Abstract
Objective
To examine the association between medication expectations and subsequent experience on treatment satisfaction and intention to continue using the medication.
Methods
A longitudinal study with two surveys administered to each patient. Patients prescribed a new medication were recruited in pharmacies within Michigan. Medication-related expectations were evaluated at baseline. Experiences, satisfaction and intent to continue were evaluated a month later. Analyses used included factorial ANOVA models, multiple linear regressions and structural equation modeling (SEM). Impact of satisfaction on intention to continue was evaluated using correlation analysis and SEM.
Results
A total of 344 usable responses were obtained. SEM showed that expectation scores were not associated with both experience (path coefficient = 0.10) and satisfaction (path coefficient = 0.02, NS). On the other hand, experience was strongly associated with satisfaction (path coefficient = 0.89) and satisfaction was strongly associated with intent to continue using the new medication (path coefficient = 0.81).
Conclusions
This study empirically supports the value of the patient’s experience and its contribution to satisfaction, which in turn is associated with intended continued use mainly due to greater effectiveness of the newly prescribed medication. Satisfied consumers should be more adherent, thus enhancing the probability of positive therapeutic outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medication-related treatment outcomes, such as resolution of symptoms and lack of adverse events are highly correlated with treatment satisfaction with the medication. Satisfaction affects patients’ health-related decisions and treatment-related behaviors [1], specifically with the continuance of pharmaceutical treatment, correct medication use, and adherence with medication regimens [2–4]. Treatment satisfaction has been measured using self-report assessment tools [5].
Patient satisfaction is a specific class of patient-reported outcomes (PROs), others being measures of quality of life and symptom severity [6, 7]. PRO data, specifically patient satisfaction data can be used to diminish unpleasant characteristics of medications such as side effects, inconvenience of use or less-than-ideal effectiveness [5, 8]. Patient satisfaction with the medication experience has been documented [9] and such measures have been successfully incorporated into clinical trial protocols [10–12].
Patients’ satisfaction with their medication experience is thought to be heavily influenced by initial consumer expectations regarding the medication [13]. Expectations are based on patients’ beliefs about the anticipated effects of a prescribed medication. The medication experience is the consumer’s assessment of the medication effects.
The discrepancy between initial expectations and later experience produces disconfirmation [13]. The probability of encountering disconfirmation is greatest with new medications before the patient has an opportunity to adjust expectations based on experience. It has been proposed that a major cause of (dis)satisfaction with medication is the interaction between prior medication-related expectations and later experiences with the medication [14, 15]. Moreover, patients’ intention to continue or discontinue a medication therapy may be positively associated with satisfaction levels that result from the confirmation or disconfirmation of earlier expectations. Medication adherence levels have revealed to have strong relationships with overall satisfaction with care and also with satisfaction related to specific aspects of care. For example, one study found that medication compliance was significantly and positively related to satisfaction with access to care, satisfaction with financial aspects of care, satisfaction with interpersonal manner of physicians and overall satisfaction with care [16, 17].
The literature describes the relationship between expectations, experience and satisfaction in a very organized manner through the use of several theories. However, the foundation of most of the theoretical underpinnings of the above relationship arises from Oliver’s expectancy disconfirmation model [15]. The expectancy disconfirmation theory has been widely used to explain the association of expectations and experience on product/service-related satisfaction [14, 15]. Studies using Oliver’s model have generally concluded that satisfaction is highly and positively impacted by expectations being met and positive disconfirmation (more positive experience relative to expectations).
These relationships are not undisputed. There have been studies where positive disconfirmation has not always generated increased satisfaction levels [18]. Moreover, some studies have shown that over and above the effect of experience, individuals with higher expectations have greater satisfaction contrary to the philosophy of the expectancy disconfirmation model [19]. Additionally, certain other studies found that the construct of expectations being met is not important in determining satisfaction [20]. This lack of conclusive evidence further highlights the importance of the current research.
In our current research, we assess patient satisfaction with new prescription medications. The constructs we use include expectations, experience, disconfirmation (interaction of expectation versus experience) and satisfaction.
