Abstract
Purpose
We examine the impact of menopausal status, beyond menopausal symptoms, on health-related quality of life (HRQoL).
Methods
Seven hundred thirty-two women aged 40–65, regardless of health condition or menopausal status, were enrolled from single general internal medicine practice. Women completed annual questionnaires including HRQoL, and menopausal status and symptoms.
Results
The physical health composite of the RAND-36 is lower in late peri (45.6, P < .05), early post (45.4, P < .05), and late postmenopausal women (44.6, P < .01), and those who report a hysterectomy (44.2, P < .01) compared to premenopausal women (47.1), with effect sizes of Cohen’s d = .12-.23. The mental health composite of the RAND-36 is lower in late peri (44.7, P < .01), early post (44.9, P < .01), and late postmenopausal women (45.0, P < .05) and those who report a hysterectomy (44.2, P < .01) compared to premenopausal women (46.8), with effect sizes of Cohen’s d = .15–.20. Findings are comparable adjusted for menopausal symptom frequency and bother.
Conclusions
Over a 5-year follow-up period, we found a negative impact of menopause on some domains of HRQoL, regardless of menopausal symptoms. Clinicians should be aware of this relationship and work to improve HRQoL, rather than expect it to improve spontaneously when menopausal symptoms resolve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Menopause is a universal phenomenon for women. It is a biologic process, characterized by falls in estradiol and progesterone, increases in follicle stimulating hormone [1], as well as a life stage, characterized by changing roles such as the end of childbearing potential and children leaving home [2, 3]. While the biologic impact of menopause (e.g., bone loss) is well characterized, the impacts of menopause on a woman’s function and well-being, or health-related quality of life (HRQoL), are less clear.
Some studies have shown that the transition through menopause negatively impacts HRQoL [4, 5], while others have found no impact of menopausal status (i.e., the fluctuation or cessation of menses) alone [6–8], but rather an impact of menopausal symptoms (e.g., hot flashes and vaginal dryness) on HRQoL [7, 8]. These hallmark symptoms of menopause are caused in part by changes in reproductive hormone levels. Early in the menopause, most women experience hot flashes, which can persist for more than 5 years. Not all women who experience hot flashes, however, report them as bothersome [9]. In the later stages of menopause and persisting until death, women can experience vaginal dryness; bother associated with vaginal dryness has not been well studied. Recently, the Study of Women’s Health Across the Nation (SWAN), a community-based sample of women across the menopausal transition, found a negative impact of menopausal symptoms on HRQoL and much less of an impact of menopausal status [10].
Overall, studies that draw from populations of women seeking care for menopausal symptoms have shown a negative impact of later menopausal stage on HRQoL [11–13], while general population studies have either reported a negative impact only of menopausal symptoms, but not status, on HRQoL [6, 7] or failed to find any impact of menopause at all [8, 14].
Understanding the impact of menopause on HRQoL is important as our population ages. In this longitudinal study of patients in a primary care setting, we examine the impact of menopausal status alone, or in the context of menopausal symptoms, on HRQoL. We hypothesize that HRQoL initially declines in the early transition and then improves in the later postmenopause as women adapt to a new stage of life.
Methods
Study setting and population
Do stage transitions result in detectable effects? (STRIDE) is a longitudinal study of 732 midlife women enrolled between January and November 2005 from a single, academic general internal medicine practice. At the end of the practice’s computerized intake form [15], all women aged 40–65 were asked whether they would be interested in participating in a study examining the impact of menopause on HRQoL. Those who responded “yes” or “I’d like more information” were approached at the time of the outpatient visit. If a woman was not approached at the time of visit, she was asked about study participation at her next visit. Women who consented to participate were included in the study; women who did not consent were excluded. Details of recruitment have been previously described [16]. Of the 2,181 women asked during the computer intake about participation in the study, 1,280 responded “yes” or “I’d like more information” and 732 women enrolled in the study [16, 17]. Data presented here are from the first 5 years of STRIDE. STRIDE was approved by the University of Pittsburgh’s Institutional Review Board (#IRB0407165) and registered with Clinical Trials.gov (#NCT00097994). All participants provided written informed consent.
