Abstract
Purpose
We determined the association of neighborhood foreclosure risk on the health status of a statewide sample of breast cancer survivors (n = 1047) and the extent to which covariates accounted for observed associations.
Methods
Measures of self-rated health and several covariates were obtained by telephone interview 1 year after diagnosis. We used the federal Housing and Urban Development agency’s estimated census-tract foreclosure-abandonment-risk score and multilevel, logistic regression to determine the association of foreclosure risk (high, moderate versus low) with self-rated health (fair-poor versus good, very good, excellent) and whether covariates could explain the observed association.
Results
Women who resided in high-foreclosure-risk (HFR) areas were 2.39 times (95% CI: 1.83–3.13) more likely to report being in fair-poor health than women who lived in low-foreclosure-risk areas. The odds ratio (OR) was reduced for women who lived in high-foreclosure-risk versus low-foreclosure-risk areas after adjusting for income (HFR OR: 1.78; 95% CI: 1.01–3.15), physical activity (HFR OR: 1.74; 95% CI: 0.98–3.08), and perceived neighborhood conditions (HFR OR: 1.76; 95% CI: 1.02–3.05).
Conclusions
Breast cancer survivors who lived in census tracts with high- versus low-foreclosure risk reported poorer health status. This association was explained by differences in household income, physical activity, and perceived neighborhood conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the first 6 months of 2009, more than 1.5 million homes in the United States were affected by foreclosure (default notices, auction sales, and bank repossessions),Footnote 1 a nine percent increase in total properties from the previous 6 months and nearly a 15% increase in total properties from the first 6 months of 2008 [1]. One of every 84 housing units received at least one foreclosure filing in the first half 2009. Some have called this the most pressing economic crisis in a generation [2]. Despite changes in the mortgage industry, legislative action, and increased levels of loan modifications earlier in 2009, foreclosures have continued to increase to record levels fueled in part by high unemployment. Home foreclosures threaten to undermine the economic recovery before it can get under way.
Little is known about the health of those directly affected by home foreclosure. A recent study showed worse health status of those whose homes were foreclosed relative to those not so affected, but this difference was explained by differences in sociodemographic characteristics of the study participants [3]. In the United Kingdom, home repossession increased the risk of poor mental health [4]. Despite escalating mortgage foreclosure rates, a literature review recently demonstrated that few studies have examined this topic [5].
Even less is known about the indirect effect of foreclosures on the health of neighborhood residents. One recent study showed that an increase in home foreclosures led to an increase in neglected swimming pools, which was associated with an increase in the number of cases of West Nile Virus [6]. And while adverse neighborhood conditions are associated with worse health status [7], it is unclear whether the overall health status of residents is affected by neighborhood foreclosures. Since vulnerable populations (i.e., those with a history of poor health or chronic disease) appear to be at greater risk of adverse health outcomes following the foreclosure of their home [5], we hypothesized that breast cancer survivors would be at greater risk of poor health if they lived in neighborhoods with higher foreclosure rates. The purpose of this study was to determine the association between neighborhood foreclosure and health status of women with breast cancer. Specifically, this study determined (1) whether breast cancer survivors who lived in areas of high-foreclosure risk reported worse health status than those who lived in low-foreclosure-risk areas and (2) the extent to which covariates (including sociodemographics, behaviors, census-tract poverty rate, perceived neighborhood conditions, access to medical care, psychosocial factors, and clinical factors) accounted for any observed associations between foreclosure risk and self-reported health status.
Methods
Study sample
Missouri women age 25 or older diagnosed with first primary breast cancer from June 2006 through June 2008 were identified from the statewide Missouri Cancer Registry. Women were recruited by mail; up to 15 phone calls were made to nonrespondents. After obtaining Institutional Review Board approval and informed consent, trained interviewers administered computer-assisted telephone interviews 1 year after diagnosis.
