Abstract
Purpose
To review published studies on the effect of diabetes and its complications on utility scores to establish whether there is systematic variation across studies and to examine the implications for the estimation of quality-adjusted life years (QALYs).
Methods
A systematic review was performed using studies reporting QALY measures elicited from people with diabetes including those with a history of complications. Meta-analysis was used to obtain the average utility, and meta-regression was employed to examine the impact of study characteristics and elicitation methods on these values. The effect of different utility scores on QALYs was examined using diabetes simulation models.
Results
In the meta-analysis based on 45 studies reporting 66 values, the average utility score was 0.76 (95% CI 0.75–0.77). A meta-regression showed significant variation due to age, method of elicitation and the proportion of males. The average utility score for individual complications ranged from 0.48 (95% CI 0.25, 0.71) for chronic renal disease to 0.75 (95% CI 0.73, 0.78) for myocardial infarction, and these differences produced meaningful changes in simulated QALYs. There was significant heterogeneity between studies.
Conclusions
We provide summary utility scores for diabetes and its major complications that could help inform economic evaluation and policy analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality-adjusted life years (QALYs) are a commonly used outcome measure in economic evaluations of interventions to manage diabetes and its complications. The weights used to calculate QALYs (often referred to as utility scores) are based on preference-based measures of health-related quality of life (HRQoL). These can be determined directly from patients through techniques such as the ‘time trade-off’ (TTO) method or indirectly using generic instruments such as the EQ-5D. There are now a substantial number of studies reporting utility scores for people with diabetes and for common complications associated with the disease. Typically, these utilities are used in economic evaluations of interventions for the prevention or management of diabetes and often involve use of either Markov modelling or discrete-time simulation to estimate QALYs with and without the intervention [1–3]. In this context, it is important to consider the appropriateness of values of particular health states when there is often considerable heterogeneity of utility scores reported in the literature.
Currently, most models use utility values from a single study and often use the same source of information for different types of complications. Meta-analysis allows us to systematically synthesise information on quality of life from many different studies. Not only does this facilitate use of summary scores when determining the impact complications can have on quality of life, it also provides a range of values that could be used when testing model sensitivity. Hence, meta-analysis is likely to become integral to diabetes and other health economic modelling in the future.
The main purpose of this study is to undertake a systematic review of preference-based measurements of QoL in patients with diabetes and with common diabetes-related complications (stroke, myocardial infarction, blindness, end stage renal disease (ESRD), amputation and ulcers). Meta-analysis is employed to estimate summary measures of key utilities for people with diabetes. We also examine whether there are systematic differences associated with direct and indirect approaches to measuring utility or between different generic QoL instruments when measuring utility. Using a diabetes simulation model, we examine the degree to which the use of different utility values may impact on lifetime estimates of QALYs. Finally, we investigate the effect different utility values may impact on incremental QALYs gained by simulating a theoretical diabetes therapy.
Methods
Study selection
A literature search was carried out to identify potentially relevant studies reporting utility scores for diabetes and diabetes-related complications (either directly elicited or generated from generic QoL instruments). Databases used in the search included OVID, MEDLINE, EMBASE, CINAHL, PubMed as well as Cochrane’s systematic reviews database. Other databases searched included the Health Technology Assessment website, Health Economic Evaluation Database (HEED), NHS Economic Evaluation Database, the TUFTS CEA register, the Digital Theses Database and Google Scholar. Bibliographies of review articles and articles that reported utility values were also examined, as well as articles which included the reported articles in their citations list. These were examined through Google Scholar and PubMed.
Our review was confined to preference-based measures of HRQoL. These included the index scores from the Euro-Qol (EQ-5D) [4], Health Utilities Index 3 (HUI3) [5] and SF-6D score [6] as well as directly elicited utility values from time trade-off (TTO) or standard gamble (SG) [7] exercises. Inclusion criteria were as follows: articles must be published before the end of 2009 in English in peer reviewed journals. In addition, all study subjects were required to have type 1 or type 2 diabetes and had to be 18 years or older at the time their QoL was elicited. Search terms (detailed in an appendix of ESM) included both keywords relating to major diabetes-related complications and health state valuation keywords.
Abstracts and the full text of all articles were examined with regards to these criteria by two independent reviewers to determine whether they fulfilled the inclusion criteria and the correct estimates were reported. All discrepancies between reviewers were resolved.