The first objective is to examine the degree to which discrepancies between consumer expectations towards a new medication and subsequent medication experience(s) influence treatment satisfaction. A disconfirmation effect is hypothesized. The possible interactions of the disconfirmation are listed below in descending order of the magnitude of satisfaction based on the expectancy disconfirmation theory [14, 15]:
-
(a)
Negative expectations towards the medication therapy and a positive experience will provide the highest satisfaction scores.
-
(b)
Positive expectations towards the medication therapy and a positive experience will provide high satisfaction scores.
-
(c)
Negative expectations towards the medication therapy and a negative experience will provide low satisfaction scores.
-
(d)
Positive expectations towards the medication and a negative experience will provide the lowest satisfaction scores.
The second objective is to test the relationship between consumer satisfaction with the new medication and intention to continue the medication therapy in similar future episodes of illness. It is hypothesized that satisfaction scores will be positively associated with intent to continue using medication.
Methods
A short-term longitudinal study design was adopted, with two surveys administered to each patient a month apart. Pharmacists were engaged from a broad geographic distribution of pharmacies within Michigan and asked to identify ambulatory care patients receiving a new medication. Chain and independent pharmacies participated in our study from a diverse group of rural and urban cities.
Pharmacists identified potential study participants by asking consumers if they were filling a prescription for a new medication, one they had not taken before. The sample was also limited to consumers who were at least 18 years of age and able to read and write in English. The research protocol for this study was implemented with approval of the University of Michigan Institutional Review Board and was compliant with health insurance portability and accountability act (HIPAA) guidelines.
Respondents were compensated a total of $25 for their participation which consisted of completing two surveys. Patients were given the choice of a paper and pencil questionnaire or logging onto a secure website to complete online surveys. Participants were requested to complete the first survey before they started the new medication therapy. This survey measured consumer expectations for the medication based on four domains including effectiveness, side effects, convenience of use and overall expectations of the medication along with a variety of questions to determine factors that predict expectations, such as medication history, insurance status, relationships with providers, information seeking behaviors and demographic characteristics. The second survey captured information regarding experience and satisfaction with the new medication using items measuring the same four domains and their intention to continue therapy. Descriptive statistics were generated to describe the demographic characteristics of the study sample.
The previously developed Treatment Satisfaction Questionnaire for Medications (TSQM ver 1.4) [5, 8] was selected as the satisfaction scale because it generates scores on each of the domains generally recognized as comprising treatment satisfaction and it has been studied across a range of health conditions and treatment types. The expectations and experience scales used the same general items with the wording modified as appropriate for each of the two new constructs, i.e. expectations and experiences. The creation of the expectations and experience scales was conducted using a Delphi technique [21] with five social scientists, four of whom were also pharmacists and one research psychologist. All item changes were unanimously approved. Final modifications to the instrument were made based on pilot tests conducted with a convenience sample of 20 individuals. For example, in the final instruments the first item on effectiveness within the expectations scale read: “How effective or ineffective do you think the new medication will be at preventing or treating your medical condition?” Alternatively, the first item on effectiveness within the experience scale read: “How effective or ineffective was the medication in preventing or treating your medical condition?”
The original wording of the TSQM items was retained as previously developed. The scoring for each of these four content domains of the expectations, experience and satisfaction constructs was based on a scoring algorithm used in the TSQM [5]. Raw domain scores were calculated using a composite score (summing the obtained scores of each item within the domain). The raw domain scores were subsequently transformed so that their possible scores ranged from 0 to 100, with higher scores indicating more positive perceptions.
Consumers who reported no expectations of side effects were assigned a maximum positive perception score of 100 for the side effects domain. Total scale (summary) scores for each of the three constructs were computed by adding three of the four domain scores (effectiveness + side effects + convenience of use). Total scale (summary) scores ranged from 0 to 300. The fourth domain, overall or summary assessment, was similarly scored but with values ranging from 0 to 100.
Psychometric properties of the effectiveness, side-effects and convenience of use domains for each of the three types of scales were tested through a confirmatory factor analysis using the principal components method with varimax rotation and a reliability analysis. The overall domain items were not included within the factor analysis as they may have tended to overlap with the other, more specific domain items. Additional psychometric testing of the satisfaction domains measured by the TSQM from the current research results has already been published elsewhere [8].