Self-rated health
Self-rated health, based on a single question, is a strong independent predictor of health care utilization, functional ability, and subsequent mortality [8–10]. It is considered to be a reliable and valid measure of population health [11–13]. Self-rated health was based on responses to the question, ‘‘In general, would you say your health is excellent, very good, good, fair, or poor?’’ Analyses were based on dichotomizing self-rated health responses as ‘‘fair’’ or ‘‘poor’’ versus all other categories, following common practice [14–16].
Predicted census-tract foreclosure risk
We used the federal Housing and Urban Development (HUD) agency’s estimated census-tract foreclosure-abandonment-risk score. This score, ranging from 0 to 10, predicts the risk for foreclosed and abandoned homes in census tracts across the United States. This score was designed to target funds by state or local governments as part of the Neighborhood Stabilization Program [17]. Rather than documenting the actual number of foreclosures, it indicates the risk for foreclosures at the census-tract level using the following four federal data elements: (1) the decline in home values as of June 2008 compared with peak home value since 2000 at the Metropolitan/Micropolitan/NonMetropolitan level from the Office of Federal Housing Enterprise Oversight, (2) percent of all loans made between 2004 and 2006 that are high cost (loans being made at 3 basis points or more above prime rate) at the census-tract level from the Federal Reserve Home Mortgage Disclosure Act, (3) the unemployment rates in places and counties as of June 2008 from the Labor Department, and (4) the percentage of residential addresses identified as being vacant for 90 days or longer as of June 2008 at the census-tract level from the United States Postal Service. HUD analysis shows that 75% of the variance between states on foreclosure rates can be explained by the first three variables. In Missouri, the correlation between estimated county foreclosure risk and Equifax 90-day mortgage delinquency data for counties with more than 15,000 households was 0.59. The street address of 26 breast cancer survivors could not be geocoded and therefore not assigned a foreclosure-abandonment-risk score.
Property foreclosure
Listings of Missouri properties, which are publicly filed court documents, were obtained from Realtytrac.com for the period January 2007 through August 2009. By linking with the respondents’ street addresses, we were able to determine whether any of the breast cancer survivors were directly affected by home foreclosure. This was done both for women who owned and for women who rented their homes. Renters may be directly affected by foreclosure of the owner’s house in which they lived. Realtytrac.com collects foreclosure data from more than 2,200 counties across the United States, which accounts for more than 90% of the US population. We considered all three phases of foreclosure: default, auction, and real estate owned.
Covariates associated with self-rated health
We examined seven blocks of factors that could explain a potential association between census-tract foreclosure risk and self-rated health, including: (1) sociodemographic factors, (2) cancer-related behaviors, (3) perceived neighborhood conditions, (4) census-tract poverty rate, (5) access to medical care, (6) psychosocial factors, and (7) clinical characteristics. Covariates included in the analysis were patterned after other studies of cancer survivors and the general population [18].
First, sociodemographic factors included race, age group, Hispanic origin, income, educational attainment, employment, marital status, urbanicity, home ownership, length (in years) at current residence, food security, and income adequacy. After geocoding the street address of the study participants, we used the census-tract-based rural–urban commuting codes to classify the location of residence into seven groups: urban core, other urban, large rural core, other large rural, small rural core, other small rural, and isolated rural census tracts [19]. Food security was based on the question whether participants reported having been concerned about having enough food in the past month. Income adequacy was measured by asking participants whether they felt their household income was comfortable, enough to make ends meet, or not enough to make ends meet.
Second, cancer-related behaviors consisted of current smoking status, participation in any physical activity, and alcohol use during the past month, all of which were from the Behavioral Risk Factor Surveillance System (BRFSS). One question assessed participation in any physical activity in the past month. Although no universally agreed upon recommendations exist for alcohol consumption in survivors, there is some agreement that female survivors who consume alcohol are generally urged to limit its use to one drink per day [20]. We coded alcohol status as elevated use or not based on these recommendations.
Third, perceived neighborhood conditions were measured using four scales. Perceived neighborhood disorder was measured with the 15-item Ross-Mirowsky scale consisting of two subscales, perceived social disorder and perceived physical disorder/decay [21]. Collective efficacy was measured with two subscales, informal social control and social cohesion and trust [22]. Neighborhood fear was measured with 3 items capturing the number of days in the previous week during which respondents feared violent or criminal activities or were afraid to leave their home [23]. Scale internal consistency was ≥0.70.
