Abstract
Objective
The impact of irritable bowel syndrome (IBS) on HRQOL has been widely studied in the West. However, there are few data from Asian countries. The aim of this study was to assess the health-related quality of life (HRQOL) of patients suffering from IBS in Korea.
Methods
Consecutive patients from six secondary and six tertiary medical centers in Korea were enrolled and completed self-administered questionnaires on sociodemographics and IBS-associated symptoms. HRQOL was assessed using the generic Short Form 36 (SF-36) and the disease-specific IBS-QOL questionnaires.
Results
Of the 932 patients with abdominal pain and bowel symptoms, 664 IBS patients who fulfilled the Rome II criteria were analyzed. On all eight SF-36 scales, IBS patients had a significantly worse HRQOL than the general population (P < 0.01). The overall score for the IBS-QOL was 74.2. The health concern domain was most affected (mean score 64.2), and the sexual domain (mean score 86.7) was least affected in the IBS-QOL. Significant impairment of HRQOL was only observed in patients with severe symptoms both in the generic and specific HRQOL measurement, whereas patients with mild and moderate symptoms showed only mild impairment (P < 0.01). Female patients reported a significantly lower HRQOL than male patients (P < 0.05), but the difference was minimal. The IBS-QOL was significantly associated with female gender, total symptom score, self-reported symptom severity, and level of education in the multivariate analysis.
Conclusions
IBS-related symptoms had a great effect on the HRQOL of Korean patients. These results and the considerable prevalence of IBS in Korea indicate that IBS has a substantial social impact in this country.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of health-related quality of life (HRQOL) assessments has increased with the concurrent increase in awareness of clinicians and clinical researchers of the impact of functional gastrointestinal (GI) disorders on HRQOL. In addition to physical dimensions, HRQOL assessments encompass emotional and social dimensions [1]. HRQOL assessment is recognized as an important element of clinical and epidemiological research and is useful for understanding the biopsychosocial model of functional GI disorders [2, 3]. The social impact of IBS in Korea has increased because of an increase in its prevalence.
The impact of IBS on HRQOL has been widely studied in the West. The HRQOL of patients with IBS is worse than that of patients with end-stage renal disease, diabetes mellitus, gastroesophageal reflux disease, or asthma [4, 5]. Although the effect of IBS on HRQOL could well differ between the West and East because of genetic, cultural, nutritional, and socioeconomic differences, this aspect has received little attention. It is possible that even when the same criteria are used for IBS diagnosis, the relevance of the domains used in the evaluation of HRQOL may differ between the East and West. Furthermore, there is no information available on factors associated with the HRQOL of IBS patients for the East.
The primary aim of this study was to assess the impact of IBS on HRQOL in Korea. The secondary aim was to identify factors that influence the HRQOL of patients with IBS.
Materials and methods
Subjects
This study involved 12 research institutions (6 secondary and 6 tertiary institutions), which were represented by 12 investigators who were members of the Korean Society of Neurogastroenterology and Motility. Consecutive patients with bowel symptoms were invited to complete questionnaires between May 2005 and April 2006. The following criteria were used to select participants: 18–75 years of age, absence of abnormal colonoscopic examination results, and symptoms consistent with the Rome II criteria [6]. If patients underwent a colonoscopic examination or barium enema at the time of enrollment, we did not repeat the colonoscopic examination. Patients with a history of GI, renal, or gynecological pathology or surgery that could cause IBS-like symptoms were excluded. Men and women who took medication specific for IBS (e.g., antidiarrheal, laxative, or antispasmodic drugs) for 6 months or less before the study were also excluded. Levels of thyroid-stimulating hormone and fasting plasma glucose and other biochemical indices were analyzed to rule out IBS-like symptoms caused by diseases. Eligible participants gave informed consent and provided details of their age, gender, annual income, marital status, and level of education upon entry to the study. The study protocol was approved by the institutional review board of each hospital that participated in this study.
We used data for control subjects from a previous study that assessed chronic GI symptoms and their effects on quality of life in the general population (unpublished data). A cross-sectional survey, using a reliable and valid questionnaire based on Rome II, was performed on randomly selected residents in Asan-si, Chungchungnam-do Province. All respondents were interviewed at their homes or offices by a team of interviewers. The impact of chronic gastrointestinal symptoms on HRQOL was assessed using the Korean version of SF-36.
