Abstract
Purpose
Patients with multiple sclerosis (MS) are at significant risk for decreased quality of life (QoL), in part due to factors such as cognitive impairment and depression. However, objective versus subjective assessments of cognitive functioning may differentially predict QoL, and it remains unknown whether they each impact QoL through levels of depression. The aims of the present study included (1) testing the effects of cognitive impairment on MS-related QoL via depression symptoms and (2) examining whether perceived and objective cognitive functioning differentially predict QoL through depression.
Methods
Patients formally diagnosed with MS (N = 128) participated in cognitive assessment (Brief International Cognitive Assessment for Multiple Sclerosis) and completed self-report measures of perceived cognitive functioning (perceived deficits questionnaire), depression (Hospital Anxiety and Depression Scale), and MS-related QoL (functional assessment of multiple sclerosis).
Results
Mediational hypotheses were tested by regression and structural equation modeling. As hypothesized, both perceived and objective cognitive functioning independently predicted lower QoL controlling for the effects of depression (p < 0.001). Consistent with hypotheses, depression mediated effects of both perceived (95% CI [0.31, 0.68]) and objective cognitive functioning (95% CI [0.09, 6.96]) on QoL when tested in separate models. However, when both predictors were modeled simultaneously, depression only mediated the effects of perceived (not objective) cognitive functioning (95% CI for standardized effect [0.10, 0.61]).
Conclusions
This study, thus, suggests the need to conceptualize different pathways by which objective and subjective cognitive impairment may shape QoL in the lives of individuals with MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
Multiple sclerosis (MS) is a brain disease characterized by decreased quality of life (QoL). Cognitive difficulties (problems with memory and thinking) are a major reason for lower QoL in people with MS. However, the ways that these thinking problems contribute to QoL in MS are not fully clear. One possibility is that cognitive difficulties contribute to QoL by increasing depressed mood. It remains unknown whether depression accounts for links to QOL for thinking problems measured by actual objective tests, or just for patients’ perceptions of their own thinking. This study aimed to address this question. The findings showed that both patients’ perceptions of their thinking problems and objective cognitive performance were related to QoL, but depression played a larger role in explaining links of subjective perceptions to QoL. These findings suggest the need to better understand how actual thinking problems and one’s perceptions of them may contribute to QoL in different ways for people with diseases such as MS.
Introduction
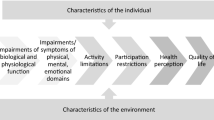
Most individuals (40–65%) with multiple sclerosis (MS) experience cognitive impairment [1]. Both objective [2] and perceived cognitive functioning predict quality of life (QoL) in MS [3], but the differential impact of these factors on QoL and their mediating paths remain poorly understood. The present study examined the differential prediction of QoL in MS by objective and perceived cognitive functioning, and whether depression may mediate these effects on QoL.
MS is a relatively common, immune-mediated neurodegenerative condition [4]. In MS, the immune system attacks the myelin on nerve fibers, interrupting nerve communication. Symptoms may include cognitive difficulties, dizziness, sensory disturbances, weakness, spasticity, loss of balance/coordination, and bladder/bowel dysfunction [1]. MS severity and course varies between subtypes of relapsing–remitting (fluctuations between exacerbations and remission), primary-progressive (symptoms progress without remission), or secondary-progressive (progressive worsening after periods of relapse/remission). Given this heterogeneity, long-term prediction of the course of MS remains elusive [5].
MS patients experience lower QoL compared to healthy controls and patients with other chronic conditions [6]. Lower QoL is strongly associated with MS disease progression, likely resulting from neurologic disability and concomitant difficulties with daily activities and social roles [7]. Factors predicting QoL may shape how patients manage an unpredictable disease, warranting research on factors that predict QoL and their pathways [4]. Such factors may include cognitive functioning and depressed mood.
Factors predicting quality of life
Cognitive impairment
Cognitive dysfunction might account for lower QoL [3]. In early MS, the immune system attacks the central nervous system (CNS), causing inflammatory lesions in the brain, spinal cord, and optic nerves, and nerve demyelination. At later stages, axonal degeneration and severe neurological effects occur, impairing memory, processing speed, attention, and executive functioning [1].
Objective assessment of cognitive functioning
The impact of cognitive functioning on QoL in MS might be attributable to actual neurocognitive impairments. Studies assessing objective cognitive functioning (i.e., attention, memory, executing functioning) have found links to QoL in MS. For instance, lower cognitive function predicted higher MS severity and duration [2] and lower ability to work, which in turn predicted worse QoL in MS [8]. Similarly, demyelination lesions in MS correlated with lower scores on objective measures of cognitive function [9] and lower QoL [10]. Thus, diminished QoL in MS might derive from difficulties with objective cognitive functioning.