Fourth, census-tract poverty rate was obtained from the 2000 census. Poverty was selected because it is a robust indicator of socioeconomic status across levels of geography and time, has been associated with various health outcomes, and has relevance for policymakers [24]. Area poverty level was determined using data on the percent living in poverty in the residents’ census tract and classified in three categories: 0–9.9, 10–19.9, and ≥20%.
Fifth, access to medical care consisted of having health care insurance at the time of the interview, being unable to see a doctor during the previous 12 months because of cost, and having a place to go when sick or needing advice about health. All questions were from the BRFSS. Women were considered to have reduced access to medical care if they answered “yes” to any of the questions.
Sixth, psychosocial factors consisted of social support using the Medical Outcomes Study Social Support Survey [25], two measures of perceived stress [26, 27], and depressed mood using the validated 11-item version of the Center for Epidemiologic Studies Depression (CES-D) scale [28].
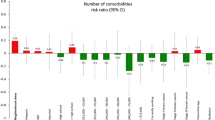
Seventh, clinical characteristics consisted of collaborative stage at diagnosis from the Missouri Cancer Registry, comorbid conditions using Katz’s validated adaptation of the Charlson comorbidity index [29], breast-surgery-associated side effects, and types of treatment received. Based on the literature [30] and surgeons’ anecdotal reports of patients’ complaints after surgery, we developed a five-item measure of breast-surgery-associated side effects with higher scores indicating more severe side effects (alpha = 0.74). Treatment received consisted of type of surgery, axillary lymph node removal, receipt of chemotherapy, receipt of radiotherapy, and taking hormonal therapy at the time of the interview. Self-reported treatment is accurate relative to medical record review [31].
Statistical analysis
We assessed the correlation between census-tract foreclosure-risk score and poverty rate using Pearson’s correlation. We used multilevel, logistic regression models to determine the association of foreclosure risk and each of the covariates on self-rated health status. Next, we determined whether the covariates explained the association between foreclosure risk and self-rated health by adding all variables comprising a block of factors to the logistic model containing only foreclosure risk. This was done for each of the seven blocks of factors separately. Reduction in the parameter estimate for the foreclosure risk relative to unadjusted analysis was evidence for the explanatory power of the blocks of factors. We examined specific variables within a particular block of factors when the block showed a significant reduction in odds ratio (at least 20%) for foreclosure-risk status; we report these data for specific variables in the text of the Results section. We used the GLIMMIX macro in SAS 9.1 to construct the multilevel models. The fit of the models was analyzed by the calculation of Akaike information criterion goodness-of-fit statistic, with lower values indicating better fit. This statistic allows for the comparison of non-nested models.
We estimated a multivariable logistic regression model of whether or not participants were included in the analytic sample and computed their predicted probability of inclusion based on age, race, and stage at diagnosis using Missouri Cancer Registry data. We determined the probability of participation rate (i.e., inclusion in the analytic sample), and we used the inverse to re-weight the data. This method gives greater weight to participants included in the analytic sample who are similar to women who were not included in the sample [32]. The total of the weighted participants reflects the actual number of women interviewed, implying that some women received weights that were greater than 1, while others received weights that were less than 1.
To assess the extent to which a woman’s characteristics may help determine the location of her residence, we examined the probabilities for living in census tracts with high- versus moderate/low-foreclosure risk modeled as a function of individual demographic factors using a propensity score model [33–35]. This allowed us to examine whether there was overlap between people of different demographic factors who lived in high- versus moderate/low-foreclosure risk. If the women who lived in high- and moderate/low-foreclosure-risk census tracts had similar and predominantly overlapping distributions of propensities, then we would know that there was little social stratification, implying that women of all “types” lived in both types of census tracts and that the analysis did not rely on extrapolation.
