview was adequate to address sensitive topics, and c) verifying that scheduling 60–90 min per interview was sufficient. The first author conducted all interviews using an interview guide that had been developed in collaboration with all the co-authors. An illustrative question from the interview guide is: ‘Is there anything that you feel was (or would have been) helpful in managing the impact of cancer and its treatment on your sexuality?’ This question aimed to investigate participants' insights into strategies, experiences, resources, support, information, or recommendations. The research was approved by The UniSC Human Research Ethics Committee (S201448). As this study is part two of a two-part study, the methods and data collection processes have been fully reported in the previously published article [7].
Data analysis
Participant characteristics were collected in Qualtrics [16], analysed in Excel and represented as descriptive statistics. Interviews were transcribed verbatim. A thematic analysis [17], following the steps recommended by Braun and Clarke [18], was used to code interview transcripts in NVivo Version 1.5 [19]. Through this systematic process, the first author used both written interview transcripts and audio recordings to become intimately familiar with the data set’s content and reflect on what the data meant [18]. Special attention was given to strategies for protecting or improving SQoL, in line with the study’s goal.
The words and phrases used by participants were organised using an inductive analysis approach to create initial codes. Braun and Clarke [18] describe the process of identifying themes as an active process, explaining that themes do not spontaneously emerge; instead, researchers make deliberate decisions about the meaning of the data. In this context, the first author actively sought patterns within the data that could signify strategies for approaching SQoL. These codes were then organised into code clusters, using a deductive data analysis approach, guided by our previous research on the factors of SQoL for GC [20] and Salutogenic Theory [21]. The coded clusters were developed into the strategies for SQoL themes reported in this article. Data analysis was conducted by the first author and peer-reviewed by the co-authors. Quality control was carried out using the Critical Appraisal Skills Programme (CASP) checklist for qualitative studies [22]. The checklist comprises 10 statements designed to evaluate various aspects, including the suitability of the research aim and methods, the validity of the results, the contribution the study makes to existing knowledge, and the applicability of the findings to other populations.
Results
Participant characteristics
Fifteen participants from various regions across Australia, diagnosed with cervical (n = 8) and ovarian (n = 7) cancer, joined the SQoL in YGCS study. The distribution of participants across FIGO stages was as follows: Stage I (n = 5), Stage II (n = 5), Stage III (n = 2), and Stage IV (n = 3). Our analysis revealed that the data collected from fifteen participants was sufficient to reach theoretical sufficiency to meet the study’s goal [23]. In this context, it implies that the collected data provided researchers with a substantial level of insight, enabling them to identify themes that could inform strategic recommendations for YGCS.
Among participants, all were cisgender women with heterosexual orientation, except for one participant who was in a same-sex relationship. The study encompassed both single and partnered women, with six of them reporting a change in their partner or relationship status since their cancer diagnosis. The SQoL in YGCS study also included participants with diverse 'time since diagnosis': 1 year or less (1 participant), 2–3 years (5 participants), 4–5 years (4 participants), 6–7 years (2 participants), and more than 8 years (3 participants). Participants reported their age at diagnosis, with 2 participants aged 18–24 years, 8 participants aged 25–31 years, 4 participants aged 32–38 years, and 1 participant aged 39–45 years. Five participants were still receiving cancer treatment and nine were not, one did not respond to that question. Cancer treatment included a combination of surgery, chemotherapy, radiotherapy, and hormonal therapy. Fourteen participants reported they were sexually active (defined as sexual contact or self-pleasure) at the time of the survey.
Theme 1: psychosexual education
A recurrent theme was the need for patient information and education, with YGCS reporting feeling ‘left in the dark’ (#3611). This section describes four subthemes that emerged under psychosexual education (Table 1): impact of cancer and treatment on SQoL, post-treatment care and psychosexual wellbeing, patient-doctor communication and self-advocacy, and partner communication and intimacy.
