Abstract
Purpose
There were two objectives in this study: (1) to identify, among women and men with MS, the extent to which different MS-related symptoms, including fatigue, pain, sleep disturbance, depression, anxiety, irritability, cognitive impairment, spasticity, and poor balance, cluster and (2) to compare the contribution of generated symptom clusters to MS consequences including functional walking capacity, perceived health, illness intrusiveness, and quality of life (QOL).
Methods
This was a cross-sectional study. A center-stratified random sample comprising 139 women and 49 men was recruited from three major MS clinics in Montreal. Subjects completed several self-report and performance-based measures that assessed symptoms and downstream MS consequences. Hierarchical and K-means cluster analyses were used to create clusters.
Results
Three symptom clusters were identified. Cluster 1, labeled the “emotional/cognitive symptom cluster,” comprised of depression, anxiety, cognitive impairments, and irritability. The second cluster, labeled the “physical symptom cluster,” included pain, fatigue, and sleep disorders. Cluster 3, labeled the “motor symptom cluster,” included spasticity and poor balance. Furthermore, the motor symptom cluster had a strong effect on functional walking capacity, while it did not affect significantly illness intrusiveness and QOL. On the other hand, the physical symptom clusters and emotional/cognitive symptom clusters showed a significant contribution to prediction of illness intrusiveness and QOL. All symptom clusters showed a significant effect in predicting the overall variability of perceived health status.
Conclusions
The findings of this study provide useful information to help healthcare professionals, clinicians, and researchers to target symptoms that are often in the same cluster when one or two of them are present. Identification of the strength of the contributions of each symptom clusters to the targeted MS consequences would further help to prioritize treatment approaches for the MS population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic, inflammatory disease of the central nervous system (CNS) [1]. Canada has one of the highest prevalence rates of MS in the world, affecting as many as 240 people per 100,000 [2].
MS symptoms can be either a direct result of disease itself, or related to treatments [3]. Symptoms of MS affect people differently and, even in the same person, change from time to time. MS symptoms mostly include fatigue [4, 5], pain [6–10], sleep disturbance [11–14], balance problems [15], spasticity [16], memory and concentration problems [17, 18], depression [19], anxiety, and irritability [11, 20].
The majority of MS studies are focused on a single symptom and its related prevalence, assessment, and management [21]. However, symptoms of MS often occur concurrently [21–26].
Two [27] or more [28–32] symptoms that are related to each other and occur together are defined as a symptom cluster (SC). The relationships among symptoms are complex and can be either a real relationship (common etiology mechanism) or a statistical association via a shared common variance [28, 30, 31]. Symptom clusters of pain, fatigue, and depression [33] as well as poor sleep quality and perceived cognitive dysfunction have been identified in persons with MS [21, 26, 33]. Based on the theory of unpleasant symptoms [34, 35], it is believed that multiple concurrent symptoms, in comparison with a single symptom, have a stronger effect on disease consequences [28, 32, 33, 36, 37].
Walking difficulty affects more than 75 % of persons with MS [38]. Reduced walking capacity is related, either alone or in combination, to MS symptoms such as muscle weakness, poor balance, fatigue, pain, and depression [39–42]. Diminished perceived health is another frequent disease consequence among individuals with MS and has been found to be associated with the presence and severity of MS symptoms such as muscle weakness, pain, and fatigue [43]. Due to the impact of MS on symptoms, activities of daily living, and health perception, MS is one of the more intrusive illnesses, affecting lifestyle, plans for the future, activities, and interests [44–48]. Literature on illness intrusiveness in MS shows that an increased perceived lifestyle disruption is associated with poor sleep quality, psychological distress [49], fatigue [50], and mental health [51]. As a result of the psychological and physical challenges confronted by people with MS, they rate their quality of life (QOL) lower than healthy peers. Fatigue, depression, cognitive impairment, muscle weakness, gait disturbance, and disease severity have been found to be associated with poor QOL among MS persons [52–58].
Symptom clusters have been investigated broadly in other clinical conditions such as cancer [59, 60], brain tumors [61], and heart disease [28, 62, 63]. A search of the MS literature using the term “symptom cluster” provided only a few citations of cluster analyses [21, 26, 32, 33, 64–66]. The majority of studies on MS and symptom clusters have examined the clusters of pain–depression–fatigue, and sometimes sleep disturbances and cognitive impairment. However, the existence and composition of many MS-related symptoms such as poor balance, spasticity, anxiety, and irritability across the symptom clusters still remain unanswered. In addition, some of the previous studies on symptom clusters in MS used small samples of convenience and a single statistical approach. Furthermore, this study was as part of a larger study on “Gender Life Impact of MS.” Subjects completed a battery of self-report and performance-based measures that assessed symptoms and downstream MS consequences. The preliminary results of the original study showed that the symptoms and disease consequence included in the current study were the most common symptoms and MS consequences experienced by participants.
There were two objectives in this study: (1) to identify, among women and men with MS, the extent to which different MS-related symptoms, including fatigue, pain, sleep disturbance, depression, anxiety, irritability, cognitive impairment, spasticity, and poor balance, cluster and (2) compare the contribution of generated symptom clusters to MS consequences, including functional walking capacity, perceived health, illness intrusiveness, and QOL.
Methods
Participants
A center-stratified random sample of 139 women and 49 men, registered at the three major MS clinics in greater Montreal including: Montreal Neurological Hospital, Centre Hospitalier de l’Université de Montréal, and Clinique Neuro Rive-Sud, comprised the study sample population. Eligibility was based on diagnosis of MS since 1995. Participants had to be older than 18 years old. Participants with severe cognitive impairments and preexisting health conditions affecting functioning such as cancer, heart disease, and arthritis were excluded from participating in the study. Participants who had a relapse in the preceding month of evaluation were excluded from participating in the study as well.
Measures
Eligible people were sent a letter of invitation from the director of each related MS clinic. A research coordinator contacted the participants to verify whether persons met the eligibility criteria and invited them to participate. If persons consented to participate, an appointment was arranged for assessment of study measures. Table 1 outlines the measurement strategy, study variables and their related constructs, units, and scales.