Results
During the study period, 4,020 women with first primary breast cancer were eligible to participate, 675 of whom we were unable to contact. Of the remaining women, 1,164 women completed the telephone interview for a participation rate of 35.2%. The cancer registry data of all eligible women indicated that nonparticipants were on average 4.9 years older (P < 0.001) and more likely to be African-American (11.9% vs. 6.1%, P < 0.001) than women who participated in the study. There was no difference in stage at diagnosis and rural versus urban location among study participants and nonparticipants. Seventy women were excluded because of high scores on the Orientation-Memory-Concentration test. Forty-seven women were excluded because of missing data on one or more of the covariates of interest, leaving 1,047 women available for analysis.
Based on the distribution of the census tracts in our study data, we categorized the ten foreclosure-abandonment-risk scores into three groups: 0–3 (low risk, n = 242), 4–6 (moderate risk, n = 207), and 7–10 (high risk, n = 201). The street address of 26 breast cancer survivors could not be geocoded and therefore not assigned a census-tract foreclosure-risk score.
Table 1 shows the characteristics of the study population according to area foreclosure risk and their unadjusted association with fair-poor self-rated health. Compared with women who lived in low-foreclosure-risk areas, women who lived in high-foreclosure-risk areas were more likely to be African-American, unmarried, rent their home, have lower incomes, unable to make ends meet, be unemployed, stressed, concerned about food security, uninsured, unable to see a doctor because of cost, and perceive conditions in their neighborhoods as poor, and they were less likely to participate in physical activity, have lymph nodes removed, and receive radiotherapy. Several characteristics also were associated with increased likelihood of fair-poor self-rated health. The home of only one woman was foreclosed between the date of diagnosis and the interview. The correlation between area foreclosure risk and poverty rate was 0.384 (P < 0.0001).
Sixteen percent of all participants reported being in fair or poor health. A higher percentage of women who lived in high-foreclosure-risk areas reported being in fair-poor health (22.9%) compared with those who lived in moderate (14.0%) or low-foreclosure-risk (13.3%) areas. Women who resided in high-foreclosure-risk areas were 2.39 times (95% CI: 1.83–3.13) more likely to report fair-poor health than women who lived in low-foreclosure-risk areas (Table 2, Model 1). Women who lived in moderate-foreclosure-risk areas were equally likely to report fair-poor health as the reference group (OR: 1.15; 95% CI: 0.67–1.96).
The odds ratio for women living in high-foreclosure-risk areas was reduced to nonsignificance after including sociodemographic factors (Model 2) and behavioral factors (Model 3) separately to Model 1 (Table 2). However, the odds ratio changed little for women living in high-foreclosure-risk areas when each of the other four blocks of factors (poverty rate, access to medical care, psychosocial factors, and clinical factors) was added separately to Model 1 (Table 2).The best model fit (lowest Akaike information criterion) was observed when adding the following variables from Models 2 and 3: physical activity, physical disorder, and household income to Model 1 (Table 2). The best fitting model (Model 9) showed that breast cancer survivors who lived in high-foreclosure-risk areas were equally likely as those who lived in low-foreclosure-risk areas to report being in fair-poor health (OR: 1.15; 95% CI: 0.62–2.13). In this model, survivors with annual household incomes of less than $25,000 (OR: 4.43; 95% CI: 2.52–7.79), who were not physically active (OR: 4.19; 95% CI: 2.89–6.08), and who reported more physical disorder (OR: 1.19; 95% CI: 1.10–1.27 per point) were more likely to report being in fair-poor health. The fit of a model containing all covariates was very bad (AIC: 7291.0) and is not reported here.
Examining the propensities for living in neighborhoods with high- versus moderate/low-foreclosure risk, we found that the minimum, mean, median, and maximum propensity scores were all essentially the same across both foreclosure-risk scores. Thus, women who lived in high and moderate/low-foreclosure-risk census tracts had similar and predominantly overlapping distributions of propensities, indicating little social stratification.