Two factorial ANOVA analyses were used to determine the interaction effect between the expectations and experience scores (dichotomized based on the median cut) on satisfaction scores. One ANOVA analysis was run using the total scale (summary) scores and a second analysis using the overall domain scores. The first ANOVA model contained overall assessment of the expectations and overall assessment of the experience construct scores as the independent factors each having two categories, high and low (based on the median cut). The dependent variable for the first ANOVA model was the overall assessment of satisfaction score, with scores ranging from 0 to 100. The second ANOVA model contained the same variables but total (summary) instead of overall scores, i.e., the sum of domain scores (effectiveness, side-effects and convenience of use).
Multiple regression analyses were also conducted. The regression analyses were similar to the ANOVA models, except that the constructs of expectation, experience and satisfaction were operationalized as continuous variables. The relationship between consumer satisfaction with the medication and intent to continue using the medication if needed was tested using a correlation analysis. Pearson’s r values were calculated to test the association between the various satisfaction scores and participants’ intent to continue.
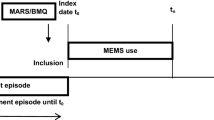
The test of the relationship between expectations, experience, satisfaction, and intent to continue was conducted within a structural equation model (SEM) framework. In the SEM model (Fig. 1), the effectiveness, side effect and convenience domains within the three scales (expectations, experience and satisfaction) were latent constructs. The items within each domain were parceled into two groups. These two groups served as indicators for the latent domains. For example, the effectiveness domain was measured using four items. These four items were divided into two groups. The mean score of item one and two was the first indicator of the effectiveness domain. The mean score of items three and four formed the second indicator for the effectiveness domain.
The latent domains then formed the latent scales (expectations, experience and satisfaction). The latent scales in turn were specified to be indicated by three items each from the overall domain of expectations, experience and satisfaction, respectively. Therefore, this model takes into consideration the overall domain items as well as the items belonging to the effectiveness, side effects and convenience of use domain within the three scales (expectations, experience and satisfaction). The discrepancy scores were excluded within the SEM model, since they were created using the difference between expectation and experience scores, leading to linear dependency and lack of good model fit. Also, intent to continue with medication was measured using a single item. Therefore, reliability values for this variable could not be calculated and the measurement error associated with the intention to continue variable could not be reasonably accounted for due to the absence of additional items.
For an SEM model to be acceptable the normative fit index (NFI), the non-normative fit index (NNFI) and the comparative fit index (CFI) should preferably be above 0.950 but values above 0.900 are acceptable [22]. The root-mean square error of approximation (RMSEA) should ideally be below 0.05 but values below 0.10 are acceptable [19]. Data analyses were conducted using SPSS 11.0 and EQS 6.1 (SEM).
Results
The total responses for the first survey was 450 (72%) out of a total of 616 surveys distributed at the pharmacies. Of 420 initial usable surveys, a total of 344 follow-up usable surveys were received. Non-response bias was not detected based on demographic characteristics and expectation scores. The demographic characteristics of consumers completing both phases of the study are shown in Table 1. Most respondents were female (65%), as females take more medications than males [23] and are also more likely to pick-up medications from the pharmacy for either themselves or a family member. In the state of Michigan the proportion of females in the population is 51% [24].
The sample comprised consumers with a wide age range, with a mean age of approximately 50 years and a range between 18 and 88 years. In the state of Michigan, 61% of the population is between 18 and 64 years [24]. Household income was fairly evenly distributed between the five categories. The median household income in the state of Michigan is $44,476. The mean family size was 2.42 (±1.2 standard deviation). In Michigan, 55% of adults live with children and 45% of adults have no children at home [24]. The sample was predominantly Caucasian (87%). In the state of Michigan, Caucasians comprise 78% of the population, followed by African-Americans (14%) and Hispanics (3%) [24].
The four domain scores (effectiveness, side effects, convenience and overall) within each of the scales are listed in Table 2. The mean scores for expectations, experience and satisfaction were similar for all domains. Comparing between domains, the effectiveness scores were the lowest followed by convenience of use and side effects. The convenience of use domain scores were high indicating that the medications were extremely easy to use. The side effects domain yielded the highest scores mainly because 31% of the sample expected side effects and only 26% of the respondents experienced side effects. The remaining consumers were assigned a maximum score of 100. The overall domain scores were slightly lower compared to the other three domains.