Data extraction
Information on mean (standard error) of reported utility scores for diabetes patients and a number of selected health states was extracted from each study. These included a history of: (1) myocardial infarction; (2) stroke; (3) ulcer; (4) amputation; (5) diabetic retinopathy or blindness; (6) end stage renal disease; (7) no complications. The following information was also extracted from each study for use in the meta-regression: (1) sample size of the study; (2) mean age of study participants; (3) proportion of males and (4) method of QoL elicitation. If data were not reported on any of these characteristics, studies were excluded from the meta-regression but included in the meta-analysis [8–13]. Studies that did not report a measure of variance around the estimated mean utility value were excluded from both the meta-analysis and meta-regression.
Meta-analysis and meta-regression
Meta-analysis was used to combine the results of multiple studies into a single overall value often termed the effect size for each health state. We performed random effects meta-analyses using the metan command in STATA [14]. Meta-analyses were conducted for seven health states listed above as well as an overall analysis for the presence of diabetes (categorised as general diabetes). For the seven health states, we ignored potential within-study correlation in estimates because of the small numbers of studies and estimates (fewer than 10 studies and estimates in each case). However, for the meta-analysis of general diabetes patients, we conducted an additional analysis to account for potential within-study variability using the methods described in Hedges et al. [15] implemented using STATA. Since this method requires specifying the correlation between estimates within-studies, we conducted a sensitivity analysis by varying this correlation from 0 to 0.9 in increments of 0.1.
For patients with diabetes, a random effects meta-regression model was used to examine heterogeneity of utility values across study characteristics. We conducted two analyses: the first used standard meta-regression methods in STATA (through the metareg command) and the second used the methods described in Hedges et al. [15]. Again, we conducted a sensitivity analysis by varying this correlation from 0 to 0.9 in increments of 0.1. Meta-regression allowed for pooling of utility scores while simultaneously accounting for variation in study methods [16]. Studies determining separate QoL measures pertaining to different patient groups, e.g., trial based studies that reported separate outcomes for treatment and control groups [17–23], or studies that compared different populations [24–32] were included as separate observations in the meta-analysis and the meta-regression (provided they included study characteristics of the different population groups). In the meta-regression, the utility value was the dependent variable. Study characteristics hypothesised to be associated with the treatment effect [14] were as follows:
-
Number of participants in the study;
-
Average age of the sample respondents;
-
Proportion of males;
-
Method of QoL elicitation using the following categories (i) TTO & SG; (ii) SF-6D and HUI-3 scores; EQ-5D as the reference;
Simulations using reported utility estimates
Using an existing diabetes simulation model, the UKPDS Outcomes Model [1], we investigated the impact on lifetime QALYs of using different utility values as determined in the meta-analysis. The input population for the model simulations was a cohort of 10,000 identical patients (to reduce Monte Carlo error), aged 65, male, non-smoking and with mean clinical risk factors as determined from a recent large diabetes study [32]. To estimate the base case for all comparisons, patients were run through the simulations in annual cycles for a period of 35 years, and QALYs were determined using mean values of utility for each state, presented in Table 1. If a patient experienced multiple complications during the simulation, the utility score was set to the lowest value of all the health states they had previously experienced.
We then investigated by simulating the impact of using minimum and maximum reported utility scores for each of the following states both separately and then combined: no complications; myocardial infarction, stroke, amputation, blindness and end stage renal disease. We report the results as the difference in QALYs compared to the base model.
Secondly, we investigated the impact on calculated QALYs of using maximum and minimum reported utilities for particular patient groups with each complication. For these simulations, the input dataset was changed to represent a cohort of patients who had all experienced one of the complications. The effect of maximum and minimum reported utility scores on QALYs was determined by simulation, and the results were presented as differences in QALYs compared to the reference case, using mean utility scores.
Lastly, we investigate how choice of utility may impact on incremental QALYs gained as the result of an intervention. For this application, we simulate a theoretical diabetes therapy by reducing initial Hba1c by 1% of the mean level [32] and maintaining this level of Hba1c throughout the patients’ lifetime. Incremental QALYs for the intervention are estimated using three sets of utility scores: the baseline set of utility scores, the maximum and minimum utility score sets across all states.
