Abstract
Purpose
Health-related quality of life (HRQoL) is considered an important measure of treatment and rehabilitation outcomes in multiple sclerosis (MS) patients. In this study, we used multivariate regression analysis to examine the role of cognitive appraisals, adjusted for clinical, socioeconomic and demographic variables, as correlates of HRQoL in MS.
Methods
The cross-sectional study included 257 MS patients, who completed Multiple Sclerosis Impact Scale, Generalized Self-Efficacy Scale, Rosenberg Self-Esteem Scale, Brief Illness Perception Questionnaire, Treatment Beliefs Scale, Actually Received Support Scale (a part of Berlin Social Support Scale) and Socioeconomic Resources Scale. Demographic and clinical characteristics of the participants were collected with a self-report survey. Correlation and regression analyses were conducted to determine associations between the variables.
Results
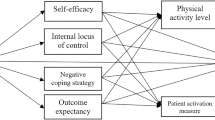
Five variables, illness identity (β = 0.29, p ≤ 0.001), self-esteem (β = −0.22, p ≤ 0.001), general self-efficacy (β = −0.21, p ≤ 0.001), disability subgroup “EDSS” (β = 0.14, p = 0.006) and age (β = 0.12, p = 0.012), were significant correlates of HRQoL in MS. These variables explained 46 % of variance in the dependent variable. Moreover, we identified correlates of physical and psychological dimensions of HRQoL.
Conclusions
Cognitive appraisals, such as general self-efficacy, self-esteem and illness perception, are more salient correlates of HRQoL than social support, socioeconomic resources and clinical characteristics, such as type and duration of MS. Therefore, interventions aimed at cognitive appraisals may also improve HRQoL of MS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health-related quality of life (HRQoL) is a multidimensional concept related to subjective impact of a disease on physical, psychological and social functioning of an individual. Currently, HRQoL is an established measure of treatment and rehabilitation outcomes [1], and as such is often considered in clinical trials, everyday medical practice and determination of health policies [2]. This concept is particularly relevant as a treatment goal in the case of chronic conditions with unpredictable outcomes, variable symptoms and lack of curative treatments, such as multiple sclerosis (MS). As this neurological disorder is characterized by progressive and unstable course, MS patients may experience many variable symptoms, and clinical assessment does not necessarily reflect the true complexity of the condition’s impact.
The important role of HRQoL in MS is reflected by a large number of previous studies dealing with the problem in question. MS patients were consistently shown to present with lower HRQoL than healthy subjects [3, 4] and individuals with other conditions, such as epilepsy, diabetes mellitus, inflammatory bowel disease, liver transplant recipients, ischemic stroke, Parkinson’s disease and rheumatoid arthritis [5–10]. This suggests that MS may negatively affect both physical and psychological dimension of HRQoL [4]. Therefore, improvement of HRQoL is an important objective of MS management. However, modifiable predictors of HRQoL need to be identified in order to achieve this goal.
Recent studies showed that the impact of MS on HRQoL results primarily from the influence of physical and psychosocial factors, such as depression [11, 12], disability level, fatigue [12], duration and clinical course of the disease [13], social support [14, 15], illness perception [16] and self-efficacy [17]. Moreover, some authors emphasized the role of socio-demographic factors, such as age, educational level, employment and marital status [15, 18]. However, the role of each factor varied depending on the concept of research, measurement method, enrollment criteria and analyzed dimensions of HRQoL. Nevertheless, most previous studies confirmed that all these factors not only influence HRQoL but also interact with each other [19].
We identified several drawbacks while reviewing previous studies dealing with the problem in question. First, most of them centered around a small number of potential HRQoL predictors [20–23]. HRQoL is a complex construct and as such requires a comprehensive approach, and only a few studies analyzed interactions between several factors in multivariate models [14, 16, 24, 25]. Second, the available data on the role of clinical, psychological and socio-demographic factors as correlates of HRQoL in MS patients are inconclusive. Third, we found only one study analyzing the role of cognitive appraisal as an independent predictor of HRQoL [16].