Procedures
Investigators interviewed the participants and documented the bowel symptom questionnaire on their first visit. If patients fulfilled the criteria for IBS, they were then asked to complete the SF-36 and the IBS-QOL themselves while at the clinic. At the beginning of the study, we enrolled subjects who had experienced IBS symptoms for at least 1 month. However, at a later date, to rule out short-lived functional gastrointestinal disorder, we strictly applied Rome II criteria, which include having experienced IBS symptoms for at least 3 months during the previous 12 months. We only included the patients who fulfilled the Rome II time criteria in the analysis.
Questionnaires
Bowel symptom questionnaire
We used the bowel symptom questionnaire, which, together with the original IBS-QOL questionnaire, was provided by the MAPI Research Institute, a company that deals with linguistic validation. We translated both questionnaires into Korean and back into English to confirm that the translation was appropriate and evaluated their usefulness in a preliminary test using patients with IBS. This test confirmed the discriminant validity of the bowel symptom questionnaire, as was done for the IBS-QOL questionnaire in a previous linguistic validation study [7]. This questionnaire included the Rome II criteria and nine symptoms supportive of IBS diagnosis, viz., abdominal discomfort; pain or cramps; hard or lumpy stools; loose or watery stools; straining during a bowel movement; having to rush to the toilet for a bowel movement; a feeling of incomplete bowel movement; passing mucus (white material) during a bowel movement; abdominal fullness, bloating or swelling; passing gas; heartburn or chest pain; feeling full soon after starting a meal; passing urine frequently; nausea. Patients were classified as having constipation-predominant IBS (C-IBS), diarrhea-predominant IBS (D-IBS), or mixed-type IBS (M-IBS) according to primary bowel patterns [8].
We evaluated the severity of symptoms in two ways. One was a total symptom score, defined as the sum of symptom frequency and bothersomeness. The other was an integrated measure of symptoms such as self-reported symptom severity. A previous validation study showed that these methods are highly correlated [7]. However, the total symptom score has limitations because each symptom is given equal weight. Although a similar method was used in other studies [7, 9], we used self-reported symptom severity in our previous analyses. Therefore, we used self-reported symptom severity for analysis of the data of the present study.
The frequency and bothersomeness of each symptom was assessed. Symptom frequency was assessed using a seven-point response scale (0 = never, 1 = almost never, 2 = seldom, 3 = sometimes, 4 = often, 5 = almost always, 6 = always). Symptom bothersomeness was assessed using similar a seven-point response scale (0 = not bothersome to 6 = extremely bothersome). Total symptom score was defined as the sum of the symptom frequency and bothersomeness scores. The potential range of scores for both symptom frequency and bothersomeness was 0 to 78, and that for total score was 0 to 156. All questions related to the previous 4 weeks.
Self-reported symptom severity was measured using the question “How bad is the discomfort usually?,” where discomfort referred to “pain and associated IBS symptoms.” Responses were rated as mild (“can be ignored if I don’t think about it”), moderate (“cannot be ignored, but does not affect my lifestyle”), or severe (“affects my lifestyle”). To ensure that patients interpreted questions correctly, a table of 13 IBS-specific bowel symptom frequency and bothersomeness categories was shown to the patients before they were supplied with questions on global assessment of symptom severity.
SF-36 questionnaire
Quality of life was evaluated using the Korean version of generic SF-36 questionnaire (version 2). This 36-item questionnaire scores eight domains of patient functioning: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health [10]. Each subscale was scored from 0 to 100; a high score indicated a good health status. All questions related to the previous 4 weeks. Because there is an overall gender bias in SF-36 scores for the normative sample (females score lower than males for HRQOL), we converted our raw scores to z scores, applying general population sample means and standard deviations for males and females separately.