Predominantly, YGCS wanted to understand what treatment options were available, what adverse effects they may encounter on their SQoL, and where to find help to relieve trauma and post-treatment ailments.
It was never spoken about that there would be any impact on my sexuality or how I would feel. I was never offered any options to speak to a professional around how to still feel sexual after this. Just being upfront with what it means for your long-term sexual life would have been really useful. (#5137)
With respect to patient-communication and self-advocacy, YGCS expected doctors to initiate and normalise conversations around SQoL, “We already feel so abnormal. It’s a conversation that does need to come from your GP or your oncologist.” (#5453) For individuals who are uncomfortable talking about sexuality, take-home brochures could help ‘break the ice’ (#2967) and convey the message that help is available, “I think making them feel more comfortable or giving out a pamphlet saying, these are some of the things you may be feeling, feel free to bring up anything to me, I can refer you on to the specialists.” (#2318) Written information could also be used in combination with educational resources and follow-ups, “We had educational sessions with nurses at the cancer clinic. They would provide written information. Then the oncologist would check in as well.” (#3469) Healthcare providers were expected to ‘lead the care pathway’ (#2967), yet phrases such as ‘you’ve got to take ownership’ (#2788) and ‘I have to fight really hard to advocate for the recovery of my sex life and sexuality’ (#6260) explain the importance of providing YGCS with the tools and support they need to raise sexual concerns with healthcare professionals and become active participants in their health.
You’ve got to be in control. Not everything of what they say is going to be correct for you. They wanted to leave me with a catheter bag for six months. I was, ‘That’s not going to happen so what are my options?’. They were, ‘Oh, you can self-catheterise but it’s really hard’. I went, ‘Show me how to do it and I’ll make it work’. (#5166)
Moreover, the understanding that other young women share similar challenges may help break isolation and remove barriers in seeking help, “It’s very isolating. I’d like to see more information out there for younger women going through cancer. I feel like I still don’t know anyone else my age who’s gone through it.” (#2318) According to our participants, partners may also benefit from receiving practical information on how cancer treatment impacts SQoL, and what they can do to help.
Any support would have been helpful. I’ve been stumbling my way through it, trying to explain things to him, but I don’t think he understood the medications, or the effects on me, my body, and my sexuality. If they had a brochure for the partner to explain, ‘This is what your partner’s body could go through with menopause. This is how your partner might feel. This is what you can do to support them’. (#2318)
Younger couples may also value communication on new ways to express intimacy.
You hear the new normal a lot. It turns out that applies to your sex life as well, to be completely redefined. We've had to not compare aspects of life to what it used to be but evolving it into whatever is working for us. If there was a silver lining, it’s that we’re having to look into different ways of being intimate. That’s something exciting that could have been put in any communication given to us. (#6260)
Theme 2: psychosocial support
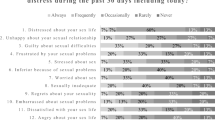
When it comes to sexuality, there isn’t one-size-fits-all, but psychosocial support might help improve SQoL, “Sexuality isn’t in a manual, there isn’t one right way. Surely, we can lean on each other. Information sharing is very important” (#3611). Three subthemes were identified (Table 2): expert-led peer support, partner involvement and support, and counselling for individuals and couples.
These themes highlighted that the lack of conversation and peer support dedicated to SQoL for YGCS contributed to psychosocial distress.
There isn’t much discussion about your life outside of the physical aspect of the body surviving. It’s easy to say you’re not alone, but when we don’t have platforms to reach out to each other, it’s very easy to feel alone. And yes, if there were platforms for us to connect, suggest, play and commiserate. (#4845)
Hence, peer-to-peer support could help address stigma around sexuality and GC when it offers a safe space for YGCS to share experiences, “I find it helpful because it removes any stigma around what the women are experiencing. I feel like everyone’s very respectful of each other's journeys and it’s a safe place to ask questions”. (#5137) However, participants had mixed feelings or negative experiences about unmonitored support groups. Some individuals found these groups triggered negative emotions and others felt it could be dangerous when diagnosis or treatment options are suggested by uneducated peers.
