Abstract
Purpose
The aim of the study was to further validate the Assessment of Quality of life at the End of Life (AQEL) questionnaire, to explore whether conceptually consistent scales could be confirmed and how the instrument relates to other widely used and validated HRQL instruments.
Methods
A total of 106 patients with lung cancer in palliative care completed the 20-item AQEL, the EORTC QLQ-C30, Hospital Anxiety and Depression Scale (HADS), Sense of Coherence (SOC-13) and Social Support Survey (SSS). Construct validity of the AQEL was tested by multitrait scaling, principal components analysis, inter-scale correlations and known-groups comparisons.
Results
Five scales were supported by multitrait scaling: Basic function, Activity, Emotional function, Cognitive function and Existential needs, with satisfactory (>.7) internal consistency for the latter three and intermediate (>.5) for the remaining two. A Social support scale was supported by principal components analysis, but exhibited a low internal consistency. Items on health care issues and physical symptoms worked best as individual items. Expected correlations with other instruments were found for all scales. Activity was sensitive to different levels of functioning as defined by performance status.
Conclusions
This study provided some evidence for the validity of the AQEL and its feasibility in patients with cancer in palliative care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The care of patients with end-stage cancer is directed to be palliative, with management of symptoms and maintenance of quality of life as integral parts of care [1] Quality of life (QoL) is a multidimensional evaluation of an individual’s life circumstances [2] and has been defined as “a personal sense of well-being encompassing physical, psychological, social and spiritual dimensions” [3]. Inherent in measures of health-related quality of life (HRQL) are symptoms, functioning and global QoL.
There is a need for careful evaluation of HRQL in palliative research, where standardized questionnaires play an important role. In cancer research, a limited number of multidimensional assessment tools such as the European Organization for Research and Treatment of Cancer (EORTC) Core Quality-of-Life Questionnaire (QLQ-C30) [4] or the Functional Assessment of Cancer Therapy (FACT) [5] have been established. However, there has been less consensus as to which instruments should be recommended in palliative care populations [6, 7]. Except for functioning and symptom control, issues concerning social support, sense of coherence and satisfaction with care have been recognized by both respondents/patients and scientists as important to patients in palliative care [8, 9]. In addition, one needs to consider also the amount of patient burden associated with data collection, and the instruments need to be reasonably brief.
By the time of initiation of the present study, a few other instruments intended for use in palliative care were available, such as The McMaster Quality of Life Scale [10] which is comprehensive but somewhat lengthy (32 items) and the Hospice Quality of Life Index which in its revised form [11] comprises 28 items. Neither of these instruments includes a total quality of life measure and they do not address issues concerning perception of care.
Since the initiation of the present study, a few instruments intended for assessment of QoL in palliative care were developed. In 2006, the EORTC QLQ-C15 PAL was published [8]. Essentially, it is a 15-item short form of the QLQ-C30 and it has been acknowledged that key issues in palliative care patients, such as existential issues, issues related to satisfaction with care and social support are missing [9]. More recently, a validation of the Functional Assessment of Chronic Illness Therapy (FACIT) PAL was published [12]. It is a combined instrument, including the generic FACIT-G questionnaire and a 19-item palliative care subscale, the combined measure comprising 46 items. The FACIT-PAL covers both social and existential dimensions, but does not address issues related to satisfaction with care.
The Assessment of Quality of life at the End of Life (AQEL) questionnaire was developed for use with patients in palliative care in order to combine brevity and usefulness with comprehensiveness. It elucidates the importance of multidimensional assessment of QoL as suggested by the WHO: “Care of the dying extends beyond pain and symptom relief. It also supports the social, psychological and spiritual needs of the patients and their families” [1]. It also comprises items concerning satisfaction with care and global quality of life.
The first validation study of the AQEL was undertaken in a sample of 71 patients with cancer of different sites receiving palliative home care [13]. The patients had a median Karnofsky performance status (KPS) of 70 (range 30–90). Test–retest correlations were between 0.52 and 0.90 with 13 items scoring more than 0.70. The AQEL items were compared with parallel completion of the Cancer Inventory of Problem Situations (CIPS). Correlations between corresponding items within the two questionnaires varied in the range of 0.54–0.81, the only exception being the social items which did not correlate well. The hypothesized dimensionality of the AQEL was not completely supported by factor analysis, and the authors suggested that the AQEL be analysed as either single items, or as a summated scale of all items, until further validation data emerged. The total AQEL score dropped significantly during the last weeks in life suggesting responsiveness to clinical change.