Sociodemographics characteristics
Sociodemographic factors of gender, age, weight, and employment status were recorded on the day of testing using the sociodemographic questionnaire.
Disease-related characteristics
The clinical records of each person were reviewed to obtain data on MS-related characteristics. The severity of neurological impairment was assessed by a neurologist based on the Expanded Disability Status Scale (EDSS) [67].
Symptoms
The two-item bodily pain subscale (BPS) from RAND-36 was used as a measure of pain severity [68]. The scale scores from 0 to 100, with lower scores indicating higher levels of pain severity [68]. Internal consistency of this scale in the MS population has been reported to range from 0.77 to 0.94 [69, 70].
The Vitality subscale of RAND-36 was used, which is comprised of 4 items asking about the level of energy and feeling of tiredness [68]. The sum scores range from 0 to 100, higher score indicating lower fatigue. RAND-36 has been used widely in MS population, and its psychometric properties have been provided [71, 72].
To assess sleep disturbance, we used a specific sleep questionnaire created from a Rasch analysis of the Pittsburgh sleep quality index (PSQI) [73]. The scale contains 4 items that assess factors affecting sleep quality during the previous month. Total score ranges from 0 to 8, higher score indicating worse sleep quality. Reliability and validity of the original questionnaire have been determined [73].
The levels of anxiety and depression of persons were measured using the hospital anxiety and depression scale (HADS) [74, 75]. The HADS has 14 items; each item on the questionnaire is scored from 0 “most of the time” to 3 “not at all,” and the total score ranges between 0 and 21 for either anxiety or depression [76]. Higher scores indicate worse depression/anxiety symptoms. The HADS is a reliable and valid tool and has been used in a number of MS studies [74, 76–78].
Irritability was measured using a specific irritability index created from Rasch analysis of psychiatric symptom index (PSI) [79]. The scale comprised 4 items ranging from 1 “never” to 4 “very often.” A maximum total score of 16 representing the most irritability symptom.
Cognitive impairment was assessed using the perceived deficits questionnaire (PDQ) [80]. PDQ contains 20 items, each score ranging from 0 to 4 with a maximum total score of 80, where higher scores indicate greater cognitive impairment [81]. The validity and reliability of PDQ in MS persons have been widely accepted [80, 82].
Spasticity was assessed using the modified Ashworth scale (MAS) [83]. The MAS assigns grades to a manually determined resistance of muscle [83]. For each segment, scores range from 0 (no increase in muscle tone) to 5 (affected part rigid in flexion or extension) with a maximum total score of 60 for both sides. Validity and reliability of MAS in a number of MS studies have been examined [83–88].
To assess balance, we used the EQUI-Scale, which is a MS-specific balance scale created using Rasch modeling from the items of Tinetti Performance Oriented Balance Scale and the Berg Balance Scale [89]. The scale has ten items that are listed in order of difficulty. Each item scores from 0 to 2 with a maximum total score of 20; higher scores indicate better balance skills [89].
Disease consequences
Walking capacity was measured using the six-minute walk test (6MWT) in which the maximum distance a person can walk over 6 min at their own pace is recorded [90]. The 6MWT has been used widely in MS population [91] and is correlated strongly with the 12-Item MS Walking Scale (r = 0.81, P < 0.001) [92] and the shuttle Walk Test (r = 0.68) [93]. An excellent test–retest reliability (ICC = 0.96) and inter-rater reliability (ICC = 0.93) have been reported for the 6MWT [94].
Perceived health status was measured using the EuroQOL VAS (EQ-VAS) [95]. Participants were asked to rate their overall health on 0–100 VAS scale, with 0 showing the worst perceived health and 100 showing the best perceived health. VAS has been widely used in research and clinical settings and has several good qualities in terms of practicality, sensitivity, reliability, and adaptability [96].
Illness intrusiveness was measured using the Illness Intrusiveness Ratings Scale, which determines the ratings of the degree to which one’s illness interferes with different life domains [97]. It consists of 13 questions each with a 7-point response option, with a maximum total score that can range from 13 to 91. Higher scores indicate increased illness intrusiveness. The psychometric properties of the scale have been administered across numerous chronic disease populations including MS [48, 98].
Person generated index (PGI) was used to capture life domains that have been affected by MS and its related treatment [99–101]. The total score ranges from 0 to 100; higher scores indicates better health QOL. The reliability, validity, and responsiveness of the PGI have been assessed [99, 100, 102].
Statistical analyses
Descriptive statistics were used to describe the sample and summarize data. Selection bias was tested using chi-squared test for categorical variables and t test for continuous variables. Associations between all variables were assessed using Spearman’s and Pearson’s correlation coefficients for categorical and continuous variables, respectively.
As in contrast to other scales, higher scores from fatigue, pain, and balance scales indicated better health status; scores from these scales were reversed. In addition, as the measurement scales differed, each scale was transformed into a 0–100 scores. Hierarchical (centroid, average, and ward methods) and non-hierarchical clustering with a squared Euclidean distance were used. Hierarchical cluster analysis, characterized by the development of a hierarchy (tree-like structure), is the main statistical method for providing homogeneous clusters. It begins with treating each symptom as a separate cluster and then merges the similar symptoms into consecutively larger clusters. While hierarchical cluster analysis does not need the number of clusters as input, the non-hierarchical clustering method referred to as k-means clustering uses a defined number of clusters. Additionally, a hierarchical tree diagram, called a dendrogram, and a scree plot were produced to help identify the correct number of clusters. As different statistical methods may produce different SCs, exploratory factor analysis was also carried out for comparison purposes.
Since each generated cluster was to be used as a predictor of downstream outcomes, using principal component analysis, a unique value per person on each SC was generated. Then, factor loading for each symptom in a particular cluster was combined to create the SC latent variable. This cluster was then entered in multiple regression analysis to identify the relative contribution of each latent cluster on the downstream disease consequences.