I did join a Facebook group. I left it, I found it really depressing. It needs to be done through the right avenues and not just people sitting around that are uneducated talking about a topic because that can get them stuck in ‘poor me’. It’s not healing, it’s not proactive. What about something potentially online for people remotely? (#9547)
Besides improving the accessibility of expert-led peer support, the needs of young women must be accounted for throughout the cancer journey, “I imagine the needs of all cancer survivors change as they progress through their recovery”. (#4845) Finally, some participants suggested that a ‘cancer buddy’ (#7987) may be helpful in addressing feelings of aloneness and sharing tips to overcome challenges, “They paired me up with somebody to talk to that’d been through it already, which was really helpful”. (#5166).
Participants recognised that ‘all care is always centred around the person who is ill’ (#1634) and that healthcare providers should facilitate partner involvement and support, “I don't know if it's encouraging the partner to come to appointments or even if there are appointments where we're just going to talk about sex, to encourage to bring your partner.” (#3711) “Support and coping mechanisms; how they can feel useful, needed and still valued in that relationship when the spotlight is always on the person with the illness.” (#1634) Short oncology appointments were raised as a barrier to addressing sexual concerns. Participants suggested sexual health appointments, e.g., ‘check-up for your sexual health and your husband’ (#2698), and questionnaires to identify areas for support, “Every time I did my little questionnaire at the start of chemo; they'd always ask how my husband was, how he was coping, and how we were coping together as a couple. I think if we identified that we needed support or had questions, we could get that information.” (#3469) Lastly, access to counselling and practical tools for YGCS, partners and couples could be vital to SQoL.
For us, it’d be having help. Having somebody who understands what we’re going through to help guide us. We could sit down together and understand better what’s happening to us. Be given tools on how to navigate and improve our situation. (#5166)
Theme 3: healthcare policy and strategy
Establishing SQoL as standard care in gynaecologic oncology, with a focus on ‘continuity of care’ (#9547) is key for YGCS, “Just like mental health plans, there needs to be a follow up plan for every degree of cancer.” (#9547). This is vital as YGCS admitted it’s hard to ask for help, “They could give it to me, so it's not a matter of me admitting, ‘Okay, I need help’. But it was more, ‘This is what we do as standard practice, standard care’.” (#6260). Our data analysis revealed three subthemes under healthcare policy (Table 3): clinical guidelines for risk and needs assessment, multidisciplinary teams for delivery of psychosexual care, and training to improve clinician’s knowledge in SQoL, confidence, and communication skills.
First, clinical guidelines may assist healthcare providers in assessing needs and risk factors to SQoL, “I think that would be of benefit to identify those needs”. (#9547) YGCS suggest ‘a checklist of questions that gets asked’ (#5453), which could act as conversation starter.
Before you see your specialist, because it’s such a short timeframe, perhaps there is a sexual questionnaire that you complete, which gives your doctor a quick tick box overview of whether they should ask you about it. Completing a pre-appointment questionnaire, which will prompt them to ask a few questions, could help to open those communication channels. (#5137)
Second, YGCS want a ‘more rounded approach’ (#2318) to post-treatment care, “What needs to be done is a clinical pathway that has multiple components, not just the surgeon who cuts it out and the medical oncologist that gives you the chemo… holistic care, so not just treating the disease but treating the person.” (#2967) Participants believe that gynaecologic oncologists have a role to play, notably by providing referrals to ‘support clinics’ (#5166) or in-hospital services, “When I go for check-ups, if there was someone there in the same building or in the hospital that you could talk to, as part of the routine package of post-treatment care. That would have been amazing to talk to someone who wanted to find a solution for you, because it shouldn’t be this hard to be intimate.” (#1634).
