Abstract
Purpose
Obesity is associated with impaired quality of life (QoL), but less is known about physical activity. We investigated how decreases in body mass index (BMI) and increases in activity affect obesity-specific QoL and potential gender differences in associations.
Methods
In a large worksite randomized trial of a multilevel intervention on diet and physical activity behaviors, we conducted a cohort analysis at two years of follow-up. Self-reported activity and Obesity and Weight Loss Quality of Life (OWLQOL) were analyzed for individual-level associations using linear mixed models accounting for random worksite effects.
Results
Gender modified the BMI–OWLQOL relationship, so analyses were conducted for males and females separately. Adjusting for demographic confounders, baseline OWLQOL, and several worksite-level variables including intervention arm, a 1.9 unit decrease in BMI (the interquartile range) was associated with an OWLQOL increase of 1.7 (95 % CI: 1.2, 2.2) in males and 3.6 (95 % CI: 3.2, 4.0) in females. Similarly, a 23 unit increase in physical activity score was associated with an OWLQOL increase of 0.9 (95 % CI: 0.5, 1.4) in males and 1.6 (95 % CI: 1.0, 2.3) in females. Physical activity associations were attenuated when adjusting for change in BMI, but remained significant for women (mean BMI 27.8 kg/m2).
Conclusions
This is the first study to demonstrate that increasing physical activity may improve obesity-specific QoL to a greater extent in women, particularly among overweight women, independent of BMI. Results may inform the design of interventions tailored to women targeting well-being through messages of increasing physical activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity among U.S. adults has increased dramatically over the past decade [1], which is particularly concerning given that obesity is associated with numerous detrimental health conditions such as hypertension, type 2 diabetes, heart disease, stroke, and certain types of cancer [2]. While there has been an increased focus on additional outcomes, such as well-being and psychosocial functioning, there is a relative paucity of research regarding health-related quality of life (HRQOL), and specifically, weight-related quality of life. These health outcomes are of increasing interest in relation to weight and lifestyle as the proportion of the U.S. population who are overweight or obese continues to grow.
Several studies have found that obesity is associated with a lower perceived QoL [3–7], and a higher body mass index (BMI, kg/m2) has been associated with lower scores in physical, social, and emotional domains of HRQOL [8]. Furthermore, individuals with higher BMIs tend to report lower scores on weight-specific measures [5, 9] such as the Impact of Weight on Quality of Life-Lite instrument [10]. Weight loss has also been strongly linked to improved weight-related HRQOL [11].
Recently, research has focused on changing behaviors to modify QoL, and various studies have suggested that physical activity may be one primary target [12–14]. At least one systematic review has supported a strong association between physical activity and HRQOL [15]. Although cross-sectional research has previously shown that physical activity and BMI are associated with obesity-specific quality of life [9], it remains to be seen if changes in physical activity and weight are associated with changes in obesity-specific quality of life.
The literature also suggests that gender differences may exist for weight and QoL associations. Women tend to report lower weight-related QoL [16–18], and the negative effects of obesity on HRQOL are more pronounced for women [11, 19]. Similarly, the benefits of behavioral change on HRQOL may be more pronounced for women: at least one study has shown that the association between greater levels of physical activity and higher HRQOL exists only for women [20]. Nonetheless, no longitudinal studies have examined any gender differences in the associations of BMI and physical activity with weight-related QoL.
Given the aforementioned gaps in the literature, we sought to examine BMI and physical activity over 2 years as predictors of change in obesity-specific QoL and potential gender differences in these associations within the context of a worksite-based intervention study, the promoting activity and changes in eating (PACE) study. Specifically, we hypothesized that decreases in BMI and increases in physical activity were associated with increases in obesity-specific quality of life, a measure of how various domains of quality of life are affected by one’s weight. We further hypothesized that these associations would be stronger for women compared to men. A conceptual model for these hypotheses is depicted in Fig. 1. To date, no study has examined potential gender differences in the associations of either BMI or physical activity with obesity-specific QoL using longitudinal data.
