Abstract
Objective
To determine the relationship between baseline overall HRQOL as well as domain-specific HRQOL and incident cardiovascular (CV) events over 10 years of follow-up in a Chinese general population.
Methods
We examined the above link using data from a prospective cohort study, conducted between 2002 and 2012 in 11 villages of Beijing. HRQOL was assessed using Chinese 35-item quality of life instrument, and CV risk factors were recorded in either 2002 or 2005. Subjects were followed through the end of the study period, or until they were censored due to an incident CV event [including myocardial infarction (MI) and stroke] or loss to follow-up.
Results
A total of 1739 participants were eligible to be included in the current study [female 64.2 %, age 57.7 (8.4) years]. There were a total of 190 CV events during the follow-up (14,364 total person-years). Participants in the bottom 20 % had 85 % increase in risk of CV event [hazard ratio (HR) 1.85; 95 % CI 1.14–3.02] compared to those in top 20 % of overall HRQOL, after adjusting for sex, age, education, marital status, smoking, alcohol consumption, being physically active, hypertension, diabetes, high cholesterol, and obesity. Among the six HRQOL domains, the independence domain had the largest effect size (fully adjusted HR 2.91; 95 % CI 1.67–5.07), followed by physical domain (HR 1.66; 95 % CI 1.03–2.67). Other domains did not predict the incidence CV events in this cohort.
Conclusions
While overall lower HRQOL predicts subsequent risk of stroke and MI events, this appeared to be driven mainly by the independence domain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases (CVD) account for the largest fraction of deaths related to non-communicable diseases globally [1]. About 80 % risk of CVD could be predicted by known CVD risk factors [2], i.e., older age, male sex, high systolic blood pressure, high serum total cholesterol, high body mass index, current smoking status, and diabetes mellitus in China [2] and in the USA [3]. It is still unknown what the major determinants are for the remaining 20 % risk in CVD.
Health-related quality of life (HRQOL) has been defined as an ‘individual’s perception of their position in life, in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns [4]. Traditionally, quality of life has been considered as a major outcome of CVD [5, 6]. Relatively fewer studies explore whether lower HRQOL is a risk factor of CVD. A small prospective study of 416 middle-aged blue-collar workers followed for 3 years showed that impaired quality of life was related to high prevalence of overt cardiovascular disease [7]. Recently, Muñoz et al. [8] found that Physical Health assessed by SF-12 was significantly associated with CV events 3724 individuals during 6.3-year follow-up in a Spain Community-based cohort. Myint et al. [9] have also shown physical component summary score of SF-36 predicted incidence of CVD in a 6.5 years of follow-up in EPIC-Norfolk, a large population-based study in UK. However, it is not well known that early impaired total HRQOL influence later CVD event in longer-term follow-up in non-European populations, and if so which domains of HRQOL serves as the best predictor of such a risk.
The primary objective of this study was to explore whether impaired HRQOL influence 10-year CV events independently of known CV risk factors in a large Chinese general population sample. The secondary objective was to examine the relationship with individual domains of the HRQOL.
Methods
Study population
The current study sample was drawn from the original cohort of the People’s Republic of China-United States of America (PRC-USA) Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology which has been published elsewhere [10, 11]. Briefly, a clustered random sample of 2313 participants was selected from all 11 villages of the Shijingshan district of Beijing in autumn 1993 and autumn 1994. Of the 2313 participants, 39 participants died, 71 were excluded because of a previous history of CHD and/or stroke, and the remaining 2203 participants were invited for health-related quality of life assessment in either 2002 or 2005. Of the total 2203 eligible participants, 1815 individuals (1356 included in 2002 and 459 included in 2005; response rate 82 %, 662 men and 1153 women) consented to participate in the HRQOL study and underwent baseline HRQOL measurements (see Supplement A in File S1).
Baseline health-related quality of life (HRQOL) measurement
Health-related quality of life was assessed using self-reported Chinese 35-item quality of life instrument (QOL-35) [11, 12]. The reliability and validity of the QOL-35 has been previously reported [13]. The 35 items in the QOL-35 were classified into six domains and then the additional item of HRQOL transition based on our previous research (Supplement B in File S1). HRQOL scores for each item, domain, and total HRQOL score were scaled to range from 0 to 100 (Supplement C in File S1).