If someone had said to me, ‘Here’s the name of a pelvic floor physio, you need to go and see her’. Thereby, not allowed the tissues to contract to the extent that they did. If someone had moved in that direction, I’d possibly still have a sex life today. (#2698)
The role of interdisciplinary care teams (e.g., pelvic floor physiotherapists, oncology nurses, specialised psychologists, and sexual health experts) was a recurrent theme, “maybe it’s an appointment or a telephone call with the nurse” (#3611). Notably, individuals living remotely stated that nurses could help overcome barriers to access support services, “I was dropped back into the country where they have no knowledge, not a lot of anything. If I had a nurse or nurse check-up in the country” (#7987), especially when using a practical approach to post-treatment care, “I don’t do well with people telling me what to do. But rather showing me exactly what to do.” (#7987).
Third, YGCS feel ‘medical oncologists tend to be very blunt… poor bedside manners’ (#2318). Thus, clinical training on ‘how to get comfortable to have that conversation’ (#3711) is critical in tackling shame, establishing patient-doctor trust, and improving SQoL. In fact, YGCS want gynaecologic oncologists to be both ‘confident and competent’ in SQoL (#2967) and use a trauma-informed approach to communication and care.
I have a lot of guilt and shame about the diagnosis and potentially the impact on others. Especially in a gyn-oncology ward, to have a man my age, who probably has not had to deal with a woman with trauma, they can’t have that lived experience. He said, ‘Okay, take your pants off and get on the bed’, I said, ‘I don’t think I will’. But if I didn’t have the guts to stick up for myself, I’d have felt almost not violated, but I wouldn’t have felt heard and supported. (#9547)
Lastly, integrating a self-reflective practice in clinical training may be beneficial, “There are so many different variables on doctors as to who they are and how they operate in themselves and what they believe”. (#2788).
Discussion
Our data show SQoL matters to YGCS. Our data analysis identified three key areas for strategy development that are relevant to YGCS: psychosexual education, psychosocial support, and healthcare policy to establish SQoL as standard care. Clinical care guidelines in Australia emphasise patient-centred care, recognising that cancer diagnosis and treatment can have a significant impact on a person’s sexual health and relationships. Although healthcare providers are encouraged to discuss sexual concerns and provide appropriate support, these recommendations may not consistently translate into practice. Notably, this research revealed the need for clear guidelines to help clinicians perform risk assessments and assess ongoing needs for sexual rehabilitation through the cancer journey. In saying that, we recognise that guidelines, practices, and the availability of services related to physical therapy, counselling, and education on sexual health may vary across different healthcare institutions and regions in Australia. Moreover, the strategies put forward by YGCS showed an alignment with the protective factors of SQoL for GCS (Tables 1, 2 and 3) [20]. Themes and subthemes are discussed below.
Psychosexual education
YGCS reported that sexual complications came ‘as a shock’ and that psychosexual distress was aggravated by the lack of information on the multifaceted impact of GC on SQoL. Participants felt ill-prepared to manage the psychological trauma of cancer and long-term aftermaths of treatment, which hampered their sexual recovery [24]. Information about how to prepare for adverse effects and how to be an active participant in care planning can help YGCS regain a sense of control [1]. Our findings confirmed that psychosexual information and support are acceptable to YGCS [1, 6, 25]. For instance, Vermeer et al. [25] found that GCS want information about treatment effects on sexual functioning, practical advice on dealing with sexual complaints, and reassurance that it is common to experience sexual dysfunction. Another study [12] reported that YGCS demand information on fertility, sexual functioning, partner relationships, vaginal changes, and premature menopause.
By improving access to psychosexual education, gynaecologic oncologists may help reduce psychological distress [26]. Providing basic information before cancer treatment begins [26] may also provide an opportunity for YGCS to make informed treatment and care decisions [1]. Conversely, a cancer diagnosis can be a traumatic experience for a young woman. Healthcare providers should be wary of ‘information overload’, especially in the immediate diagnosis and postoperative periods. Thus, information needs may vary between patients and through the treatment and care continuum [1, 2, 12] and adopting a patient-centric approach [1] to assessing needs and risk factors is suggested. We also recommend asking YGCS about their preferences [1] or being guided by the widely recommended PLISSIT model (Permission, Limited Information, Specific Suggestions, and Intensive Therapy) as a framework to discuss sexuality [3, 27, 28].