Other predictor variables were disease severity, weight, sex, and age. Using stepwise multiple regression, each predictor variable was entered into the model and retained or discarded based on their contribution to the overall model (statistical significance at the 0.05, beta estimate, and R square). The standardized coefficient of each predictor was also calculated permitting a quantifiable way of identifying which predictor had the largest effect on disease consequences.
There are no rules about the appropriate number of participants in cluster analysis. The only recommendation is to critically question whether the dimensionality is not too high for the number of variables/participants to be grouped [103, 104]. Considering that there were 9 symptoms in our analysis, and in most rules-of-thumb criteria, 10–20 cases per variable are recommended, a sample size of 188 participants would be suitable for the purpose of this study.
Results
Descriptive statistics
Response rate was 52 %, and no significant difference was found between responders (n = 188) and non-responders (n = 176) on age, sex, MS severity, date of diagnosis, and duration of symptom. Sociodemographic and clinical characteristics of the sample are presented in Table 2.
Descriptive characteristics of the study variables are presented in Table 3. The mean values of pain severity and fatigue measured by RAND-36 for the whole sample were lower than age-expected norms of Canadian general population (76/100 and 66/100, respectively) [105]. Distance walked was 66 % of predicted for healthy individuals with the same age, height, and weight (range 400–700 m) [106]. Mean rating on perceived health was 73 out of 100, lower that what has been reported for a general Quebec population (mean 80) [107].
Results of correlation analysis among symptoms and outcomes of the study are presented in Table 4. Most of the variables were correlated. However, spasticity, poor balance, and walking capacity were not correlated with anxiety, cognitive deficits, and irritability.
Cluster analysis on symptoms
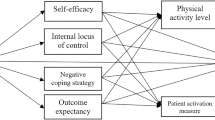
As shown in Table 5, nine symptoms formed three symptom clusters, which were the same irrespective of the analysis method used to generate clusters. Cluster 1, labeled the emotional/cognitive SC, comprised depression, anxiety, cognitive impairments, and irritability. The second cluster, labeled the physical SC, included pain, fatigue, and sleep disorders. Cluster 3, labeled the motor SC, included spasticity, and poor balance. The resulting dendrogram (Fig. 1) and scree plot further confirmed the 3-cluster solution for the study. Scree plot resulting from cluster analysis is interpreted much like a scree plot used in factor analysis where the number that appears before the distinctive break shown the cluster solution (Elbow rule). There were some differences in cluster composition by gender.
Impact of symptom clusters on disease consequences
Results of principal component analyses on each SC are presented in Table 6. As it is indicated, the factor loadings for the indicators of the SC latent variable were all sufficiently large. Additionally, all symptoms indicated almost equal weight on their particular cluster, except fatigue that has the greatest factor loading on its related latent cluster.
Table 7 displays the results of multiple linear regression analyses. Considering 6MWT, symptom clusters of spasticity and poor balance were the only clusters that showed a significant strong effect. Gender, MS severity, age, and weight also made a significant contribution to prediction of the 6MWT (P < 0.05). The final multiple regression model explained 75 % of the variance in 6MWT. The regression coefficients for gender indicated that women, on average, walked 73 m less than men. In addition, for every unit increase in spasticity and balance problems, the distance walked at the 6MWT decreased by 78 m (P < 0.0001), holding all other variables constant. A difference of 54 m is considered clinically important [108].
All symptom clusters showed significant effect in predicting the overall variability of EQ-VAS; however, the effect of physical symptom clusters was greater than others. MS severity also made a significant contribution to prediction of the perceived health (P < 0.05). The final multiple regression model explained 50 % of the variance in EQ-VAS. The regression results further showed that for every unit increase in EDSS, the individual’s perception about their health status decreased by 2, holding all other variables constant.
Illness intrusiveness was significantly predicted by physical and emotional/cognitive symptom clusters (Table 7). The final multiple regression model explained 60 % of the variance in illness intrusiveness measure. MS severity and age also made a significant contribution to prediction of illness intrusiveness. For every unit increase in EDSS, the person’s disruption of lifestyle increased by 3, while for every unit increase in age (year), it decreased by 0.4.
Finally, the results of multiple linear regression analysis on QOL indicated that again physical and emotional/cognitive symptom clusters significantly contributed in predicting the overall QOL (Table 7). However, physical symptom clusters showed the greater effect. MS severity also made a significant contribution to prediction of the QOL. The final multiple regression model explained 43 % of the variance in PGI. The results of regression results further showed that for every unit increase in EDSS, scores of QOL decreased by 5.
Discussion
We conducted this study to determine which MS symptoms are clustered together and to examine the effect of SC on MS consequences. Results identified three symptom clusters including emotional/cognitive SC, physical SC, and motor SC. In addition, patterns of women’s symptoms clusters were different from men’s. Furthermore, the current study indicated that motor SC had a strong effect on functional walking capacity, while it did not significantly affect illness intrusiveness and QOL. Physical SC and emotional/cognitive SC showed a significant contribution to prediction of illness intrusiveness and QOL. Results further suggested that all symptom clusters showed significant effect in predicting the overall variability of perceived health status.
An important finding of this study was the confirmation of the existence of SC of fatigue, pain, and sleep disorders in individuals with MS. This SC has been identified previously in the MS population [21, 32, 33] and other chronic conditions such as cancer [109]. Pain and fatigue together may produce sleep disturbance, and poor sleep can also contribute to fatigue. While the etiologies of specific clusters of symptoms are generally unknown, these symptoms are possibly correlated through common etiology due to the simultaneous damage to nerve fibers across different parts of the CNS [3] or expression of proinflammatory cytokines [110] such as Lymphotoxin-alpha (LT-alpha), interferon-gamma (IFN-gamma), and tumor necrosis factor-alpha (TNF-alpha) in cerebrospinal fluid mononuclear cells.
In contrast to another study [33], in the current study, depression was not placed in the same cluster along with pain and fatigue. This may be partly explained by the greater number of symptoms included in the analysis, especially other psychological symptoms that have a greater association with depression.