Measurement of baseline risk factors
At the baseline, all major conventional cardiovascular risk factors were measured using the standard protocols of the PRC-USA study [14]. Date of birth, sex, educational level, marital status, smoking, alcohol consumption, and medication used were collected using a standard questionnaire. Based on self-reported data, current smoking was defined as having smoked at least one cigarette per day for at least the past year. Former smoker was defined as having stopped smoking for at least the past month. Alcohol consumption was defined as yes for those drinking alcohol at least once per week. Being physically active was defined as playing sports (walk, run, ride bike, dance, swim, play balls, etc.) at least half an hour each day for at least the past year. Hypertension was defined as mean systolic blood pressure (SBP) ≥ 140 mm Hg and/or mean diastolic blood pressure (DBP) ≥ 90 mm Hg (based on 3 measurements), or the use of antihypertensive drugs in the past 2 weeks. Diabetes mellitus (DM) was defined as a fasting blood glucose ≥126 mg/dL or current use of insulin or oral hypoglycemic medication. Body mass index (BMI) was calculated as kg/m2, and obesity was defined as BMI ≥ 28 kg/m2 according to the threshold for Chinese population [15]. High cholesterol was defined as fasting serum cholesterol ≥200 mg/dL.
Follow-up and definition of cardiovascular events
Follow-up data on deaths and cardiovascular events (including myocardial infarction and stroke) were obtained by re-surveying the cohort in 2005, 2007, 2010, and 2012 according to a standardized protocol. The follow-up data for MI and stroke events were first collected by investigators using a standardized form at each follow-up survey via face-to-face interviews (80.3 %) or telephone interviews (19.7 %). The standardized form for MI collected information on the date of acute occurrence, name of hospital, symptoms, ECG diagnosis, serum myocardial enzymes levels, co-morbid clinical conditions, treatments, survival status at 28 days, autopsy if available and applicable. The form for stroke collected the information on the date of occurrence, name of hospital, symptoms and duration, co-morbid clinical conditions, CT scan, type of stroke, treatments, survival status at 28 days, autopsy if available and applicable. Suspected events were further investigated with a repeat visit of a doctor to the patient or family or the hospital if applicable to collect clinical data to confirm the diagnosis (including symptoms, personal history, ECG, brain CT scan or autopsy findings). The final diagnosis was made by independent adjudication committee which reviewed the medical history and death certificates using pre-specified criteria from the MONICA Project [16] and the PRC-USA Collaborative Study [14].
Only the first non-fatal or fatal myocardial infarction (MI) and stroke during the follow-up were used for analysis. Criteria used to define MI were adapted from diagnostic criteria developed by the PRC-USA Collaborative Study and have been described in detail elsewhere. MI was defined as having had clinical diagnosis of fatal or non-fatal MI with severe chest pain for at least half an hour with supporting evidence (ECG, cardiac enzymes) as per standardized data collection form. Non-fatal or fatal stroke was defined using the WHO MONICA criteria 10: rapidly developing signs of focal or global disturbance of cerebral function lasting >24 h (unless interrupted by surgery or death) with no apparent non-vascular cause. The definition of stroke included cerebral thrombosis, cerebral embolism, intracerebral hemorrhage, and subarachnoid hemorrhage. Those cerebral events associated with transient ischemic attacks and silent brain infarctions (cases without obvious clinical symptoms or signs), trauma, hematological disorder or malignancy were not included. All of the stroke cases underwent brain CT scans.
The CV event was defined as the composite of MIs and stroke events. If an individual had both MI and stroke, only one CVD event, whichever occurred first was included.