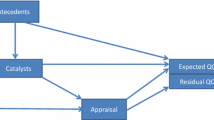
Many authors analyzed emotional factors as correlates of HRQoL. HRQoL of MS patients, particularly its mental dimension, was shown to be associated with depression [11, 13, 23, 25, 26]. However, this association may reflect the similarity of depression and HRQoL measures, rather than a causal relationship [27]. Most HRQoL scales, especially those measuring its mental dimension, refer to mood and satisfaction. In this context, the association between HRQoL and depression is not surprising. Depressive patients typically perceive their quality of life as inferior, which constitutes a principal symptom of depression. Moreover, HRQoL and mood are determined by the same factors [19], which may further confound the results of multivariate analyses. Therefore, we hypothesized that cognitive appraisals, representing evaluation of self, illness and treatment, are more accurate predictors of HRQoL. According to the cognitive-behavioral theory, perception of a situation influences one’s emotional and behavioral responses and often also physiological reactions. This is a core assumption behind the Beck’s cognitive theory of depression. Beck’s main argument was that depression is instituted by one’s view of oneself, rather than one has a negative view of oneself due to depression [28]. Critical events (e.g., MS diagnosis) can promote negative beliefs which then trigger depressive symptoms. In line with other cognitive models for adjustment, these are the appraisals that people make after a trauma, which determine their response [29]. This assumption is supported by the results of other studies. For example, Kennedy, Evans, and Sandhu [30] have found appraisals as a strong predictor of anxiety and depression in individuals with spinal cord injury. Consequently, subjective perception of self, disease and treatment may affect behavior, emotional state and quality of life of the patients. This makes cognitive appraisals related to self, illness and treatment, an interesting subject of research as potentially modifiable correlates of HRQoL in MS.
The aim of this study was to analyze the role of cognitive appraisals, adjusted for clinical, socioeconomic and demographic variables, as correlates of HRQoL in MS. We hypothesized that illness perception, treatment beliefs, self-esteem and self-efficacy are more salient correlates of HRQoL in MS than other measured variables. To the best of our knowledge, this was the first study to analyze cognitive appraisals related to self, illness and treatment as correlates of HRQoL in MS.
Methods
Participants and procedure
The study included 257 individuals with MS, recruited in cooperation with Multiple Sclerosis Rehabilitation Centre in Borne Sulinowo and the Polish Society of Multiple Sclerosis. The inclusion criteria were: (1) lack of MS exacerbation at the time of the study and during four preceding weeks, (2) lack of other comorbidities and (3) absence of MS-related cognitive problems, as confirmed by a neurologist. The study was granted permission from the head of MS rehabilitation clinic, and written informed consent was obtained from all the participants prior to the survey. All the instruments were administrated face-to-face by the research team members. Patients from rehabilitation clinic were interviewed individually in their own rooms after rehabilitation, and community sample patients were examined individually in their homes by a social worker from the Polish Society of Multiple Sclerosis. The patients were assured that their data will be treated as confidential. Overall, 36 out of the 293 invited persons were not interested in participation in the study or withdrew during the survey. There were no missing data as the surveys were checked for their completeness immediately after returning, and the respondents were asked to fill all the gaps.
Measures
A dependent variable, disease-specific HRQoL, was measured using a 29-item Multiple Sclerosis Impact Scale (MSIS-29) [31]. This self-report instrument was designed to measure physical (20 items) and psychological (9 items) impact of MS, using a scale from 1 (not at all) to 5 (extremely), with higher numbers corresponding to worse HRQoL. MSIS-29 is a widely accepted, accurate and valid measure of quality of life in MS [32]. Internal consistency rates for the physical and psychological subscales of MSIS-29 used in this study were α = 0.965 and α = 0.948, respectively.
Four groups of independent variables were included:
-
1.
Cognitive appraisals: Illness perception was assessed with the Brief Illness Perception Questionnaire (B-IPQ) [33] based on the Leventhal Commonsense Model of Illness [34]. B-IPQ includes eight items graded on a linear 0–10 response scale, measuring cognitive and emotional representation of illness. Each item refers to one dimension of illness perception (consequences, timeline, personal control, treatment control, illness identity, concern, coherence and emotional representation). We excluded two dimensions, concern and emotional representation, from the analysis since they both refer to emotional, rather than the cognitive area. Treatment beliefs were represented by eight items corresponding to patient perception of treatment effectiveness. The scores for Treatment Beliefs Scale (TBS) ranged from 1 (not at all) to 5 (completely). Treatment beliefs were expressed as the sum of scores for the eight items, with higher scores corresponding to more positive perception. Internal consistency rate of the TBS was acceptable (Cronbach’s α = 0.954). General self-efficacy was measured with General Self-Efficacy Scale (GSES) [35], a widely used 10-item psychometric scale designed to assess optimistic self-beliefs to cope with a variety of difficult demands in life. GSES demonstrated high internal consistency rate (Cronbach’s α = 0.947). To assess self-esteem, we used Rosenberg Self-Esteem Scale (RSES) [36] which consists of 10 items rated on a four-point scale, from 3 (strongly agree) to 0 (strongly disagree). Higher cumulative RSES scores correspond to more positive self-esteem. Internal consistency rate of this scale was α = 0.748.
-
2.
Socioeconomic variables: The survey included questions on employment status and monthly income per family member. Furthermore, the availability of socioeconomic resources (doctor, physiotherapist, psychologist, social worker, public buildings, medical equipment and medications) was determined with our original nine-item resource scale, including such items as “I have no problem with access to my doctor” or “My place of residence is adapted to my needs and capabilities.” The availability of resources was scored from 1 (strongly disagree) to 4 (strongly agree), and the global score represented the sum of scores for the nine individual items, with higher scores corresponding to greater availability. Internal consistency rate of this scale was α = 0.801. To measure the level of received social support, we used the Actually Received Support Scale, a part of the Berlin Social Support Scale (BSSS) [37]. Due to its high reliability and validity, BSSS has been used to study social support in various groups of patients [38]. The instrument used in our study had high internal consistency rate (Cronbach’s α = 0.950).