Results
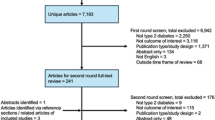
Figure 1 reports a flow chart of the literature search. Our initial search identified 9,492 studies with which 9,191 were excluded after an examination of the abstract. The full text of 301 studies was retrieved for further review. From the 301 studies, 126 were duplicates (studies which appeared more than once in our search results), 50 were eliminated as they reported HRQoL scores from another primary source, 26 were removed because they used measures that did not meet the inclusion criterion and a further 23 studies were eliminated because they did not report sufficient information about the utility scores of the outcomes of interest. Of the 76 studies left, 30 did not report a measure of variance around the reported utility to be included in the meta-analysis or reported other statistics such as median utility values [33]. One further study was omitted [34] from our analysis due to the standard deviation being implausibly high. The final meta-analysis for general diabetes used 45 studies and 66 observations, and the meta-regression was based on 40 studies and 59 observations.
A full listing of the studies used in the meta-analysis of overall utility score for people with diabetes is reported in Table A in the appendix of ESM. In regard to elicitation methods, 33 studies used the EQ-5D; 8 used the HUI 3 or SF-6D each; 15 studies used TTO and 2 used SG. For the meta-regression, which involved only studies reporting patient and study characteristics, the number of respondents ranged from 22 to 7348 with an average of 806. Using a weighted (by sample size) average, there were 52.7% men (range 25–99%) and the weighted average age of patients was 62.6 years (range 37–77 years).
In regard to reporting utility values for studies of patients with a history of complications (see Table B in the appendix of ESM), the number of studies ranged from 4 for ESRD to 6 for blindness, with 5 studies for myocardial infarction, stroke, ulcer and amputation. The average number of respondents per study ranged from 128 (for myocardial infarction) to 284 for stroke and blindness. In addition, seven studies with an average of 578 respondents indicated that the patient had no history of complications.
Summary information for studies reporting utility values for the seven diabetes complications and for no history of complications are presented in Table 1. There was considerable heterogeneity in the number of patients in each study and the utility values presented. Overall, the EQ-5D was the most frequent method of eliciting preference-based measures of HRQoL.
Figure 2 reports 66 utility scores for diabetic patients in 45 studies, ordered by date of publication [8–13], [17–32], [35–58]. The QoL scores ranged from 0.53 [24] to 0.88 [41], with an inter-quartile range of 0.71–0.9. The mean utility value from the random effects meta-analysis was 0.76 (95% confidence interval 0.75–0.78). There was considerable heterogeneity in the utility values (I2 = 98.4%; Q = 4157.9, degrees of freedom = 65, P < 0.001; between-study estimate of variability = 0.003).
We used a within-study correlation of 0.8 in our models, because the sensitivity analysis showed little difference across the range of values from 0.1 to 0.9. Accounting for within-study correlation, the overall utility value was 0.76 (95% confidence interval 0.74–0.79).
The results of the meta-regression to examine heterogeneity in the 41 studies reporting overall measure of utility for people with diabetes are reported in Table 2. By way of interpretation for every 10 year increase in the average age of participants, the average utility score declined by 0.06 points. For every 10% increase in the proportion of males, the average utility score increased by 0.01. In regard to method of elicitation, the mean utility for studies that used TTO/SG was 0.07 higher than for studies that used the EQ-5D, and studies that used other generic methods such as the HUI and SF-6D produced lower mean utility scores than the EQ-5D by 0.08. The estimate of between-study variability was 0.003.
The estimates from accounting for within-study correlation were similar to those from the standard meta-regression (see Table C in appendix of ESM). Without accounting for within-study correlation, average utility score decreased by 0.05 points for every 10 year increase in the average age of participants; for every 10% increase in the proportion of males, average utility increased by 0.01; studies that used TTO/SG as their method of elicitation produced a higher utility score by 0.07 when compared to the EQ-5D, and studies that used HUI/SF-6D had lower utility scores than EQ-5D studies by 0.08 points.
The variation in estimated QALYs as a result of using maximum and minimum reported utility values are presented in Fig. 3. These values refer to a representative 65-year-old male diabetes patient who initially does not have any complications. Changing individual utility scores of selected complications resulted in a change in simulated outcomes of between −0.04 and 0.24 QALYs. However, changes to the no complications state produced larger changes of around ± 1 QALY. Setting the utility scores for all states to their maximum or all states to their minimum values produced changes of +1.06 and −1.11 QALYs respectively.