The present study was conducted to further validate the AQEL in a homogenous sample of patients with lung cancer in palliative care, in order to explore whether conceptually consistent scales could be confirmed by multitrait analysis and how the instrument relates to other HRQL instruments. Comparison with the EORTC QLQ-C30, one of the most widely used and well-validated HRQL instruments in cancer research, was deemed as relevant for the future development work with AQEL. To be able to also validate domains not covered by the QLQ-C30 (i.e. social support, existential needs), other domain-specific instruments were included in the analysis.
Methods
Patients
Patients were consecutively recruited among those referred to the Pulmonary Oncology Department at Sahlgrenska University Hospital, Sweden, between May 2003 and February 2005. The inclusion criteria were: a diagnosis of lung cancer, not amenable to curative treatment; not undergoing treatment with life-prolonging intent; ability to speak and read Swedish and oral and written informed consent. Exclusion criterion was: severe mental or cognitive impairment. Palliative chemo- or radiotherapy primarily aimed at alleviating symptoms was permitted. At study entry, the patients completed a battery of questionnaires as described below. The study was approved by the Regional Ethical Review Board in Gothenburg (S112-03).
Assessment of Quality of life at the End of Life (AQEL)
The AQEL questionnaire was developed to assess HRQL in palliative care patients [13]. It covers physical, psychological, social, existential and global aspects of HRQL. The original version comprised of 19 items, but the authors proposed that an item on dyspnea be added, and in the present study the 20-item version was used. All items have a response format of a numeric rating scale ranging from 1 to 10, with extreme values indicated by verbal anchors. Scores were initially calculated by simple summation, where higher scores indicate better functioning or less symptom bother. For the purpose of comparability with the EORTC QLQ-C30 questionnaire, all item and scale scores were linearly transformed to a 0–100 format, where 100 indicates best functioning or, as regards the physical symptom measures, worst symptom bother.
The AQEL has previously been tested in patients with incurable and symptomatic cancer [13] and was used in patients with lung cancer attending a breathlessness clinic [14].
Reference instruments
The EORTC QLQ-C30 is a core HRQL instrument which was developed for use with patients undergoing treatment for cancer [4]. It consists of 30 items measuring physical, role, emotional, cognitive and social functioning in multi-item scales, as well as symptoms commonly reported by patients with cancer, such as fatigue, nausea and vomiting, pain, dyspnea, sleeping problems, appetite loss, constipation and diarrhoea. It also comprises a 2-item scale measuring global QoL. The response format for symptom and function items is categorical, with numbers from 1 to 4 anchored by the verbal categories “not at all”, “a little”, “quite a lot” and “very much”. The global QoL scale is a numeric rating scale ranging from 1 to 7, with extreme values indicated by verbal anchors. In the analysis, all item and scale scores were linearly transformed to a 0–100 format, where 100 indicates best functioning or, as regards the symptom measures, worst-experienced symptoms [15].
The QLQ-C30, usually complemented by one of several available diagnosis-specific questionnaire modules [16], is one of the most frequently used HRQL instruments worldwide in cancer clinical trials [17], but it has also been used in palliative care studies, e.g. in palliative home care [18], and in nurse-led follow up of patients with gastro-intestinal cancer [19]. The validity, reliability and clinical relevance of the Swedish version of the QLQ-C30 have been documented in patients with lung cancer in a palliative setting [20]. Normative and reference data are available [21, 22].
Sense of coherence was measured by the SOC-13 questionnaire [23, 24]. The SOC-13 measures a person’s resources to cope with difficulties in three subscales; comprehensibility, manageability and meaningfulness. Subscale scores may be summated to a total score. The SOC-13 has been widely used in research, e.g. in older patients with cancer [25] and in patients with thyroid cancer [26].
The Social Support Survey (SSS) [27] has previously been used in patients with cancer [28]. It measures the patients’ perceived availability of social support in 20 items. The items are grouped into four subscales measuring emotional/informational support, tangible support, affectionate support and positive social interaction. In the present analysis, only the total score, i.e. the summated score of the four subscales, was used.
The Hospital Anxiety and Depression Scale (HADS) was used to assess emotional distress. It measures depression and anxiety in two separate subscales comprising 7 items each [29, 30]. A Swedish version was developed in 1986 and has been used in patient with various cancers [31–33].
