Abstract
Purpose
The maintenance of good health-related quality of life (HRQoL) is an important goal for end-stage renal disease (ESRD) patients. Whether hemodialysis (HD) and peritoneal dialysis (PD) have different impacts on HRQoL is a concern shared by both physicians and patients. A comparison study of HRQoL between Taiwanese HD and PD patients was conducted.
Methods
ESRD patients at 14 hospitals or dialysis centers in northern Taiwan were recruited in this cross-sectional study. The Chinese-language version of the 36-item Short Form Health Survey Questionnaire (SF-36, Taiwan Standard Version 1.0) was used to evaluate HRQoL. Ordinal regression analyses were used to explore the independent association between HRQoL scores and dialysis modality. By Bonferroni correction test, a P value of <0.005 was regarded as significant.
Results
A total of 866 HD patients and 301 PD patients were included. After adjusting for confounding factors, no difference in HRQoL was found among the entire cohort and the diabetic subgroup.
Conclusion
This study demonstrated that Taiwanese HD and PD patients had similar HRQoL. The current survey improves our understanding of the association of HRQoL with dialysis modality in Taiwan ESRD population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The maintenance of well-being in health, the so-called good health-related quality of life (HRQoL), is an important treatment goal of end-stage renal disease (ESRD) patients. Dialysis, a long-term and time-consuming treatment, remains the major choice for ESRD patients at present. Physicians and patients are eager to determine whether the dialysis modalities have different impacts on HRQoL. Information about the quality of life of patients undergoing renal replacement therapy is needed to assist physicians, nurses, patients, and their families to make treatment decisions.
Several previous studies comparing HRQoL between hemodialysis (HD) and peritoneal dialysis (PD) patients have conflicting findings [1–4]. In a study of HRQoL, many factors may influence the reported quality of life by investigation subjects [5], such as differences in disease burden, socioeconomic status, family support, social support, and spiritual resources [6]. Hence, regional and national disparities exist in the study of HRQoL. Even ethnic differences in HRQoL have also been demonstrated in the dialysis population [7, 8]. Thus, surveys of HRQoL should be regional and ethnicity specific.
Taiwan is a highly endemic region for end-stage renal disease (ESRD) [9], and dialysis therapy is still the treatment of choice for most patients. The study of impact of different dialysis modalities on long-term clinical results is lacking. Therefore, we conducted cross-sectional study comparing HRQoL between Taiwanese patients undergoing HD and PD. In order to eliminate selection bias based on socioeconomic status, patients from 14 dialysis centers, both in rural and urban districts, were included.
Patients and methods
Subjects
A total of 1,167 patients with ESRD at 14 hospitals or dialysis centers in northern Taiwan were recruited for this cross-sectional study. Inclusion criteria were age more than 18 years, able to complete the questionnaires by themselves, and had received stable dialysis for more than 1 month before this study. Patients who had cognitive impairment, active psychiatric disease, active infection, uncontrolled congestive heart failure (more severe than New York Heart Association functional class II), or acute complications from uremia at the time of study were excluded.
Biochemical and hematologic parameters were obtained within 1 month of the survey. Other clinical variables, including dialysis modalities, body weight, duration on dialysis, primary renal disease, highest education level, marital and employment status were also recorded.
This study was approved by the ethics committee of all 14 hospitals and monitored by the Institutional Review Board of National Taiwan University Hospital.
Questionnaires
After written informed consent was obtained, patients were asked to complete the Chinese-language version 36-item Short Form Health Survey Questionnaire (SF-36, Taiwan Standard Version 1.0) by themselves. The SF-36 is a validated instrument [10], which is commonly used to measure HRQoL in dialysis populations [11, 12]. It includes the following eight domains: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). A total score ranging from 0 to 100 is calculated for each domain. Low scores in the eight domains indicate lower quality-of-life state. These eight scales have been compressed into two primary summary scales: the physical component scale (PCS) and the mental component scale (MCS). The PCS and MCS scores are also converted into a 0- to 100-point scale [13].