In accordance with findings reported by Lovera [23], this study confirmed the existence of a SC of emotional and cognitive deficit symptoms in persons with MS. These symptoms may be linked through a common etiological mechanism based on the cytokine-induced manifestation of sickness behavior or co-occurring of pathological changes and diffuse axonal damage across different regions of the CNS [26, 65, 110].
The current study, for the first time, provided preliminary evidence for the existence of SC of poor balance and spasticity in individuals with MS, and this is consistent with the finding in persons with cancer [109]. Muscle weakness, spasm, and stiffness in the legs may produce unsteady gait and difficulty with keeping balance.
Interestingly, findings of the current study suggested that motor SC with only two symptoms showed stronger effect on a particular outcome than a broader cluster with three or four symptoms. This is linked with the results reported by Motl [26] and inconsistent with the theory of unpleasant symptoms [34, 35]. As walking capacity, in comparison with other outcomes of the current study, is the only physical consequence of MS, it should be more affected by synergistic effects of motor symptoms such as balance and leg spasm. Another explanation can be related to the greater amount of association between walking capacity with spasticity and poor balance in comparison with other symptoms. Such findings support consideration of nature and the magnitude of association of symptoms rather than a broadly defined cluster of a higher number of symptoms.
QOL and illness intrusiveness were only affected by emotional/cognitive and physical SCs. These results are acceptable as illness intrusiveness has been found to be associated more with sleep quality, fatigue, psychological distress, and mental health [49–51]. Previous works on SC in MS have also shown that SCs of pain, fatigue, and depression as well as SCs of pain, fatigue, depression, poor sleep, and cognitive deficits were associated with diminished QOL [21, 32, 33]. Perceived health, however, was affected by all three clusters. This shows that symptoms, despite their nature and severity, all impact persons’ well-being and general health perception. Interestingly, physical SC indicated to be the most disabling SC in our study as it significantly affected all disease consequences except walking capacity. Considering that fatigue is the most disabling symptom of MS, this result is not far from our expectations.
To be able to compare the results of our study with other works and enhance the validity of our results and conclusions, we used different clustering methods. Interestingly, the results were similar. Using both analytical and conceptual approaches has been recommended for creating a SC [26, 27, 30, 31]. The conceptual approaches suggest using both bivariate correlations and factor analysis for identifying SC [30, 31]. Cluster analysis in comparison with factor analysis may produce clusters with less overlapping. Furthermore, cluster analysis is often used when there is no prior hypothesis about which symptoms should be grouped together.
We further compared the existence of such SC among men and women. Although the existence of emotional/cognitive and motor symptom clusters was confirmed across genders, fatigue and sleep disorders were clustered differently. In women, fatigue made a cluster with other psychological symptoms and cognitive deficits rather than pain and sleep disorders. This association between cognitive impairments, fatigue, and emotional distress has already been reported [82]. On the other hand, in men, sleep disorders were placed in the same cluster with spasticity and poor balance rather than with pain and fatigue. This difference in the sex SC compositions might be linked with different synergetic effects of symptoms or underlying mechanisms of symptoms in men and women [27, 28, 30, 31].
This study has several strengths. While the majority of previous studies on SC in MS had a small sample size and included mostly women, we believe this is the first application of cluster analysis to gender differences using a well-designed epidemiologic study of MS. The study sample was randomly selected from three different MS clinics in the greater Montreal area from populations who were culturally diverse and who were living in different areas of the city, including the whole range of disease severity, type, and gender. We then believe it is representative of the general MS population. However, as we only included persons diagnosed since 1995, this sample may not be fully generalizable to MS persons diagnosed before 1995 [111]. Finally we, for the first time, compared the predictability of different clusters on the downstream disease consequences.
A limitation of this study was to examine symptom clusters and their association with several MS consequences using a cross-sectional pattern. So it was not possible to examine changes in the number and pattern of symptom clusters and their effects on outcomes over the time. This issue is particularly important in MS because as disease progresses throughout its course, variables contributing to each cluster could be different.
Results from the current study provide useful information to help healthcare professionals, clinicians, and researchers to recognize SC in MS and target symptoms that are often in the same cluster when one or two of them are present. Identification of the strength of the contributions of each SC to the targeted MS consequences is essential for their improvement as this would further help researchers, clinicians, and professionals to prioritize treatment approaches for the MS population.
There are many questions in the area of SC that need more research and consideration, for instance: methodological and statistical challenges related to clustering, number of symptoms included in the cluster, degree of correlation among symptoms, and the length of time the symptoms occur concurrently [28, 30, 31, 112]. Moreover, researchers will need to determine which dimensions of a symptom (i.e., presence and severity) are critical for the assessment of a symptom within a SC [26, 32, 33, 65]. Longitudinal studies are also needed to evaluate the change in pattern of clusters over time. Future efforts also need to examine the validity of these symptom clusters across different MS types, severity, and age. More research needs to be done on etiology or biologic mechanisms of symptom clusters to better understand the connection between symptoms and inflammatory cytokine factors.
Finally, although the preliminary results of this manuscript provided us with new insights on the relationship between MS symptoms and several important disease consequences, the analytical methods that we used in this study could only determine the direct relationship among symptoms and disease consequences. For example, regression only predicts variance in a single outcome variable due to the direct effects of variability of several observed predictors, and not an indirect effect where the relationship between a predictor and outcome is mediated by an intervening variable. Advanced statistical methods such as structure equation modeling (SEM) are needed to simultaneously examine both direct and indirect relationships between and among predictor symptoms and their impacts on an individual’s life.
Conclusion
Overall, the findings of the current study provide preliminary results for considering the role of the motor SC as an independent correlate of functional walking capacity in persons with MS. Moreover, physical SCs indicated to be the most disabling SC as it affected all other health outcomes except walking capacity. Illness intrusiveness has been affected mostly by the emotional/cognitive SC, while perceived health status and QOL are mostly affected by physical symptoms. The role of symptoms in MS consequences is an important area of research as it may lead to identification of appropriate intervention approaches to adequately manage symptoms in persons with MS.