Discussion
The adverse effect of foreclosures on various neighborhood characteristics is well established [36]. Foreclosure reduces the value of the foreclosed home, but it also reduces the value of neighboring properties, which lowers property tax revenue for local and state governments. This may subsequently lower availability and access to needed services not only for those people whose homes have been foreclosed but also for people who live nearby whose homes were not foreclosed. This study showed that breast cancer survivors who resided in high-foreclosure-risk areas were 2.39 times more likely to report fair-poor health than women who lived in low-foreclosure-risk areas. Our findings extend previous studies that focused on individuals directly affected by foreclosure by showing that area-level foreclosure risk also indirectly affects the health of breast cancer survivors [3]. Our findings show that area-level foreclosure risk conveys effects beyond that of area-level poverty rate.
Our study also examined the extent to which covariates accounted for observed associations and determined that lower household income, no physical activity, and worse perceived neighborhood conditions (physical disorder) explained why breast cancer survivors who lived in high-foreclosure-risk areas reported poorer health than those in low-foreclosure-risk areas. Household income may act as both a confounder and a mediator for the observed association. Household income can be a compositional confounder (i.e., a confounder that describes characteristics of a person living in a geographic area) if low-income persons are more likely to live in high-foreclosure-risk areas. Household income also may act as a mediator as a potential result of high local unemployment rates (included in the foreclosure-risk score) or of other unmeasured variables. Of all measured sociodemographic factors, household income explained the observed association between high-foreclosure risk and self-rated health, whereas race, age, perceived income adequacy, and the other demographic variables did not.
In addition to household income, lack of any physical activity in the past 30 days explained our observed association. It could be that persons who are more physically active live in neighborhoods with more resources to be physically active, which also are more likely to be low-foreclosure-risk areas. It is unlikely that the perceived neighborhood conditions of fear, collective efficacy, and social disorder were responsible for the mediating effect of physical activity since only physical disorder was able to explain the observed association, and this factor was independently associated with self-rated health in our final model. It also is unlikely that aspects of the built environment, such as street density and mixed land use, allow breast cancer survivors to be more physically active, since these are typically located in more urban areas, which also is where foreclosure risk was higher. Importantly, access to medical care, psychosocial factors (perceived stress and depressive symptoms), and clinical factors did not explain the observed associations between foreclosure-risk areas and health.
Thus, it may be that household income, physical activity, and perceived neighborhood conditions capture important and relevant aspects of neighborhoods that are at high-foreclosure risk. Although we included many covariates that were previously found to be associated with self-rated health, due to the cross-sectional nature of the study, we were unable to test more complex conceptual models. Unmeasured variables might explain the association between foreclosure risk and self-rated health. Future studies may examine this in more detail.
This study was limited by the low response rate, increasing the likelihood for selection bias, the use of census tract as a proxy for neighborhood, and the lack of data about the foreclosure risk at the individual level. We have attempted to reduce the effect of selection bias using a propensity score model. It is difficult to determine the direction of potential bias based on the data available to us. If there was no difference in participation rates by exposure status (foreclosure risk) or disease status (self-rated health), then the effect of our low participation rate would be negligible. It is only when differential misclassification exists that the observed odds ratio could have overestimated the actual risk. Since we did not have any information about the participation rates by exposure and disease status, we weighted the data using propensity score methods to reduce the effect of potential selection bias. Lack of data about a participant’s own foreclosure risk is unlikely to have affected our findings, since factors such as income, income adequacy, home ownership, and employment were available in the analysis. Also, because of the response rate, generalizability is limited in older and African-American breast cancer survivors. However, the strengths of our study included a statewide sample of breast cancer survivors, the extensive list of predictors of self-rated health that were included, the multilevel approach used, and the examination of social stratification.
In conclusion, breast cancer survivors who lived in high-foreclosure-risk versus low-foreclosure-risk areas reported poorer health status. This association was explained by lower household income, no physical activity, and worse perception of neighborhood conditions.
Notes
Foreclosure: A situation in which a homeowner is unable to make principal and/or interest payments on his or her mortgage, so the lender, be it a bank or building society, can seize and sell the property as stipulated in the terms of the mortgage contract.