Table 3 shows the variation in outcomes derived from a simulation model when all patients start with a pre-specified complication. Differences in life expectancy when using the maximum and minimum reported utility scores for the complication ranged from 0.78 QALYs (myocardial infarction) to 5.16 QALYs (stroke). Outcomes are subject to much greater variations as all patients in the simulation are affected by the utility scores. Stroke (whose utility scores ranged from 0.31 to 0.79) produced the largest variation in predicted QALYs ranging from 3.56 to 8.72. In comparison, diabetes patients with myocardial infarction (utility range 0.68–0.77) predicted QALYs ranging from 6.49 to 7.27.
The prediction of incremental undiscounted QALYs gained as a result of a hypothetical intervention that reduced HbA1c (glycosylated haemoglobin) by 1% point produced relatively small effects when comparing the use of mean, maximum or minimum reported utility values (Mean of 0.31 (range 0.30–0.32). This is reported in the appendix (Table C) of ESM.
Discussion
This systematic review has shown that there is a wide range of utility values of diabetic patients for both overall HRQol and for some major complications. The meta-analysis results suggested a high degree of heterogeneity in reported utility values, and the meta-regression results indicate that this is in part due to variations in average patient characteristics such as age, the proportion of males and the methods used for eliciting QoL values. In this meta-analysis (having accounted for within-study correlation), the overall average utility for people with diabetes was 0.76 (0.75, 0.77) and the average values for individual health states ranged from 0.81 for diabetic patients with no complications to 0.48 for patients with ESRD.
This study builds on some recent reviews of QoL for people with diabetes. Mills et al. [59] and Imayama [60] both conducted a systematic literature review of utility scores for patients with diabetes mellitus, whilst Cochran’s [61] meta-analysis was based upon the QoL outcomes for diabetes patients following self-management training. However, these prior studies involved many non-preference-based QoL scores and are therefore less relevant to health economists. Also, this is the first analysis we are aware of to specifically focus on summary scores for a range of diabetes complications in addition to overall QoL of people with diabetes.
The meta-regression results indicated that heterogeneity of utility scores between studies was partly due to age, proportion of males in the study and elicitation method. Due to the lack of patient characteristics reported by studies, some factors, which have been shown to be associated with health utility in diabetes (type of therapy, duration of diabetes, obesity, co morbidities, etc.), were unable to be included. These characteristics potentially can affect utility scores and studies need to consistently report these about their respective populations. The meta-regression results were similar to the EQ-5D population norms in the UK and in the USA [62, 63]; in that lower utility values are associated with older populations and for populations with a higher proportion of women. Similarly, the utility scores obtained from TTO/SG methods were greater than the scores obtained from HUI3/SF-6D scores [16] and larger than EQ-5D scores [64, 65].
There have been reported analyses of the utility scores from the general population associated with some of the events examined in this study. Tengs & Lin’s [16] QoL meta-analysis score for a moderate stroke was 0.68, whilst Leungo–Fernandez [65] found a moderate stroke score to be 0.63. In comparison, our study did not classify the severity of stroke but scored a slightly lower score of 0.59. Liem et al.’s [66] QoL estimate (TTO studies only) for patients undertaking peritoneal dialysis of 0.50 compared to our ESRD estimate of 0.48. The summary scores reported here appear generally lower than those based on the general population, which raises the important question as to whether diabetes actually has an additional impact on QoL. This is an important area for further research.
In regard to the use of these values in simulation models, the range in reported utility values do generate differences in QALYs, but the simulated range is generally less than one year for people who initially do not have any diabetic complications. The variation is much greater for patients with a prior history of these complications. For example, using the mean summary scores obtained from the meta-analysis, a 65-year-old male patient with stroke could expect a quality-adjusted life expectancy of 6.71 QALYs. However, if the maximum reported value from the literature was used, the expected QALYs would increase by 2.01 years, and if the minimum reported value was used, it would decrease by 3.15 years. Approximately 50% variation in remaining lifetime QALYs. Despite the high variation in lifetime QALYs obtained by using different sets of utility values, the incremental QALYs gained as a result of a theoretical therapy to reduce Hba1c only had slight variation regardless of which utility scores were used. This suggests the variation in utility values may have less of an impact on evaluative studies measuring incremental effects than studies looking into the burden of disease.