In addition to the patient-rated questionnaires, patients’ performance status was estimated at baseline, using the WHO scale [34], ranging from 0 (no limits to activity) to 4 (unable to perform self-care).
Data analysis
A main purpose of the present study was to investigate and confirm the structure and validity of the AQEL instrument. Items that were considered conceptually related and hypothesized to measure a common HRQL dimension were grouped into multi-item scales. The following scales were hypothesized: Basic function (2 items: hours recumbent during the day; help with hygiene), Activity (2 items: physical strength; ability to do what one wants), Emotional function (3 items: anxiety; insomnia; depression), Cognitive function (2 items: memory; concentration), Social support (2 items: sharing worries with family; regarded as usual by friends), Existential needs (2 items: meaningfulness; make you happy), and Perception of care (2 items: reach staff; receive care), as is also indicated in Table 3. Items concerning physical symptoms, i.e. pain, nausea, bowel function and dyspnoea were used as single items.
The hypothesized multi-item scales of the AQEL were tested for construct validity in two ways. First, a multitrait scaling analysis was applied [35]. In this analysis, each item was expected to correlate stronger with its own hypothesized scale, corrected for overlap, than with the other scales. For convergent validity, a correlation coefficient of at least 0.4 within the scale was required. Discriminant scaling error existed if the correlation of an item with another scale exceeded 1 SE of the correlation with its own hypothesized scale. In all correlation analyses, Pearson’s correlation was used.
Second, a principal component analysis was conducted to explore if the conceptually consistent scales would be reproduced. Varimax rotation with Kaiser normalization was used.
Construct validity was also analysed by multimethod scaling to examine convergence and divergence of the hypothesized scales in the AQEL with other instruments [36]. The physical, emotional and cognitive function measures in the AQEL were hypothesized to correlate best with corresponding measures in the QLQ-C30. In addition, the Emotional function scale was assumed to correlate with the HADS scales. The AQEL Social support scale was supposed to correlate with the SSS total score and with QLQ-C30 social functioning and the Existential needs scale with the SOC meaningfulness subscale scale and summary score.
Clinical validity, as an additional aspect of construct validity, of the AQEL Basic function and Activity scales was analysed by the ability of the AQEL scale to distinguish between groups differing in health status assessed by WHO performance status [37]. Independent t-test was used for significance testing.
Internal consistency, or homogeneity, of hypothesized scales or factors was measured by Cronbach’s alpha coefficient [36, 37].
According to Kline [38], a sample size of 100 is a desirable minimum to conduct a factor analysis. It has also been suggested by Kline that a subjects-to-items ratio of 2:1 may be enough. Therefore, the sample size was determined to 100.
Results
Patient characteristics
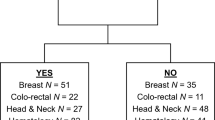
During the data collection period, 151 patients were asked to participate and 106 (70%) accepted. Forty-five patients (22 men and 23 women) declined to participate. The non-participants were slightly older (median age 74; range 58–85) compared with the participants (median age 69; Table 1). Baseline demographic and medical data of the 106 evaluable participants are shown in Table 1. Time since diagnosis varied widely since three of the patients had been diagnosed more than 7 years prior to inclusion. A majority of patients had metastatic disease. The most frequent sites of metastases were the lung, pleura and bone. Most patients only had elementary school education, while 15% had a university education. Sixty-nine per cent were retired. Only two patients were born in non-Scandinavian countries.
Quality of life
Descriptive data from both AQEL and EORTC QLQ-C30 are presented in Table 2. As measured with the AQEL, the mean Basic function score was close to maximum (93.1 on a standardized 0 to 100 scale), indicating that the patients on average experienced very little impact on their ability of self-care. In contrast, the mean Activity score was comparably low, pointing to a more pronounced impact on components of physical functioning that are not primarily related to self-care. The QLQ-C30 Physical functioning scale, which comprises items on both basic functioning and activity, displayed a mean score value in between the two AQEL scales measuring physical function.
Both instruments displayed similar mean score levels with regard to Emotional function, Cognitive function, Social function/support and Global QoL.
Concerning the symptom measures, mean score levels for pain, nausea, bowel problems and insomnia were similar with both measurements, while the reported level of dyspnea was somewhat higher (i.e. more pronounced) with the QLQ-C30 measure.