Methods
Recruitment
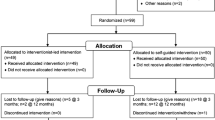
Methods for the PACE study have previously been described in detail [21]. In brief, worksites were recruited from the Seattle metropolitan area along the I-5 corridor between Everett and Tacoma Washington. Worksites were identified using U.S. Standard Industrial Classification (SIC) 2-digit codes (U.S. Census Bureau, 2008) [22], which included manufacturing (SIC 20–39), transportation or utilities (SIC 40–49), personal services (SIC 70–79), household and miscellaneous services (SIC 88–89), and non-classifiable establishments (SIC 99). Eligibility criteria included worksites with the following: a large portion of sedentary workers (>25 %); a low turnover rate (<30 %) over the past 2 years; a low proportion of non-English speaking employees (<30 %); a workforce between 40 and 350 employees; no more than two locations participating; at least a 3 years history of being in business; and willingness to be randomized to either the intervention or the comparison (delayed intervention) arm of the study. Worksites with a wellness program that had an on-site, active physical activity or nutritional component were excluded.
Worksites were recruited on a rolling basis, constituting four waves. Each wave contained between six and ten worksites (three to five pairs), randomized to either intervention or control arms and paired according to similarity in baseline response rates. Thirty-four worksites were randomized. Here, we report on data from 33 worksites (one worksite dropped after randomization) at baseline and follow-up. Data collection took place from November 2005 to September 2009. The study was conducted in accordance with the Declaration of Helsinki, and all procedures involving human subjects were approved by the Institutional Review Boards at the University of Washington and the Fred Hutchinson Cancer Research Center. Written informed consent was obtained from all participants.
Baseline measurements
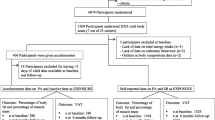
Assessment of BMI
Baseline and follow-up BMIs were calculated using self-reported height and weight. Measured height and weight were also obtained from a majority of employees at baseline and follow-up. The correlation between self-reported and measured BMI was very strong (r = 0.98, p < 0.0001); thus, self-reported BMI was used in subsequent data analyses to maximize statistical power. Sensitivity analyses using measured BMI were also conducted. The log of BMI was used in all analyses and then back transformed for interpretation. BMI was also grouped according to the standard categories “underweight” (<18.5 kg/m2), “normal weight” (18.5–24.9), “overweight” (25–29.9), and “obese” (30+) using cutpoints established by the U.S. Centers for Disease Control and Prevention [23] in order to evaluate whether BMI group modified the effect of weight and behavior change on obesity-related quality of life.
Assessment of physical activity
Physical activity was defined as free-time physical activity of at least 10-min duration assessed using a modified Godin Leisure-Time Exercise Questionnaire [24], which asked about the frequency during a typical 7-day period of strenuous, moderate, and mild exercise (assessed separately). Reported frequencies were then weighted using approximate metabolic equivalents (METs) of 9, 5, and 3 respectively, and a total weighted score was then calculated by summing weighted frequencies across all three categories [24, 25]. A higher score is indicative of greater levels of activity. This questionnaire is reliable (test–retest correlation coefficient ranging from 0.48 for light activity to 0.94 for strenuous activity) and valid in relation to maximal oxygen consumption [25–28]. Godin values were examined for plausibility and evaluated statistically using histograms and boxplots. After conducting sensitivity analyses for various potential cutpoints, the following cutpoints were established: 30 times per week for mild exercise, 20 times per week for moderate exercise, and 15 times per week for strenuous exercise. Values were excluded if they were equal to or exceeded these cutpoints.