A motivation for this study has been the lack of reference values of utilities for diabetes and complications of diabetes that are used in economic evaluations of diabetes prevention and management. Cost-utility analyses may take the form of spreadsheet calculations, Markov modelling or more complex computer simulation modelling, but currently there seems to be no clear procedure by which to determine the most appropriate utility values to use in an analysis. In this context, an advantage of undertaking a meta-analysis is that it provides both an average value as well as extreme values that could be used in a sensitivity analysis. Such an approach could improve the comparability of models, as well as eliminate the possibility that a particular utility value has been chosen to produce a desired outcome. By providing a range of values alongside the summary utility scores, this could be useful in helping inform outcomes used in economic evaluations and policy analysis. This is particularly important in the field of diabetes as there is considerable heterogeneity in the utility values between studies. The greater use of meta-analysis of HRQoL outcomes would seem particularly important when they are used to help inform economic evaluations for re-imbursement decisions of new diabetes therapies and technologies (such as by NICE [67] and PBAC [68]).
In conclusion, this study represents one of the first meta-analyses of preference-based outcomes for diabetes patients and diabetic complications. There was a large range of utility values for diabetes patients, and its complications found in the literature search due in part to the average age, proportion of males in the study and the elicitation method. These can produce substantial differences in QALYs estimates for people with diabetes, particularly those experiencing major complications. However, our results of testing a hypothetical new diabetes therapy showed that the heterogeneity of utility values had a lesser impact on the incremental QALYs gained for a new diabetes therapy or intervention.
References
Clarke, P. M., Gray, A. M., Briggs, A., et al. (2004). A model to estimate the lifetime health outcomes of patients with Type 2 diabetes: the United Kingdom prospective diabetes study (UKPDS 68) Outcomes Model. Diabetologia, 47, 1747–1759.
Palmer, A. J., Roze, S., Valentine, W. J., et al. (2004). The CORE diabetes model: Projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (Type 1 and 2) to support clinical and reimbursement decision-making. Current Medical Research and Opinion, 20(Suppl), S5–S26.
Herman, W. H., Hoerger, T. J., Brandle, M., Hicks, K., Sorensen, S., Zhang, P., et al. (2005). Diabetes Prevention Program Research Group. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Annals of Internal Medicine, 142(5), 323–332.
EuroQol Group. (1990). EuroQol–a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Horsman, J., Furlong, W., Feeny, D., & Torrance, G. (2003). The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health and Quality of Life Outcomes, 1, 54.
Walters, S. J., & Brazier, J. E. (2003). What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health and Quality of Life Outcomes, 1, 4.
Torrance, G. W. (1986). Measurement of health state utilities for economic appraisal: A review. Journal of Health Economics, 5(1), 1–30.
Bharmal, M., & Thomas, J. (2006). Comparing the EQ-5D and the SF-6D Descriptive Systems to assess their ceiling effects in the US general population. Value in Health, 9(4), 262–271.
Barnett, T. E., Chumbler, N. R., Vogel, B. W., Beyth, R. J., Ryan, P., & Figueroa, S. (2007). The cost-utility of a car coordination/home telehealth programme for veterans with diabetes. Journal of Telemedicine and Telecare, 13(6), 318–321.
Douzdjian, V. (1998). Treatment strategies for insulin-dependent diabetics with ESRD: a cost-effectiveness. American Journal of Kidney Diseases, 31(5), 794–802.
Barofsky, I., Erickson, P., & Eberhardt, M. (2004). Comparison of a single global item and an index of a multi-item health status measure among persons with and without Diabetes in the US. Quality of Life Research, 13(10), 1671–1681.
Chancellor, J., Aballea, S., Lawrence, A., Sheldon, R., Cure, S., Plun-Favreau, J., et al. (2008). Preferences of patients with diabetes mellitus for inhaled versus injectable insulin regimens. Pharmacoeconomics, 26(3), 217–234.
Maddigan, S. L., Feeny, D. G., & Johnson, J. A. (2005). Health-related quality of life deficits associated with diabetes and comorbidities in a Canadian national population health survey. Quality of Life Research, 14(5), 1311–1320.
Sterne, J. A. C., Bradburn M. J., & Egger M. (2001) Meta-analysis in Stata. (Chapter 18) Resource document. Blackwell Publishing.
Hedges, L. V., Tipton, E., & Johnson, M. C. (2010). Robust variance estimation in meta-regression with dependent effect size estimates. Research Synthesis Methods, 1(1), 39–65.
Tengs, T. O., & Lin, T. H. (2003). A Meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics, 21(3), 191–200.