-
3.
Clinical variables: The survey included questions on MS-specific problems, such as time elapsed since the diagnosis of MS and type of the disorder. Moreover, the patients were subjected to neurological assessment including examination with Expanded Disability Status Scale (EDSS), widely used scale of disease progression and neurological impairment [39]. As suggested by Papuc and Stelmasiak [25], the participants were divided into three subgroups based on their EDSS scores: with mild (1.0–3.5), moderate (4.0–6.5) and high physical disability (7.0–9.5).
-
4.
Demographic variables: Personal characteristics of the patients, such as gender, age, place of residence, marital status and educational level, were documented.
Data analysis
All statistical analyses were performed with the IBM Statistical Package for Social Sciences (IBM SPSS Statistics 21). The data were screened and checked against the assumptions of regression analysis. Mann–Whitney test (Z), Kruskal–Wallis test (H) and Spearman’s rank correlation coefficients (r s) were used to assess the significance and power of relationships between the independent variables and HRQoL (MSIS-29). To verify the study hypotheses, three separate hierarchical multiple regression models were built, with MSIS-29, MSIS-physical and MSIS-psychological scores as dependent variables. All three models included only the independent variables that turned out to be significantly associated with HRQoL on univariate analyses. The threshold of statistical significance for the inclusion of independent variables to the multiple regression models was set at p < 0.05.
Results
Group characteristics
The study group included 172 women and 85 men with mean age of 48 years. Most of the participants were married (58 %), with higher education (49 %) and disability pension (49 %). The majority of participants lived in towns (85 %) and had household monthly income below 1000 PLN to one family member (37 %). The mean time elapsed since MS diagnosis was 13 years (SD = 9.3). Relapsing-remitting MS (RRMS, 37 %) was the most frequently self-reported type of the condition, followed by primary progressive MS (PPMS, 29.5 %), secondary progressive MS (SPMS, 23 %) and progressive-relapsing MS (PRMS, 8 %). Thirty patients (2 %) were unable to specify the type of their MS (DKMS). The majority of the study subjects (70 %) presented with a moderate-degree physical disability (3.5 < EDSS ≤ 6.5) corresponding to involvement of a number of functional systems (e.g., problems with vision and coordination) and/or difficulty walking distances <500 m. Mean EDSS scores for specific MS subtypes were as follows: RRMS = 4.6, PPMS = 6.3, SPMS = 6.0, PRMS = 5.7. The socio-demographic and illness-related characteristics are summarized in Table 1.
Preliminary analyses
Two demographic factors, age at the time of the study and marital status, were significantly associated with HRQoL (Table 2). Older participants presented with higher MSIS-29 scores than younger subjects. Separated, divorced or widowed subjects showed higher scores than married/cohabitant ones and singles (higher scores corresponded to worse HRQoL).
Also two illness-related factors, disability subgroup “EDSS” and time elapsed since diagnosis, were significantly associated with HRQoL (Table 2). Participants with mild disability showed better HRQoL than those with moderate or high disability. Similarly, individuals with moderate disability presented with better HRQoL than those with high disability. Moreover, patients with longer history of MS presented with higher MSIS-29 scores than those in whom the disease was diagnosed more recently.
All socioeconomic factors were correlated significantly with HRQoL (Table 2). Higher levels of social support and socioeconomic resources were associated with better HRQoL. Participants who were employed presented with better HRQoL than disability and age pensioners. Individuals with monthly per capita incomes >2000 PLN had better HRQoL than those with the incomes <1000 PLN.
Seven cognitive appraisals were significantly correlated with HRQoL (Table 2). Two illness perception variables, i.e., consequences and identity, were positively correlated with HRQoL, whereas another two, i.e., personal control and treatment control, showed inverse correlations with this parameter. Also another three cognitive factors, treatment beliefs, self-esteem and general self-efficacy, were correlated inversely with MSIS-29 scores. Mean scores for all analyzed scales are presented in Table 3.
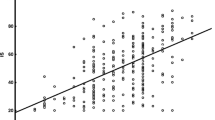
Hierarchical multiple regression
Three separate hierarchical multiple regression models were built, with MSIS-29, MSIS-physical and MSIS-psychological scores as dependent variables (Table 4). All 17 independent variables included in the models turned out to be significantly associated with the MSIS-29 scores.
According to the first model, HRQoL (MSIS-29 score) was predicted by five variables: identity, self-esteem, general self-efficacy, disability subgroup “EDSS” and age. The model was significant and explained a considerable proportion of variance in global HRQoL level (R 2 = 0.46; F(5,249) = 42.640; p < 0.001).