Subjective perceptions of cognitive functioning
Alternatively, individuals with MS often subjectively appraise their cognition as impaired [11], which may contribute to lower QoL. Lower perceptions of cognitive abilities (e.g., planning and memory) predicted lower QoL, beyond disease severity [3]. Perceived cognitive function in MS has also been linked to depression and anxiety [12], which generally predict lower QoL in MS [13]. However, studies have not examined both objective and perceived cognitive functioning as simultaneous predictors of QoL to tease apart distinct independent effects, which may have implications for interventions (e.g., objective functioning may indicate neurologic decline and necessitate disease-modifying medical treatment; perceived cognitive functioning may require psychological intervention, such as cognitive behavioral therapy). Moreover, understanding mediators may clarify understanding of disease processes and inform treatment.
Depression as a mediator
Objective and perceived and cognitive impairment may shape QoL via the mechanism of depression (e.g., negative mood, anhedonia, fatigue, change in sleep or appetite, and psychomotor difficulties) [13]. Depression rates are higher in MS than other chronic illnesses, with a lifetime prevalence of 40–60% [14]. Longer MS illness duration has been linked to higher depression and lower QoL [2, 15, 16]. Even after accounting for fatigue and MS disability, depression predicted lower QoL [13].
On one hand, objective cognitive functioning—a marker of brain pathology—might predict QoL via depression. Indeed, demyelination lesions due to MS, particularly in the left inferior medial frontal and left anterior temporal brain regions [14], and neurological impairment [17] are correlated with higher depression. Although psychological impact [18], loss of social support [4], and coping problems [19] influence depression, effects of CNS lesions may partially account for increased depression [14]. A longitudinal MS study linked cognitive functioning to mental health QoL and depression to physical QoL [20], though not directly testing mediation. In another study, objective cognition predicted QoL only when controlling for depression [21], implying no mediation by depression in a mildly impaired sample. However, research must directly test whether objective cognitive functioning predicts QoL via depression symptoms.
Alternatively, perceived cognitive functioning might predict QoL via depression. Depression may be a reaction to patients’ ideas about how MS impairs their cognition [17], consistent with links of such perceptions to depression [12]. As MS progresses, patients’ perceived cognitive ability often worsens, and depressed patients may underestimate cognitive functioning [22]. Given robust links of depression to lower QoL [16], one might therefore expect perceived cognitive functioning to predict QoL through depression. Moreover, although one study examining perceived and objective cognitive functioning in MS found stronger links of the former to depression [23], no studies investigated differential effects of perceived versus objective functioning on QoL via depression.
The present study
The present study aimed to clarify the relationships between perceived and objective cognitive functioning, depression, and QoL in MS. In a cross-sectional, correlational study of MS patients, we examined (1) depression as a possible mediator in the relationship between each type of cognitive functioning and QoL, and (2) distinct indirect effects of perceived and objective cognitive functioning on QoL via depression.
Based on the studies linking poor perceived cognitive functioning to lower QoL in MS [3] and depressive symptoms [24], and depressive symptoms to QoL in MS [16], we hypothesized these direct effects, and expected that lower levels of depression would mediate the relationship between perceived cognitive functioning and QoL. Additionally, given associations of objective cognitive functioning to higher QoL [2] and lower depression in MS [14], we expected these effects and hypothesized that depression would partially mediate effects of objective cognitive functioning on QoL.
Depression has often been more strongly linked to perceived than objective cognitive functioning. Thus, we hypothesized that when modeling both cognitive measures as simultaneous predictors, only the indirect effect of perceived cognitive functioning predicting QoL through depression would remain statistically significant.
Method
Participants
Patients at an MS center (N = 128; 69.5% female) ranged from 21 to 78 years old (M = 48.9; SD = 13.2). MS was diagnosed by physicians (or confirmed by a neurologist) through evidence of damage to at least two brain regions, assessed at two or more time points (e.g., via symptom assessment, patient history, and MRI) [25]. Diagnoses included relapsing–remitting MS (82%), primary-progressive MS (10.2%), and secondary-progressive MS (7.8%). Time since diagnosis ranged three months to 52 years (M = 10.0 years, SD = 9.0). Years of education ranged from 9 to 23 (M = 15.0, SD = 2.4). Participants identified as White (82%), Asian American (3.1%), Hispanic/Latinx (3.1%), African American (5.5%), American Indian/Alaska Native (0.8%), Bi-racial (2.3%), or Other (3.1%).