Psychosocial support
Our findings revealed that psychosocial support, through expert-led peer support, partner involvement and support, and counselling with individuals and couples may be a key piece of the puzzle in improving SQoL for YGCS. Our data, consistent with findings from Walton et al. [1], related to Bloom’s [29] three dimensions of social support: informational, emotional and practical. An Australian study [30] also found that the lack of support and public discourse about GC may contribute to stigma and that sharing experiences in online support groups may improve support accessibility and anonymity for those who felt marginalised. As such, disease-specific peer support is well supported for GC [12]. Other feasibility studies with gynaecological cancer patients (GCP) found that moderated online-based psychosocial support could help address psychosexual concerns while also improving quality of life (QoL). Wiljer et al. [31] found that web-based support groups are both feasible and accepted by GCP with psychosexual distress. Participants reported feeling at ease in discussing sexuality online and benefiting from support from both peers and moderators for improved body image, sexuality, and emotional well-being. Similarly, Classen et al. [32] found that a 12-week online intervention, including a discussion forum moderated by professionals and psycho-educational materials on the impact of treatment, was acceptable to remitted GCP. A similar study by Brotto et al. [33] discovered that an online-based 12-weekly psychosexual education and mindfulness program was feasible and beneficial to GCS. Furthermore, moderated virtual support groups could provide mutual validation and support, thus helping to break feelings of isolation and aloneness reported in similar studies [34, 35].
Our findings confirmed that there is a lack of support for partners, yet ‘a supportive partner’ is a protective factor of SQoL [20, 27]. Besides experiencing psychological challenges (e.g. helplessness, fear for the future, concerns of causing harm during intercourse), some partners may also take the caregiver role, which can interfere with resuming sexual activity [27]. Healthcare providers can offer avenues for partner involvement and support, such as inviting partners to appointments and providing take-home information or referrals to support services. Lastly, offering counselling may help individuals and couples develop communication skills and find new ways to enjoy intimacy together [24, 25, 27, 36].
Healthcare policy and strategy
Healthcare policy and strategy to establish SQoL as standard care in gynaecologic oncology, notably through continuity of care [1], has been reported elsewhere when it comes to risk and needs assessment [1, 2], multidisciplinary care teams [26, 37] and clinical training [6, 37]. Systematic screening of women’s needs for support [2] is recommended and The Brief Sexual Symptoms Checklist for Women is known as a useful screening tool [26, 38]. In a study by Vermeer et al. [6], gynaecologic oncologists, radiation oncologists and oncology nurses involved in GC treatment, cited embarrassment and lack of time as barriers for providing psychosexual support. Adopting a holistic and integrated approach to SQoL [1], such as encouraging referrals to fertility and menopause specialists [1, 2, 12] and the greater involvement of nurses, pelvic floor physiotherapists and specialist psychologists in follow up care [12]. For example, nurse-led interventions have been effective in improving sexual health and sexual satisfaction [39] as well as the QoL, sexual function, and family function of GCP [39]. Lastly, YGCS expressed their wish for greater community awareness and education to help de-stigmatise GC, HPV, and sexuality [30]. Valuing and normalising conversations about sexuality and gynaecological health would create the umbrella to implement practical strategies towards greater sexual wellbeing for YGCS.