Assessment of obesity-specific quality of life
Obesity-specific quality of life was measured using the Obesity and Weight Loss Quality of Life (OWLQOL) Questionnaire [29, 30]. The OWLQOL is a 17-item self-administered questionnaire that was developed to address shortcomings of preexisting instruments that focus on functional status or behaviors associated with obesity. In addition, previously existing measures were not developed cross-culturally (a strength of this instrument) or were developed primarily for application in severely obese populations [18], limiting their validity and reliability in multi-cultural populations and in normal weight and overweight populations. The theoretical foundation for the OWLQOL instrument is Maslow’s theory of human needs [31], and items tap unobservable needs such as freedom from stigma and attainment of culturally appropriate goals. For example, respondents are asked the degree to which they agree with statements such as “I feel frustrated that I have less energy because of my weight” and “My weight prevents me from doing what I want to do.” Response category options (n = 7) range from 0 (“not at all”) to 6 (“a very great deal”), and scores are transformed to a scale from 0 to 100, where a higher score is indicative of a higher obesity-specific QoL. The OWLQOL measure has been tested extensively and reliability and validity is strong [18], there is high internal consistency for the included items (Guttman–Cronbach’s α = 0.96), and factor analyses support a single factor [18]. In addition, the OWLQOL was able to detect differences between genders (p < 0.001), presence of disability days (p < 0.05), BMI levels (p < 0.05), and levels of symptom bothersomeness (p < 0.001). For ≥2.5 % weight loss at 12 weeks, effect sizes were 0.77 for the OWLQOL and −0.54 for the Weight-related Symptoms Measure (WRSM). For ≥10 % weight change at ≥50 weeks, effect sizes were 1.63 and −0.73, respectively [18].
Statistical methods
Analyses were restricted to those participants with complete data for the outcome of interest, a change in OWLQOL score between baseline and follow-up. We conducted descriptive analyses on baseline demographic characteristics, and means for age and proportions of race, education, income, and smoking categories were computed within each worksite and then averaged across worksites. We also used this average of means approach to examine the mean baseline and follow-up values for OWLQOL scores, BMI, and Godin physical activity scores. This approach allows for equal representation of worksites, regardless of the number of employees at each worksite. The difference in these values was tested for statistical significance using a paired sample t test.
Estimated effects relating the differences in BMI and physical activity to the difference in OWLQOL scores were established in longitudinal analyses using linear mixed models and were calculated as the estimated regression coefficient times the interquartile range (IQR). The IQR is commonly used as a meaningful difference in a predictor (particularly when a 1-unit difference is minimal), and it has been used in multiple papers examining physical activity [32, 33]. Both gender and BMI group (i.e., normal weight, overweight, or obese) were examined as potential effect modifiers in the relationship between the predictors and our outcome, a decision based on prior research. Effect modification was tested by creating multiplicative interaction terms and testing for significance using a likelihood ratio test. For example, for exploring effect modification by gender in the association between physical activity and OWLQOL score, a cross-product term between the difference in physical activity score (from baseline to follow-up) and gender was tested. A similar approach was taken for BMI, using established categories of BMI (<25, 25–29.9, 30+). When effect modification was found, analyses were conducted separately for men and women, and again separately within BMI group. Analyses were presented as 1) unadjusted, 2) age adjusted (continuous), and 3) adjusted for covariates including race (non-Hispanic White; Hispanic; Asian; other), income (<$50,0000; $50,000–$74,999; $75,000– <$100,000; $100,000+), education (high school graduate, GED, or less; some technical college, technical college graduate, or some college; college graduate; postgraduate or professional degree), and smoking (never smoked; former smoker; current smoker). When evaluating physical activity as a predictor, an additional set of analyses further adjusted for change in BMI. Race was collapsed into four categories (non-Hispanic White, Hispanic, Asian, and other) when included as a covariate. All regression models (including the unadjusted version) controlled for baseline OWLQOL score, in addition to the following worksite-level characteristics: number of employees, percent of employees who are considered “white collar,” intervention arm, and the presence or absence of a health promotion or wellness program in the worksite at baseline.
The longitudinal regression analyses were based on 1,139 individuals from all four randomization waves who had complete data on OWLQOL scores, although the sample size varied based on missing data for predictors and covariates. All statistical tests were two-sided, and results were considered significant if the p value was less than 0.05. Statistical analyses were conducted in 2010 using Stata/IC (version 11.0; StataCorp LP, College Station, TX).