Procedure
Participants were recruited through an urban MS treatment center in the Pacific Northwest. Researchers contacted patients with scheduled ongoing care appointments to inquire about participation in research. Interested individuals providing informed consent visited the clinic to complete cognitive assessment and self-reports of mood, cognitive functioning, and QoL. Participants received no compensation.
Measures
Objective cognitive functioning
The Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) [26] is an assessment battery including the Symbol Digit Modalities Test (SDMT), California Verbal Learning Test-II (CVLT-II), and Brief Visual Spatial Memory Test-Revised (BVMT-R). The BICAMS battery was designed as a clinical/research screening of cognitive function in MS [26]. SDMT, CVLT, and BVMT scores are converted to z-scores and summed into a total BICAMS score indexing cognitive functioning broadly. Correlations among the three scales were large, ranging from 0.57 to 0.73 (p < 0.001). The BICAMS demonstrated test–retest reliability [9], discrimination between MS and healthy groups [9], and sensitivity and specificity in predicting cognitive deficits [27].
Perceived cognitive functioning
The perceived deficits questionnaire (PDQ) [28] is a 20-item self-report developed in an MS sample, assessing attention/concentration, retrospective memory, prospective memory, and organization/planning (five items each). Participants rate a 0 (never) to 4 (almost always) scale. Total scores range 0–80. Scores were reversed for parallelism with objective cognition scores, so higher scores reflect higher perceived functioning. The PDQ showed validity and internal consistency [28]. In this study, α = 0.95.
Depression symptoms
The Hospital Anxiety and Depression Scale (HADS) [29] depression subscale is a seven-item depression screen for medical populations. Participants rate items on a 0 (not at all) to 3 (most of the time) scale (e.g., “I have lost interest in my appearance”). The scale demonstrated internal consistency [29], and validity in MS populations, with high specificity and sensitivity [30]. In this study, α = 0.79.
Quality of life
The functional assessment of multiple sclerosis (FAMS) [31] measured health-related QoL in MS via items assessing mobility (seven items), MS symptoms (seven items), general contentment (seven items), cognitive and physical fatigue (nine items), and family and social well-being (nine items). The emotional well-being subscale was omitted to avoid construct overlap with the HADS. Participants rate items on a 0 (not at all) to 4 (very much) scale. The FAMS demonstrated retest reliability, concurrent validity [31], and internal consistency [32]. In this study, α = 0.94.
Data analysis plan
Power analyses suggested that to achieve > 0.80 power, small-to-medium effects of objective cognitive functioning (0.20, our smallest expected effect) and large effects of depression (0.50) on QoL would require at least 120 participants. Mediational hypotheses were tested via the PROCESS macro for SPSS, model 4 [33], followed by structural equation modeling (SEM). We used AMOS 23.0 to test distinct indirect effects of both predictors in a single structural equation model, and because SEM explicitly models measurement error by the use of latent variables [34]. Whereas observed variables (raw total scores) do not correct for measurement error, SEM modeling latent constructs via multiple indicators (subscales or item parcels) explicitly distinguishes shared construct variance from measurement error, thereby enhancing precision for estimating effects of interest. Bootstrapped 95% confidence intervals tested indirect effects. Initially, analyses included sex, age, years of MS, and years of education as covariates. Only years of education was a significant predictor, so other covariates were removed. Additionally, fatigue is a symptom of both MS [1] and depression [14], and thus might suggest a spurious association. This risk was minimized by using a depression measure that does not include somatic symptoms such as fatigue [29]. Additionally, because effects were similar when analyzing with and without fatigue items in QoL, we report results with fatigue items included in QoL.
Results
Preliminary analyses
First, data pre-screening suggested normal distributions and no nonlinearity between variables. Means, standard deviations, reliability estimates, and zero-order correlations are represented in Table 1. Data were 99.4% complete.
Depression mediating between perceived cognitive functioning and quality of life
Analyses tested direct effects of perceived cognitive functioning on QoL and depression symptoms and QoL, and depression on QoL after accounting for perceived cognition, then the indirect effect on QoL via depression. As expected (see Table 2), perceived cognitive functioning predicted higher QoL, and predicted lower depressive symptoms. Controlling years of education and depression (which predicted higher and lower QoL, respectively), perceived cognition still predicted higher QoL. These models predicted 35% of variability in depression and 67% of QoL. As hypothesized, perceived cognitive functioning predicted higher QoL through lower depression (B = 0.47, SE = 0.10, 95% CI [0.31, 0.68]), a significant indirect effect accounting for 39% of the variability in QoL.