Strengths and limitations
The SQoL in YGCS study presented novel and practical findings for the 18–45 age group. Strengths included the use of an evidence-based interview guide, which was pilot tested with YGCS. Both single and partnered women living with cervical and ovarian cancer, stage I to IV, were represented across Australia. However, vaginal, vulvar, and uterine cancer were not represented. The limited representation of certain gynaecological cancers in our study can be attributed, in part, to our focus on specific study populations and the budgetary limitations that restricted our access to these groups. While we successfully employed grassroots recruitment strategies in partnership with ovarian cancer and cervical cancer charities, it should be noted that other gynaecological cancer groups are not comprehensively represented in Australia. Thus, the small sample size (n = 15) influences the generalisability or transferability of results outside of Australia or to women who do not have internet access. The study included only women who considered themselves proficient in communicating in English. This limited the potential representation of perspectives from non-English speakers or people who consider themselves non-proficient in English. Consequently, our focus on language proficiency may have excluded insights from culturally diverse populations, hindering an understanding of experiences, especially relating to cultural context. Similarly, since only one participant was in a same-sex relationship, the views of LGBTIQA+individuals were under-represented.
Conclusion
This qualitative study demonstrated the need to integrate SQoL in gynaecologic oncology. To protect and improve SQoL, YGCS proposed three areas for strategy development, with an emphasis on normalising SQoL to remove stigma, break isolation and build self-efficacy for YGCS, partners and clinicians. First, improving psychosexual education on the impact of cancer and treatment on SQoL, post-treatment care and psychosexual wellbeing, patient-doctor communication and self-advocacy, and partner communication and intimacy. Second, facilitating psychosocial support, using a trauma-informed approach to communication and care, through expert-led peer support, partner involvement and support, and counselling to individuals and couples. Third, developing healthcare policy and strategy to establish SQoL as standard care in gynaecologic oncology through clinical guidelines for risk and needs assessment, multidisciplinary teams for delivery of psychosexual care, and training clinicians in SQoL and communication. A better understanding of the strategies acceptable to YGCS may help health professionals deliver cancer care and communication that are relevant and helpful to young women.
References
Walton, L. M., Reeve, J., Brown, P. M., & Farquhar, C. M. (2010). Gynaecologic cancer patients’ needs and experiences of supportive health services in New Zealand. Psycho-Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer., 19(2), 201–8.
Lopez, A. L. J., Butow, P. N., Philp, S., Hobbs, K., Phillips, E., Robertson, R., Juraskova, I. (2019). Age-related supportive care needs of women with gynaecological cancer: A qualitative exploration. European Journal of Cancer Care., 28(4), e13070.
Perz, J., Ussher, J. M., & Australian, Canc S. (2015). A randomized trial of a minimal intervention for sexual concerns after cancer: A comparison of self-help and professionally delivered modalities. Bmc Cancer. https://doi.org/10.1186/s12885-015-1638-6
Akalin, A., & Pinar, G. (2016). Unmet needs of women diagnosed with gynecologic cancer: An overview of literature. Journal of Palliative Care & Medicine, 6(2), 1–6.
Beesley, V., Eakin, E., Steginga, S., Aitken, J., Dunn, J., & Battistutta, D. (2008). Unmet needs of gynaecological cancer survivors: implications for developing community support services. Psycho-Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer., 17(4), 392–400.
Vermeer, W. M., Bakker, R. M., Stiggelbout, A. M., Creutzberg, C. L., Kenter, G. G., & Ter Kuile, M. M. (2015). Psychosexual support for gynecological cancer survivors: Professionals’ current practices and need for assistance. Supportive Care in Cancer., 23(3), 831–839. https://doi.org/10.1007/s00520-014-2433-7
Roussin, M., Lowe, J., Hamilton, A., & Martin, L. (2023). Sexual quality of life in young gynaecological cancer survivors: A qualitative study. Quality of Life Research. https://doi.org/10.1007/s11136-023-03386-1
Beesley, V. L., Alemayehu, C., & Webb, P. M. (2019). A systematic literature review of trials of survivorship interventions for women with gynaecological cancer and their caregivers. European journal of cancer care., 28(3), e13057.