Data collection
Women could complete the annual STRIDE questionnaires from their home computers through the Internet, on tablet computers at the time of a primary care doctor’s visit, or over the telephone with a research staff member. Telephone surveys were read directly from and entered directly into the Internet-based form. Baseline body mass index (BMI: weight in kilograms/height in m2) was abstracted from the electronic medical record at the physician visit corresponding to study enrollment.
Women received reminder post cards, emails, and telephone calls beginning 1 month before they were due to complete their survey and continuing until they either completed the survey or 1 month beyond the survey due date had passed, whichever came first. Seven hundred twenty-eight women completed the baseline survey; 677, 636, 565, and 535 women completed the first, second, third, and fourth annual follow-up surveys, respectively.
Determination of menopausal status and symptom information
Participants’ self-reported menstrual bleeding patterns were assessed annually and used to determine menopausal status. Because women taking oral contraceptive pills (OCPs) and women who had a hysterectomy could not be classified based on bleeding patterns, they were placed in separate groups. Classification was otherwise based on the Stages of Reproductive Aging Workshop classifications with modification described previously [17]. Briefly, women were classified as premenopausal if they had regular bleeding patterns, early peri-menopausal if they had irregular bleeding patterns but their last menstrual period (LMP) occurred within the last 3 months; late peri-menopausal if their LMP was between 3 and 12 months ago; early postmenopausal if their LMP was between 12 months and 5 years ago; and late postmenopausal if LMP was 5 or more years ago.
Participants were asked to report the presence of (1) hot flashes and (2) vaginal dryness over the last 4 weeks. Response options were (1) none of the time; (2) rarely; (3) some of the time; (4) most of the time; and (5) all of the time. Women who reported symptoms at least some of the time were classified as having the symptom and were also asked to rate how often, over the last 4 weeks, the symptom bothered them using the same 5-point response scale. Those reporting bother at least some of the time were classified as being bothered. We constructed two summary symptom frequency-plus-bother variables, one for hot flashes and another for vaginal dryness, which was coded as (1) not having the symptom; (2) having the symptom but not reporting bother; or (3) having the symptom and reporting bother.
Outcomes
Women completed the RAND-36 annually. The RAND-36 has identical questions and responses to the Short Form 36 (SF-36) version 1, but uses a more sophisticated item response theory-based scoring mechanism [18]. The RAND-36 has two composite scores (the Physical and Mental Health Composites, our primary outcomes) comprised of eight scales (physical functioning, role limitations-physical, pain, general health perceptions, emotional well-being, role limitations-emotional, social functioning, and energy and fatigue, our secondary outcomes). Lower scores on the RAND-36 represent worse HRQoL.
Other variables
Social support was ascertained annually using the interpersonal support evaluation list (ISEL). Participants reported medical comorbidities annually using a checklist of nine common medical conditions: heart disease (including heart attack), heart failure, depression, stroke, emphysema or lung disease, arthritis, cancer (other than skin cancer), diabetes, and high blood pressure, summarized as none, 1–2, and ≥3 medical comorbidities. Hormone therapy use was determined based on self-reported use of estrogen with or without progesterone at the time of questionnaire completion. Participants reported marital status and educational attainment annually.
Baseline attitudes toward menopause and attitudes toward aging were summarized from questions developed for the SWAN [19]. Higher scores represent more negative attitudes. Age was calculated by subtracting date of birth from date of survey completion. Race was self-reported by participants at enrollment.
Analyses
Baseline participant characteristics are presented as frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Using linear mixed effects models, we initially examined the longitudinal relationship between (1) menopausal status and HRQoL, and (2) menopausal symptom frequency-plus-bother and HRQoL. We used multinomial logistic regression to examine the associations among menopausal status, symptom-plus-bother.