Maddigan, S. L., Feeny, D. H., Johnson, J. A., & Investigators., D. O. V. E. (2004). Construct validity of the RAND-12 and Health Utilities Index Mark 2 and 3 in type 2 diabetes. Quality of Life Research, 13(2), 435–448.
Maddigan, S. L., Majumdar, S. R., Guirguis, L. M., Lewanczuk, R. Z., Lee, T. K., Toth, E. L., et al. (2004). Improvements in patient-reported outcomes associated with an intervention to enhance quality of care for rural patients with type 2 diabetes. Diabetes Care, 27(6), 1306–1312.
Boye, K. S., Matza, L. S., Oglyesby, A., Malley, K., Kim, S., Hayes, R. P. & Brodows, R. (2006). Patient-reported outcomes in a trial of exenatide and insulin glargine for the treatment of type 2 diabetes. Health and Quality of Life Outcomes, October 4, 80.
Currie, C. J., Morgan, C. L., Poole, C. D., Sharplin, P., Lammert, M., & McEwan, P. (2006). Multivariate models of health-related utility and the fear of hypoglycaemia in people with diabetes. Current Medical Research and Opinion, 22(8), 1523–1534.
Huang, E. S., Shook, M., Jin, L., Chin, M. H., & Meltzer, D. O. (2006). The impact of patient preferences on the cost-effectiveness of intensive glucose control in older patients with new-onset diabetes. Diabetes Care, 29(2), 259–264.
Ose, D., Wensing, M., Szecsenyi, J., Joos, S., Hermann, K., & Miksch, A. (2009). Impact of primary care-based disease management on the health-related quality of life in patients with type 2 diabetes and comorbidity. Diabetes Care, 32(9), 1594–1596.
Farmer, A. J., Wade, A. N., French, D. P., Simon, J., Yudkin, P., Gray, A., et al. (2009). Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial. Health Technology Assessment, 13(15), 1–50.
Hammerschmidt, T., Zeitler, H. P., Gulich, M., & Leidl, R. (2004). A comparison of different strategies to collect standard gamble utilities. Medical Decision Making, 24(5), 493–503.
Shah, V. A., Gupta, S. K., Shah, K. V., Vinjamaram, S., & Chalam, K. V. (2004). TTO utility scores measure quality of life in patients with visual morbidity due to diabetic retinopathy or ARMD. Ophthalmic Epidemiology, 11(1), 43–51.
Lundkvist, J., Berne, C., Bolinder, B., & Jönsson, L. (2005). The economic and quality of life impact of hypoglycaemia. European Journal of Health Economics, 6(3), 197–202.
Wee, H. L., Li, S. C., Cheung, Y. B., Fong, K. Y., & Thumboo, J. (2006). The influence of ethnicity on health-related quality of life in diabetes mellitus: a population-based, multiethnic study. Journal of Diabetes and Its Complications, 20(3), 170–178.
Brown, S. E. S., Meltzer, D. O., Chin, M. H., & Huang, E. S. (2008). Perceptions of quality-of-life effects of treatments for diabetes mellitus in vulnerable and nonvulnerable older patients. Journal of the American Geriatrics Society, 56(7), 1183–1190.
Lloyd, A., Nafees, B., Gavriel, S., Rousculp, M. D., Boye, K. S., & Ahmad, A. (2008). Health utility values associated with diabetic retinopathy. Diabetic Medicine, 25(5), 618–624.
Sakthong, P., Charoenvisuthiwongs, R., & Shabunthom, R. (2008). A comparison of EQ-5D index scores using the UK, US and Japan preference weights in a Thai sample with type 2 diabetes. Health and quality of life outcomes, 23(6), 71.
McEwen, L. N., Kim, C., Haan, M. N., Ghosh, D., Lantz, P. M., Thompson, T. J., et al. (2009). Are health-related quality-of-life and self-rated health associated with mortality? Insights from translating research into action for diabetes (TRIAD). Primary Care Diabetes, 3(1), 37–42.
ADVANCE Collaborative Group. (2007). Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet, 370, 829–840.
Wexler, D. J., Grant, R. W., Wittenburg, E., Bosch, J. L., Cagliero, E., Delahanty, L., et al. (2006). Correlates of health-related quality of life in Type 2 diabetes. Diabetologia, 49, 1489–1497.
Levy, A. R., Christensen, T. L., & Johnson, J. A. (2008). Utility values for symptomatic non-severe hypoglycaemia elicited from persons with and without diabetes in Canada and the United Kingdom. Health and Quality of Life Outcomes, 29(6), 73.