According to the second model, physical dimension of HRQoL was predicted by four variables: identity, disability subgroup “EDSS,” general self-efficacy and age. Also this model was significant and explained a large proportion of variance in the dependent variable (R 2 = 0.45; F(4,250) = 50.148; p < 0.001).
The third model included four variables, i.e., self-esteem, identity, general self-efficacy and marital status; all of them turned out to be the significant predictors of psychological HRQoL dimension. The model was significant and explained a considerable proportion of variance in MSIS-psychological (R 2 = 0.38; F(4,250) = 37.567; p < 0.001).
Discussion
The principal aim of this study was to analyze a relationship between cognitive appraisals and HRQoL. Multivariate regression analysis demonstrated that cognitive appraisals were strong significant correlates of HRQoL in MS patients. Specifically, we revealed that younger participants presenting with higher levels of general self-efficacy and self-esteem, lesser experience of illness symptoms (identity) and functional limitations according to EDSS showed a tendency to better HRQoL. Regression model with all these independent variables explained up to 46 % of variance in the dependent variable. Further analyses showed that physical dimension of MSIS-29 was associated with four factors: general self-efficacy, experience of illness symptoms (identity), EDSS score and age, whereas the psychological dimension was associated with self-esteem, general self-efficacy, experience of illness symptoms (identity) and marital status.
General self-efficacy was the only correlate of both HRQoL dimensions in our regression models. A role of this parameter as a determinant of HRQoL in MS patients was previously documented by Riazi, Thompson and Hobart [40]. They concluded that since self-efficacy is significantly associated with MSIS-29 scores, it may constitute an important target for interventions aimed at HRQoL improvement. Our findings support this hypothesis as we showed that self-efficacy was strongly associated with HRQoL also if analyzed together with a number of other factors. Another perception of self, self-esteem, turned out to be a significant determinant of both general MSIS-29 score and its psychological dimension. This observation is consistent with the results published by Dlugonoski and Motl, who also showed that greater self-esteem is associated with better HRQoL [41]. The fact that the two self-related perceptions were correlates of HRQoL in our participants is not surprising as according to the literature they are interrelated in MS patients [42]. Higher level of self-esteem promotes greater self-confidence which strengthens one’s self-efficacy and vice versa: Subjective self-efficacy interferes with self-esteem of MS patients.
The role of illness perceptions as determinants of HRQoL has not been a subject of extensive research in MS patients. This is quite surprising as research involving other groups of patients showed strong associations between these variables [43–46]. Our findings are consistent with these data, since the perceptions of serious consequences of the disease, high symptom burden (identity), low personal control and low treatment control of the disease were correlated with lower levels of HRQoL. The only two dimensions that did not correlate with HRQoL in our study were perception of the disease as chronic (timeline) and understanding of the disease (comprehensibility). While this is consistent with the results of some previous studies involving individuals with other conditions [16, 43], it stays in opposition to the findings published by other authors [44, 46].
Although most of the illness perceptions were correlated with MSIS-29 score, only one of them was included in our regression model. We showed that experiencing burdensome symptoms of the illness (identity) may contribute to worse HRQoL in physical domain. This is consistent with the results obtained by Spain et al. [16] in a cross-sectional study on 580 MS patients. These authors demonstrated that increased illness identity is associated with decreased physical function and physical role limitations. In another study, involving a group of 94 MS patients, illness identity was the only strong predictor of the disease impact on functional impairment [47]. Also the studies of individuals with chronic obstructive pulmonary disease [43], cardiac [44], rheumatologic [48] and dialysis patients [49] documented a relationship between illness identity and HRQoL.
Treatment beliefs were the only cognitive appraisal that was not included in the regression model despite its significant correlation with HRQoL documented on univariate analysis. Perhaps this resulted from the fact that this variable may be modulated by treatment aggressiveness, a parameter which was not included in our analysis. Nevertheless, the role of treatment beliefs as a predictor of HRQoL in MS patients should be a subject of further more comprehensive research.
Our regression models included three variables that were not cognitive appraisals. First of them was EDSS score, a measure of functional disability. The role of disability level as a correlate of HRQoL in MS is not fully understood. The results of previous studies dealing with the problem in question are inconclusive: Correlations between the two variables were surprisingly weak (R 2 between 2 and 29 %) and modulated by a number of other factors [19] and measurement methods. Most previous studies showed that EDSS score is significantly associated with the physical dimension of HRQoL in MS patients [24, 50, 51], which is also consistent with the hereby presented data. However, we did not find significant associations between HRQoL and other clinical factors, such as type and duration of MS.