Irritable bowel syndrome quality of life (IBS-QOL) questionnaire
The IBS-QOL questionnaire was developed by Patrick et al. [11]. It consists of 34 IBS-specific QOL items with high internal consistency and reproducibility. Previously, we developed the Korean version of the IBS-QOL using a standard, accepted process, and validated it cross-culturally [7]. It is the only questionnaire that has been validated for use in Korea. Patients were asked to choose between descriptive statements using a recall period of the previous 30 days [11]. A five-point Likert response scale was used to assess the degree to which the statement described the feelings of the respondent (not at all, slightly, moderately, quite a bit, and extremely or a great deal). There were eight subscales: dysphoria (e.g., “I feel vulnerable to other illnesses because of my bowel problems”), interference with activities, body image, health concerns, food avoidance (e.g., “I feel frustrated that I cannot eat when I want to because of my bowel problems”), social reaction, sexual function (“Because of my bowel problems, sexual activity is difficult for me” or “My bowel problems reduce my sexual desire”), and relationships (e.g., “I feel uncomfortable when I talk about my bowel problems”). Each subscale can be transformed to a 0–100 scale, ranging from 0 (poor quality of life) to 100 (maximum quality of life). All items were sum-scored to calculate the overall score, which was transformed to a 0–100 scale. If a patient responded with “not at all” for all 34 items, the overall score of IBS-QOL would be 100. If a patient responded with “slightly,” a score of 4, for all items, the overall IBS-QOL score would be 80. Therefore, if a score was more than 80, the item or domain was not considered to be associated with bowel problems. Moderate to severe IBS corresponds to an IBS-QOL score of 60–65 [12].
Data analysis
Continuous data are presented as the mean ± standard deviation, and categorical data are presented as quantities and proportions. Univariate analyses were conducted to compare demographic profiles within IBS subtypes. For categorical data, group differences were tested using the chi-square test. Analysis of variance (ANOVA) and the two-sample independent t-test were used for analysis of continuous variables. We used the Tukey–Kramer method to make adjustments when QOL measurements were compared with respect to disease severity. The association between QOL and symptom score was analyzed using Pearson’s correlation coefficient. Multiple linear regressions were performed to adjust data for age and gender, and to identify factors that were significantly related to the QOL of patients with IBS. All analyses were performed using SAS for Windows software (version 8.02; SAS Institute Inc., Cary, NC). A P-value ≤ 0.05 was considered statistically significant.
Results
Characteristics of the study population
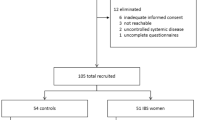
The demographic data of the participants are shown in Table 1. Of the 932 consecutive patients with abdominal pain and bowel symptoms that were considered as potential subjects for this study, 108 were excluded because of the time constraints of the Rome II criteria. Thirty patients were excluded by the minimal screening process: 10 with thyroid diseases and 20 with diabetes mellitus. One hundred thirty subjects were excluded because they did not complete the questionnaire. We compared the demographic data of responders and nonresponders. Nonresponders were not significantly different from responders in respect to gender, income, and marital status (P = NS). Data of 664 patients were analyzed. The mean age of the IBS patients was 43.0 ± 14.0 years, and 55.3% were women (Table 1). A total of 1,417 subjects were enrolled in the control group (mean age, 43.9 ± 14.8 years; females, 46.2%). The age distribution did not differ between control and IBS groups. The proportion of female subjects in the IBS group was greater than in the control group (P < 0.001; Table 1).
Information on referral centers, age groups, gender, IBS subtypes, symptom duration, self-reported symptom severity, marital status, level of education, annual income, and symptom scores according to these items is presented in Table 2. Total symptom score was greater for females than for males (64.2 ± 26.1 vs. 59.5 ± 24.8; P = 0.018). Total symptom score also differed according to age group, subtype, duration, level of education, marital status, and level of income (Table 2). Self-reported symptom severity was strongly correlated with symptom score (P < 0.01).
Generic HRQOL
Results of the SF-36 questionnaire for IBS patients and scores for the general population are presented in Table 3. The lowest scores were for vitality, general health, and mental health (44.7, 47.0, and 59.9, respectively). IBS patients had a lower score (a lower quality of life) than the general Korean population (P < 0.001, Fig. 1).