Statistics
The Kolmogorov–Smirnov test of normality was used for data distribution analysis. Normally distributed data were presented as mean ± SD and the non-Gaussian data as median (25th, 75th percentile). The Student’s unpaired t-test, non-parametric Mann–Whitney U-test, and chi-square test were used to test differences between two groups of patients. We explored the independent association between HRQoL scores and dialysis modality by two models of ordinal regression analyses. Model 1 included adjustment for age, dialysis vintage, cardiovascular disease, and diabetes. Model 2 included adjustment for all the variables in model 1, plus serum albumin and hematocrit. The scores of eight HRQoL domains were analyzed as ordinal variables and dialysis modality as a categorical variable. In these regression analyses, the PCS and MCS scores were divided to four quartiles and treated as ordinal variables. We also tested for statistical interactions by including cross-product interactions terms as independent variables in the regression models adjusted for age, diabetes, dialysis vintage, cardiovascular disease, serum albumin, and hematocrit. Since multiple testing was accomplished in our analyses, the Bonferroni test, α = 0.05/10 or 0.005, was used to define significance. The Bonferroni test is a more conservative post hoc method for avoiding the phenomenon of mass significance. Accordingly, a P value of <0.005 was regarded as significant, and higher P values were regarded as tendencies. All calculations were performed using a standard statistical package (SPSS 15.0 for Windows; SPSS Inc, Chicago, IL).
Results
Clinical and demographic characteristics
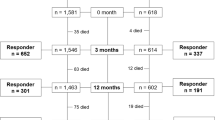
The study cohort was predominantly women (56.9%) with an average age of 55.6 ± 14.0 years. There were 866 HD patients and 301 PD patients. Among the PD patients, 268 patients received continuous ambulatory peritoneal dialysis and 33 patients received automated peritoneal dialysis. The clinical and demographic characteristics of the HD and PD groups are compared in Table 1. Compared with HD patients, PD patients were significantly younger (P < 0.001), had higher education levels (P < 0.001), were less likely to be widowed (P = 0.023), and were more likely to be employed (P < 0.001). A significantly smaller proportion of PD patients had diabetes (P = 0.001), but more PD patients had hypertension (P < 0.001). The HD patient group had a higher prevalence of cardiovascular disease (P < 0.001). Compared to the HD patient group, the PD patient group had lower serum albumin (P < 0.001) and lower hematocrit levels (P = 0.004).
Comparison of SF-36 scores between HD and PD patients
The eight HRQoL domains, PCS, and MCS scores are compared between the HD and PD patient groups in Fig. 1. Compared to the HD patients, PD patients had higher scores in the PF (P = 0.040), VT (P = 0.008), SF (P = 0.012), and MH domain (P = 0.043). No significant difference was found in the scores of the RP, BP, GH, and RE domains. The PCS and MCS scores were higher in the PD patient group, but these differences were not statistically significant.
Independent association between dialysis modality and HRQoL
After adjusting age, diabetes, cardiovascular disease history, and dialysis vintage, the association between dialysis modality and HRQoL presented in the BP domain (P = 0.031), VT domain (P = 0.034), and SF domain (P = 0.044) (Table 2). In the model 2 analysis, although not significantly, the PD patients tended to have higher scores in BP (P = 0.014), VT (P = 0.017), and SF domain (P = 0.009).
Subgroup analysis of differences in HRQoL between HD and PD patients
In the model of regression analyses, only diabetes was found to be significantly interacting with dialysis modality. The HRQoL summary scores between HD and PD patients were not significantly different in diabetic or non-diabetic subgroups by Mann–Whitney U-test (P > 0.100, data not shown). But in the diabetic subgroup, after adjusting age, dialysis vintage, cardiovascular diseases history, albumin, and hematocrit, the scores of BP, VT, and SF domains tended to be higher in the PD patients (P = 0.015, 0.009, and 0.016, respectively) (Table 3). No differences of HRQoL domains were found in subgroup analysis of non-diabetic patients (data not shown).