References
Noseworthy, J. H., Lucchinetti, C., Rodriguez, M., & Weinshenker, B. G. (2000). Multiple sclerosis. New England Journal of Medicine, 343, 938–952.
O’Connor, P. (2002). Key issues in the diagnosis and treatment of multiple sclerosis: An overview. Neurology, 59(6 Suppl. 3), S1–S33.
Lublin, F. D., & Reingold, S. C. (1996). Defining the clinical course of multiple sclerosis: results of an international survey. national multiple sclerosis society (USA) advisory committee on clinical trials of new agents in multiple sclerosis. Neurology, 46(4), 907–911.
Fisk, J. D., Pontefract, A., Ritvo, P. G., Archibald, C. J., & Murray, T. J. (1994). The impact of fatigue on patients with multiple sclerosis. Canadian Journal of Neurological Sciences, 21, 9–14.
Ford, H., Trigwell, P., & Johnson, M. (1998). The nature of fatigue in multiple sclerosis. Journal of Psychosomatic Research, 45, 33–38.
Archibald, C. J., McGrath, P. J., & Ritvo, P. G. (1994). Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients. Pain, 58, 89–93.
Ehde, D. M., Gibbons, L. E., Chwastiak, L., Bombardier, C. H., Sullivan, M. D., & Kraft, G. H. (2003). Chronic pain in a large community sample of persons with multiple sclerosis. Multiple Sclerosis, 9, 605–611.
Kalia, L. V., & O’Connor, P. W. (2005). Severity of chronic pain and its relationship to quality of life in multiple sclerosis. Multiple Sclerosis, 11, 322–327.
Svendsen, K. B., Jensen, T. S., Overvad, K., Hansen, H. J., KochHenriksen, N., & Bach, F. W. (2003). Pain in patients with multiple sclerosis. Archives of Neurology, 60, 1089–1094.
Svendsen, K. B., Jensen, T. S., Hansen, H. J., & Bach, F. W. (2005). Sensory function and quality of life in patients with multiple sclerosis and pain. Pain, 114, 473–478.
Bamer, A. M., Johnson, K. L., Amtmann, D., & Kraft, G. H. (2008). Prevalence of sleep problems in individuals with multiple sclerosis. Multiple Sclerosis, 14(8), 1127–1130.
Brass, S. D., Duquette, P., Proulx-Therrien, J., & Auerbach, S. (2010). Sleep disorders in patients with multiple sclerosis. Sleep Medicine Reviews, 14, 121–129.
Stanton, B. R., Barnes, F., & Silber, E. (2006). Sleep and fatigue in multiple sclerosis. Multiple Sclerosis, 12(4), 481–486.
Tachibana, N., Howard, R. S., Hirsch, N. P., Miller, D. H., Moseley, I. F., & Fish, D. (1994). Sleep problems in multiple sclerosis. European Neurology, 34(6), 320–323.
Grytten, N., & Maseide, P. (2006). ‘When I am together with them I feel more ill’. The stigma of multiple sclerosis experienced in social relationships. Chronic Illness, 2, 195–208.
Leussink, V. I., Husseini, L., Warnke, C., Broussalis, E., Hartung, H. P., & Kieseier, B. C. (2012). Symptomatic therapy in multiple sclerosis: the role of cannabinoids in treating spasticity. Therapeutic Advances in Neurological Disorders, 5(5), 255–266.
Rao, S. M., Leo, G. J., Bernardin, L., & Unverzagt, F. (1991). Cognitive dysfunction in multiple sclerosis. Frequency, patterns, and prediction. Neurology, 41(5), 685–691.
Teng, S.Y., Bartlett, S., Koski, L., Chamelian, L., Duquette, P., Grand’Maison, F., Lapierre, Y., Mayo, N.E. (2009). Self-perceived and tested cognition in multiple sclerosis: Differences across gender. Journal of Multiple Sclerosis Clinical and Laboratory research, 15 (2).
Feinstein, A. (2002). An examination of suicidal intent in patients with multiple sclerosis. Neurology, 59, 674–678.
Mohr, D. C. (2007). Stress and multiple sclerosis. Journal of Neurology, 254(2), II65–II68.
Newland, P. K., Fearing, A., Riley, M., & Neath, A. (2012). Symptom clusters in women with relapsing-remitting multiple sclerosis. Journal of Neuroscience Nursing, 44(2), 66–71.
D’Alisa, S., Miscio, G., Baudo, S., Simone, A., Tesio, L., & Mauro, A. (2006). Depression is the main determinant of quality of life in multiple sclerosis: A classification-regression (CART) study. Disability and Rehabilitation, 28(5), 307–314.
Lovera, J., Bagert, B., Smoot, K. H., Wild, K., Frank, R., Bogardus, K., et al. (2006). Correlations of perceived deficits questionnaire of multiple sclerosis quality of life inventory with beck depression inventory and neuropsychological tests. Journal of Rehabilitation Research and Development, 43(1), 73–82.
DeLuca, J. (2006). What we know about cognitive changes in multiple sclerosis. In N. L. LaRocca & R. Kalb (Eds.), Multiple sclerosis: Understanding the cognitive changes (pp. 17–39). New York: Demos Medical Publishing.
Krupp, L. B. (2004). Fatigue in multiple sclerosis: A guide to diagnosis and management. New York, NY: Demos Medical Publishing.
Motl, R. W., Weikert, M., Suh, Y., & Dlugonski, D. (2010). Symptom cluster and physical activity in relapsing-remitting multiple sclerosis. Research in Nursing & Health, 33, 398–412.
Kim, H. J., & Abraham, A. L. (2008). Statistical approaches to modeling symptom clusters in cancer patients. Cancer Nursing, 31, 162–220.