SF-36 scale scores were significantly lower in patients with IBS (■; n = 664) than in the Korean general population (□; n = 1,417). Values are expressed as means ± standard deviations. PF physical function, RP role limitations—physical, BP bodily pain, GH general health, VT vitality, SF social functioning, RE role limitations—emotional, MH mental health
Female IBS patients reported greater SF-36 scores and greater raw scores than male patients for all eight domains. However, when we compared z scores, which adjust for general population differences in SF-36 responses between male and female, gender-related differences between the scores of IBS patients were only observed for bodily pain and vitality (Table 3). None of the dimensions of SF-36 differed between secondary and tertiary centers. No differences were observed in SF-36 scores among the three IBS subtypes.
SF-36 scores for self-reported symptoms differed significantly between groups for all variables except physical functioning. With the exception of physical functioning, the self-reported subgroup classed as having severe symptoms had significantly lower SF-36 scores than those of the self-reported mild and moderate symptom subgroups.
IBS-specific QOL
Table 4 shows the perceptual and attitudinal features of Korean IBS patients. The mean overall score for IBS-QOL was 74.2. Of the eight domains, the greatest impairment (i.e., a score less than 65) was for health concern, followed by food avoidance. The mean for the sexual domain, which is comprised of two items, was 86.7. This indicates that IBS does not affect the sex life of most Korean IBS patients. The score for relationships was also high.
The overall score for IBS-QOL differed significantly between male and female patients. Because IBS-QOL is greatly affected by bowel symptoms and because female patients expressed more severe IBS-related symptoms than male patients, the overall score of the IBS-QOL was adjusted for total symptom score. Even after adjusting for total symptom score, the overall score was lower in female patients than in male patients (P < 0.05).
Except for the sexual domain, scores for all domains of the IBS-QOL were significantly lower in female IBS patients than in male IBS patients (P < 0.05).
IBS-QOL scores for body image and health concern were significantly lower in the C-IBS subgroup than in the other IBS subgroups.
All IBS-QOL scores decreased as self-reported symptom severity classification worsened (Table 4) after the other factors were taken into account (P < 0.01 for all domains). The mean scores for all IBS-QOL domains were significantly lower for the severe group compared with the moderate and mild groups (pairwise comparisons). There was no statistical difference in any IBS-QOL domain score between patients with mild or moderate symptoms.
None of the domains of the IBS-QOL differed between secondary and tertiary centers.
Relationship between HRQOL and IBS symptoms
Scores for the SF-36 and IBS-QOL questionnaires decreased with increasing frequency and bothersomeness of IBS symptoms (P < 0.01; Table 5). The correlation between symptom scores and HRQOL was higher for the IBS-QOL questionnaire than for the SF-36 questionnaire.
Multivariate analysis of factors affecting HRQOL
Factors associated with the overall score for IBS-QOL in multivariate analyses are listed in Table 6. The factors were gender, total symptom score, self-reported symptom severity, and level of education.
Discussion
This study showed that HRQOL is impaired in Korean patients with IBS. The QOL of Korean IBS patients was significantly impaired in all dimensions of generic HRQOL compared with the general population, as measured by the SF-36. Bowel symptoms had a strong impact on HRQOL. Female patients reported a lower HRQOL than male patients (the difference was statistically significant, but the difference was minimal). HRQOL scores were significantly associated with symptom severity. The IBS-QOL was significantly associated with female gender, symptom severity, and low level of education. Our data support the importance of inclusion of HRQOL assessment as a component of the evaluation of IBS patients.
Although there are substantial data on quality of life and IBS for Western countries, there are relatively few data for Asian countries. In Japanese studies, 30 and 102 patients with IBS were assessed for impairment of HRQOL [13, 14]. Chinese studies involved 41 and 73 patients with IBS [15, 16]. However, the small sample sizes in these studies constitute a limitation. The strengths of our study are that the sample size was large and that both a disease-specific IBS-QOL and the generic SF-36 were used. However, 108 patients were excluded because of the strict time-limited Rome II diagnostic criteria. The Rome III criteria [17], in which the time limitation was ameliorated, were not published when we designed this study.
Even though the social and cultural environment in which our study was carried out differs from that in the West, our results are agreement with those studies conducted in the West [4, 18]. HRQOL in IBS patients is significantly lower than the general population or for healthy subjects.