Depression mediating between objective cognitive functioning and quality of life
The second model tested direct effects of objective cognitive functioning on depression symptoms and QoL, and depression on QoL after accounting for objective cognition, then the indirect effect on QoL via depression. As hypothesized (see Table 2), objective cognitive functioning predicted higher QoL and lower depression. In the full model (controlling for a positive effect of years of education and negative effect of depression), objective cognitive function predicted higher QoL. These models predicted 6% of variability in depression and 60% of QoL. Consistent with hypotheses, results indicated a significant indirect effect: objective cognitive functioning predicted lower QoL through lower depression (B = 3.55, SE = 1.73, 95% CI [0.09, 6.96]), although it accounted for only 9% of the variance in QoL.
When both indirect effects were tested simultaneously, depression symptoms mediated effects of perceived (not objective) cognitive functioning on quality of life
Lastly, we used SEM to incorporate latent variables (i.e., enhance reliability) and model all pathways simultaneously. Indices of model fit included: χ2 (non-significant p values imply good fit but this test is overly sensitive to sample size and therefore not interpreted), normed χ2 (good fit < 2.0), CFI (good fit > 0.95), and RMSEA (< 0.06) [35]. The SEM included four latent constructs: perceived cognitive functioning, objective cognitive functioning, depression, and QoL. A latent perceived cognitive functioning factor was composed of PDQ subscales. Latent QoL was composed of FAMS subscales. The depression measure had no subscales, so we created three-item HADS (depression) parcels to improve reliability [36], averaging items 4 and 8, 2 and 10, and 6, 12, and 4. A baseline model was tested first, providing model fit indices to make theoretically reasonable modifications as needed, then testing the a final “structural” model relevant to core hypotheses (i.e., direct and indirect effects).
By freeing covariances between latent variables (perceived cognitive functioning, objective cognitive functioning, depression, and QoL), the initial structural equation model (Model 1) tested the baseline model. Model 1 achieved minimally acceptable fit, χ2 (84, N = 128) = 170.76, p < 0.001, normed χ2 = 2.03, CFI = 0.921, RMSEA = 0.090, RMSEA 95% CI [0.070, 0.110]. Based on modification indices and the rationale that some self-report items may share method variance separate from the objective tasks, we allowed several self-report scales’ error terms to covary. This included e3 (Prospective Memory) with e2 (error for PDQ Retrospective Memory) and e5 (HADS Parcel 1, which includes feeling “slowed down”); e11 (FAMS Mobility) was permitted to covary with e1, e4, and e5, given that these assess perceptions of cognitive/motor responding which may involve shared variance not explained by the broader constructs. Errors were allowed to covary for FAMS General Contentment (e13) and Family Well-Being (e14), given the plausibility of shared variance between emotional and interpersonal well-being [37]. The modifications resulted in Model 2 (see Fig. 1).
Model 2 fit significantly better than the baseline model (Δχ2 = 61.44, Δdf = 6, p < 0.001), with relatively good fit overall, χ2 (78, N = 128) = 109.32, p = 0.01, normed χ2 = 1.40, CFI = 0.971, RMSEA = 0.056, RMSEA 95% CI [0.028, 0.080]. To avoid model overfitting, Model 2 was used as the primary model. In this model, all standardized factor loadings were significant (p < 0.001). Perceived and objective cognitive functioning were not significantly associated (r = 0.19, p = 0.069), showing the non-redundancy of these variables.
Given reasonable model fit, the relationships between latent variables were examined. As expected, depression predicted lower QoL, and perceived cognitive functioning predicted lower depression and higher QoL, even when controlling for effects of objective cognitive functioning. The indirect effect from perceived cognitive functioning to QoL (independent of objective cognition) through depression was significant (β = 0.30, p = 0.017, 95% CI [0.10, 0.61], and this indirect effect explained 62% of the variance in QoL. Removing the direct effect of perceived cognitive functioning on QoL resulted in significant loss of model fit (Δχ2 = 11.50, p < 0.001), suggesting the need to account for both direct and indirect effects of perceived cognitive functioning on QoL. In contrast, while there was a significant direct effect of objective cognitive functioning on depression, the independent indirect effect of objective cognitive functioning on QoL through depression was not significant (β = 0.04, p = 0.170, 95% CI [− 0.02, 0.15], controlling for perceived cognitive functioning.
Discussion
Few studies have examined pathways by which perceived and objective cognitive functioning predict QoL in MS. This study expands on current literature by examining (a) whether depression symptoms separately mediated the effects of both perceived and objective cognitive functioning on QoL, and (b) whether there were distinct indirect effects of cognitive function on QoL through depression when both objective and perceived cognitive functioning were in the same model. Previous studies have generally examined only one type of cognitive function, and not partialed out independent pathways of each to QoL.