Brown, M. M., Brown, G. C., Sharma, S., & Shah, G. (1999). Utility Values and Diabetic Retinopathy. American Journal of Ophthalmology, 128(3), 324–330.
Brown, G. C., Brown, M. M., Sharma, S., Brown, H., Gozum, M., & Denton, P. (2000). Quality of life associated with diabetes mellitus in an adult population. Journal of Diabetes and Its Complications, 14(1), 18–24.
Brown, M. M., Brown, G. C., Sharma, S., Landy, J., & Bakal, J. (2002). Quality of life with visual acuity loss from diabetic retinopathy and age-related macular degeneration. Archives of Ophthalmology, 120(4), 481–484.
Redekop, W. K., Koopmanschap, M. A., Stolk, R. P., Rutten, G. E., Wolffenbuttel, B. H., & Niessen, L. W. (2002). Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care, 25(3), 458–463.
Sullivan, S. D., Lew, D. P., Devine, B. E., Hakim, Z., Reiber, G. E., & Veenstra, D. L. (2002). Health state preference assessment in diabetic peripheral neuropathy. Pharmacoeconomics, 20(15), 1079–1089.
Clarke, P., Gray, A., & Holman, R. (2002). Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Medical Decision Making, 22(4), 340–349.
Hart, H. E., Bilo, H. J. G., Redekop, W. K., Stolk, R. P., Assink, J. H., & Meyboom-de Jong, B. (2003). Quality of life of patients with type 1 diabetes mellitus. Quality of Life Research, 12(8), 1089–1097.
Sharma, S., Oliver-Fernandez, A., Bakal, J., Hollands, H., Brown, G. C., & Brown, M. M. (2003). Utilities associated with diabetic retinopathy: results from a Canadian sample. The British Journal of Ophthalmology, 87(3), 259–261.
Bagust, A., & Beale, S. (2005). Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Economics, 14(3), 217–230.
Wee, H. L., Cheung, Y. B., Li, S. C., Fong, K. Y., & Thumboo, J. (2005). The impact of diabetes mellitus and other chronic medical conditions on health-related quality of life: Is the whole greater than the sum of its parts? Health and Quality of Life Outcomes January, 3, 2.
Clarke, P. M., Simon, J., Cull, C. A., & Holman, R. R. (2006). Assessing the impact of visual acuity on quality of life in individuals with type 2 diabetes using the short form-36. Diabetes Care, 29(7), 1506–1511.
Morgan, C. L., McEwan, P., Morrissey, M., Peters, J. R., Poole, C., & Currie, C. J. (2006). Characterization and comparison of health-related utility in people with diabetes with various single and multiple vascular complications. Diabetic Medicine, 23(10), 1100–1105.
Sakamaki, H., Ikeda, S., Ikegami, N., Uchigata, Y., Iwamoto, Y., Origasa, H., et al. (2006). Measurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value in Health, 9(1), 47–53.
Supina, A. L., Feeny, D. H., Carroll, L. J., & Johnson, J. A. (2006). Misinterpretation with norm-based scoring of health status in adults with type 1 diabetes. Health and Quality of Life Outcomes, 16(4), 15.
Boye, K. S., Yurgin, N., Dilla, T., Cordero, L. A., Badia, X., Suriñach, N. L., et al. (2007). Health-related quality of life of patients with type 2 diabetes mellitus in primary care in Spain: self-reported and proxy assessment using the EQ-5D. Journal of Medical Economics, 10(1), 41–58.
Huang, E. S., Brown, S. E., Ewigman, B. G., Foley, E. C., & Meltzer, D. O. (2007). Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care, 30(10), 2478–2483.
Glasziou, P., Alexander, J., Beller, E., Clarke, P. M., & The ADVANCE Collaborative Group. (2007). Which health-related quality of life score? A comparison of alternative utility measures in patients with type 2 diabetes in the ADVANCE trial. Health and Quality of Life Outcomes, 27(5), 21.
Matza, L. S., Boye, K. S., Yurgin, N., Brewster-Jordan, J., Mannix, S., Shorr, J. M., et al. (2007). Utilities and disutilities for type 2 diabetes treatment-related attributes. Quality of Life Research, 16(7), 1251–1265.