Multitrait scaling
Results of the multitrait scaling analysis of the AQEL questionnaire is displayed in Table 3. In this analysis, the single item on Global QoL was excluded, since it was assumed to capture multiple dimensions. Items that were assumed to form the scales Basic function, Activity, Emotional function, Cognitive function and Existential needs all correlated at least 0.4 with their own hypothesized scales, corrected for overlap, and no scaling errors were seen with these items. In contrast, the four items that were assumed to measure Social support and Perception of care, respectively, correlated less strongly with their own hypothesized scales, and they all exhibited scaling errors in that they correlated more than 1 SE better with at least one other, conceptually different scale.
Cronbach’s alpha coefficients for the hypothesized scales are presented at the bottom of Table 3. Alpha coefficients exceeding 0.7, which is conventionally considered as a minimum requirement for multi-item scale constructions intended for group comparisons, were seen with Emotional function, Cognitive function and Existential needs. Alpha coefficients for Basic function and Activity were somewhat lower, in the range of 0.55 to 0.58, while alpha coefficients for Social support and Perception of care were quite low. The physical symptom measures Pain, Nausea, Bowel problems and Dyspnea, which were assumed as single item measures, did not correlate above 0.4 with any of the hypothesized multi-item scales.
Principal components analysis
A principal components analysis including all items except the symptom items in the AQEL was performed and resulted in a five-factor solution explaining 65% of the variance (Table 4). Essentially, the factors extracted supported the dimensionality and scale construction based on the multitrait analysis. The first factor was related to Emotional function, including items on anxiety, insomnia and depression. The second factor was related to Basic function, encompassing items on hours recumbent during the day and help with hygiene. However, this factor also comprised the two items assumed to form the Existential needs scale. The third factor was related to Cognitive function and included the items addressing memory and concentration, respectively, but it also captured one item concerned with receiving care. The fourth factor was related to Social support, and included the items on sharing worries with family, being regarded as usual by friends and reaching staff. Finally, a fifth factor related to Activity included items on physical strength and ability to do what one wants.
Cronbach’s alpha coefficients for the factors found in the factor analysis in the present study ranged from 0.43 to 0.76 and is presented in the last row in Table 4.
Multimethod scaling
The hypothesized scales within the AQEL questionnaire were compared with the functioning and global quality of life scales from the QLQ-C30 questionnaire, the two HADS scales on Anxiety and Depression, the SSS total score, the SOC-13 subscales and total score in a correlation matrix (Table 5). For each of the AQEL scales, the correlations that were expected to be strongest are marked with bold lines in the table.
The AQEL Basic function and Activity scales correlated well (r > .50) with the QLQ-C30 Physical functioning measure. In addition, the AQEL Activity scale correlated well with the QLQ-C30 measures of Role and Social functioning and Global QoL.
The AQEL Emotional function scale correlated strongly (r > .70) with the corresponding QLQ-C30 measure and the HADS Anxiety scale, while the correlation with HADS Depression was moderate (>.40), although highly significant. Similarly, the AQEL Cognitive function scale correlated well (r > .05) with the corresponding QLQ-C30 measure.
The Social support scale correlated best, although moderately (r > .40) with the SSS total score, while the correlation with the QLQ-C30 measure of Social functioning was weak (r < .20) and non-significant.
The Existential needs scale correlated well (r > .50) with the SOC-13 subscale of Meaningfulness, but similar magnitudes of correlation were seen also with the QLQ-C30 measures of Emotional functioning and Global Quality of Life, as with the HADS Depression scale.
The AQEL scale Perception of Care was not expected to exhibit strong correlations with any of the other measures, but it correlated best (r > .30) and highly significantly (P < 0.001) with the QLQ-C30 Global Quality of Life and the SOC-13 Meaningfulness measures.
Finally, the AQEL Quality of life scale correlated strongly (r > .70) with the corresponding QLQ-C30 measure, but exhibited substantial correlations also with other measures within the QLQ-C30, HADS and SOC-13 questionnaires.
Correlations between the physical symptom measures in the AQEL and QLQ-C30 questionnaires are shown in Table 6. In general, strong correlations were seen between conceptually related or equivalent measures, while other correlations were of significantly lower magnitude. The AQEL item on bowel problems seemed to measure primarily constipation, while the correlation with diarrhoea was weak.