The results of the three factor analysis are presented in Tables 3 and 4. As expected, three different factors were identified, reflecting the three domains of expectations, experience and satisfaction. The three factors were produced through the principal components analysis using the Varimax rotation. The rotated factor structure demonstrated high item loadings for selected domains. The effectiveness, side effects and convenience of use items loaded on three separate factors for each of the three scales. Table 5 depicts the reliability analysis results. Reliability values for most individual domains except one within the three scales were above 0.80, indicating acceptable internal consistency between domain item scores.
The factorial ANOVA models to test objective one (the discrepancy between expectations and the medication experience on consumer satisfaction) produced significant main effects for expectations and experience (Table 6). This result suggests that consumers with high and low expectations and experience when independently viewed had significantly different satisfaction scores. The interaction between expectations and experience was not significant in either of the two models, but approached significance in the overall model (P = 0.063). The multiple regression models analyzing both total satisfaction (R 2 = 0.791) and overall satisfaction (R 2 = 0.739) produced only one significant predictor with a positive association: experience (Table 7). The expectations variable and the interaction term of expectations and experience were not significant.
Total and overall satisfaction scores were also highly correlated with participants’ ratings on the intent to continue using the medication item. Testing objective 2 we found that total satisfaction scores (effectiveness plus side effects plus convenience of use) had a Pearson’s r value of 0.648 (P < 0.001) and the overall satisfaction scores had a Pearson’s r value of 0.769 with the intention to continue variable, respectively.
The SEM model is presented in Fig. 1. All significant (P ≤ 0.05) path coefficients are highlighted. The SEM analysis produced a reasonable model fit. The NFI =0.913, NNFI = 0.931, CFI = 0.945 and RMSEA = 0.07. Examining the path coefficients it was found that each of the indicators of the individual latent domains (effectiveness, side effects and convenience of use) for all three scales (expectations, experience and satisfaction) produced high and positive values. Similarly, high path coefficients were also observed for each of the overall domain items, used as indicators of the constructs of expectations, experience and satisfaction.
The constructs of expectations and experience were most strongly associated with the effectiveness domain, having path coefficients of 0.75 and 0.73, respectively. Expectation scores were not associated with both experience (path coefficient = 0.10, NS) and satisfaction (path coefficient = 0.02, NS). On the other hand, experience was strongly associated with satisfaction (path coefficient = 0.89) and satisfaction was strongly associated with intent to continue using the new medication when the need arises in the future (path coefficient = 0.81).
Discussion
Few researchers have evaluated treatment satisfaction with medications. These studies have involved the comparison of specific products to placebo, competing medications, or other forms of treatment [25–27]. Also, these studies have been primarily conducted within clinical trials and are limited to a particular medication class or disease state [25–27]. The current study addressed gaps in the literature of treatment satisfaction related to medication use by including all medication classes and demonstrated relationships between several important theoretical constructs in a real world setting.
Our results showed that the psychometric performance of the three scales (expectations, experience and satisfaction) demonstrated acceptable reliability. Internal consistency (cronbach’s ά) results were high. Additionally, each of the items within the effectiveness, side effects and convenience of use domains loaded together on the same factor. The three domains as a whole loaded on separate factors. Evaluating the individual domain scores, it is not surprising that the side effects exhibited the highest domain scores since less than a third of the sample expected or experienced side effects and most were assigned the maximum possible score of 100.
Nearly all of the study medications were in oral or topical dosage forms (84%), which are more convenient to use than injections and inhalations. The effectiveness domain showed slightly lower scores within the experience construct scale and higher but comparable scores within the expectations and satisfaction scales. This is an interesting observation. Our sample contained approximately equal numbers of medications to treat/manage chronic (n = 150) and acute conditions (n = 156). The slightly lower effectiveness scores within the experience scale may be due to the attenuated impact of chronic disease related medications. Medications for chronic conditions do not cure patients’ conditions and/or respondents may have expected this, alternately they may have had hoped that their drugs would act faster or relieve symptoms sooner than they in fact did.