Dodd, M. J., Miaskowski, C., & Paul, S. M. (2001). Symptom clusters and their effect on the functional status of patients with cancer. Oncology Nursing Forum, 28, 465–470.
McSweeney, J. C., Cleves, M. A., Lefler, L., & Yang, S. (2010). Cluster analysis of women’s prodromal and acute myocardial infarction symptoms by race and other characteristics. Journal of Cardiovascular Nursing, 25(4), 311–322.
Miaskowski, C., Dodd, M., & Lee, K. (2004). Symptom clusters: The new frontier in symptom management research. Journal of National Cancer Institute Monographs, 32, 17–21.
Miaskowski, C. (2006). Symptom clusters: establishing the link between clinical practice and symptom management research. Supportive Care in Cancer, 14, 792–794.
Motl, R. W., & McAuley, E. (2009). Symptom cluster as a predictor of physical activity in multiple sclerosis: Preliminary evidence. Journal of Pain and Symptom Management, 38, 270–280.
Motl, R. W., & McAuley, E. (2009). Pathways between physical activity and quality of life in adults with multiple sclerosis. Health Psychology, 28, 682–689.
Lenz, E. R., Pugh, L. C., Milligan, R. A., Gift, A., & Suppe, F. (1997). The middle-range theory of unpleasant symptoms: An update. Advances in Nursing Science, 19(3), 14–27.
Lenz, E. R., & Pugh, L. C. (2003). The theory of unpleasant symptoms. In M. J. Smith & P. R. Liehr (Eds.), Middle range theory for nursing (pp. 69–90). New York: Springer.
Given, C. W., Given, B., Azzouz, F., Kozachik, S., & Stommel, M. (2001). Predictors of pain and fatigue in the year following diagnosis among elderly cancer persons. Journal of Pain and Symptom Management, 6, 456–466.
Given, B., Given, C. W., & McCorkle, R. (2002). Pain and fatigue management: results of a nursing randomized clinical trial. Oncology Nursing Forum, 29, 949–956.
Pearson, O. R., Busse, M. E., Van Deursen, R. W. M., & Wiles, C. M. (2004). Quantification of walking mobility in neurological disorders. Quarterly Journal of Medicine, 97(8), 463–475.
Motl, R. W., Snook, E. M., McAuley, E., & Gliottoni, R. (2006). Symptoms, self-efficacy, and physical activity among individuals with multiple sclerosis. Research in Nursing & Health, 29, 597–606.
Motl, R. W., Arnett, P. A., & Smith, M. M. (2008). Worsening of symptoms is associated with lower physical activity levels in individuals with multiple sclerosis. Multiple Sclerosis, 14, 140–142.
Motl, R. W., Snook, E. M., & Schapiro, R. T. (2008). Symptoms and physical activity behavior in individuals with multiple sclerosis. Research in Nursing & Health, 31, 466–475.
Snook, E. M., & Motl, R. W. (2008). Physical activity behaviors in individuals with multiple sclerosis: Roles of overall and specific symptoms, and self-efficacy. Journal of Pain and Symptom Management, 36, 46–53.
Parkin, D., Rice, N., Jacoby, A., & Doughty, J. (2004). Use of a visual analogue scale in a daily person diary: Modelling cross-sectional time-series data on health-related quality of life. Social Science and Medicine, 59(2), 351–360.
Devins, G. M., Edworthy, S. M., Paul, L. C., Mandin, H., Seland, T. P., Klein, G., et al. (1993). Restless sleep, illness intrusiveness, and depressive symptoms in three chronic illness conditions: rheumatoid arthritis, end-stage renal disease, and multiple sclerosis. Journal of Psychosomatic Research, 37(2), 163–170.
Devins, G. M., Edworthy, S. M., Seland, T. P., Klein, G. M., Paul, L. C., & Mandin, H. (1993). Differences in illness intrusiveness across rheumatoid arthritis, end-stage renal disease, and multiple sclerosis. The Journal of Nervous Mental Disease, 181(6), 377–381.
Devins, G. M. (1994). Illness intrusiveness and the psychosocial impact of lifestyle disruptions in chronic life-threatening disease. Advanced Renal Replacement Therapy, 1, 251–263.
Devins, G. M., Styra, R., O’Connor, P., Gray, T., Seland, T. P., & Klein, G. M. (1996). Psychosocial impact of illness intrusiveness moderated by age in multiple sclerosis. Psychology, Health & Medicine, 1, 179–191.
Devins, G. M., Dion, R., Pelletier, L. G., Shapiro, C. M., Abbey, S., Raiz, L. R., et al. (2001). Structure of lifestyle disruptions in chronic disease: a confirmatory factor analysis of the illness intrusiveness ratings scale. Medical Care, 39(10), 1097–1104.
Mullins, L. L., Cote, M. P., Fuemmeler, B. F., Jean, V. M., Beatty, W. W., & Paul, R. H. (2001). Illness intrusiveness, uncertainty, and distress in individuals with multiple sclerosis. Rehabilitation Psychology, 46(2), 139–153.
Culp, D. (2010). Illness intrusiveness and sexual satisfaction among women with multiple sclerosis. Master of Arts Thesis in Psychology, Ryerson University.
Turpin, K. V., Carroll, L. J., Cassidy, J. D., & Hader, W. J. (2007). Deterioration in the health-related quality of life of persons with multiple sclerosis: the possible warning signs. Multiple Sclerosis, 13(8), 1038–1045.
Amato, M., Battaglia, M., & Caputo, D. (2002). The costs of multiple sclerosis: A cross-sectional, multicenter cost-of-illness study in Italy. Journal of Neurology, 249, 152–163.
Benedict, R., Wahlig, E., Bakshi, R., Fishman, I., Munschauer, F., & Weinstock-Guttman, B. (2005). Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. Journal of the Neurological Sciences, 231(1, 2), 29–34.
Benito-Leon, J., Morales, J. M., & Rivera-Navarro, J. (2002). Health-related quality of life and its relationship to cognitive and emotional functioning in multiple sclerosis persons. European Journal of Neurology, 9, 497–502.