Patient’s age was another significant correlate of HRQoL in MS identified in our study. Specifically, older persons presented with worse HRQoL in physical dimension than younger individuals. This finding may be at least partially related to the duration and progress of the disease. Importantly, some authors documented an inverse relationship between age and HRQoL and interpreted it as a consequence of adjustment to the disease in older persons [52, 53]. Our findings do not support this hypothesis and are consistent with the results of previous studies in which worse HRQoL, especially in physical dimension, was associated with older age of MS patients [54, 55].
Last of the significant correlates identified during regression analysis was marital status. Married/cohabitant participants presented with better HRQoL than those who were singles and those who used to have partners in the past (separated, divorced, widowed). This observation is consistent with the results of some previous studies in which marital status was identified as a determinant of HRQoL in MS [18, 56], but stays in opposition to the data published by other authors, claiming that predictive value of marital status for HRQoL in MS patients is limited [57, 58]. Probably, these discrepancies reflect differences in research methods and study samples and need to be addressed during the course of future research.
Our regression models did not include any of the socioeconomic factors, although all of them were correlated positively with HRQoL on univariate analyses, which is in line with the results of previous studies [25, 59, 60]. The fact that none of these factors turned out to be an independent predictor of HRQoL on multivariate analysis is quite surprising, as social support is generally considered an important predictor of QoL and a determinant of HRQoL in MS patients [14, 52, 56, 61]. Our findings seem to support the hypothesis proposed by Jaracz et al. [15], according to whom the role of social support as a determinant of HRQoL in MS patients is neither unconditional nor one-dimensional. Perhaps social support lost its importance when analyzed together with strong correlates of HRQoL, such as cognitive appraisals. Also the authors of a study of women after stroke came to similar conclusions, showing that cognitive appraisals of the stroke’s impact are more important determinant of HRQoL than social support [62]. This issue needs to be addressed during future research.
Our findings have several practical implications. We identified cognitive appraisals as potentially modifiable correlates of HRQoL in MS patients. Early identification of the determinants of worse HRQoL may help in selection of high-risk patients who require more intensive care, service enhancement and psychological intervention. The results of this study suggest that intervention aimed at improvement of self and illness perception of MS patients is vital for optimization of their HRQoL. This goal can be achieved with cognitive restructuring programs, providing adequate disease-related information, training sessions and cognitive-behavioral therapy. Such interventions should be complementary to standard rehabilitation program, since the disability level is also an important determinant of HRQoL in MS patients.
This study has some potential limitations. First, we used cross-sectional design and therefore were unable to conclude on causal relationships between the analyzed variables. Our study did not explain whether cognitive appraisals preclude HRQoL, and the hereby presented conclusions are based on an assumed cognitive-behavioral paradigm. This problem should be addressed during future longitudinal studies. Second, our analysis was based on self-reported data which also might constitute a source of bias. Moreover, we used a one-shot questionnaire survey which always poses a risk for the result falsification due to a tendency to respond unidirectionally. Another limitation is the study sample which is not representative for the whole population of MS patients. We excluded individuals with cognitive problems and other comorbidities. The majority of included patients presented with moderate-degree disability (69.6 % of them had EDSS 3.5–6.5) were retired prematurely, and their mean age was 48 years. Moreover, a large proportion of patients with PPMS were included in the sample. Only 17 % of our participants had EDSS > 6.5. The level of disability may confound the results of such persons, and therefore, the hereby presented findings should be generalized carefully. Additionally, we excluded cognitive impairment solely on the basis of subjective neurological examination not supported with an objective research instrument, which puts in question the reliability of this exclusion criterion. Furthermore, the results of this study were not controlled for medications taken by MS patients, and this factor might modulate cognitive appraisals, especially treatment beliefs. Also, Treatment Beliefs Scale and Socioeconomic Resources Scale were created by the authors of this work and did not undergo validation; consequently, the results for these scales should be interpreted cautiously. Finally, our regression models explained no more than 46 % of variance in the dependent variables, which suggests that HRQoL of MS patients is determined also by other factors. This justifies further research on a larger group of potential HRQoL predictors.
Even taking into account these limitations, our findings suggest that cognitive appraisals, such as general self-efficacy, self-esteem and illness perception, are more salient correlates of HRQoL in MS than social support, socioeconomic resources and clinical variables. Therefore, we suggest that cognitive appraisals should be evaluated in every patient with MS as interventions aimed at this target may likely improve HRQoL of individuals with this condition.
References
Johnson, K. L., Amtmann, D., Yorkston, K., Klasner, E. R., & Kuehn, C. M. (2004). Medical, psychological, social, and programmatic barriers to employment for people with multiple sclerosis. Journal of Rehabilitation-Washington, 70, 38–49.
Patrick, D. L., & Bergner, M. (1990). Measurement of health status in the 1990s. Annual Review of Public Health, 11, 165–183.
McCabe, M. P., & McKern, S. (2002). Quality of life and multiple sclerosis: Comparison between people with multiple sclerosis and people from the general population. Journal of Clinical Psychology in Medical Settings, 9, 287–295.