Abbreviations
- OR:
-
Odds ratio
- HUD:
-
Housing and urban development
- BRFSS:
-
Behavioral risk factor surveillance system
- CES-D:
-
Center for epidemiologic studies depression
References
RealtyTrac Staff. (2009). 1.9 million foreclosure filings reported on more than 1.5 million US properties in first half of 2009. http://www.realtytrac.com/contentmanagement/pressrelease.aspx?channelid=9&accnt=0&itemid=6802. Accessed October 6, 2009.
Schumer, C. E. (2009). Schumer on record home foreclosures report. http://jec.senate.gov/public/index.cfm?p=PressReleases&ContentRecord_id=5a01bd59-ab4f-3e18-eba8-c1914fb33982&ContentType_id=efc78dac-24b1-4196-a730-d48568b9a5d7&66d767ed-750b-43e8-b8cf-89524ad8a29e&14f995b9-dfa5-407a-9d35-56cc7152a7ed&Group_id=13cba799-f4a9-43ae-be11-76d2994d7042. Accessed October 6, 2009.
Pollack, C. E., & Lynch, J. (2009). Health status of people undergoing foreclosure in the Philadelphia region. American Journal of Public Health, 99, 1833–1839.
Pevalin, D. J. (2009). Housing repossessions, evictions and common mental illness in the UK: Results from a household panel study. Journal of Epidemiology and Community Health, 63(11), 949–951.
Bennett, G. G., Scharoun-Lee, M., Tucker-Seeley, R. (2009). Will the public’s health fall victim to the home foreclosure epidemic? PLoS Medicine, 6(6), e1000087. Epub 2009 Jun 16.
Reisen, W., Takahashi, R., Carroll, B., & Quiring, R. (2008). Delinquent mortgages, neglected swimming pools, and West Nile Virus, California. Emerging Infectious Diseases, 14, 1747–1749.
Riva, M., Gauvin, L., & Barnett, T. A. (2007). Toward the next generation of research into small area effects on health: A synthesis of multilevel investigations published since July 1998. Journal of Epidemiology and Community Health, 61(10), 853–861.
Idler, E. L., & Angel, R. J. (1990). Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. American Journal of Public Health, 80(4), 446–452.
Idler, E. L., & Benyamini, Y. (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38(1), 21–37.
Idler, E. L., Russell, L. B., & Davis, D. (2000). Survival, functional limitations, and self-rated health in the NHANES I epidemiologic follow-up study, 1992. American Journal of Epidemiology, 152(9), 874–883.
Hennessy, C. H., Moriarty, D. G., Zack, M. M., Scherr, P. A., & Brackbill, R. (1994). Measuring health-related quality of life for public health surveillance. Public Health Reports, 109(5), 665–672.
Andresen, E. M., Catlin, T. K., Wyrwich, K. W., & Jackson-Thompson, J. (2003). Retest reliability of surveillance questions on health related quality of life. Journal of Epidemiology and Community Health, 57(5), 339–343.
Moriarty, D., Zack, M., & Kobau, R. (2003). The Centers for Disease Control and Prevention’s Healthy Days measures—Population tracking of perceived physical and mental health over time. Health and Quality of Life Outcomes, 1(1), 37.
Power, C., Matthews, S., & Manor, O. (1996). Inequalities in self rated health in the 1958 birth cohort: Lifetime social circumstances or social mobility? British Medical Journal, 313(7055), 449–453.
Shetterly, S. M., Baxter, J., Mason, L. D., & Hamman, R. F. (1996). Self-rated health among hispanic vs non-hispanic white adults: The San Luis Valley Health and Aging Study. American Journal of Public Health, 86(12), 1798–1801.
Finch, B. K., Hummer, R. A., Reindl, M., & Vega, W. A. (2002). Validity of self-rated health among Latino(a)s. American Journal of Epidemiology, 155(8), 755–759.
US Department of Housing and Urban Development. (2010). Neighborhood stabilization program data. HUD provided local level data. http://www.huduser.org/portal/datasets/nsp_foreclosure_data.html. Accessed May 5, 2010.