Results
The average worksite had 140 employees, and the average proportion of white-collar employees was 19.6 %, similar to the companies in the recruiting pool that were not randomized. Randomized worksites reflected the SIC code distribution of the underlying recruiting pool, with randomized worksites having a slightly higher proportion of transportation and communication companies.
The original dataset of employees in randomized companies (n = 1,386) was restricted to individuals with non-missing values for OWLQOL (n = 1,139, 82.2 % of original dataset). Those with missing OWLQOL scores were slightly less likely to have gone to college and more likely to have a household income of $50,000 or less. Mean values of predictors were similar between those with and without complete information on OWLQOL.
Among those with complete information on OWLQOL (Table 1), the majority of employees were non-Hispanic White (76.3 %, n = 869), reflecting the general demographics in the Pacific Northwest. Approximately 58.4 % (n = 665) of employees were either overweight (32.7 %) or obese (25.7 %) at baseline. Mean age and the distribution of race, education, and income were similar between males and females. Women were slightly more likely to have never smoked. Mean values for OWLQOL, BMI, and physical activity are presented in Table 2. Of these measures, only the change in physical activity (p = 0.0001) was significant and only among men. The IQRs for BMI and Godin score were 1.9 and 23.0, respectively. The IQR for OWLQOL was 27.5, with the middle 50 % of scores falling between 69.6 and 97.1. The averages of means approach employed in the calculation of estimates resulted in similar values to the averages in the overall sample.
Gender modified the effects of BMI and physical activity on obesity-specific QoL (interaction p = 0.001 for BMI as predictor, interaction p < 0.001 for physical activity as a predictor). Adjusting for age, race, income, education, smoking, and intervention arm, a 1.9 unit decrease in BMI (i.e., a change in BMI as large as the IQR of its distribution) was associated with a 1.7 unit increase in mean OWLQOL (95 % CI: 1.2, 2.2) in males and a 3.6 unit increase (95 % CI: 3.2, 4.0) in females (Table 3). Similarly, a 23 unit increase in Godin score was associated with a 0.9 unit increase in mean OWLQOL (95 % CI: 0.5, 1.4) in males and a 1.6 unit increase (95 % CI: 1.0, 2.3) in females. Associations between physical activity and OWLQOL were attenuated when controlling for change in BMI in both men and women, but notably remained significant for women, with a 23 unit increase in Godin score being associated with a 1.5 unit increase (95 % CI: 0.9, 2.2) in mean OWLQOL.
BMI group was also an effect modifier (interaction p = 0.026 for BMI as predictor, interaction p = 0.009 for physical activity as a predictor). Adjusting for age, gender, race, income, education, smoking, and intervention arm, a 1.9 unit decrease in BMI was associated with a 4.4 unit increase in mean OWLQOL (95 % CI: −5.3, −3.6) among normal weight individuals, a 3.8 unit increase (95 % CI: −4.3, −3.4) among overweight individuals, and a 2.8 unit increase (95 % CI: −3.4, −2.2) among the obese (Table 4). When adjusting for the same covariates, change in physical activity was associated with a change in OWLQOL in overweight individuals; a 23 unit increase in Godin score related to a 1.4 unit increase (95 % CI: 0.8, 2.0) in mean OWLQOL. After adjusting additionally for change in BMI, a 23 unit increase in Godin score was associated with a 1.2 unit increase (95 % CI: 0.66, 1.74) and a 1.3 unit increase (95 % CI: 0.8, 1.8) in mean OWLQOL for normal weight and overweight individuals, respectively. Sensitivity analyses revealed that all results were similar when using measured BMI and self-reported BMI.