Benito-León, J., Manuel Morales, J., Rivera-Navarro, J., & Mitchell, A. J. (2003). A review about the impact of multiple sclerosis on health-related quality of life. Disability and Rehabilitation, 25(23), 1291–1303.
Rudick, R. A., Miller, D., Clough, J. D., Gragg, L. A., & Farmer, R. G. (1992). Quality of life in multiple sclerosis. Comparison with inflammatory bowel disease and rheumatoid arthritis. Archives of Neurology, 49, 1237–1242.
Hermann, B. P., Vickrey, B., Hays, R. D., Cramer, J., Devinsky, O., Meador, K., et al. (1996). A comparison of health-related quality of life in patients with epilepsy, diabetes and multiple sclerosis. Epilepsy Research, 25(2), 113–118.
Naess, H., Beiske, A. G., & Myhr, K. M. (2008). Quality of life among young patients with ischaemic stroke compared with patients with multiple sclerosis. Acta Neurologica Scandinavica, 117, 181–185.
Fernández-Jiménez, E., Pérez-San-Gregorio, M. A., Martín-Rodríguez, A., Domínguez-Cabello, E., Navarro-Mascarell, G., & Bernardos-Rodríguez, A. (2012). Comparison of quality of life between two clinical conditions with immunosuppressive therapy: Liver transplantation and multiple sclerosis. In Transplantation proceedings (Vol. 44, No. 9, pp. 2609–2611). Amsterdam: Elsevier.
Riazi, A., Hobart, J. C., Lamping, D. L., Fitzpatrick, R., Freeman, J. A., Jenkinson, C. A. A., et al. (2003). Using the SF-36 measure to compare the health impact of multiple sclerosis and Parkinson’s disease with normal population health profiles. Journal of Neurology, Neurosurgery and Psychiatry, 74(6), 710–714.
Rudick, R. A., & Miller, D. M. (2008). Health-related quality of life in multiple sclerosis. CNS Drugs, 22(10), 827–839.
Fruehwald, S., Loeffler-Stastka, H., Eher, R., Saletu, B., & Baumhackl, U. (2001). Depression and quality of life in multiple sclerosis. Acta Neurologica Scandinavica, 104, 257–261.
Mikula, P., Nagyova, I., Krokavcova, M., Vitkova, M., Rosenberger, J., Szilasiova, J., et al. (2015). Social participation and health-related quality of life in people with multiple sclerosis. Disability and Health Journal, 8(1), 29–34.
Benito-Leon, J., Morales, J. M., & Rivera-Navarro, J. (2002). Health-related quality of life and its relationship to cognitive and emotional functioning in multiple sclerosis patients. European Journal of Neurology, 9(5), 497–502.
Yamout, B., Issa, Z., Herlopian, A., El Bejjani, M., Khalifa, A., Ghadieh, A. S., & Habib, R. H. (2013). Predictors of quality of life among multiple sclerosis patients: A comprehensive analysis. European Journal of Neurology, 20(5), 756–764.
Jaracz, K., Pawlak, M., Górna, K., Kołcz, B., Wołoszyn, D., & Kozubski, W. (2010). Quality of life and social support in patients with multiple sclerosis. Neurologia i Neurochirurgia Polska, 44(4), 358–365.
Spain, L. A., Tubridy, N., Kilpatrick, T. J., Adams, S. J., & Holmes, A. C. N. (2007). Illness perception and health-related quality of life in multiple sclerosis. Acta Neurologica Scandinavica, 116(5), 293–299.
Motl, R. W., McAuley, E., Snook, E. M., & Gliottoni, R. C. (2009). Physical activity and quality of life in multiple sclerosis: Intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychology, Health and Medicine, 14(1), 111–124.
Fernandez, O., Baumstarck-Barrau, K., Simeoni, M. C., & Auquier, P. (2011). Patient characteristics and determinants of quality of life in an international population with multiple sclerosis: Assessment using the MusiQoL and SF-36 questionnaires. Multiple Sclerosis, 17(10), 1238–1249.
Mitchell, A. J., Benito-León, J., González, J. M. M., & Rivera-Navarro, J. (2005). Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. Lancet Neurology, 4(9), 556–566.
Pfaenberger, N., Pfeiffer, K. P., Deibl, M., Hofer, S., Gunther, V., & Ulmer, H. (2006). Association of factors influencing health-related quality of life in MS. Acta Neurologica Scandinavica, 114, 102–108.
Lobentanz, I. S., Asenbaum, S., Vass, K., Sauter, C., Klösch, G., Kollegger, H., et al. (2004). Factors influencing quality of life in multiple sclerosis patients: Disability, depressive mood, fatigue and sleep quality. Acta Neurologica Scandinavica, 110, 6–13.