Major findings
Perceived cognitive functioning predicted QoL through depression
As hypothesized, higher perceived cognitive functioning predicted both lower depressive symptoms and higher QoL, replicating past studies. Past research focused on associations between perceived cognitive functioning and depression [23, 24], perceived cognitive functioning and QoL [3], and depression and QoL [13, 15], but not how these may relate beyond a bivariate approach. Similar to our study, Samartzis et al. [3] found that perceived cognitive functioning associated with depression and predicted QoL independently of depression; however, mediation was not directly tested. Extending past findings, perceived cognitive functioning in our study predicted higher QoL indirectly through lower depressive symptoms. In other words, depression provides one reason individuals who subjectively perceive difficulties with their cognitive abilities endorse lower QoL. Individuals who believe their cognition is flawed may be more likely to experience mood disruption and anhedonia, which may have downstream effects on QoL in MS. Although further research is warranted to consider causality, results suggest that depression may be one pathway (among others, given the lack of full mediation) by which perceived cognitive function contributes to QoL in MS.
Objective cognitive functioning predicted QoL through depression
Similarly, objective cognitive functioning predicted higher QoL through lower depression, when perceived cognitive functioning was not considered. These effects are consistent with past findings that objective cognitive functioning and lower depression positively predicted QoL [2], although not all studies have linked objective cognitive functioning to depression [38]. The results also parallel studies linking brain lesions to depressive symptoms [14]. The indirect effect found in the present study is consistent with the possibility that depression symptoms [18] and poorer cognitive functioning [9] might share overlapping causes such as physical aspects of demyelination or brain lesions. However, we also note the “radiological paradox” that MS clinical presentation does not always correlate with radiological markers of brain lesions, so future studies should also consider other explanations for why depression might mediate effects of objective cognitive impairment (e.g., executive impairments making mood regulation more difficult in general, or poorer cognitive functioning making daily living tasks more challenging and thereby undermining QoL). Alternatively, disability [13, 16], social support, employment, or fatigue [8] might serve as mediators. These possibilities remain to be examined further. Nonetheless, given that no study has directly assessed the mediating role of depression between objective cognitive functioning and QoL in an MS population, the finding of an indirect effect is novel. However, to test whether the mediating role of depression was specific to either index of cognitive functioning required additional analyses modeling these effects simultaneously.
Differential indirect effects of perceived versus objective cognitive functioning
The present investigation is the first to simultaneously test indirect effects of perceived and objective cognitive functioning on QoL via depression, providing a more conservative estimate of effects. When indirect effects of both perceived and objective cognitive functioning on QoL via depression were simultaneously estimated in the same model, only the distinct indirect effect of perceived cognitive functioning on QoL through depression remained significant. Although both indirect effects were significant when examined separately, the SEM results suggest that depressive symptoms played an independent mediating role only for perceived cognitive functioning. Although perceived cognitive dysfunction has been linked to changes in thalamic and cortical gray matter volumes [39], the indirect effect controlling for objective cognitive dysfunction suggests that organic changes do not explain effects on QoL.
The fact that the indirect effect from objective cognitive functioning to QoL disappeared when perceived cognitive functioning was in the model suggests that depression may represent a core pathway between cognition and QoL particularly with regard to subjective appraisals of cognitive ability. As depression and perceptions of poor cognitive functioning both entail negative cognitive appraisals, it makes sense that depression would serve as a stronger mediator for perceived cognition relative to actual cognitive performance. This fits with relatively weak effects of objective cognitive impairment on QoL after accounting for covariates [40].
Clinical implications
Unlike pharmacological treatments [9], cognitive rehabilitation therapy for MS has shown promise for reducing fatigue and improving working memory and attention. However, with irreversible brain damage, training may focus on compensating for cognitive deficits rather than restoring cognitive functioning [9]. Research is mixed on the effect of cognitive rehabilitation on mood in MS [41], suggesting a gap in treatment for MS. Given partial mediation of the cognitive functioning-QoL links by depression, and the likelihood that objective cognitive functioning operates by a different pathway, our results suggest the need to assess perceived cognitive functioning alongside objective assessments in clinical practice, as these may suggest differential treatment plans. For example, interventions that target the source of depression relative to cognition (perceived and/or objective) may be indicated. Thus, supplementing cognitive rehabilitation with interventions focused on improving mood (e.g., activity scheduling, accumulating positives) may provide benefit. Similarly, cognitive interventions to reframe beliefs about cognitive functioning may be indicated to improve perceived cognition, given links of perceived cognitive deficits to internalized stigma (i.e., negative illness cognitions) and QoL [42]. In addition, individuals’ perceptions of their cognitive functioning may have a low correlation to their objective performance on full cognitive batteries [11, 24], so perceived cognitive functioning might improve with clear feedback from cognitive testing, especially if patients overestimate their decline. For true decline in cognitive functioning, it may be beneficial to provide psychoeducation and resources for coping with cognitive dysfunction (e.g., cognitive rehabilitation, behavioral therapy, exercise, problem-focused coping) to increase self-efficacy in managing cognitive deficits. Further research on the relationship between cognitive functioning (objective and perceived) and depression may aid clinicians to provide specific, focused interventions targeted to improve mood and QoL.