Discussion
This was the first study to use longitudinal data to examine potential gender differences for associations between changes in BMI, physical activity, and obesity-specific QoL. Our findings confirm our hypothesis that decreases in BMI and increases in physical activity are associated with an increase in self-reported obesity-specific HRQOL. Furthermore, we observed that these effects were stronger in women than men, a novel finding regarding weight-related quality of life. In our study, women were more likely to report lower obesity-specific quality of life, consistent with prior studies suggesting that women tend to report lower general HRQOL [10, 16–18]. Our results also complement previous findings showing that the impact of obesity on HRQOL is more severe for women than men [16, 17].
Our data also suggest that an increase in free-time physical activity is associated with an increase in obesity-specific HRQOL. Previous literature has found an effect of physical activity on HRQOL for both men and women [13, 14] and for women alone [20]. Our finding of a variable effect by gender for obesity-specific quality of life using longitudinal data is novel and may be useful in evaluating the importance of physical activity on HRQOL, as it supports a larger impact for women.
When examining the data with BMI group as an effect modifier, it is interesting to note that the effect of a change in BMI on a change in OWLQOL was strongest for employees with normal weight. This may be due to the fact that when comparing a normal weight individual and an obese individual who both lose a specific number of kg, the normal weight individual experiences losing a greater proportion of his or her weight. If proportion of weight change is important, a larger change in BMI might be required to affect quality of life among obese individuals.
Our study has several limitations that should be noted. All variables used in the analyses were assessed using self-report survey data and are thus subjected to report bias. However, we also conducted analyses within the intensive assessment sub-sample with measured BMI and found similar results. In addition, we found a very high correlation between self-reported and directly measured BMI, suggesting that perhaps BMI was less prone to reporting bias than the behavioral predictors. We must also note that approximately 18 % of respondents were missing data on OWLQOL at baseline, follow-up, or both. These respondents were slightly less likely to have gone to college and more likely to have a household income of $50,000 or less, so our results may not fully reflect the association between BMI or physical activity and obesity-specific quality of life for those with low SES. As is the case with any observational study, unmeasured confounding may exist, making it difficult to draw conclusions concerning causality. Thus, it is unclear whether changes in BMI and physical activity influence changes in obesity-specific HRQOL or whether this relationship is reversed. For instance, it is possible that obesity-specific quality of life is a predictor of obesity-specific behaviors.
This study also has several noteworthy strengths. Whereas the current body of literature has focused on general HRQOL; our study examined obesity-specific HRQOL. The large sample size also separates ours from nearly all other studies in this area. Additionally, using a linear mixed model, we were able to control for worksite-level effects in order to examine individual-level associations. A clinically meaningful difference in OWLQOL has not yet been established, but an approximately 2-point increase in OWLQOL is about 10 % of the range occupied by the middle 50 % of OWLQOL scores, and so could reasonably be considered an important difference.
Conclusion
Our results suggest that decreases in BMI and increases in physical activity are associated with improved obesity-specific quality of life, with the impact being more pronounced in women. These results support the concept that changes in weight and physical activity may have important implications for overall well-being and highlight potential approaches to improving obesity-specific quality of life. The observation of stronger effects of obesity and physical activity on obesity-specific HRQOL in women compared to men is truly informative and may prove useful in designing specific interventions to address the mental health and overall well-being, especially of overweight women and men. For example, our work suggests that targeting improving levels of physical activity may be a more beneficial tactic for improving obesity-specific quality of life among women, whereas for men, the evidence is less strong and alternative approaches should be explored. For women, approaches may include tailored messaging and reducing barriers to physical activity, for example. It will be important for future research and evidence-based practice to explore potential mechanisms for our observations, determine the best strategies for improving obesity-specific quality of life through increased physical activity and weight loss, and test feasibility within various populations.
References
U.S. Centers for Disease Control and Prevention. Overweight and Obesity: FastStats (2010). http://www.cdc.gov/nchs/fastats/overwt.htm. Accessed August 22 2011.
U.S. Centers for Disease Control and Prevention. Overweight and Obesity: Health Consequences (2011). http://www.cdc.gov/obesity/causes/health.html. Accessed August 22 2011.
Fontaine, K. R., & Barofsky, I. (2001). Obesity and health-related quality of life. Obesity Reviews, 2(3), 173–182.