For subsequent analyses, we constructed separate linear mixed effects models with random intercepts and slopes, to account for heterogeneity, examining the longitudinal impact of menopausal status and symptom frequency-plus-bother on each of the two composites (primary outcomes) and eight individual scales (secondary outcomes) of the RAND-36. Base models included menopausal status, time-varying covariables (social support, medical comorbidities, hormone therapy use, and marital status), and baseline covariables (educational attainment, attitudes toward menopause, attitudes toward aging, race, and BMI). Fully adjusted models included the addition of either hot flash frequency-plus-bother or vaginal dryness frequency-plus-bother to the base models.
From these multivariable linear mixed effects models, we ascertained adjusted HRQoL scores for each menopausal status and symptom frequency-plus-bother group. To allow our findings to be placed in a context that includes other medical conditions, we calculated effect sizes (Cohen’s d) as the difference in HRQoL scores between the test group (e.g., early peri-menopausal women) and referent group (i.e., premenopausal women) divided by the test and referent groups average year-1 standard deviation in HRQoL scores [20]. Prior work has found effect sizes in the range of 0.09–0.28 to be clinically meaningful in studies using a variety of scoring algorithms for the RAND-36 [20, 21]. We used Stata version 11.0 (StataCorp, College Station, TX) for all analyses.
Results
The characteristics of the 728 STRIDE women who completed baseline questionnaires are shown in Table 1. On average, women were 50.8 years old. Twenty-two percent were premenopausal, 15% early peri, 6% late peri, 15% early post, and 19% late postmenopausal, 17% of women reported having had a hysterectomy and 6% reported taking OCPs. Consistent with the practice and Pittsburgh population, 25% of women were non-white. Forty-one percent of women reported hot flashes and 32% of women reported vaginal dryness at least some of the time; 79% of these women found at least one of these symptoms bothersome. The average HRQoL scores in this sample were slightly lower than population samples and similar to clinical samples, ranging from 43.8 (pain) to 46.9 (physical functioning) (Table 1) [18].
Initial models showed significant relationships between (1) menopausal status and HRQoL, (2) menopausal symptom frequency-plus-bother and HRQoL, and (3) menopausal status and symptom frequency-plus-bother (data not shown).
Impact of menopausal status on HRQoL
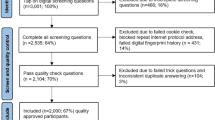
The impact of menopausal status on HRQoL (based on multivariable models, adjusted for time-varying and baseline covariables) is shown in Fig. 1 and Table 2.
The RAND-36 composite scores, adjusted for year, social support, hormone therapy use, educational attainment, medical comorbidities, body mass index, attitudes toward menopause, attitudes toward aging, marital status, race, and baseline age, for each menopausal status group. Significant differences are indicated as follows: a P < .05, b P < .01
Physical health quality of life
Compared to premenopausal women, the physical health composite of the RAND-36 is significantly lower in late peri, early post, and late postmenopausal women, as well as those who have had a hysterectomy (Fig. 1, panel A). The effect sizes are small, ranging from Cohen’s d = .12-.23 (Table 2). The results are qualitatively similar in models that adjust for (1) hot flash frequency-plus-bother and (2) vaginal dryness frequency-plus-bother (Table 2), showing that the impact of menopausal status on the physical health-related quality of life is partially independent of menopausal symptoms.
In secondary analyses, similar results (Table 2; Fig. 1, panel B) are seen across three of the four scales of the RAND-36 that comprise the physical health component: physical functioning, pain, and general health perceptions with the strongest and most consistent effects seen between menopausal status and pain and general health perceptions.
Mental health quality of life
Compared to premenopausal women, the mental health composite of the RAND-36 is lower in late peri, early post, and late postmenopausal women, as well as those who report a hysterectomy, with effect sizes of Cohen’s d = .17, .16, .15, and .20, respectively (Table 2; Fig. 1). In models adjusted for hot flashes frequency and associated bother, the results are qualitatively similar but the significance of the relationship is attenuated (Table 2). Models adjusted for vaginal dryness frequency and associated bother are similar to base models, including only menopausal status (Table 2). This indicates that the impact of menopausal status on mental health-related quality of life is at least partially accounted for by menopausal symptom frequency and associated bother.