Statistical analysis
For descriptive purpose, means or medians were calculated to present continuous variables depending on sample distribution and were compared by t tests or appropriate nonparametric tests between those with and without CV events during the follow-up. Categorical variables were presented as number (percentage) and differences between groups were tested by Pearson Chi-squared analysis. The cardiovascular events rate was calculated as the number of CV events per 1000 person-years of follow-up. Cox proportional hazards regression models were fitted to cardiovascular events data to calculate hazard ratios (HR) and corresponding 95 % confidence intervals (CI). Model 1 fitted an age- and sex-adjusted Cox model regressing cardiovascular events on Total HRQOL score (highest quintiles as the reference category). Model 2 fitted a multivariable Cox model to account for confounding variables, including sex, age, education level, marital status, smoking, alcohol consumption, being physically active, hypertension, diabetes, high cholesterol and obesity. Both models were then constructed for individual six HRQOL domains and HRQOL transition. To eliminate the impact of reverse causality, analyses were repeated after exclusion of early event occurring within the first 2 years of follow-up. We also constructed used Cox regression models to analyze the prospective relationship between HRQOL and incidence of myocardial infarction and stroke, respectively. Similar sensitivity analyses were carried out for these two outcomes after excluding early events occurring within 2 years of follow-up to rule out reverse causality. The C-statistics on area under the receiver operating characteristic curve (ROC) was used to check whether the addition of total HRQOL scores or independence domain improve the predictive ability of the classic Chinese prediction model [2] based on this current Chinese data. All p values were two sided, and values <0.05 were considered significant. All analyses were performed using SAS 9.2 (SAS Institute Inc, Cary, NC, USA).
Results
A total of the 1739 participants (622 men and 1117 women) were included in this report. The mean age of the cohort was 57.7 (SD 8.4) years at the baseline. During the follow-up period (median 10.1 years, range 0.2–10.2 years), there were a total of 190 CV events and 109 people were lost to follow-up. During the 14,364 total person-years of follow-up, the incidence of CV events was 13.23 events per 1000 person-years. Participants who developed CV events during the follow-up tended to be older, single/widowed, had no school education, more likely to be cigarette smokers, had higher prevalence of risk factors such as hypertension and diabetes, had lower total HRQOL score and lower score for physical domain at the baseline (p < 0.05) (Table 1).
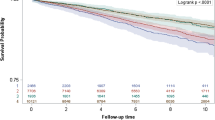
The incidence of CV events decreased from 18.43 per 1000 person-years in people with lowest total HRQOL score (quintile 1) to 8.88 per 1000 person-years in top quintile (quintile 5). Model 1 showed that, compared to those with the highest quintile HRQOL score (quintile 5), the adjusted HR increased from 1.23 (95 % CI 0.74–2.03) in the quintile 4 group to 1.86 (95 % CI 1.15–3.01) in the quintile 1 group (p for trend <0.05). The similar trend was observed in fully adjusted model (Model 2): HR increased from 1.19 (95 % CI 0.72–1.97) in the quintile 4 group to 1.85 (95 % CI 1.14–3.02) in the quintile 1 group (p for trend <0.05) (Table 2).
Domain-specific analyses showed that the Independence domain had the strongest prospective association with future CV events (quintile 1 vs. quintile 5, HR 3.09; 95 % CI 1.79–5.53) (p for trend <0.05), which was followed by the physical domain (HR 1.67; 95 % CI 1.04–2.69) (p for trend <0.05). The remaining Psychological, General, Social, Environmental, and the HRQOL transition item did not show any statistically significant relationship with the future CV events over 10 years of follow-up. Similar results were observed in fully adjusted models albeit with mild attenuation in effect size (Table 3).
Then we did receiver operating characteristic curve (ROC) analyses. The area under curve (AUC) increased from 0.6982 (95 % CI 0.6528–0.7436) for the classic Chinese prediction model [2] to 0.7174 (0.6719–0.7629) (p = 0.0029 using C-statistics) as total HRQOL score was added, and to 0.7257 (0.6805–0.7710) (p = 0.0005 using C-statistics) as independence domain was added. The addition of other domains did not improve the predictive ability.
We furthered to analyze the association of HRQOL with MI and stroke events, respectively. Fully adjusted Cox regression models showed that lower total HRQOL score was significantly associated with MI event (quintile 1 vs. quintile 5, HR 5.37; 95 % CI 1.50–5.53), while the association with stroke events was weaker and not significant (HR 1.62; 95 % CI 0.95–2.76) (Supplement D in File S1). Of six individual domains, Physical and Independent domains were significantly associated with incident MI events, while only Independent domain was significantly associated with incident stroke events. Overall, the HRs were higher for MI than for stroke.