Egner, A., Phillips, V. L., Vora, R., & Wiggers, E. (2003). Depression, fatigue, and health-related quality of life among people with advanced multiple sclerosis: results from an exploratory telerehabilitation study. Neurorehabilitation, 18, 125–133.
Janssens, A. C., Doorn, P. A., de Boer, J. B., Kalkers, N. F., Meche, F. G., & Passchier, J. (2003). Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Multiple Sclerosis, 9, 397–403.
Miller, D. M., Rudick, R. A., Baier, M., Cutter, G., Doughtery, D. S., & Weinstock-Guttman, B. (2003). Factors that predict health-related quality of life in persons with relapsing–remitting multiple sclerosis. Multiple Sclerosis, 9, 1–5.
O’Connor, P., Lee, L., Ng, P. T., Narayana, P., & Wolinsky, J. S. (2001). Determinants of overall quality of life in secondary progressive MS: A longitudinal study. Neurology, 57, 889–891.
Esper, P., & Heidrich, D. (2005). Symptom clusters in advanced illness. Seminars in Oncology Nursing, 21, 20–28.
Wilmoth, M. C., Coleman, E. A., Smith, S. C., & Davis, C. (2004). Fatigue, weight gain, and altered sexuality in persons with breast cancer: Exploration of a symptom cluster. Oncology Nursing Forum, 31, 1069–1075.
Armstrong, T. S., Cohen, M. Z., Eriksen, L. R., & Hickey, J. V. (2004). Symptom clusters in oncology persons and implications for symptom research in people with primary brain tumors. Journal of Nursing Scholarship, 36, 197–206.
Gift, A. G., Stommel, M., Jablonski, A., & Given, W. (2003). A cluster of symptoms over time in patients with lung cancer. Nursing Research, 52, 393–400.
Gift, A. G., Jablonski, A., Stommel, M., & Given, C. W. (2004). Symptom clusters in elderly patients with lung cancer. Oncology Nursing Forum, 31, 202–212.
Drew, M., Tippett, L. J., Starkey, N. J., & Isler, R. B. (2008). Executive dysfunction and cognitive impairment in a large community-based sample with Multiple Sclerosis from New Zealand: A descriptive study. Archives of Clinical Neuropsychology, 23, 1–19.
Motl, R. W., Suh, Y., & Weikert, M. (2010). Symptom cluster and quality of life in multiple sclerosis. Journal of Pain and Symptom Management, 39(6), 1025–1032.
Nocentini, U., Pasqualetti, P., Bonavita, S., Buccafusca, M., De Caro, M. F., Farina, D., et al. (2006). Cognitive dysfunction in patients with relapsing-remitting multiple sclerosis. Multiple Sclerosis, 12, 77.
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology, 33(11), 1444–1452.
Hays, R. D., & Morales, L. S. (2001). The RAND-36 measure of health- related quality of life. Annals of Medicine, 33, 350–357.
Brunet, D. G., Hopman, W. M., Singer, M. A., Edgar, C. M., & MacKenzie, T. A. (1996). Measurement of health-related quality of life in multiple sclerosis patients. The Canadian Journal of Neurological Sciences, 23(2), 99–103.
Freeman, J. A., Hobart, J. C., Langdon, D. W., & Thompson, A. J. (2000). Clinical appropriateness: A key factor in outcome measure selection: The 36 item short form health survey in multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry, 68, 150–156.
McHorney, C. A., Ware, J. E., & Raczek, A. E. (1993). The MOS 36-item short-form health survey (SF-36): II. A psychometric and clinical test of validity in measuring physical and mental health constructs. Medical Care, 31, 247–263.
McHorney, C. A., Ware, J. E., & Sherbourne, C. D. (1994). The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32, 40–66.
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370.
Herrmann, C. (1997). International experiences with the hospital anxiety and depression scale-a review of validation data and clinical results. Journal of Psychosomatic Research, 42(1), 17–41.
Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale; an updated review. Journal of Psychosomatic Research, 52(2), 69–77.
da Silva, A. M., Vilhena, E., Lopes, A., & Santos, E. (2011). Depression and anxiety in a Portuguese MS population: Associations with physical disability and severity of disease. Journal of the Neurological Sciences, 306(15), 66–70.
Honarmand, K., & Feinstein, A. (2009). Validation of the hospital anxiety and depression scale for use with multiple sclerosis patients. Multiple Sclerosis, 15(12), 1518–1524.
Ilfeld, F. W, Jr. (1976). Further validation of a psychiatric symptom index in a normal population. Psychological Reports, 39, 1215–1228.
Sullivan, M. J. L., Edgley, K., & Mikail, S. (1993). Psychological correlates of health care utilization in chronic illness. Canadian Journal of Rehabilitation, 6, 13–21.
Shevil, E., & Finlayson, M. (2006). Perceptions of persons with multiple sclerosis on cognitive changes and their impact on daily life. Disability and Rehabilitation, 28(12), 779–788.
Marrie, R. A., Miller, D. M., Chelune, G. J., & Cohen, J. A. (2003). Validity and reliability of the MSQLI in cognitively impaired patients with multiple sclerosis. Multiple Sclerosis, 9(6), 621–626.
Bohannon, R., & Smith, M. (1987). Interrater reliability of a modified Ashworth scale of muscle spasticity. Physical Therapy, 67(2), 206–207.
Ashworth, B. (1964). Preliminary trial of carisoprodal in multiple sclerosis. The Practitioner, 192, 540–542.
Leslie, G. C., Muir, C., Part, N. J., & Roberts, R. C. (1992). A comparison of the assessment of spasticity by the Wartenberg pendulum test and the Ashworth grading scale in patients with multiple sclerosis. Clinical Rehabilitation, 6, 41–48.
Nuyens, G., De Weerdt, W., Ketelaer, P., Feys, H., De Wolf, L., Hantson, L., Nieuboer, A., Spaepen, A., & Carton, H. (1994). Inter-rater reliability of the Ashworth scale in multiple Sclerosis. Clinical Rehabilitation, 8, 286–292.