Flynn, P., Kew, F., & Kisely, S. R. (2009). Interventions for psychosexual dysfunction in women treated for gynaecological malignancy. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD004708.pub2
Ahmed-Lecheheb, D., & Joly, F. (2016). Ovarian cancer survivors’ quality of life: A systematic review. Journal of Cancer Survivorship., 10(5), 789–801.
Roland, K. B., Rodriguez, J. L., Patterson, J. R., & Trivers, K. F. (2013). A literature review of the social and psychological needs of ovarian cancer survivors. Psycho-Oncology., 22(11), 2408–2418. https://doi.org/10.1002/pon.3322
Beesley, V. L., Alemayehu, C., & Webb, P. M. (2018). A systematic literature review of the prevalence of and risk factors for supportive care needs among women with gynaecological cancer and their caregivers. Supportive Care in Cancer., 26(3), 701–710.
Komblith, A. B., Powell, M., Regan, M. M., Bennett, S., Krasner, C., Moy, B., Younger, J., Goodman, A. K., Berkowitz, R., Winer, E. (2007). Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psycho-Oncology., 16(10), 895–903. https://doi.org/10.1002/pon.1146
Jeppesen, M. M., Mogensen, O., Dehn, P., & Jensen, P. T. (2015). Needs and priorities of women with endometrial and cervical cancer. Journal of Psychosomatic Obstetrics and Gynecology., 36(3), 122–132. https://doi.org/10.3109/0167482x.2015.1059417
McCallum, M., Lefebvre, M., Jolicoeur, L., Maheu, C., & Lebel, S. (2012). Sexual health and gynecological cancer: Conceptualizing patient needs and overcoming barriers to seeking and accessing services. Journal of Psychosomatic Obstetrics & Gynecology., 33(3), 135–142. https://doi.org/10.3109/0167482X.2012.709291
Qualtrics. August (2021) ed. Provo, Utah, USA2021.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative research in psychology., 3(2), 77–101.
Clarke, V., Braun, V., & Hayfield, N. (2012). Chapter 4: Thematic Analysis. APA Handbook of Research Methods in Psychology (pp. 57–71). American Psychological Association.
NVivo. 1.5 (2021). ed: QSR International Pty Ltd.
Roussin, M., Lowe, J., Hamilton, A., & Martin, L. (2021). Factors of sexual quality of life in gynaecological cancers: A systematic literature review. Archives of gynecology and obstetrics., 304(3), 791–805. https://doi.org/10.1007/s00404-021-06056-0
Antonovsky, A. (1996). The salutogenic model as a theory to guide health promotion. Health promotion international., 11(1), 11–18.
Critical Appraisal Skills Programme UK. (n.d.). CASP checklists. [Available from: https://casp-uk.net/casp-tools-checklists/.
Braun, V., & Clarke, V. (2021). To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative research in sport, exercise and health., 13(2), 201–216.
Fischer, O. J., Marguerie, M., & Brotto, L. A. (2019). Sexual function, quality of life, and experiences of women with ovarian cancer: A mixed-methods study. Sex Med., 7(4), 530–539.
Vermeer, W. M., Bakker, R. M., Kenter, G. G., Stiggelbout, A. M., & ter Kuile, M. M. (2016). Cervical cancer survivors’ and partners’ experiences with sexual dysfunction and psychosexual support. Supportive Care in Cancer., 24(4), 1679–1687. https://doi.org/10.1007/s00520-015-2925-0
Boa, R., & Grenman, S. (2018). Psychosexual health in gynecologic cancer. International Journal of Gynaecology and Obstetrics, 143(Suppl 2), 147–152. https://doi.org/10.1002/ijgo.12623
Abbott-Anderson K. (2015). Sexual Concerns of Gynecological Cancer Survivors: Development of the Sexual Concerns Questionnaire-Gynecological Cancer: University of Wisconsin - Madison.