Clinical validity
Clinical validity of the AQEL physical scales and QoL measure was investigated by comparing mean score values among groups of patients defined by performance status levels (PS 0-1 vs. PS 2-4) (Table 7). For illustration and comparison, the corresponding results with the EORTC QLQ-C30 physical functioning and global QoL scales are included in the table. There were group differences in the expected direction concerning all three AQEL scales, with a more compromised functioning and QoL level among patients with PS 2-4 compared with PS 0-1. However, the differences were small with regard to Basic function and QoL, and it did not reach statistical significance with the Basic function scale.
The group differences in corresponding three QLQ-C30 measures were substantial and highly significant.
Discussion
In the present study, the AQEL instrument was evaluated in patients with lung cancer in palliative care and compared with three other established HRQL instruments. Overall, this study gathered some evidence for the validity of AQEL when used with palliative care patients. The potential advantage of AQEL over disease-specific questionnaires, such as the EORTC QLQ-C30 [4] or its short version QLQ-C15 PAL [8], and even over instruments designed for use with palliative care populations [10–12] is that it combines practicality, due to its relative shortness, with comprehensiveness. The potential disadvantage would be that several of the measures of complex HRQL domains by necessity are brief.
With the aim of enhancing the reliability of complex functioning measures, the scalability of the questionnaire was investigated. Items were grouped into multi-item scales that were assumed to measure a common HRQL domain. Five of the scale constructs, i.e. Basic function, Activity, Emotional function, Cognitive function and Existential needs were supported by the multitrait scaling method. Alpha coefficients of internal consistency of these scale constructs varied between 0.55 and 0.76, with two of the scales (i.e. Basic function and Activity) exhibiting alpha coefficients below 0.7 which is conventionally required for group comparisons. A possible explanation for the comparably low alpha coefficient for Basic function is a low score variance, with a majority of patients scoring high on the function range. The comparably low internal consistency of the Activity scale may be related to diverging focus of the two items, and indicates that further work needs to be done to establish the composition of this measure.
The factor solution in the present study was fairly consistent with the original evaluation [13] although, in the present study, items presumed to measure Basic function and Existential needs loaded on the same factor. The alpha coefficient for this conceptually heterogeneous factor was lower compared with the alpha coefficient for the two-item Existential needs scale as presented in Table 3.
The items assumed to measure Perception of care exhibited scaling errors in the multitrait analysis, and in the factor analysis they were split between two factors, one of which was labelled social support that may conceptually be related to availability of health care. The results suggest that the two items be used and analysed as single-item measures.
One may argue that issues concerning patients’ perception of care should be measured by an instrument focusing on satisfaction with care rather than being incorporated in a HRQL questionnaire. Nevertheless, both items concerned with availability and satisfaction with care, respectively, correlated moderately but statistically highly significant with the QLQ-C30 Global QoL measure, indicating that these issues are indeed components of the HRQL concept. Furthermore, the incorporation of health care–related questions enhances the face validity of the questionnaire to patients in palliative care, who frequently report “iatrogenic distress” as one of the most distressing concerns of their disease [39].
Measures of functional status are included in most HRQL instruments and concerns a person’s ability to perform specific activities [40]. In a study of 231 hospice homecare patients, functional status was the most problematic HRQL domain [41], pointing to the need for appropriate measurements of this domain also in palliative care. The hypothesized Basic function and Activity scales in the AQEL correlated moderately with corresponding measures in the QLQ-C30. The Activity scale was also sensitive to differences in health status as defined by WHO performance status, while the association between Basic function and PS did not reach statistical significance. Since patients with a PS 2 are still able of self-care, a cut off between PS 2 and 3 may have yielded a stronger association, but the group of patients with a PS above 2 in the study sample was small (n = 5).
Anxiety and depression contribute to deteriorated health and cognitive functioning [42], and mental health is a key determinant of QoL [43]. Two scales concerning psychological issues were supported by the analysis, i.e. the Emotional and Cognitive function scales, which is consistent with the scale construct in the QLQ-C30 [4]. The corresponding scales in the two questionnaires correlated well.
The hypothesized two-item Social support scale was not fully supported by the multitrait scaling, but in the principal components analysis both items loaded on the same factor together with the reach staff item, which could also reflect social ability. The scale correlated well with the SSS total score, but not with the Social functioning scale in the QLQ-C30, which is conceptually concerned with social activities rather than with social support.
We found it appropriate to include existential items in a HRQL questionnaire elaborated for palliative care, which is also indicated in the conceptual definitions [2, 3] and in research in palliative care patients [6, 9]. As was hypothesised, the Existential needs scale correlated well with Meaningfulness in SOC-13. The 2-item scale construct was also supported by the multitrait analysis. In the principal components analysis, however, the Existential needs items were grouped together with Basic function items. We have no conceptually valid explanation for this and propose that the two scales be analysed separately.