Limitations and future research
Several limitations exist in this study. First, the cross-sectional design reduced patient burden, but our correlational findings do not permit causal inference. Future studies should include longitudinal and potentially experimental designs (e.g., in which cognitive rehabilitation or other interventions can be shown to improve QoL via shifts in depression). Second, generalizability to all subtypes of MS is limited, as 82% of participants in the current study were diagnosed with relapsing–remitting MS (although consistent with prevalence rates of relapsing–remitting MS [1]). Furthermore, although the BICAMS assesses the most common impairments in cognitive functioning, more comprehensive neurocognitive assessments would provide greater cognitive specificity. Additionally, fatigue is a common MS symptom, comorbid with depression, and can impact cognitive functioning [15], and might shape the results. However, using assessments limiting construct overlap provided some countermeasures. Lastly, more research is warranted in MS samples with people of color.
Conclusion
The present study provides support for both perceived and objective cognitive functioning as predictors of QoL. Depression is one salient mechanism underlying this relationship, important for understanding the well-being of MS patients, particularly for perceived cognitive functioning. This finding implies the need to further consider interventions that target both perceived cognitive functioning and depressive symptoms, which in turn might improve QoL in individuals with MS—the ultimate goal of this research.
Data availability
The authors are open to sharing the data upon request.
Code availability
The authors are open to sharing the code upon request.
References
Javůrková, A., Zimová, D., Tomašovičová, K., & Raudenská, J. (2016). Cognitive deficits and neuropsychological assessment in multiple sclerosis. In A. Gonzalez-Quevedo (Ed.), Trending topics in multiple sclerosis (pp. 211–226). InTech. https://doi.org/10.5772/63968
Benito-León, J., Morales, J. M., & Rivera-Navarro, J. (2002). Health-related QoL and its relationship to cognitive and emotional functioning in multiple sclerosis patients. European Journal of Neurology, 9, 497–502. https://doi.org/10.1046/j.1468-1331.2002.00450.x
Samartzis, L., Gavala, E., Zoukos, Y., Aspiotis, A., & Thomaides, T. (2014). Perceived cognitive decline in multiple sclerosis impacts quality of life independently of depression. Rehabilitation Research and Practice, 2014, https://doi.org/10.1155/2014/128751.
Buchanan, R. J., Huang, C., & Kaufman, M. (2010). Health-related quality of life among young adults with multiple sclerosis. International Journal of MS Care, 12, 190–199. https://doi.org/10.7224/1537-2073-12.4.190
Rolak, L. A. (2003). Multiple sclerosis: It’s not the disease you thought it was. Clinical Medicine & Research, 1, 57–60. https://doi.org/10.3121/cmr.1.1.57
Sprangers, M. A., de Regt, E. B., Andries, F., van Agt, H. M., Bijl, R. V., de Boer, J. B., Foets, M., Hoeymans, N., Jacobs, A. E., Kempen, G. I. J. M., Miedema, H. S., Tijhuis, M. A. R., & de Haes, H. C. J. M. (2000). Which chronic conditions are associated with better or poorer quality of life? Journal of Clinical Epidemiology, 53, 895–907. https://doi.org/10.1016/S0895-4356(00)00204-3
Janardhan, V., & Bakshi, R. (2000). Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Archives of Neurology, 57, 1485–1491. https://doi.org/10.1001/archneur.57.10.1485
Benedict, R. H., Wahlig, E., Bakshi, R., Fishman, I., Munschauer, F., Zivadinov, R., & Weinstock-Guttman, B. (2005). Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. Journal of the Neurological Sciences, 231, 29–34. https://doi.org/10.1017/S1355617706060723
Winkelmann, A., Engel, C., Apel, A., & Zettl, U. K. (2007). Cognitive impairment in multiple sclerosis. Journal of Neurology, 254, 1135–1142. https://doi.org/10.1007/s00415-007-2010-9
Mowry, E. M., Beheshtian, A., Waubant, E., Goodin, D. S., Cree, B. A., Qualley, P., Lincoln, R., George, M. F., Gomez, R., Hauser, S. L., Okuda, D. T., & Pelletier, D. (2009). Quality of life in multiple sclerosis is associated with lesion burden and brain volume measures. Neurology, 72, 1760–1765. https://doi.org/10.1212/WNL.0b013e3181a609f8