Significant impairment of HRQOL, assessed by both generic and specific HRQOL measurements, was only observed in patients with severe symptoms, whereas patients with mild and moderate symptoms showed only mild impairment, despite having been referred. Patients who experienced mild symptoms scored over 80 for all domains except health worry. In contrast, patients who experienced severe IBS symptoms scored below 80 for all domains except sexuality, which indicates that they experienced a significant impairment of HRQOL. Moreover, the overall score for IBS-QOL was less than 65 in the severe symptom group, which is similar to the results of Western studies [12, 19, 20].
Interestingly, the score for social functioning in the SF-36 and that for the sexual and relationship domain of the IBS-QOL were somewhat higher than those of Western studies [19–21], suggesting that IBS has little impact on social function in Korean patients. Similarly, a high score for the social-functioning dimension of the SF-36 was also observed in an epidemiologic study conducted in China [15]. This response may be related to the Eastern cultural milieu, which may differ from that of Western countries in the level of tolerance and acceptance of lower bowel symptoms. These aspects and their relationship with the perception of quality of life should be elaborated further by studies conducted in various cultural environments.
In the previous studies, participants who sought professional advice showed greater impairment in QOL than participants who had not sought professional advice [18, 22]. However, there was no difference in symptom severity, SF-36, or IBS-QOL scores between the secondary and tertiary centers in our study. This may stem from the referral system in Korea. In the Korean health-care system, patients can easily be referred to either a secondary or a tertiary center. Thus, in contrast to other countries, Korean consultants work in both secondary and tertiary care centers, in which patients have similar degrees of IBS severity. One of the common reasons for this is that psychological comorbidity ultimately influences QOL [23]. A limitation of our study was that we did not evaluate nonintestinal symptoms and psychological comorbidity, which might have influenced HRQOL.
Functional limitations were noted for all eight subscales of the IBS-QOL. This indicates that IBS patients experience emotional dysphoria (feelings of helplessness, having lost control, depression, and irritability) and that they also perceive their lifestyle as being restricted by their GI symptoms because of having to organize their day around toilet accessibility and having to modify their diet and food consumption. The lowest scores were for the health concern and food avoidance domains. The score for the health concern domain of the IBS-QOL was the lowest of all eight domains, irrespective of symptom severity. Therefore, health was the greatest concern among our patients. In studies conducted using the IBS-QOL questionnaire in the UK [24] and the US [11], scores for the health concern domain were consistently lower than scores for most other domains. Psychosomatic disorders, including IBS, are closely associated with health concerns [25]. However, participants in our study were examined at referral centers. Such participants might have had a greater propensity to seek medical care and might have had more severe forms of IBS than IBS patients who never seek medical care or who are examined at primary care or community gastroenterology practices.
Mean scores for HRQOL subscales may differ between countries. It is noteworthy that the scores for the sexual and relationship domains were greater than 80, which means that most responses were “not at all” or “slightly,” which is contrary to findings of a study conducted in the West [26]. In the validation study of the Korean version of the IBS-QOL, high scores for the sexual domain in Korean IBS patients suggested that IBS might affect their sex life marginally. Sociocultural differences between Koreans and Westerners may account for the high differences; Koreans are raised and educated in a Confucian society in which both males and females avoid discussing sexual concerns.
Our study showed that women with IBS have a lower HRQOL compared with men with IBS. Whereas the SF-36 score was lower for female patients than for male patients when raw data were used for analysis, there was no difference when data were adjusted for general population differences in the SF-36 responses of male and female, as reported previously [27]. IBS-QOL scores of males and females differed significantly even when adjusted for symptom score, but the difference was minimal. Interestingly, the score for bodily pain was significantly lower in female patients than in male patients in a US study [27] and in our study. In general, females are more sensitive than males to pain perception, including pain in internal organs [28]. Several mechanisms, such as differences in sex hormones [29, 30], psychological symptoms [31], and biobehavioral responses to stress [32], may be responsible for the difference between sexes.