Franzini, L., Caughy, M., Spears, W., & Eugenia Fernandez Esquer, M. (2005). Neighborhood economic conditions, social processes, and self-rated health in low-income neighborhoods in Texas: A multilevel latent variables model. Social Science and Medicine, 61(6), 1135–1150.
USDA Economic Research Service. (2010). Measuring rurality: Rural-urban commuting area codes. http://www.ers.usda.gov/briefing/rurality/ruralurbancommutingareas/. Accessed May 5, 2010.
Castellino, S. M., Casillas, J., Hudson, M. M., Mertens, A. C., Whitton, J., Brooks, S. L., et al. (2005). Minority adult survivors of childhood cancer: A comparison of long-term outcomes, health care utilization, and health-related behaviors from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 23(27), 6499–6507.
Ross, C., & Mirowsky, J. (1999). Disorder and decay. The concept and measurement of perceived neighborhood disorder. Urban Affairs Review, 34, 412–432.
Sampson, R. J., Raudenbush, S. W., & Earls, F. (1997). Neighborhoods and violent crime, a multilevel study of collective efficacy. Science, 277, 918–924.
Ross, C., Reynolds, J., & Geis, K. (2000). The contingent meaning of neighborhood stability for residents’ psychological well-being. American Sociological Review, 65, 581–597.
Krieger, N., Chen, J., Waterman, P., Soobader, M., Subramanian, S., & Carson, R. (2002). Geocoding and monitoring of socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? American Journal of Epidemiology, 156, 471–482.
Sherbourne, C., & Stewart, A. (1991). The MOS social support survey. Social Science and Medicine, 32, 705–714.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health Social Behavior, 24(4), 385–396.
McHorney, C. A., & Lerner, J. (1991). The 1990 NORC National Health Survey: Documentation and codebook. Chicago: National Opinion Research Council.
Kohout, F. J., Berkman, L. F., Evans, D. A., & Cornoni-Huntley, J. (1993). Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. Journal on Aging and Health, 5(2), 179–193.
Katz, J. N., Chang, L. C., Sangha, O., Fossel, A. H., & Bates, D. W. (1996). Can comorbidity be measured by questionnaire rather than medical record review? Medical Care, 34(1), 73–84.
Schag, C. A., Ganz, P. A., Polinsky, M. L., Fred, C., Hirji, K., & Petersen, L. (1993). Characteristics of women at risk for psychosocial distress in the year after breast cancer. Journal of Clinical Oncology, 11, 783–793.
Schootman, M., Jeffe, D., West, M., & Aft, R. L. (2005). Comparison of self-reported breast cancer treatment and medical records among older women. Journal of Clinical Epidemiology, 58, 1316–1319.
Wolinsky, F. D., Andresen, E. M., Malmstrom, T. K., Schootman, M., Miller, J. P., & Miller, D. K. (2009). Three-year measured weight change in the African American Health Study. Journal of Aging and Health, 21(2), 231–243.
D’Agostino, R. B., Jr. (1998). Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine, 17(19), 2265–2281.
Rosenbaum, P. R., & Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55.
Rubin, D. B. (1979). Using multivariate matched sampling and regression adjustment to control bias in observational studies. Journal of the American Statistical Association, 74(366), 318–328.
Schuetz, J., Been, V., & Ellen, I. G. (2008). Neighborhood effects of concentrated mortgage foreclosures. Journal of Housing Economics, 17(4), 306–319.
Acknowledgments
This research was supported in part by grants from the National Cancer Institute (CA112159, CA91842). The funders did not have any role in the design of the study; the analysis and interpretation of the data; the decision to submit the manuscript for publication; or the writing of the manuscript. We thank the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, Missouri, for the use of the Health Behavior, Communications, and Outreach Core. We also thank Jeannette Jackson-Thompson and the Missouri Cancer Registry for the identification of eligible women and data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schootman, M., Deshpande, A.D., Pruitt, S.L. et al. Neighborhood foreclosures and self-rated health among breast cancer survivors. Qual Life Res 21, 133–141 (2012). https://doi.org/10.1007/s11136-011-9929-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-011-9929-0