Groessl, E. J., Kaplan, R. M., Ganiats, T. G., & Barrett-Conner, E. (2002). The relationship between past body mass index and future quality of life. Quality of Life Research, 11(7), 633.
Kolotkin, R. L., Crosby, R. D., & Williams, G. R. (2002). Health-related quality of life varies among obese subgroups. Obesity Research, 10(8), 748–756.
Jones, G. L., & Sutton, A. (2008). Quality of life in obese postmenopausal women. Menopause International, 14(1), 26–32.
Cameron, A. J., Magliano, D. J., Dunstan, D. W., Zimmet, P. Z., Hesketh, K., Peeters, A., et al. (2011). A bi-directional relationship between obesity and health-related quality of life: evidence from the longitudinal AusDiab study. International Journal of Obesity, doi: 10.1038/ijo.2011.103.
Karlsson, J., Taft, C., Ryden, A., Sjostrom, L., & Sullivan, M. (2007). Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: The SOS intervention study. International Journal of Obesity, 31(8), 1248–1261.
Cash, S. W., Beresford, S. A., Henderson, J. A., McTiernan, A., Xiao, L., Wang, C. Y., et al. (2012). Dietary and physical activity behaviours related to obesity-specific quality of life and work productivity: Baseline results from a worksite trial. British Journal of Nutrition, 108(6), 1134–1142. doi:10.1017/S0007114511006258.
Kolotkin, R. L., Crosby, R. D., Kosloski, K. D., & Williams, G. R. (2001). Development of a brief measure to assess quality of life in obesity. Obesity Research, 9(2), 102–111. doi:10.1038/oby.2001.13.
Kolotkin, R. L., Crosby, R. D., Williams, G. R., Hartley, G. G., & Nicol, S. (2001). The relationship between health-related quality of life and weight loss. Obesity Research, 9(9), 564–571. doi:10.1038/oby.2001.73.
Plaisted, C. S., Lin, P. H., Ard, J. D., McClure, M. L., & Svetkey, L. P. (1999). The effects of dietary patterns on quality of life: A substudy of the Dietary Approaches to Stop Hypertension trial. Journal of the American Dietetic Association, 99(8 Suppl), S84–S89.
Brown, D. W., Balluz, L. S., Heath, G. W., Moriarty, D. G., Ford, E. S., & Giles, W. H. (2001). (2003). Associations between recommended levels of physical activity and health-related quality of life. Findings from the, Behavioral Risk Factor Surveillance System (BRFSS) survey. Preventive Medicine, 37(5), 520–528.
Brown, D. W., Brown, D. R., Heath, G. W., Balluz, L., Giles, W. H., Ford, E. S., et al. (2004). Associations between physical activity dose and health-related quality of life. Medicine and Science in Sports and Exercise, 36(5), 890–896.
Bize, R., Johnson, J. A., & Plotnikoff, R. C. (2007). Physical activity level and health-related quality of life in the general adult population: a systematic review. Preventive Medicine, 45(6), 401–415. doi:10.1016/j.ypmed.2007.07.017.
Kolotkin, R. L., Head, S., Hamilton, M., & Tse, C. K. (1995). Assessing impact of weight on quality of life. Obesity Research, 3(1), 49–56.
Katz, D. A., McHorney, C. A., & Atkinson, R. L. (2000). Impact of obesity on health-related quality of life in patients with chronic illness. Journal of General Internal Medicine, 15(11), 789–796.
Patrick, D. L., Bushnell, D. M., & Rothman, M. (2004). Performance of two self-report measures for evaluating obesity and weight loss. Obesity Research, 12(1), 48–57. doi:10.1038/oby.2004.8.
Larsson, U., Karlsson, J., & Sullivan, M. (2002). Impact of overweight and obesity on health-related quality of life—a Swedish population study. International Journal of Obesity and Related Metabolic Disorders, 26(3), 417–424. doi:10.1038/sj.ijo.0801919.