The generic HRQOL score did not differ among the three IBS subgroups in our study. However, the IBS-specific QOL of the patients with C-IBS was significantly lower in the domains of health worry and body image than that of the other subtypes in our study. This finding might suggest that C-IBS patients worried more about health and had a worse body image than the other subgroups. The health concern score of C-IBS patients may have been elevated because one of the three items in this subscale, “I fear I won’t be able to have a bowel movement,” is much more likely to be a concern for those with constipation than those with diarrhea.
In our study, there was a strong relationship between the severity of patient-perceived disorders and the degradation of HRQOL, which is consistent with a previous study [33] and the previous validation study of the IBS-QOL questionnaire in Korean [7]. The IBS-QOL questionnaire used in this study was designed specifically for IBS. The correlation between symptom score and IBS-QOL score was greater than that between symptom score and SF-36 score. Therefore, this finding suggested that the IBS-QOL measure may reflect IBS disease status and response to treatment more accurately than the SF-36 measure.
Demographic and social factors had an effect on the HRQOL of patients with IBS. Female gender, severe symptom, and low level of education were associated with the overall IBS-QOL score after adjustment for confounding factors. The most profound effect on IBS-specific QOL score was exerted by the symptom severity. This was followed by a level of education of less than high school, which is the minimum level of compulsory education in Korea. It is unclear why education level was significant in predicting overall IBS-QOL in our study. In a retrospective review of HRQOL in chronic disease [34], patients who were older, female, had a low level of education, were not living with a partner, and had at least one comorbid condition reported the poorest level of QOL. There were no differences in HRQOL between subsets of IBS, which is consistent with previous studies in which the HRQOL of subgroups of IBS was evaluated using standardized Rome criteria [12, 35].
In conclusion, we demonstrated that Korean patients with IBS experience a mentally and physically impaired HRQOL. IBS-related symptoms had a great effect on the HRQOL of these patients. These results and the considerable prevalence of IBS in Korea indicate that IBS has a substantial social impact in this country.
Abbreviations
- IBS:
-
Irritable bowel syndrome
- IBS-C:
-
Constipation-predominant irritable bowel syndrome
- IBS-D:
-
Diarrhea-predominant irritable bowel syndrome
- IBS-M:
-
Mixed type irritable bowel syndrome
- QOL:
-
Quality of life
- SF-36:
-
Short Form 36
- IBS-QOL:
-
Irritable bowel syndrome-quality of life measure
- GI:
-
Gastrointestinal
- HRQOL:
-
Health-related quality of life
- ANOVA:
-
Analysis of variance
References
Fitzpatrick, R., Fletcher, A., Gore, S., Jones, D., Spiegelhalter, D., & Cox, D. (1992). Quality of life measures in health care. I. Applications and issues in assessment. British Medical Journal, 305(6861), 1074–1077.
Yacavone, R. F., Locke, G. R., III., Provenzale, D. T., & Eisen, G. M. (2001). Quality of life measurement in gastroenterology: What is available? The American Journal of Gastroenterology, 96(2), 285–297. doi:10.1111/j.1572-0241.2001.03509.x.
Drossman, D. A. (1998). Presidential address: Gastrointestinal illness and biopsychosocial model. Psychosomatic Medicine, 60(3), 258–267.
Gralnek, I. M., Hays, R. D., Kilbourne, A., Naliboff, B., & Mayer, E. A. (2000). The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology, 119(3), 654–660. doi:10.1053/gast.2000.16484.
Frank, L., Kleinman, L., Rentz, A., Ciesla, G., Kim, J. J., & Zacker, C. (2002). Health-related quality of life associated with irritable bowel syndrome: Comparison with other chronic diseases. Clinical Therapeutics, 24(4), 675–689. doi:10.1016/S0149-2918(02)85143-8.
Thompson, W. G., Longstreth, G. F., Drossman, D. A., Heaton, K. W., Irvine, E. J., & Muller-Lissner, S. A. (1999). Functional bowel disorders and functional abdominal pain. Gut, 45(Suppl 2), ii43–ii47.
Park, J. M., Choi, M. G., Oh, J. H., Cho, Y. K., Lee, I. S., Kim, S. W., et al. (2006). Cross-cultural validation of irritable bowel syndrome quality of life in Korea. Digestive Diseases and Sciences, 51(8), 1478–1484. doi:10.1007/s10620-006-9084-6.