In secondary analyses (Table 2; Fig. 1) of the four RAND-36 scales that comprise the mental health composite, the impact of menopausal status is most apparent for energy and fatigue. Compared to premenopausal women, late peri, early post, and late postmenopausal women as well as those who reported hysterectomies had worse scores on the energy and fatigue scale; late peri-menopausal and early postmenopausal women also had a significant decrement in emotional well-being. Social function was worse only in women who had hysterectomies compared to premenopausal women. There was no significant impact of menopausal status on role limitations due to emotional problems. In all of these models, addition of menopausal symptoms partially accounted for the relationship between menopausal status and HRQoL.
Relationships of other variables in these models to HRQoL
Menopausal symptom frequency-plus-bother
We next considered the relative associations between menopausal symptom frequency-plus-bother in relation to HRQoL. In these multivariable models (Table 3), compared to women who do not report hot flashes, those who report hot flashes but are not bothered by them do not experience declines in HRQoL, while those who report both hot flashes and associated bother have a decrement in all aspects of HRQoL, including role functioning-physical.
In contrast to hot flashes, women with vaginal dryness that they do not report as bothersome have some decrement in HRQoL, specifically the mental health composite and the emotional well-being and social functioning scales. The most striking decrements, however, were seen among women who report vaginal dryness-associated bother; these women have significantly lower scores on all aspects of HRQoL except physical functioning, pain, and role limitations-emotional.
Other variables
Higher social support (ISEL) (P < .001), higher educational attainment (P < .01, <.001, and <.001 for some college, completed college, and completed graduate school compared to high school education or less), fewer comorbid medical conditions (P < .001), lower BMI (P < .001), being married or in a committed relationship (P = .02), and more positive attitudes toward menopause (P < .001) were related to better physical aspects of HRQoL. Older age at enrollment (P < .001), more self-assessed social support (ISEL) (P < .001), higher baseline educational attainment (P < .04, <.001, and <.001 for some college, completed college, and completed graduate school compared to high school education or less), fewer comorbid medical conditions (P < .001), lower BMI (P < .01), more positive attitudes toward menopause (P < .001), and more positive attitudes toward aging (P < .02) were associated with better mental aspects of HRQoL. There were no differences in HRQoL between racial groups. (data not shown)
Comment
We followed a cohort of midlife women enrolled from a primary medical care setting. In contrast to our hypothesis, we found that, over 5 years, women who have entered the menopausal transition or are in the postmenopause, as well as those women who have undergone hysterectomy, have lower HRQoL compared to premenopausal women, even after accounting for hot flashes and vaginal dryness. The role of hysterectomy status should be examined further in future studies to understand whether women who undergo hysterectomies have lower quality of life prior to surgery or after surgery as this could impact women’s decision making.
The decrement in HRQoL associated with menopause is most prominent in overall physical health, pain, and general health, as well as energy and fatigue. These constructs represent the frequency of pain and role interference due to pain, the woman’s perception of her health in general (e.g., feeling well or ill), and feeling energetic versus feeling tired and worn out, respectively. The emotional aspects of HRQoL, including mental health overall, and emotional well-being (general mood and affect including depression, anxiety, and positive well-being) show an attenuated pattern in relation to menopausal stage, with a more pronounced negative impact of the late peri and early postmenopausal stages, and less impact in the late postmenopause. It is notable that most scales that assess interference (role limitation due to physical health problems, role limitations due to emotional health problems, social functioning, and physical functioning) are not as impacted by menopausal stage. One interpretation of these findings is that women are not allowing menopause to interfere with most aspects of their lives, despite feeling worse.