Brown, W. J., Mishra, G., Lee, C., & Bauman, A. (2000). Leisure time physical activity in Australian women: Relationship with well being and symptoms. Research Quarterly for Exercise and Sport, 71(3), 206–216.
Beresford, S. A., Locke, E., Bishop, S., West, B., McGregor, B. A., Bruemmer, B., et al. (2007). Worksite study promoting activity and changes in eating (PACE): design and baseline results. Obesity, 15(Suppl 1), 4S–15S.
U.S. Census Bureau. 1987 SIC Matched to 1997 NAICS Major Groups (2-Digit). http://www.census.gov/epcd/naics/nsic2ndx.htm#S3. Accessed July 4 2008.
U.S. Centers for Disease Control and Prevention. How is BMI calculated and interpreted? (2008). http://www.cdc.gov/nccdphp/dnpa/healthyweight/assessing/bmi/adult_BMI/about_adult_BMI.htm#Interpreted. Accessed July 28 2008.
Godin, G., & Shephard, R. J. (1997). Godin leisure-time exercise questionnaire. Medicine and Science in Sports and Exercise, June (Supplement), S36–S38.
Godin, G., & Shephard, R. J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Sciences, 10(3), 141–146.
Jacobs, D. R., Jr, Ainsworth, B. E., Hartman, T. J., & Leon, A. S. (1993). A simultaneous evaluation of 10 commonly used physical activity questionnaires. Medicine and Science in Sports and Exercise, 25(1), 81–91.
Sallis, J. F., Buono, M. J., Roby, J. J., Micale, F. G., & Nelson, J. A. (1993). Seven-day recall and other physical activity self-reports in children and adolescents. Medicine and Science in Sports and Exercise, 25(1), 99–108.
Miller, D. J., Freedson, P. S., & Kline, G. M. (1994). Comparison of activity levels using the Caltrac accelerometer and five questionnaires. Medicine and Science in Sports and Exercise, 26(3), 376–382.
Niero, M., Martin, M., Finger, T., Lucas, R., Mear, I., & Wild, D. (2002). A new approach to multicultural item generation in the development of two obesity-specific measures: The obesity and weight loss quality of life (OWLQOL) questionnaire and the weight-related symptom measure (WRSM). Clinical Therapeutics, 24(4), 690–700.
Patrick, D. L., & Bushnell, D. M. (2004). Obesity-specific patient reported outcomes: Obesity and weight loss quality of life (OWLQOL) and weight-related symptoms measure (WRSM). User’s manual and scoring diskette for united states version.
Maslow, A. H. (1943). A Theory of Human Motivation. Psychological Reviews, 50(4), 370–396.
Kaplan, G. A., Strawbridge, W. J., Cohen, R. D., & Hungerford, L. R. (1996). Natural history of leisure-time physical activity and its correlates: Associations with mortality from all causes and cardiovascular disease over 28 years. American Journal of Epidemiology, 144(8), 793–797.
Berke, E. M., Koepsell, T. D., Moudon, A. V., Hoskins, R. E., & Larson, E. B. (2007). Association of the built environment with physical activity and obesity in older persons. American Journal of Public Health, 97(3), 486–492. doi:10.2105/AJPH.2006.085837.
Acknowledgments
The authors wish to acknowledge the employees at the worksites who took the time to complete the baseline survey, follow-up survey, and physical measurements for the PACE study. Their voluntary participation made our investigation possible. The research reported here was supported by the National Heart, Lung, and Blood Institute R01 HL79491 and by the NCI Biobehavioral Cancer Prevention and Control Training Program (R25CA092408). The study sponsors played no role in any of the following: study design, the collection, analysis, and interpretation of data; the writing of the report; nor the decision to submit the paper for publication.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cash, S.W., Duncan, G.E., Beresford, S.A.A. et al. Increases in physical activity may affect quality of life differently in men and women: the PACE project. Qual Life Res 22, 2381–2388 (2013). https://doi.org/10.1007/s11136-013-0389-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-013-0389-6