Sullivan, P. W., Ghushchyan, V. H., & Ben-Joseph, R. (2008). The impact of obesity on diabetes, hyperlipidemia and hypertension in the United States. Quality of Life Research, 17(8), 1063–1071.
Vexiau, P., Mavros, P., Krishnarajah, G., Lyu, R., & Yin, D. (2008). Hypoglycaemia in patients with type 2 diabetes treated with a combination of metformin and sulphonylurea therapy in France. Diabetes, obesity and metabolism, 10(Suppl, 1), 16–24.
Arne, M., Janson, C., Janson, S., Boman, G., Lindqvist, U., Berne, C., et al. (2009). Physical activity and quality of life in subjects with chronic disease: Chronic obstructive pulmonary disease compared with rheumatoid arthritis and diabetes mellitus. Scandinavian Journal of Primary Health Care, 27(3), 141–147.
Clarke, P. M., Hayes, A. J., Glasziou, P. G., Scott, R., Simes, J., & Keech, A. C. (2009). Using the EQ-5D index score as a predictor of outcomes in patients with type 2 diabetes. Medical Care, 47(1), 61–68.
Marrett, E., Stargardt, T., Mavros, P., & Alexander, C. M. (2009). Patient-reported outcomes in a survey of patients treated with oral antihyperglycaemic medications: associations with hypoglycaemia and weight gain. Diabetes, obesity and metabolism, 11(12), 1138–1144.
Zhang, X. H., Wee, H. L., Tan, K., Thumboo, J., & Li, S. C. (2009). Is diabetes knowledge associated with health-related quality of life among subjects with diabetes? A preliminary cross-sectional convenience-sampling survey study among English-speaking diabetic subjects in Singapore. Journal of Chinese Clinical medicine, 4(3), 144–150.
Mills, T., Law, S. K., Walt, J., Buchholz, P., & Hansen, J. (2009). Quality of Life in Glaucoma and Three Other Chronic Diseases. Drugs and Aging, 26(11), 933–950.
Imayama, I. (2009). Determinants of quality of life in adults with diabetes. Centre of Health Promotion Studies, School of Public Health. US: DPhil University of Alberta.
Cochran, J., & Conn, V. S. (2008). Meta-analysis of quality of life outcomes following diabetes self-management training. The Diabetes Educator, 34(5), 815–823.
Kind, P., Hardman, G. & Macran Susan. (1999) UK population norms for EQ-5D: Discussion Paper 172 The University of York, Centre for Health Economics.
Fryback, D. G., Dunham, N. C., Palta, M., Hammer, J., Buechner, J., Cherepanov, D., et al. (2007). US Norms for six generic health-related quality of life indexes from the national health measurement study. Medical Care, 45(12), 1162–1170.
Ariza-Ariza, R., Hernandez-Cruz, B., Carmona, L., Ruiz-Montesinos, M. D., Ballina, J., Navarro-Sarabia, F., et al. (2006). Assessing utility values in rheumatoid arthritis: A comparison between time trade off and the EuroQol. Arthritis Care & Research, 55(5), 751–756.
Ramon Luengo-Fernandez. (2009). Resource costs, health outcomes and cost effectiveness in stroke care: Evidence from the Oxford Vascular Study. DPhil, Oxford University, UK.
Liem, Y. S., Bosch, J. L., & Hunink, M. G. (2008). Preference-Based quality of life of patients on renal replacement therapy: A systematic review and meta-analysis. Value in Health, 11(4), 733–741.
National Institute for Clinical Excellence (NICE) (2004), Guide to the methods of technology appraisal, NICE, London.
Commonwealth of Australia. (1995). Guidelines for the pharmaceutical industry on preparation of submissions to the Pharmaceutical Benefits Advisory Committee: including economic analysis. Canberra: Department of Health and Community Services.
Acknowledgments
This report is independent research commissioned by the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. We are grateful to Edmund Fitzgerald and Melanie Wyld for assistance with the literature review. In regard to other funding, AJH received support from an Australian National Health and Medical Research Council (NHMRC) Project Grant 512463; PMC was funded from an Australian NHMRC Career Development Award (571122). AH was funded from the NHMRC Screening a Test Evaluation Program Grant (633003).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lung, T.W.C., Hayes, A.J., Hayen, A. et al. A meta-analysis of health state valuations for people with diabetes: explaining the variation across methods and implications for economic evaluation. Qual Life Res 20, 1669–1678 (2011). https://doi.org/10.1007/s11136-011-9902-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-011-9902-y