Jensen, P. T., Groenvold, M., Klee, M. C., Thranov, I., Petersen, M. A., & Machin, D. (2003). Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. International Journal of Radiation Oncology Biology Physics., 56(4), 937–949. https://doi.org/10.1016/s0360-3016(03)00362-6
Bloom, J. R. (1986). Social support and adjustment to breast cancer (pp. 204–229). Springer.
Wray, N., Markovic, M., & Manderson, L. (2007). Discourses of normality and difference: Responses to diagnosis and treatment of gynaecological cancer of Australian women. Social Science & Medicine., 64(11), 2260–2271.
Wiljer, D., Urowitz, S., Barbera, L., Chivers, M. L., Quartey, N. K., Ferguson, S. E., To, M., Classen, C. C. (2011). A qualitative study of an internet-based support group for women with sexual distress due to gynecologic cancer. Journal of Cancer Education., 26(3), 451–458. https://doi.org/10.1007/s13187-011-0215-1
Classen, C. C., Chivers, M. L., Urowitz, S., Barbera, L., Wiljer, D., O’Rinn, S., Ferguson, S. E. (2013). Psychosexual distress in women with gynecologic cancer: A feasibility study of an online support group. Psycho-Oncology., 22(4), 930–935. https://doi.org/10.1002/pon.3058
Brotto, L. A., Dunkley, C. R., Breckon, E., Carter, J., Brown, C., Daniluk, J., Miller, D. (2017). Integrating quantitative and qualitative methods to evaluate an online psychoeducational program for sexual difficulties in colorectal and gynecologic cancer survivors. Journal of sex & marital therapy., 43(7), 645–662.
Jefferies, H., & Clifford, C. (2011). Aloneness: The lived experience of women with cancer of the vulva. European Journal of Cancer Care., 20(6), 738–746. https://doi.org/10.1111/j.1365-2354.2011.01246.x
Lloyd, P. A., Briggs, E. V., Kane, N., Jeyarajah, A. R., & Shepherd, J. H. (2014). Women’s experiences after a radical vaginal trachelectomy for early stage cervical cancer. A descriptive phenomenological study. European Journal of Oncology Nursing., 18(4), 362–71. https://doi.org/10.1016/j.ejon.2014.03.014
Perz, J., Ussher, J. M., & Gilbert, E. (2013). Constructions of sex and intimacy after cancer: Q methodology study of people with cancer, their partners, and health professionals. Bmc Cancer. https://doi.org/10.1186/1471-2407-13-270
Williams, N. F., Hauck, Y. L., & Bosco, A. M. (2017). Nurses’ perceptions of providing psychosexual care for women experiencing gynaecological cancer. European Journal of Oncology Nursing., 30, 35–42. https://doi.org/10.1016/j.ejon.2017.07.006
Hatzichristou, D., Rosen, R. C., Derogatis, L. R., Low, W. Y., Meuleman, E. J., Sadovsky, R., Symonds, T. (2010). Recommendations for the clinical evaluation of men and women with sexual dysfunction. The Journal of Sexual Medicine., 7(1), 337–348.
Estrogen and progestogen therapy in postmenopausal women. (2004). Fertility and Sterility, 82(Suppl. 1), S70–S80. https://doi.org/10.1016/j.fertnstert.2004.05.006
Acknowledgements
We thank all the individuals who participated in the study for sharing their experiences and the organisations who assisted in recruitment. Special thanks to Ovarian Cancer Australia and the Australian Cervical Cancer Foundation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Project administration was undertaken by MR and project supervision was completed by JL, AH, and LM. Material preparation, ethics application, recruitment, data collection and analysis were performed by MR. The first draft of the manuscript was written by MR and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethical approval
The research received ethical approval by the Human Research Ethics Committee of the University of the Sunshine Coast (S201448).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors consent to publish. Consent was also obtained from all participants and all data have been de-identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roussin, M., Hamilton, A., Lowe, J. et al. Sexual quality of life after gynaecological cancer: what young women want. Qual Life Res 33, 679–689 (2024). https://doi.org/10.1007/s11136-023-03553-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03553-4