Amato, M. P., Ponziani, G., Rossi, F., Liedl, C. L., Stefanile, C., & Rossi, L. (2001). Quality of life in multiple sclerosis: The impact of depression, fatigue and disability. Multiple Sclerosis, 7, 340–344.
Janardhan, V., & Bakshi, R. (2002). Quality of life in patients with multiple sclerosis: The impact of fatique and depression. Journal of the Neurological Sciences, 205, 51–58.
Benedict, R. H., Wahlig, E., Bakshi, R., Fishman, I., Munschauer, F., Zivadinov, R., & Weinstock-Guttman, B. (2005). Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. Journal of the Neurological Sciences, 231(1), 29–34.
Papuc, E., & Stelmasiak, Z. (2012). Factors predicting quality of life in a group of Polish subjects with multiple sclerosis: Accounting for functional state, socio-demographic and clinical factors. Clinical Neurology and Neurosurgery, 114, 341–346.
Hart, S., Fonareva, I., Merluzzi, N., & Mohr, D. C. (2005). Treatment for depression and its relationship to improvement in quality of life and psychological well-being in multiple sclerosis patients. Quality of Life Research, 14, 695–703.
Van Schependom, J., D’hooghe, M. B., De Schepper, M., Cleynhens, K., D’hooge, M., Haelewyck, M. C., et al. (2014). Relative contribution of cognitive and physical disability components to quality of life in MS. Journal of the Neurological Sciences, 336(1), 116–121.
McGinn, L. K. (2000). Cognitive behavioral therapy of depression: Theory, treatment, and empirical status. American Journal of Psychotherapy, 54, 254–260.
Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992.
Kennedy, P., Evans, M., & Sandhu, N. (2009). Psychological adjustment to spinal cord injury: The contribution of coping, hope and cognitive appraisals. Psychology Health and Medicine, 14(1), 17–33.
Hobart, J., Lamping, D., Fitzpatrick, R., Riazi, A., & Thompson, A. (2001). The Multiple Sclerosis Impact Scale (MSIS-29): A new patient-based outcome measure. Brain, 124, 962–973.
Gray, O. M., McDonnell, G. V., & Hawkins, S. A. (2009). Tried and tested: The psychometric properties of the Multiple Sclerosis Impact Scale (MSIS-29) in a population-based study. Multiple Sclerosis, 15(1), 75–80.
Broadbent, E., Petrie, K. J., Main, J., & Weinman, J. (2006). The Brief Illness Perception Questionnaire. Journal of Psychosomatic Research, 60, 631–637.
Leventhal, H., Meyer, D., & Nerenz, D. R. (1980). The common sense representation of illness danger. In S. Rachman (Ed.), Contributions to Medical Psychology (pp. 17–30). New York, NY: Pargamon.
Schwarzer, R., & Jerusalem, M. (1995). Generalized self-efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: Nfer-Nelson.
Rosenberg, M. (1989). Society and the adolescent self-image. Middletown, CT: Wesleyan University Press.
Schulz, U., & Schwarzer, R. (2003). Soziale Unterstu¨tzung bei der Krankheitsbewa¨ltigung. Die Berliner Social Support Skalen (BSSS) [Social support in coping with illness: The Berlin Social Support Scales (BSSS)]. Diagnostica, 49, 73–82.
Luszczynska, A., Mohamed, N. E., & Schwarzer, R. (2005). Self-efficacy and social support predict benefit finding 12 months after cancer surgery: The mediating role of coping strategies. Psychology, Health and Medicine, 10, 365–375.
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS). Neurology, 33, 1444–1452.
Riazi, A., Thompson, A. J., & Hobart, J. C. (2004). Self-efficacy predicts self-reported health status in multiple sclerosis. Multiple Sclerosis, 10(1), 61–66.
Dlugonski, D., & Motl, R. W. (2012). Possible antecedents and consequences of self-esteem in persons with multiple sclerosis: Preliminary evidence from a cross-sectional analysis. Rehabilitation Psychology, 57(1), 35.
Barnwell, A. M., & Kavanagh, D. J. (1997). Prediction of psychological adjustment to multiple sclerosis. Social Science and Medicine, 45(3), 411–418.
Bonsaksen, T., Haukeland-Parker, S., Lerdal, A., & Fagermoen, M. S. (2014). A 1-year follow-up study exploring the associations between perception of illness and health-related quality of life in persons with chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 9(1), 41–50.
Janssen, V., De Gucht, V., van Exel, H., & Maes, S. (2013). Changes in illness perceptions and quality of life during participation in cardiac rehabilitation. International Journal of Behavioral Medicine, 20(4), 582–589.
Graham, C. D., Weinman, J., Sadjadi, R., Cahlder, T., Petty, R., Hanna, M. G., et al. (2014). A multicentre postal survey investigating the contribution of illness perceptions, coping and optimism to quality of life and mood in adults with muscle disease. Clinical Rehabilitation, 28(5), 508–519.