In order to eliminate the potential influence of subclinical CVD (prior to CV events) impacting on the HRQOL (i.e., reversed causality issue), we performed sensitivity analyses after excluding 55 early events occurring within the first 2 years of follow-up. This did not alter the results (Supplement E in File S1).
Discussion
Our results demonstrate that early impaired total HRQOL score at middle age (mean age ~ 58 years) is associated with higher incidence of 10-year CV events in a community-based Chinese population. The relationship depends on the degree of impaired total HRQOL score, but independent of other known personal risk factors such as age, sex, education level, marital status, being physically active, alcohol consumption, and other classical CVD risk factors (smoking, hypertension, diabetes, high cholesterol, and obesity). Among domains of HRQOL, independence and physical domains were two strongest predictors of subsequent CVD incidence. Indeed, adding total HRQOL score or independence domain has improved the predictive power of traditional model of CVD risk prediction in this population.
Since Framingham study, over the past few decades it was established that approximately 80 % of cardiovascular events could be attributed by five modifiable major risk factors (smoking, hypertension, diabetes, high cholesterol, and obesity) in addition to non-modifiable risk factors, age and sex [3]. A large cohort study in China has also shown that about 80 % of cardiovascular events could be predicted by same risk factors [2]. Therefore, our finding that impaired baseline HRQOL predicts subsequent CV events independently of traditional risk factors in the present study is an important contribution and provide deeper insight and better understanding of new and novel CV risk factors.
HRQOL used in this study (Chinese QOL-35 item) is a complex subjective indicator that self-reported by participants based on own perception of their position in life in relation to their goals, expectations, standards, and concerns [4]. Our findings suggest that in clinical and preventive practice of cardiovascular medicine, clinicians should pay more attention on patients’ quality of life in addition to focus on traditional risk factors. A randomized controlled trial showed that incorporating standardized HRQOL assessments in daily clinical oncology practice facilitates the discussion of HRQOL issues and can heighten physicians’ awareness of their patients’ HRQOL [17]. Our finding suggest that it may be useful to include quality of life assessment using validated questionnaire in assessment of CV risk, which may be particularly useful in early identification of those who are at risk of CVD. Identifying these high-risk individuals could increase the efficacy of CVD treatment and prevention strategies.
Of the six domains of QOL-35 item score, the independence domain was the strongest predictor of subsequent CVD incidence. Myint et al. [9] have also shown similar association although they examined the prediction of CVD risk using physical functioning using physical component summary score (PCS) of Short-Form 36 (SF-36), and their study was confined to cardiovascular outcome only. However, Myint et al. [18] also noted the similar link between PCS and stroke risk in a separate paper. Intuitively, it is plausible that people with better ability of physical activities are more likely to be independent. Indeed, the presence or absence of difficulty in performing physical activities is among the items that constitute Independent domain, along with other items which assess the daily need for medicines or treatment, and satisfaction in independent living ability. This information reflects the health status in the facet of ability of independent activity which cannot be measured by traditional risk factors, such as hypertension, diabetes, obesity, etc. Further, the associations between Independent domain and these risk factors namely hypertension, obesity, dyslipidemia, and high glucose were generally weak (range of age–sex-adjusted correlation coefficient was from −0.085 to 0.014) (Supplement F in File S1). Thus, the association of Independent Domain of HRQOL with future incidence of CV events was independent of traditional risk factors. This finding is consistent with our previous finding that the strongest domain associated with all-cause mortality was independence domain [11].
In the present study, the second strongest domain associated with CV events was physical domain which included 5 items comprising bodily pain, pain interfered with normal life, appetite, difficulties in sleeping, and fatigue. These items mainly reflect the bodily physiological health determined by others unmeasured factors in the traditional risk calculations but perceived by individuals, which cannot also be determined by traditional indicators such as blood pressure, serum glucose, serum cholesterol, etc. [19]. Thus its association with CV events was also independent of traditional risk factors. In some short quality of life questionnaires, both independent and physical domains were often combined as one Physical Health domain. Recently, Muñoz et al. [8] found that Physical Health assessed by SF-12 was significantly associated with CV events in a population sample of 3724 individuals in Spain.