Pandyan, A. D., Price, C. I. M., & Curless, R. H. (1999). A review of the properties and limitations of the Ashworth & modified Ashworth Scales. Clinical Rehabilitation, 13(5), 373–383.
Pandyan, A. D., Price, C. I. M., & Rodgers, H. (2001). Biomechanical examination of a commonly used measure of spasticity. Clinical Biomechanics, 16, 859–865.
Tesio, L., Perucca, L., Franchignoni, F. P., & Battaglia, M. A. (1997). A short measure of balance in multiple sclerosis: validation through Rasch analysis. Functional Neurology, 12(5), 255–265.
Butland, R. J. A., Pang, J., Gross, E. R., Woodcock, A. A., & Geddes, D. M. (1982). Two-, six- and 12-minute walking tests in respiratory disease. British Medical Journal, 284, 1607–1608.
Savci, S., InalInce, D., & Arikan, H. (2005). Six-minute walk distance as a measure of functional exercise capacity in multiple sclerosis. Disability and Rehabilitation, 27(22), 1365–1371.
Goldman, M., Marrie, R. A., & Cohen, J. A. (2007). Evaluation of six minutes walk test in MS and healthy population. Multiple Sclerosis, 14, 383–390.
Morales, F. J., Martinez, A., Mendez, M., Agarrado, A., Ortega, F., & Fernandez-Guerra, J. (1999). A shuttle walk test for assessment of functional capacity in chronic heart failure. Americal Heart Journal, 138(2), 291–298.
Paltamaa, J., West, H., Sarasoja, T., Wikstrom, J., & Malkia, E. (2005). Reliability of physical functioning measures in ambulatory subjects with MS. Physiotherapy Research International, 10(2), 93–109.
EuroQol Group. (1990). EuroQol-a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy, 16(3), 199–208.
Nortvedt, M., Riise, T., & Myhr, K. (1999). Quality of life in multiple sclerosis: measuring the disease effects more. Neurology, 53, 1098–1103.
Devins, G. M., Binik, Y. M., Hutchinson, T. A., Hollomby, D. J., Barré, P. E., & Guttmann, R. D. (1983). The emotional impact of end-stage renal disease: Importance of persons’ perceptions of intrusiveness and control. The International Journal of Psychiatry in Medicine, 13(4), 1983–1984.
Devins, G. M. (2010). Using the illness intrusiveness ratings scale to understand health-related quality of life in chronic disease. Journal of Psychosomatic Research, 68(6), 591–602.
Ruta, D. A., Garratt, A. M., Leng, M., Russell, I. T., & MacDonald, L. M. (1994). A new approach to the measurement of quality of life. the person-generated index. Medical Care, 32, 1109–1126.
Ruta, D. A., Garratt, A. M., & Russell, I. T. (1999). Person centred assessment of quality of life for persons with four common conditions. Qualitative Health Care, 8, 22–29.
Lintern, T. C., Beaumont, J. G., Kenealy, P. M., & Murrell, R. C. (2001). Quality of life (HRQL) in severely disabled multiple sclerosis persons: Comparison of three HRQL measures using multidimensional scaling. Quality of Life Research, 10, 371–378.
Garratt, A. M., & Ruta, D. A. (1999). The person generated index. In C. R. B. Joyce, C. A. O’Boyle, & H. McGee (Eds.), Individual quality of life: Approaches to conceptualization and assessment (pp. 105–118). Amsterdam: Harwood Academic Publishers.
Anderberg, M. R. (1973). Cluster Analysis for Applications. New York: Academic Press Inc.
Everitt, B. S., Landau, S., & Leese, M. (2001). Cluster analysis. New York: Oxford University Press.
Hopman, W. M., Towheed, T., Anastassiades, T., Tenenhouse, A., Poliquin, S., Berger, C., et al. (2000). Canadian normative data for the SF-36 health survey. Canadian Medical Association Journal, 163(3), 265–271.
Enright, P. (2003). The six-minute walk test. Respiratory care, 48(8), 783–785.
Mayo, N., Goldberg, M.S., Kind, P. (1997). Calibrating the EQ-5D for a Canadian Population. In: Proceedings from EuroQol Plenary Meeting, Center for Health Policy and Law, Erasmus University, Rotterdam, The Netherlands. pp. 25–40.
Redelmeier, D., Bayoumi, A., Goldstein, R., & Guyatt, G. (1997). Interpreting small differences in functional status: the six minute walk test in chronic lung disease persons. American Journal of Respiratory and Critical Care Medicine, 155, 1278–1282.
Fox, S. W., & Lyon, D. E. (2006). Symptom clusters and quality of life in survivors of lung cancer. Oncology Nursing Forum, 33, 931–936.
Kelley, K. W., Bluthé, R. M., Dantzer, R., Zhou, J. H., Shen, W. H., Johnson, R. W., et al. (2003). Cytokine-induced sickness behavior. Brain, Behavior, and Immunity, 17(Suppl 1), S112–S118.
Mayo, N. (2008). Setting the agenda for multiple sclerosis rehabilitation research. Multiple Sclerosis, 14(9), 1154–1156.
Kirkova, J. K., Aktas, A., Walsh, D., & Davis, M. P. (2011). Cancer symptom clusters: Clinical and research methodology. Journal of Palliative Medicine, 14(10), 1149–1166.
Acknowledgments
This work was supported by a scholarship from the Canadian Institutes of Health Research. Authors acknowledge the contribution of Élaine Roger, who recruited patients from Centre Hospitalier de l’Université de Montréal.
Ethical standard
Study protocol and procedures were approved by the ethics committee of each participating hospital; informed consent was obtained and signed by all subjects on the day of testing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shahrbanian, S., Duquette, P., Kuspinar, A. et al. Contribution of symptom clusters to multiple sclerosis consequences. Qual Life Res 24, 617–629 (2015). https://doi.org/10.1007/s11136-014-0804-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0804-7