Conclusion
In summary, the analysis provided some evidence for the validity of the AQEL based on multitrait analysis and its correlation with other conceptually similar measures. Additional work is needed to understand the structure of the measure, as well as its responsiveness to palliative interventions and clinical change in populations of patients with cancer close to the end of their lives.
References
WHO. (2002). National Cancer Control Programmes. Policies and behavioural guidelines. http://www.who.int/cancer/media/en/408.pdf. Accessed January 29 2009.
Haas, B. (1999). A multidisciplinary concept analysis of quality of life. Western Journal of Nursing Research, 21, 728–742.
Ferrel, B. (1996). The quality of lives: 1525 voices of cancer. Oncology Nursing Forum, 23, 909–916.
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organisation for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365–376.
Cella, D., Bonomi, A., Lloyd, S., Tulsky, D., Kaplan, E., & Bonomi, P. (1995). Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer, 12(3), 199–220.
Kaasa, S., & Loge, J. H. (2003). Quality of life in palliative care: principles and practice. Palliative Medicine, 17(1), 11–20.
Ferrell, B. R. (2005). Assessing health-related quality of life at the end of life. In J. Lipscomb, C. C. Gotay, & C. Snyder (Eds.), Outcome assessments in cancer (pp. 264–285). Cambridge: Cambridge University press.
Groenvold, M., Petersen, M. A., Aaronson, N. K., Arraras, J. I., Blazeby, J. M., Bottomley, A., et al. (2006). The development of the EORTC QLQ-C15-PAL: A shortened questionnaire for cancer patients in palliative care. European Journal of Cancer, 42(1), 55–64.
Echteld, M. A., Deliens, L., Onwuteaka-Philipsen, B., Klein, M., & van der Wal, G. (2006). EORTC QLQ-C15-PAL: The new standard in the assessment of health-related quality of life in advanced cancer? Palliative Medicine, 20(1), 1–2.
Sterkenburg, C. A., King, B., & Woodward, C. A. (1996). A reliability and validity study of the McMaster Quality of Life Scale (MQLS) for a palliative population. Journal of Palliative Care, 12(1), 18–25.
McMillan, S. C., & Weitzner, M. (1998). Quality of life in cancer patients: Use of a revised Hospice Index. Cancer Pract, 6(5), 282–288.
Lyons, K. D., Bakitas, M., Hegel, M. T., Hanscom, B., Hull, J., & Ahles, T. A. (2009). Reliability and validity of the Functional Assessment of Chronic Illness Therapy-Palliative care (FACIT-Pal) scale. Journal of Pain and Symptom Management, 37(1), 23–32.
Axelsson, B., & Sjoden, P. O. (1999). Assessment of quality of life in palliative care-psychometric properties of a short questionnaire. Acta Oncologica, 38(2), 229–237.
Hately, J., Laurence, V., Scott, A., Baker, R., & Thomas, P. (2003). Breathlessness clinics within specialist palliative care settings can improve the quality of life and functional capacity of patients with lung cancer. Palliative Medicine, 17(5), 410–417.
Fayers, P., Aaronson, N. K., Bjordal, K., Groenvold, M., Curran, D., Bottomley, A. et al. (2001). The EORTC QLQ-C30 Scoring Manual. http://groups.eortc.be/qol/documentation_manuals.htm Accessed May 5, 2009.
EORTC. The EORTC Quality of Life Group Modules. http://groups.eortc.be/qol/questionnaires_modules.htm. Accessed May 5, 2009.
EORTC. The EORTC Quality of Life Group Bibliography. http://groups.eortc.be/qol/documentation_bibliography.htm. Accessed May 5, 2009.
Ahlner-Elmqvist, M., Jordhoy, M. S., Bjordal, K., Jannert, M., & Kaasa, S. (2008). Characteristics and quality of life of patients who choose home care at the end of life. Journal of Pain and Symptom Management, 36(3), 217–227.
Verschuur, E. M., Steyerberg, E. W., Tilanus, H. W., Polinder, S., Essink-Bot, M. L., Tran, K. T., et al. (2009). Nurse-led follow-up of patients after oesophageal or gastric cardia cancer surgery: A randomised trial. British Journal of Cancer, 100(1), 70–76.