Compared to the strong link observed with independent and physical domains and CVD event, the associations between Psychological, Social, Environmental, and General domain and subsequent CV events were weaker and statistically not significant. This is consistent with our previous finding that associations of these domains with all-cause mortality were weaker than independent and physical domain [11]. This may be due to the fact that these domains are indirect indicators (markers) that reflect physical health rather than a predictor of future CV events.
In the QOL-35, there was a item on HRQOL transition in the past 1 year which asked the participants the following question: “Compared to a year ago, how would you rate your quality of life now?” [11]. The association of HRQOL transition with CV events was weak and not significant. It may be due to the fact this item may not a sensitive item. In other words, it may have larger minimally clinically significant effect size and change in HRQOL over a short period of time may not able to adequately capture the subsequent CV risk independently of point estimate/self-report current HRQOL.
There are some limitations in our study. First, the 76 (4.2 %) study participants who were excluded likely have a higher overall risk of CV events (i.e., older age, lower HRQOL scores) [11]. However, this will only introduce bias toward the null hypothesis and attenuated the observed prospective association between HRQOL and CV events. Another limitation in our study is the statistical power might be relatively low due to low CVD event rates (13.23 events per 1000 person-years of follow-up) as the population is middle-aged population. In addition, we used HRQOL and other risk factors measured at baseline, and as such, were unable to account for changes in HRQOL or other time-varying confounders, in estimating CV events during the study period. The study was based on data from those without known cardiovascular disease, and the results should not be directly applied to those with known cardiovascular disease. Because the outcome events in the present study did not encompass other CV events such as angina pectoris or claudication, the observed association between HRQOL and CV events is likely to be attenuation of the actual association between HRQOL and any coronary heart disease (CHD) events. As an observational study, while causality could not be implied, we robustly adjusted for confounders and the relationship observed was also prospective with well-defined case ascertainment approach. Further, repeating the analyses after excluding early event within first 2 years of follow-up did not alter the results, suggesting reverse causality (i.e., low HRQOL due to subclinical illness) is very unlikely.
Conclusions
Our findings from a population-based, prospective cohort study of Chinese population provide evidence that impaired health-related quality of life, especially the perception of the subjects on inability to live independently and poor physical function, increases the CVD risk, which is independent of other known classical risk factors. Assessment of HRQOL in people with heightened CV risk may help in correctly identifying people at the highest risk of future CV events and may help to employ appropriate preventative strategy. This may have impact on overall global burden of major CVDs.
References
Murray, C. J., Vos, T., Lozano, R., et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380(9859), 2197–2223.
Wu, Y., Liu, X., Li, X., Li, Y., Zhao, L., Chen, Z., et al. (2006). Estimation of 10-year risk of fatal and nonfatal ischemic cardiovascular diseases in Chinese adults. Circulation, 114, 2217–2225.
Grundy, S. M., D’Agostino, R. B, Sr, Mosca, L., Burke, G. L., Wilson, P. W., Rader, D. J., et al. (2001). Cardiovascular risk assessment based on US cohort studies: Findings from a national heart, lung, and blood institute workshop. Circulation, 104(4), 491–496.
The Whoqol Group. (1998). The World Health Organization Quality of Life Assessment (WHOQOL): Development and general psychometric properties. Social Sciences and Medicine, 46(12), 1569–1585.
Boini, S., Briancon, S., Guillemin, F., Galan, P., & Hercberg, S. (2006). Occurrence of coronary artery disease has an adverse impact on health-related quality of life: A longitudinal controlled study. International Journal of Cardiology, 113(2), 215–222.
O’Neil, A., Stevenson, C. E., Williams, E. D., Mortimer, D., Oldenburg, B., & Sanderson, K. (2013). The health-related quality of life burden of co-morbid cardiovascular disease and major depressive disorder in Australia: Findings from a population-based, cross-sectional study. Quality of Life Research, 22(1), 37–44.
Siegrist, J. (1987). Impaired quality of life as a risk factor in cardiovascular disease. Journal of Chronic Diseases, 40(6), 571–578.