Discussion
In addition to the first report of a comprehensive survey of HRQoL using the SF-36 questionnaire in Taiwanese HD patients [14], we conducted this first large-scale multi-center survey to compare the HRQoL between Taiwanese HD and PD patients. We demonstrated that no significant difference in HRQoL scores was found in total dialysis population analysis. In the subgroup analysis, diabetic PD patients also had similar HRQoL scores to diabetic HD patients.
Because of no co-payment for PD or HD treatments in the national health insurance system in Taiwan, ESRD patients can decide the modality of dialysis therapy according to their personal preference. Patients and their families make this decision based on consideration of many issues, including co-morbidities, self-care ability, household environment, occupation, social support, family support, and physician preference. Because the assignment of PD and HD could not be randomized in this study, the characteristics of the two patient groups were significantly different. In this study, PD patients were younger, had a lower prevalence of diabetes and cardiovascular diseases, were better educated, were less likely to be widowed, and were more likely to be employed. Similar discrepancies in demographic factors were also found in previous studies [1–4, 15].
After adjustment for possible confounding variables, in a such limited subject number, diabetic PD patients still tended to have higher HRQoL scores in three domains than diabetic HD patients. This result is in conflict with a study by Mau et al. [16] in southern Taiwan. Their HD patients, enrolled in two hemodialysis centers, had higher scores in the social functioning domain. Such discrepancies may be attributable to patient selection bias. Our HD study subjects were older, more likely to be widowed, and had lower educational levels than those in the study of Mau et al. In fact, the average age of the Taiwanese HD population is about 60 [17], but only 53 in the study group of Mau et al. Because this study enrolled a much larger group of patients from 14 dialysis centers, it is likely that there was less patient selection bias.
The exact reason for the association of marginally better HRQoL with PD in diabetic patients could not be clarified in this study. The first possible reason is the different baseline patient characteristics. The high concentrations of glucose in PD dialysate [18, 19] and more peritoneal protein loss [20] may produce unfavorable results to diabetic patients. It retards physicians and diabetic patients to choose PD as dialysis modality. It is likely that some socioeconomic causes make diabetic patients to receive peritoneal dialysis. ESRD patients who had higher socioeconomic status, self-care ability, independence, or even family support tended to select PD as the dialysis modality [21–23]. Because of this selection bias, diabetic PD patients may have higher HRQoL.
The other likely reason is that PD treatment brings better improvement in HRQoL for diabetic ESRD patients. The relative risk of death is associated with the length of dialysis time [24]. Patients’ reported HRQoL is also likely to differ with the length of dialysis time as they experience different treatment loading and complications [4]. Previous longitudinal studies reported that HD patients had more improvement of physical functioning and general health perception in the first year of dialysis [25] and less physical function deterioration in an 18-month follow-up [26]. As our knowledge, there was no report showing better improvement in HRQoL for PD patients. Further longitudinal study in Taiwan dialysis population is needed to clarify this point.
This study still had several limitations. First, it was a cross-sectional observational study. We did not exclude differences in QOL before dialysis [27]. A randomized study is a better design but very difficult to perform [28]. Observational studies still remain the major methods to compare the outcomes between PD and HD patients. Second, this study included all prevalent ESRD patients. Time-dependent HRQoL changes in HD and PD patients still cannot be clarified by this study. Further longitudinal comparison study using an incident dialysis cohort is needed. Third, we did not record the symptom stress scale, co-morbid disease severity and numbers, all of which have a strong impact on HRQoL. These limitations require that our results be interpreted with caution.
HRQoL is an important treatment goal. The current survey improves our understanding of the association of HRQoL with dialysis modality in Taiwan ESRD population. The different dialysis modality is not found to affect HRQoL. Even in diabetic ESRD patients, PD is not found to have negative impact on their HRQoL.