Menopausal symptoms (hot flashes and vaginal dryness) have an additional negative impact on HRQoL, regardless of menopausal stage. Prior work has shown that the presence of menopausal symptoms may be associated with impairments in HRQoL [7, 8, 10] and has suggested an importance of hot flash-associated bother over and above simple symptom frequency [9]. We extend this work to more explicitly examine the associations among menopausal status, menopausal symptom frequency and associated bother, and HRQoL. Women with hot flashes have worse HRQoL on all aspects, including those representing interference, but only if they find the symptom bothersome. In contrast, women who report vaginal dryness even in the absence of perceiving the symptom as bothersome have worse mental health composite scores, as well as worse emotional well-being and social functioning (interference with social activities with friends, family, and groups). Women who perceive vaginal dryness as bothersome also have worse physical health composite scores and decline in role functioning due to physical health problems, energy and fatigue, and general health perception.
Our findings are not only statistically significant but also they are within the ranges for the minimally important difference. The minimally important difference is the smallest difference in score of a particular instrument that patients perceive as beneficial, worthwhile, and/or important and would, therefore, drive clinicians to consider management changes [21]. While there is no universally accepted minimally important difference, effect sizes between 0.2 and 0.5 are generally accepted [22]. As noted previously, studies using the RAND-36 [21] to examine conditions such as asthma [23], arthritis [24], and low back pain [25] have found effect sizes in the range of 0.09–0.28 to be clinically relevant.
Our findings show a more consistent negative impact of menopause on HRQoL, irrespective of symptoms, than does the current literature [7]. There are a number of reasons for this. While we enrolled a general cohort of women (i.e., they were not seeking care for menopause-related complaints), they were enrolled from a primary care population. As such, their average HRQoL scores were in a range that may have allowed us to see more variation in HRQoL scores. Other studies have enrolled women with HRQoL scores that indicated better functioning than a general population, and as such may be limited by a ceiling effect in the instrument. We also used the RAND-36 item response theory-based scoring algorithm [18]. Studies have shown this algorithm to be more responsive to change than the traditional scoring algorithm [26].
Rather than imply that the physiologic changes of menopause are intrinsically causing a decrement in HRQoL, we interpret these data as evidence that other changes that may occur concurrent to menopause, beyond hot flashes and vaginal dryness, and need to be examined. We have adjusted our models for many common confounders, including social support, race, education, marital status, BMI, and presence of medical comorbidities as well as attitudes toward menopause and aging. However, several potentially important variables that can change with aging were not examined such as changes in intimate relationships (e.g., changes in sexual activity due to self or partner functioning), alterations in sleep patterns, changes in caregiving responsibilities, and severity of chronic medical conditions (e.g., worsening of pulmonary disease, progression of arthritis). Nonetheless, the decrement in HRQoL associated with menopausal status in STRIDE is similar to decrements seen with other health conditions [26]. While some of the decrement is related to hot flashes, which may improve, the vaginal dryness associated with the menopausal transition does not spontaneously resolve. Physicians and patients should be attentive to the declines in HRQoL in midlife women, and not just expect that they will get better when hot flashes resolve. Practitioners and patients should continue to examine to other aspects of women’s lives beyond menopausal symptoms that occur simultaneously and may be amenable to intervention.
These analyses have a number of limitations that deserve mention. STRIDE participants were enrolled from a single primary care practice. Women in a postindustrial US city may not generalize to the rest of the population. While primary care is not menopause-specific care, primary care may not represent the broader population including women who chose not to access health care. They do, however, represent women primary care practitioners are likely to see in their offices and may therefore help inform clinical practice. STRIDE is an observational study and, as such, causality cannot be determined. Of the 2,181 potentially eligible women who were asked via the practice’s computer intake form to participate in this study, only 34% enrolled. While this response rate is low, it compares favorably to recruitment for other studies of midlife women; for example, about 24% of eligible women enrolled in the SWAN longitudinal study [27]. Women were also highly educated, which, because the primary care practice is located within an academic medical center, reflects the practice demographics. As more educated women tend to have better HRQoL, our observed differences could underestimate the actual differences in more diverse clinical settings. The practice’s computer information form is only available in English, which may have excluded women who were not able to complete the form in English. We also have women completing the survey through multiple modes (i.e., internet versus telephone) and did not record the mode of administration. We are therefore unable to adjust for administration mode. While this may bias results, telephone-completed surveys tend to be more positive and our older, postmenopausal women are more likely to use telephone making it likely that any bias would be in the direction of making our observed differences smaller and the true differences between premenopausal women and those in the transition larger [28].