Benyamini, Y., Goner-Shilo, D., & Lazarov, A. (2012). Illness perception and quality of life in patients with contact dermatitis. Contact Dermatitis, 67(4), 193–199.
Dennison, L., Moss-Morris, R., Silber, E., Galea, I., & Chalder, T. (2010). Cognitive and behavioural correlates of different domains of psychological adjustment in early-stage multiple sclerosis. Journal of Psychosomatic Research, 69(4), 353–361.
Hyphantis, T., Kotsis, K., Tsifetaki, N., Creed, F., Drosos, A. A., Carvalho, A. F., & Voulgari, P. V. (2013). Depressive and anxiety symptoms and illness perceptions associated with physical health-related quality of life in rheumatologic disorders. Journal of Psychosomatic Research, 74(6), 548.
Timmers, L., Thong, M., Dekker, F. W., Boeschoten, E. W., Heijmans, M., Rijken, M., et al. (2008). Illness perceptions in dialysis patients and their association with quality of life. Psychology and Health, 23(6), 679–690.
Chen, K., Fan, Y., Hu, R., Yang, T., & Li, K. (2013). Impact of depression, fatigue and disability on quality of life in Chinese patients with multiple sclerosis. Stress and Health, 29(2), 108–112.
Cioncoloni, D., Innocenti, I., Bartalini, S., Santarnecchi, E., Rossi, S., Rossi, A., & Ulivelli, M. (2014). Individual factors enhance poor health-related quality of life outcome in multiple sclerosis patients. Significance of predictive determinants. Journal of the Neurological Sciences, 345(1), 213–219.
Schwartz, C., & Frohner, R. (2005). Contribution of demographic, medical, and social support variables in predicting the mental health dimension of quality of life among people with multiple sclerosis. Health and Social Work, 30(3), 203–212.
Ford, H. L., Gerry, E., Johnson, M. H., & Tennant, A. (2001). Health status and quality of life of people with multiple sclerosis. Disability and Rehabilitation, 15, 516–521.
Merkelbach, S., Sittinger, H., & Koenig, J. (2002). Is there a differential impact of fatigue and physical disability on quality of life in multiple sclerosis? The Journal of Nervous and Mental Disease, 190, 388–393.
Krokavcova, M., van Dijk, J. P., Nagyova, I., Rosenberger, J., Gavelova, M., Middel, B., et al. (2008). Social support as a predictor of perceived health status in patients with multiple sclerosis. Patient Education and Counseling, 73(1), 159–165.
Tepavcevic, D. K., Pekmezovic, T., Stojsavljevic, N., Kostic, J., Basuroski, I. D., Mesaros, S., & Drulovic, J. (2014). Change in quality of life and predictors of change among patients with multiple sclerosis: A prospective cohort study. Quality of Life Research, 23(3), 1027–1037.
Costa, D. C., Sá, M. J., & Calheiros, J. M. (2012). The effect of social support on the quality of life of patients with multiple sclerosis. Arquivos de Neuro-Psiquiatria, 70(2), 108–113.
Riazi, A., Hobart, J. C., Fitzpatrick, R., Freeman, J. A., & Thompson, A. J. (2003). Socio-demographic variables are limited predictors of health status in multiple sclerosis. Journal of Neurology, 250(9), 1088–1093.
De Judicibus, M. A., & McCabe, M. P. (2007). The impact of the financial costs of multiple sclerosis on quality of life. International Journal of Behavioral Medicine, 14(1), 3–11.
Honarmand, K., Akbar, N., Kou, N., & Feinstein, A. (2011). Predicting employment status in multiple sclerosis patients: The utility of the MS functional composite. Journal of Neurology, 258, 244–249.
McCabe, M. P., Stokes, M., & McDonald, E. (2009). Changes in quality of life and coping among people with multiple sclerosis over a 2 year period. Psychology Health and Medicine, 14(1), 86–96.
Wu, M. H., Lee, S., Su, H. Y., & Pai, H. C. (2015). The effect of cognitive appraisal in middle-aged women stroke survivors and the psychological health of their caregivers: A follow-up study. Journal of Clinical Nursing. doi:10.1111/jocn.12926.
Acknowledgments
We would like to gratefully acknowledge all the individuals with multiple sclerosis who completed a questionnaire, Dr. Mariusz Kowalewski, the manager of Multiple Sclerosis Rehabilitation Centre in Borne Sulinowo and Mrs. Danuta Lawniczak from the Polish Society of Multiple Sclerosis for their help in enrollment of the study participants and Mrs. Magdalena Lewandowska for her assistance in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Wilski, M., Tasiemski, T. Health-related quality of life in multiple sclerosis: role of cognitive appraisals of self, illness and treatment. Qual Life Res 25, 1761–1770 (2016). https://doi.org/10.1007/s11136-015-1204-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1204-3