Maor, Y., Olmer, L., & Mozes, B. (2001). The relation between objective and subjective impairment in cognitive function among multiple sclerosis patients–the role of depression. Multiple Sclerosis Journal—Experimental, Translational and Clinical, 7, 131–135. https://doi.org/10.1177/135245850100700209
Malivoire, B. L. (2018). Psychological symptoms and perceived cognitive impairment in multiple sclerosis: The role of rumination. Rehabilitation Psychology, 63, 286–294. https://doi.org/10.1037/rep0000180
Janardhan, V., & Bakshi, R. (2002). Quality of life in patients with multiple sclerosis: The impact of fatigue and depression. Journal of the Neurological Sciences, 205, 51–58. https://doi.org/10.1016/S0022-510X(02)00312-X
Pucak, M. L., Carroll, K. A., Kerr, D. A., & Kaplin, A. I. (2007). Neuropsychiatric manifestations of depression in multiple sclerosis: Neuroinflammatory, neuroendocrine, and neurotrophic mechanisms in the pathogenesis of immune-mediated depression. Dialogues in Clinical Neuroscience, 9, 125–139. https://doi.org/10.31887/DCNS.2007.9.2/mpucak
Chen, K., Fan, Y., Hu, R., Yang, T., & Li, K. (2013). Impact of depression, fatigue and disability on quality of life in Chinese patients with multiple sclerosis. Stress and Health, 29(2), 108–112. https://doi.org/10.1002/smi.2432
Göksel Karatepe, A., Kaya, T., Günaydn, R., Demirhan, A., Ce, P., & Gedizlioğlu, M. (2011). Quality of life in patients with multiple sclerosis: The impact of depression, fatigue, and disability. International Journal of Rehabilitation Research, 34, 290–298. https://doi.org/10.1097/MRR.0b013e32834ad479
Rabins, P. V., Brooks, B. R., O’Donnell, P., Pearlson, G. D., Moberg, P., Jubelt, B., Coyle, P., Dalos, N., & Folstein, M. F. (1986). Structural brain correlates of emotional disorder in multiple sclerosis. Brain, 109, 585–597. https://doi.org/10.1093/brain/109.4.585
Kroencke, D. C., Denney, D. R., & Lynch, S. G. (2001). Depression during exacerbations in multiple sclerosis: The importance of uncertainty. Multiple Sclerosis Journal, 7, 237–242. https://doi.org/10.1177/135245850100700405
Arnett, P. A., & Randolph, J. J. (2006). Longitudinal course of depression symptoms in multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry, 77, 606–610. https://doi.org/10.1136/jnnp.2004.047712
Nourbakhsh, B., Julian, L., & Waubant, E. (2017). Fatigue and depression predict quality of life in patients with early multiple sclerosis: A longitudinal study. European Journal of Neurology, 23(9), 1482–1486. https://doi.org/10.1111/ene.13102
Glanz, B. I., Healy, B. C., Rintell, D. J., Jaffin, S. K., Bakshi, R., & Weiner, H. L. (2010). The association between cognitive impairment and quality of life in patients with early multiple sclerosis. Journal of the Neurological Sciences, 290, 75–79. https://doi.org/10.1016/j.jns.2009.11.004
Schwert, C., Stohrer, M., Aschenbrenner, S., Weisbrod, M., & Schrdöer, A. (2018). Biased neurocognitive self-perception in depressive and in healthy persons. Journal of Affective Disorders, 232, 96–102. https://doi.org/10.1016/j.jad.2018.02.031
Kinsinger, S. W., Lattie, E., & Mohr, D. C. (2011). Relationship between depression, fatigue, subjective cognitive impairment, and objective neuropsychological functioning in patients with multiple sclerosis. Neuropsychology, 24, 573–580. https://doi.org/10.1037/a0019222
Middleton, L. S., Denney, D. R., Lynch, S. G., & Parmenter, B. (2006). The relationship between perceived and objective cognitive functioning in multiple sclerosis. Archives of Clinical Neuropsychology, 21, 487–494. https://doi.org/10.1016/j.acn.2006.06.008
Thompson, A. J., Banwell, B. L., Barkhof, F., Carroll, W. M., Coetzee, T., Comi, G., & Cohen, J. A. (2018). Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. The Lancet Neurology, 17(2), 162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Langdon, D. W., Amato, M. P., Boringa, J., Brochet, B., Foley, F., Fredrikson, S., Hämäläinen, P., Hartung, H. P., Krupp, L., Penner, I. K., Reder, A. T., & Benedict, R. H. (2012). Recommendations for a brief international cognitive assessment for multiple sclerosis (BICAMS). Multiple Sclerosis Journal, 18, 891–898. https://doi.org/10.1177/1352458511431076