Conclusions
Among women accessing primary care, transitioning into the menopause, regardless of the presence of its hallmark symptoms of hot flashes and vaginal dryness, is associated with a decrement in HRQoL. Clinicians and women should be aware of this impact and work to improve HRQoL, as opposed to expecting HRQoL to spontaneously improve when symptoms resolve. Researchers need to look beyond the classic menopausal symptoms to a more comprehensive biopsychosocial model in order to better understand decline in HRQoL during the menopause.
Abbreviations
- BMI:
-
Body mass index
- HRQoL:
-
Health-related quality of life
- ISEL:
-
Interpersonal support evaluation list
- LMP:
-
Last menstrual period
- OCP:
-
Oral contraceptive pills
- STRIDE:
-
Do stage transitions result in detectable effects?
- SWAN:
-
Study of Women’s Health Across the Nation
References
Santoro, N., Brown, J. R., Adel, T., & Skurnick, J. H. (1996). Characterization of reproductive hormonal dynamics in the perimenopause. Journal of Clinical Endocrinology and Metabolism, 81(4), 1495–1501.
Dillaway, H. E. (2008). “Why can’t you control this?” How women’s interactions with intimate partners define menopause and family. Journal of Women Aging, 20(1–2), 47–64.
Olshansky, E. (2005). Feeling normal. Women’s experiences of menopause after infertility. MCN; American Journal of Maternal Child Nursing, 30(3), 195–200.
Dennerstein, L., Lehert, P., & Guthrie, J. (2002). The effects of the menopausal transition and biopsychosocial factors on well-being. Archives of Women Mental Health, 5(1), 15–22.
Mishra, G. D., Brown, W. J., & Dobson, A. J. (2003). Physical and mental health: changes during menopause transition. Quality of Life Research, 12(4), 405–412.
Avis, N. E., Assmann, S. F., Kravitz, H. M., Ganz, P. A., & Ory, M. (2004). Quality of life in diverse groups of midlife women: assessing the influence of menopause, health status and psychosocial and demographic factors. Quality of Life Research, 13(5), 933–946.
Kumari, M., Stafford, M., & Marmot, M. (2005). The menopausal transition was associated in a prospective study with decreased health functioning in women who report menopausal symptoms. Journal of Clinical Epidemiology, 58(7), 719–727.
Cheng, M. H., Lee, S. J., Wang, S. J., Wang, P. H., & Fuh, J. L. (2007). Does menopausal transition affect the quality of life? A longitudinal study of middle-aged women in Kinmen. Menopause, 14(5), 885–890.
Thurston, R. C., Bromberger, J. T., Joffe, H., Avis, N. E., Hess, R., Crandall, C. J., et al. (2008). Beyond frequency: Who is most bothered by vasomotor symptoms? Menopause, 15(5), 841–847.
Avis, N. E., Colvin, A., Bromberger, J. T., Hess, R., Matthews, K. A., Ory, M., et al. (2009). Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women’s Health Across the Nation. Menopause, 16(5), 860–869.
Blumel, J. E., Castelo-Branco, C., Binfa, L., Gramegna, G., Tacla, X., Aracena, B., et al. (2000). Quality of life after the menopause: A population study. Maturitas, 34(1), 17–23.
Genazzani, A., Nicolucci, A., Campagnoli, C., Crosignani, P., Nappi, C., Serra, G., et al. (2002). Assessment of the QoL in Italian menopausal women: Comparison between HRT users and non-users. Maturitas, 42(4), 267–280.