Nicklasson, M., & Bergman, B. (2007). Validity, reliability and clinical relevance of EORTC QLQ-C30 and LC13 in patients with chest malignancies in a palliative setting. Quality of Life Research, 16(6), 1019–1028.
Michelson, H., Bolund, C., Nilsson, B., & Brandberg, Y. (2000). Health-related quality of life measured by the EORTC QLQ-C30–reference values from a large sample of Swedish population. Acta Oncologica, 39(4), 477–484.
EORTC. (2008). The EORTC QLQ-C30 Reference Values Manual. http://groups.eortc.be/qol/downloads/reference_values_manual2008.pdf. Accessed May 5, 2009.
Antonovsky, A. (1993). The structure and properties of the sense of coherence scale. Social Science and Medicine, 36(6), 725–733.
Pallant, J. F., & Lae, L. (2002). Sense of coherence, well-being, coping and personality factors: Further evaluation of the sense of coherence scale. Personality and Individual Differences, 33(1), 134–139.
Thome, B., & Hallberg, I. R. (2004). Quality of life in older people with cancer—a gender perspective. European Journal of Cancer Care, 13(5), 454–463.
Tagay, V. S., Senf, W., Schopper, N., Mewes, R., Bockisch, A., & Gorges, R. (2007). Protective factors for anxiety and depression in thyroid cancer patients. Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie, 53(1), 62–74.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science and Medicine, 32(6), 705–714.
Requena, G. C., Salamero, M., & Gil, F. (2007). Validity of the questionnaire MOS-SSS of social support in neoplastic patients. Medicina Clinica, 128(18), 687–691.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370.
Herrmann, C. (1997). International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. Journal of Psychosomatic Research, 42(1), 17–41.
Bergquist, H., Ruth, M., & Hammerlid, E. (2007). Psychiatric morbidity among patients with cancer of the esophagus or the gastro-esophageal junction: A prospective, longitudinal evaluation. Diseases of the Esophagus, 20, 523–529.
Helgesen, F., Andersson, S. O., Gustafsson, O., Varenhorst, E., Goben, B., Carnock, S., et al. (2000). Follow-up of prostate cancer patients by on-demand contacts with a specialist nurse—A randomized study. Scandinavian Journal of Urology and Nephrology, 34(1), 55–61.
Bergman, B., Sullivan, M., & Sorenson, S. (1991). Quality of life during chemotherapy for small cell lung cancer. I. An evaluation with generic health measures. Acta Oncologica, 30(8), 947–957.
World Health Organization. (1979). WHO handbook for reporting results of cancer treatment (Vol. 48). Geneva: WHO Offset Publication.
Fayers, P., & Machin, D. (2000). Quality of life assessment, analysis and interpretation. New York: John Wiley & Sons Ltd.
Polit, D., & Beck, C. (2004). Nursing research: Principles and methods (7th ed.). London: Lippincott Williams & Wilking.
Burns, N., & Grove, S. (2001). The practice of nursing research. Conduct, critique & utilization (4th ed.). Philadelphia: WB Saunders Company.
Kline, P. (1998). The new psychometrics, science, psychology and measurement. London: Routledge.
Tishelman, C., Lövgren, M., Broberger, E., Hamberg, K., Sprangers, M. Are the most distressing concerns of men and women with inoperable lung cancer adequately assessed? A mixed-methods study. Submitted.
Garman, K. S., & Cohen, H. J. (2002). Functional status and the elderly cancer patient. Critical Reviews in Oncology/hematology, 43(3), 191–208.
McMillan, S. C., & Weitzner, M. (2000). How problematic are various aspects of quality of life in patients with cancer at the end of life? Oncology Nursing Forum, 27(5), 817–823.
Smith, E. M., Gomm, S. A., & Dickens, C. M. (2003). Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliative Medicine, 17(6), 509–513.
Smith, K. W., Avis, N. E., & Assmann, S. F. (1999). Distinguishing between quality of life and health status in quality of life research: A meta-analysis. Quality of Life Research, 8(5), 447–459.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix


Rights and permissions
About this article
Cite this article
Henoch, I., Axelsson, B. & Bergman, B. The Assessment of Quality of life at the End of Life (AQEL) questionnaire: a brief but comprehensive instrument for use in patients with cancer in palliative care. Qual Life Res 19, 739–750 (2010). https://doi.org/10.1007/s11136-010-9623-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-010-9623-7