Thompson, W. G., Longstreth, G. F., Drossman, D. A., Heaton, K. W., Irvine, E. J., Müller-Lissner, S. A.(2000). Functional bowel disorders and functional abdominal pain. In Rome II: The functional gastrointestinal disorders: Diagnosis, pathophysiology and treatment; A multinational consensus. McLean, VA: Degnon and Associates.
Talley, N. J., Haque, M., Wyeth, J. W., Stace, N. H., Tytgat, G. N., Stanghellini, V., et al. (1998). Development of a new dyspepsia impact scale: the Nepean Dyspepsia Index. Alimentary Pharmacology and Therapeutics, 13(2), 225–235. doi:10.1046/j.1365-2036.1999.00445.x.
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item Short Form Survey (SF-36): 1. Conceptual framework and item selection. Medical Care, 30(6), 473–483. doi:10.1097/00005650-199206000-00002.
Patrick, D. L., Drossman, D. A., Frederick, I. O., DiCesare, J., & Puder, K. L. (1998). Quality of life in persons with irritable bowel syndrome: Development of a new measure. Digestive Diseases and Sciences, 43(2), 400–411. doi:10.1023/A:1018831127942.
Drossman, D., Morris, C. B., Hu, Y., Toner, B. B., Diamant, N., Whitehead, W. E., et al. (2007). Characterization of health related quality of life (HRQOL) for patients with functional bowel disorder (FBD) and its response to treatment. The American Journal of Gastroenterology, 102(7), 1442–1453. doi:10.1111/j.1572-0241.2007.01283.x.
Kanazawa, M., Drossman, D. A., Shinozaki, M., Sagami, Y., Endo, Y., Palsson, O. S., et al. (2007). Translation and validation of a Japanese version of the irritable bowel syndrome-quality of life measure (IBS-QOL-J). BioPsychoSocial Medicine, 3, 1–6.
Kanazawa, M., Endo, Y., Whitehead, W. E., Kano, M., Hongo, M., & Fukudo, S. (2004). Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Digestive Diseases and Sciences, 49(6), 1046–1053. doi:10.1023/B:DDAS.0000034570.52305.10.
Lau, E. M., Chan, F. K., Ziea, E. T., Chan, C. S., Wu, J. C., & Sung, J. J. (2002). Epidemiology of irritable bowel syndrome in Chinese. Digestive Diseases and Sciences, 47(11), 2621–2624. doi:10.1023/A:1020549118299.
Huang, W. W., Zhou, F. S., Bushnell, D. M., Diakite, C., & Yang, X. H. (2007). Cultural adaptation and application of the IBS-QOL in China: A disease-specific quality-of-life questionnaire. Quality of Life Research, 16(6), 991–996. doi:10.1007/s11136-006-9141-9.
Longstreth, G. F., Thompson, W. G., Chey, W. D., Houghton, L. A., Mearin, F., & Spiller, R. C. (2006). Functional bowel disorders. Gastroenterology, 130(5), 1480–1491. doi:10.1053/j.gastro.2005.11.061.
Whitehead, W. E., Burnett, C. K., Cook, E. W., III., & Taub, E. (1996). Impact of irritable bowel syndrome on quality of life. Digestive Diseases and Sciences, 41(11), 2248–2253. doi:10.1007/BF02071408.
Creed, F., Ratcliffe, J., Fernandez, L., Tomenson, B., Palmer, S., Rigby, C., et al. (2001). Health-related quality of life and health care costs in severe, refractory irritable bowel syndrome. Annals of Internal Medicine, 134(9), 860–868.
Hahn, B. A., Yan, S., & Strassels, S. (1999). Impact of irritable bowel syndrome on quality of life and resource use in the United States and the United Kingdom. Digestion, 60(1), 77–81. doi:10.1159/000007593.
Brun-Strang, C., Dapoigny, M., Lafuma, A., Wainsten, J. P., & Fagnani, F. (2007). Irritable bowel syndrome in France: Quality of life, medical management, and costs: The Encoli study. European Journal of Gastroenterology and Hepatology, 19(12), 1097–1103.