References
Mozes, B., Shabtai, E., & Zucker, D. (1997). Differences in quality of life among patients receiving dialysis replacement therapy at seven medical centers. Journal of Clinical Epidemiology, 50, 1035–1043.
Diaz-Buxo, J. A., Lowrie, E. G., Lew, N. L., Zhang, H., & Lazarus, J. M. (2000). Quality-of-life evaluation using Short Form 36: Comparison in hemodialysis and peritoneal dialysis patients. American Journal of Kidney Diseases, 35, 293–300.
Wasserfallen, J. B., Halabi, G., Saudan, P., Perneger, T., Feldman, H. I., Martin, P. Y., et al. (2004). Quality of life on chronic dialysis: Comparison between haemodialysis and peritoneal dialysis. Nephrology, Dialysis, Transplantation, 19, 1594–1599.
Kutner, N. G., Zhang, R., Barnhart, H., & Collins, A. J. (2005). Health status and quality of life reported by incident patients after 1 year on haemodialysis or peritoneal dialysis. Nephrology, Dialysis, Transplantation, 20, 2159–2167.
Cukor, D., Cohen, S. D., Peterson, R. A., & Kimmel, P. L. (2007). Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. Journal of the American Society of Nephrology, 18, 3042–3055.
Kao, T. W., Chen, P. C., Hsieh, C. J., Chiang, H. W., Tsang, L. Y., Yang, I. F., et al. (2009). Correlations between spiritual beliefs and health-related quality of life of chronic hemodialysis patients in Taiwan. Artificial Organs, 33, 576–579.
Bakewell, A. B., Higgins, R. M., & Edmunds, M. E. (2001). Does ethnicity influence perceived quality of life of patients on dialysis and following renal transplant? Nephrology, Dialysis, Transplantation, 16, 1395–1401.
Unruh, M., Miskulin, D., Yan, G., Hays, R. D., Benz, R., Kusek, J. W., et al. (2004). HEMO Study Group. Racial differences in health-related quality of life among hemodialysis patients. Kidney International, 65, 1482–1491.
U.S. Renal Data System, USRDS 2009 Annual Data Report: Atlas of End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2009.
Yu, J., Coons, S. J., Draugalis, J. R., Ren, X. S., & Hays, R. D. (2003). Equivalence of Chinese and US-English versions of the SF-36 Health Survey. Quality of Life Research, 12, 449–457.
Lowire, E. G., Curtin, R. B., LePain, N., & Schatell, D. (2003). Medical outcomes study short form-36: A consistent and powerful predictor of morbidity and mortality in dialysis patients. American Journal of Kidney Diseases, 41, 1286–1292.
Mapes, D. L., Lopes, A. A., Satayathum, S., McCullough, K. P., Goodkin, D. A., Locatelli, F., et al. (2003). Health-related quality of life as a predictor of mortality and hospitalization: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney International, 64, 339–349.
Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36): Conceptual framework and item selection. Medical Care, 30, 473–483.
Chiang, C. K., Peng, Y. S., Chiang, S. S., Yang, C. S., He, Y. H., Hung, K. Y., et al. (2004). Health-related quality of life of hemodialysis patients in Taiwan: A multicenter study. Blood Purification, 22, 490–498.
Miskulin, D. C., Meyer, K. B., Athienites, N. V., Martin, A. A., Terrin, N., Marsh, J. V., et al. (2002). Comorbidity and other factors associated with modality selection in incident dialysis patients: The CHOICE Study. Choices for Healthy Outcomes in Caring for End-Stage Renal Disease. American Journal of Kidney Diseases, 39, 324–326.
Mau, L. W., Chiu, H. C., Chang, P. Y., Hwang, S. C., & Hwang, S. J. (2008). Health-related quality of life in Taiwanese dialysis patients: Effects of dialysis modality. Kaohsiung Journal of Medical Sciences, 24, 453–460.