Limouzin-Lamothe, M. A., Mairon, N., Joyce, C. R., & Le Gal, M. (1994). Quality of life after the menopause: influence of hormonal replacement therapy. American Journal of Obstetrics and Gynecology, 170(2), 618–624.
Smith-DiJulio, K., Woods, N. F., & Mitchell, E. S. (2008). Well-being during the menopausal transition and early postmenopause: A longitudinal analysis. Menopause, 15(6), 1095–1102.
Hess, R., Santucci, A., McTigue, K., Fischer, G., & Kapoor, W. (2008). Patient difficulty using tablet computers to screen in primary care. Journal of General Internal Medicine, 23(4), 476–480.
Hess, R., Olshansky, E., Ness, R., Bryce, C. L., Dillon, S., Kapoor, W., et al. (2008). Pregnancy and birth history influence women’s experience of menopause. Menopause, 15(5), 435–441.
Hess, R., Conroy, M. B., Ness, R., Bryce, C. L., Dillon, S., Chang, C. C., et al. (2009). Association of lifestyle and relationship factors with sexual functioning of women during midlife. Journal of Sexual Medicine, 6(5), 1358–1368.
Hays, R. D. (1998). RAND 36: Health status inventory (1st ed.). San Antonio, TX: The Psychological Corporation.
Sommer, B., Avis, N., Meyer, P., Ory, M., Madden, T., Kagawa-Singer, M., et al. (1999). Attitudes toward menopause and aging across ethnic/racial groups. Psychosomatic Medicine, 61(6), 868–875.
Samsa, G., Edelman, D., Rothman, M., Williams, G. R., Lipscomb, J., & Matchar, D. (1999). Determining clinically important differences in health status measures: A general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics, 15(2), 141–155.
Hays, R., & Woolley, J. (2000). The concept of clinically meaningful difference in health-related quality-of-life research. How meaningful is it? Pharmacoeconomics, 18(5), 419–423.
King, M. T. (2011). A point of minimal important difference (MID): A critique of terminology and methods. Expert Review of Pharmacoeconomics and Outcomes Research, 11(2), 171–184.
Ware, J., Kosinski, M., & Keller, S. (1994). SF-36 physical and mental health summary scales: A user’s manual. Boston, MA: The Health Institute.
Kosinski, M., Zhao, S. Z., Dedhiya, S., Osterhaus, J. T., & Ware, J. E., Jr. (2000). Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis and Rheumatism, 43(7), 1478–1487.
Lansky, D., Butler, J. B., & Waller, F. T. (1992). Using health status measures in the hospital setting: From acute care to ‘outcomes management’. Medical Care, 30(5 Suppl), MS57–MS73.
Nortvedt, M. W., Riise, T., Myhr, K. M., & Nyland, H. I. (2000). Performance of the SF-36, SF-12, and RAND-36 summary scales in a multiple sclerosis population. Medical Care, 38(10), 1022–1028.
Sowers, M., Crawford, S. L., Sternfeld, B., Morganstein, D., Gold, E. B., Greendale, G. A., et al. (2000). SWAN: A multicenter, multiethnic, community-based cohort study of women and the menopausal transition. In R. A. Lobo, J. Kelsey, & R. Marcus (Eds.), Menopause: Biology and pathobiology. San Diego: Academic Press.
Hays, R. D., Kim, S., Spritzer, K. L., Kaplan, R. M., Tally, S., Feeny, D., et al. (2009). Effects of mode and order of administration on generic health-related quality of life scores. Value Health, 12(6), 1035–1039.
Acknowledgments
The study was supported by grant K23 AG024254 from the National Institutes of Health’s National Institute on Aging. The funding organization was independent of the design and conduct of the study; collection, management, analysis, and interpretation of data; and preparation, review, or approval of the manuscript. We gratefully acknowledge the 732 women who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hess, R., Thurston, R.C., Hays, R.D. et al. The impact of menopause on health-related quality of life: results from the STRIDE longitudinal study. Qual Life Res 21, 535–544 (2012). https://doi.org/10.1007/s11136-011-9959-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-011-9959-7