Heaton, K. W., O’Donnell, L. J., Braddon, F. E., Mountford, R. A., Hughes, A. O., & Cripps, P. J. (1992). Symptoms of irritable bowel syndrome in a British urban community: Consulters and nonconsulters. Gastroenterology, 102(6), 1962–1967.
Drossman, D. A., McKee, D. C., Sandler, R. S., Mitchell, C. M., Cramer, E. M., Lowman, B. C., et al. (1998). Psychosocial factors in the irritable bowel syndrome. A multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology, 95(3), 701–708.
Akehurst, R. L., Brazier, J. E., Mathers, N., O’Keefe, C., Kaltenthaler, E., Morgan, A., et al. (2002). Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. PharmacoEconomics, 20(7), 455–462. doi:10.2165/00019053-200220070-00003.
Corney, R. H., & Stanton, R. (1990). Physical symptom severity, psychological and social dysfunction in a series of outpatients with irritable bowel syndrome. Journal of Psychosomatic Research, 34(5), 483–491. doi:10.1016/0022-3999(90)90022-V.
Spiegel, B. M., Gralnek, I. M., Bolus, R., Chang, L., Dulai, G. S., Mayer, E. A., et al. (2004). Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Archives of Internal Medicine, 164(16), 1773–1780. doi:10.1001/archinte.164.16.1773.
Lee, O. Y., Mayer, E. A., Schmulson, M., Chang, L., & Naliboff, B. (2001). Gender related differences in IBS symptoms. The American Journal of Gastroenterology, 96(7), 2184–2193. doi:10.1111/j.1572-0241.2001.03961.x.
Chang, L., & Heitkemper, M. M. (2002). Gender differences in irritable bowel syndrome. Gastroenterology, 123(5), 1686–1701. doi:10.1053/gast.2002.36603.
Houghton, L. A., Lea, R., Jackson, N., & Whorwell, P. J. (2002). The menstrual cycle affects rectal sensitivity in patients with irritable bowel syndrome but not healthy volunteers. Gut, 50(4), 471–474. doi:10.1136/gut.50.4.471.
Whitehead, W. E., Cheskin, L. J., Heller, B. R., Robinson, J. C., Crowell, M. D., Benjamin, C., et al. (1990). Evidence for exacerbation of irritable bowel syndrome during menses. Gastroenterology, 98(6), 1485–1489.
Blanchard, E. B., Keefer, L., Galovski, T. E., Taylor, A. E., & Turner, S. M. (2001). Gender differences in psychological distress among patients with irritable bowel syndrome. Journal of Psychosomatic Research, 50(5), 271–275. doi:10.1016/S0022-3999(01)00207-0.
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. doi:10.1037/0033-295X.107.3.411.
Hahn, B. A., Kirchdoerfer, L. J., Fullerton, S., & Mayer, E. (1997). Patient-perceived severity of irritable bowel syndrome in relation to symptoms, health resource utilization and quality of life. Alimentary Pharmacology and Therapeutics, 11(3), 553–559. doi:10.1046/j.1365-2036.1997.00160.x.
Sprangers, M. A., de Regt, E. B., Andries, F., van Agt, H. M., Bijl, R. V., de Boer, J. B., et al. (2000). Which chronic conditions are associated with better or poorer quality of life? Journal of Clinical Epidemiology, 53(9), 895–907. doi:10.1016/S0895-4356(00)00204-3.
Tillisch, K., Labus, J. S., Naliboff, B. D., Bolus, R., Shetzline, M., Mayer, E. A., et al. (2005). Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. The American Journal of Gastroenterology, 100(4), 896–904. doi:10.1111/j.1572-0241.2005.41211.x.
Acknowledgments
We thank Donald L. Patrick for kindly consenting to the use of the IBS-QOL in Korea.
Funding
This work was funded by grants from The Korean Society of Neurogastroenterology and Motility by Novartis Pharmaceuticals Corporation, Korea.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, J.M., Choi, MG., Kim, Y.S. et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res 18, 435–446 (2009). https://doi.org/10.1007/s11136-009-9461-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-009-9461-7