Munoz, M. A., Subirana, I., Elosua, R., Covas, M. I., Baena-Diez, J. M., Ramos, R., et al. (2011). Utility of a short quality of life questionnaire to predict cardiovascular events. International Journal of Cardiology, 151(3), 392–394.
Myint, P. K., Luben, R. N., Surtees, P. G., Wainwright, N. W., Wareham, N. J., & Khaw, K. T. (2010). Physical functional health predicts the incidence of coronary heart disease in the European Prospective Investigation into Cancer-Norfolk prospective population-based study. International Journal of Epidemiology, 39(4), 996–1003.
Vollmer, W. M., Tsai, R., Wu, Y., Li, Y. H., Johnson, L. R., Williams, O. D., et al. (2002). Patterns of lung function in asymptomatic nonsmoking men and women in the People’s Republic of China. Annals of Epidemiology, 12(5), 295–302.
Xie, G., Laskowitz, D. T., Turner, E. L., Egger, J. R., Shi, P., Ren, F., et al. (2014). Baseline health-related quality of life and 10-year all-cause mortality among 1739 Chinese adults. PLoS ONE, 9(7), e101527.
Wu, Y. F., Xie, G. Q., Li, Y., Zhou, B. F., Zhang, P. H., Ren, F. X., et al. (2005). The development and Assessment on the general quality of life intrument for Chinese people. Zhonghua Liu Xing Bing Xue Za Zhi, 26(10), 751–756.
Xie, G., Li, Y., Shi, P., Zhou, B., Zhang, P., & Wu, Y. (2005). Baseline pulmonary function and quality of life 9 years later in a middle-aged Chinese population. Chest, 128(4), 2448–2457.
People's Republic of China-United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. (1992). An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People’s Republic of China. Baseline report from the P.R.C.–U.S.A. Circulation, 85(3), 1083–1096.
Chen, C., Lu, F. C., & Department of Disease Control Ministry of Health, PR China. (2004). Guidelines for prevention and control of overweight and obesity in Chinese adults. Biomedical and Environmental Sciences, 17(supplement), 1–36.
Truelsen, T., Mahonen, M., Tolonen, H., Asplund, K., Bonita, R., & Vanuzzo, D. (2003). Trends in stroke and coronary heart disease in the WHO MONICA Project. Stroke, 34(6), 1346–1352.
Detmar, S. B., Muller, M. J., Schornagel, J. H., Wever, L. D., & Aaronson, N. K. (2002). Health-related quality-of-life assessments and patient–physician communication: A randomized controlled trial. JAMA, 288(23), 3027–3034.
Myint, P. K., Luben, R. N., Surtees, P. G., Wainwright, N. W., Welch, A. A., Bingham, S. A., et al. (2007). Self-reported mental health-related quality of life and mortality in men and women in the European Prospective Investigation into Cancer (EPIC-Norfolk): A prospective population study. Psychosomatic Medicine, 69(5), 410–414.
Xie, G., Li, Y., Zhou, B., Zhang, P., Shi, P., Ren, F., & Wu, Y. (2006). Factors associated with quality of life in a natural population. Chinese Journal of Chronic Disease, 5(1), 1–7.
Acknowledgments
We thank all scientists from USA and China for their hard work to establish the study cohort and a series of international standardized methods. We also thank all study participants.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by grants from the People’s Republic of China National 10th Five-Year Plan Science and Technology Key Projects (Grant No. 2001BA703B01), the National Natural Science Foundation of China (Grant Nos. 30471494 and 30872168).
Conflict of interest
None.
Patient consent
Obtained.
Ethics approval
The Peking University Health Science Center Ethics Committee approved the examination and follow-up in 2007 and 2012 and the Cardiovascular Institute and Fuwai Hospital Ethics Committee approved other studies in 2002, 2005, and 2010.
Additional information
Gaoqiang Xie and Henyun Zou have contributed equally as co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xie, G., Zou, H., Myint, P.K. et al. Baseline overall health-related quality of life predicts the 10-year incidence of cardiovascular events in a Chinese population. Qual Life Res 25, 363–371 (2016). https://doi.org/10.1007/s11136-015-1066-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1066-8