The Taiwan National Health Insurance Statistics of Quality in Dialysis Therapy, 2007.
Sitter, T., & Sauter, M. (2005). Impact of glucose in peritoneal dialysis: Saint or sinner? Peritoneal Dialysis International, 25, 415–425.
Wu, H. Y., Hung, K. Y., Huang, J. W., Chen, Y. M., Tsai, T. J., & Wu, K. D. (2008). Initial glucose load predicts technique survival in patients on chronic peritoneal dialysis. American Journal of Nephrology, 28, 765–771.
Nakamoto, H., Imai, H., Kawanishi, H., Nakamoto, M., Minakuchi, J., Kumon, S., et al. (2002). Effect of diabetes on peritoneal function assessed by personal dialysis capacity test in patients undergoing CAPD. American Journal of Kidney Diseases, 40, 1045–1054.
Caskey, F. J., Roderick, P., Steenkamp, R., Nitsch, D., Thomas, K., Ansell, D., et al. (2006). Social deprivation and survival on renal replacement therapy in England and Wales. Kidney International, 70, 2134–2140.
Lo, W. K., Li, F. K., Choy, C. B., Cheng, S. W., Chu, W. L., Ng, S. Y., et al. (2001). A retrospective survey of attitudes toward acceptance of peritoneal dialysis in Chinese end-stage renal failure patients in Hong Kong—From a cultural point of view. Peritoneal Dialysis International, 21(suppl 3), S318–S321.
Verger, C., Duman, M., Durand, P. Y., Veniez, G., Fabre, E., & Ryckelynck, J. P. (2007). Influence of autonomy and type of home assistance on the prevention of peritonitis in assisted automated peritoneal dialysis patients. An analysis of data from the French Language Peritoneal Dialysis Registry. Nephrology, Dialysis, Transplantation, 22, 1218–1223.
Vonesh, E. F., Snyder, J. J., Foley, R. N., & Collins, A. J. (2004). The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney International, 66, 2389–2401.
Wu, A. W., Fink, N. E., Marsh-Manzi, J. V., Meyer, K. B., Finkelstein, F. O., Chapman, M. M., et al. (2004). Changes in quality of life during hemodialysis and peritoneal dialysis treatment: Generic and disease specific measures. Journal of the American Society of Nephrology, 15, 743–753.
Merkus, M. P., Jager, K. J., Dekker, F. W., De Haan, R. J., Boeschoten, E. W., & Krediet, R. T. (1999). Quality of life over time in dialysis: The Netherlands Cooperative Study on the Adequacy of Dialysis. NECOSAD study group. Kidney International, 56, 720–728.
Korevaar, J. C., Jansen, M. A., Merkus, M. P., Dekker, F. W., Boeschoten, E. W., & Krediet, R. T. (2000). Quality of life in predialysis end-stage renal disease patients at the initiation of dialysis therapy. The NECOSAD Study Group. Peritoneal Dialysis International, 20, 69–75.
Korevaar, J. C., Feith, G. W., Dekker, F. W., van Manen, J. G., Boeschoten, E. W., Bossuyt, P. M., et al. (2003). NECOSAD Study Group Study Group. Effect of starting with hemodialysis compared with peritoneal dialysis in patients new on dialysis treatment: A randomized controlled trial. Kidney International, 64, 2222–2228.
Acknowledgments
The authors would like to thank the Ta-Tung Kidney Foundation and the Mrs. Hsiu-Chin Lee Kidney Research Fund for grant support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peng, YS., Chiang, CK., Hung, KY. et al. Comparison of self-reported health-related quality of life between Taiwan hemodialysis and peritoneal dialysis patients: a multi-center collaborative study. Qual Life Res 20, 399–405 (2011). https://doi.org/10.1007/s11136-010-9755-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-010-9755-9