Dusankova, J. B., Kalincik, T., Havrdova, E., & Benedict, R. H. (2012). Cross cultural validation of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) and the brief international cognitive assessment for multiple sclerosis (BICAMS). The Clinical Neuropsychologist, 26, 1186–1200. https://doi.org/10.1080/13854046.2012.725101
Ritvo, P. G., Fischer, J. S., Miller, D. M., Andrews, H., Paty, D. W., & LaRocca, N. G. (1997). Multiple sclerosis quality of life index: A user’s manual. National Multiple Sclerosis Society.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Honarmand, K., & Feinstein, A. (2009). Validation of the hospital anxiety and depression scale for use with multiple sclerosis patients. Multiple Sclerosis Journal, 15, 1518–1524. https://doi.org/10.1177/1352458509347150
Cella, D. F., Dineen, K., Arnason, B., Reder, A., Webster, K. A., Karabatsos, G., Chang, C., Lloyd, S., Steward, J., & Stefoski, D. (1996). Validation of the functional assessment of multiple sclerosis quality of life instrument. Neurology, 47, 129–139. https://doi.org/10.1212/WNL.47.1.129
Yorke, A. M., & Cohen, E. T. (2015). Functional assessment of multiple sclerosis. Journal of Physiotherapy, 61, 226. https://doi.org/10.1016/j.jphys.2015.05.021
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press.
Arbuckle, J. L. (2014). Amos 23.0 user’s guide. IBM SPSS.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford Press.
Matsunaga, M. (2008). Item parceling in structural equation modeling: A primer. Communication Methods & Measures, 2, 260–293. https://doi.org/10.1080/19312450802458935
Ruvalcaba-Romero, N. A., Fernández-Berrocal, P., Salazar-Estrada, J. G., & Gallegos-Guajardo, J. (2017). Positive emotions, self-esteem, interpersonal relationships and social support as mediators between emotional intelligence and life satisfaction. Journal of Behavior, Health & Social Issues, 9(1), 1–6. https://doi.org/10.1016/j.jbhsi.2017.08.001
Julian, L., Merluzzi, N. M., & Mohr, D. C. (2007). The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Multiple Sclerosis Journal, 13, 81–86. https://doi.org/10.1177/1352458506070255
Kletenick, I., Alvarez, E., Honce, J. M., Valdez, B., Vollmer, T. L., & Medina, L. D. (2019). Subjective cognitive concern in multiple sclerosis is associated with reduced thalamic and cortical gray matter volumes. Multiple Sclerosis Journal—Experimental, Translational and Clinical, 5, 1–9. https://doi.org/10.1177/2055217319827618
Baumstarck-Barrau, K., Simeoni, M. C., Reuter, F., Klemina, I., Aghababian, V., Pelletier, J., & Auquier, P. (2011). Cognitive function and quality of life in multiple sclerosis patients: A cross-sectional study. BMC Neurology, 11, 17. https://doi.org/10.1186/1471-2377-11-17
Mitolo, M., Venneri, A., Wilkinson, I. D., & Sharrack, B. (2015). Cognitive rehabilitation in multiple sclerosis: A systematic review. Journal of Neurological Sciences, 354, 1–9. https://doi.org/10.1016/j.jns.2015.05.004
Shin, Y. J., Joo, Y. H., & Kim, J. H. (2016). Self-perceived cognitive deficits and their relationship with internalized stigma and quality of life in patients with schizophrenia. Neuropsychiatric Disease and Treatment, 12, 1411–1417. https://doi.org/10.2147/NDT.S108537
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
TAC, HER, and CMQ performed data collection. Analyses were conducted by TAC and TME. The first draft of the manuscript was written by TAC, and all authors contributed to revisions. All authors read and approved the manuscript. TME mentored the project. The study was approved by the Seattle Pacific University institutional review board.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or competing interests to disclose.
Ethical approval
The study (#151602029) was approved by the Institutional Review Board of Seattle Pacific University.
Consent to participate
All participants provided informed consent to be part of this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Crouch, T.A., Reas, H.E., Quach, C.M. et al. Does depression in multiple sclerosis mediate effects of cognitive functioning on quality of life?. Qual Life Res 31, 497–506 (2022). https://doi.org/10.1007/s11136-021-02927-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02927-w