The ANOVA results indicated that although expectations and experience with a new medication both impact satisfaction significantly, there is no interaction effect. The highest satisfaction score was observed in consumers with positive expectations and experiences, followed by those with positive experiences and negative expectations. Consumers with positive expectations but negative experiences ranked third. The lowest satisfaction score was found in consumers with negative expectations and experiences. Experiences were more strongly correlated with satisfaction scores compared to expectations. The regression models of the same relationship generated similar results, except that the main effect (expectations) was not significant. This may have been primarily because of multicollinearity within the model (expectations and experience were moderately correlated with correlation coefficient values near 0.5).
The interaction effect between expectations and experience was non-significant in the ANOVA and regression tests. Therefore, consumers recruited within this study may have had reliable and valid information regarding the medication product they were about to obtain. Most consumers in our sample had similar expectation and experience scores, indicating expectations were realized. The expectations were not greatly superseded or unmet, resulting in no observed interaction between expectations and experience and consequently a lack of the disconfirmation effect. However, Ho et al. did observe a significant relationship between disconfirmation and satisfaction for OTC products [13]. The different results could be due to patients having greater contact with health professionals while obtaining prescriptions and having more realistic expectations which are later confirmed, leading to lack of a disconfirmation effect.
This study also found that the higher the satisfaction with the new medication, the greater the intent to continue using the drug. Treatment satisfaction data could, therefore, be used as a proxy indicator for future adherence with medications. However, there may be other factors that prevent intentions from translating into actual behavior. These include enabling factors based on the Andersen’s health care utilization model [28] such as insurance coverage, type of health plan and formulary changes within the health plan that may give preference to another medication.
Based on the structural equation modeling (SEM) results, we find the effectiveness domain strongly influenced the constructs of expectations and experience. The side effects and convenience of use domains had low or non-significant path coefficients with the expectations and experience constructs. Therefore, the medication’s effectiveness weighs primarily within the mind of consumers when they form expectations regarding a medication or when they report their experience with a medication. Side effects and convenience of use of the medication do not seem as important, these results are consistent with the findings of the validation study for the TSQM [5]. However, only approximately 25% of the respondents expected or experienced side effects and medications were predominantly topical/oral dosage forms (94%). The side effects and convenience of use domains may be important when evaluating specific medications which exhibit more frequent side effects or are not administered orally.
The constructs of expectations, experience and satisfaction were indicated by the three items within their respective overall domains. The path coefficient values were found to be above 0.80. This finding provides evidence that the items assessing the overall domains showed construct validity by representing the latent constructs of expectations, experience and satisfaction.
In the SEM model, expectations were shown not to be associated with experience (path coefficient = 0.10) and satisfaction (path coefficient = 0.02). This finding may be due in part to temporal effects. Expectations were measured a month earlier, leading to lower correlations compared to those between experience and satisfaction scores. A strong association was observed between satisfaction and intention to continue using the medication (path coefficient = 0.81). This relationship was higher compared to the results obtained while testing objective 2 (to test the relationship between satisfaction and intention to continue the medication). Therefore, the general impact of satisfaction taking into consideration all four domains (effectiveness, side effects, convenience of use and the overall domain) produced a much higher path coefficient with intent to continue.
Our study did have limitations. Our results cannot be generalized to the overall population due to sampling issues. Pharmacists did not recruit consumers randomly but may have recruited consumers they knew who would participate leading to lower rates of non-response or loss to follow-up. It is also possible that the $25 incentive to participate may have attracted consumers with financial need who responded more favorably due to the payment they received. Participants may have been prone to higher expectations as they have already adopted the behavior of acquiring the medication. The responses provided, especially within the experience and satisfaction scales may have been prone to contamination effects from respondents who had comorbidities and were using other medication products concurrently. Patients with negative experiences may not have responded to the second survey.
Consumers may not have provided their expectations data until after they began using the new medication. Study results may have been prone to recall bias due to the longitudinal nature of the study design. Consumers responded to the experience and satisfaction scales at least a month after starting the medication. The recall bias may be present within those consumers who were prescribed the new medication for a very short period (e.g., less than 10 days) or who discontinued use of the product shortly after initiation. However, only 12 consumers had a recall period greater than 30 days. The short follow-up period also may not have captured the occurrence of adverse events that develop over an extended time period.
This study supports the value of the patient’s experience and its contribution to satisfaction and the contribution of satisfaction to intended adherence mainly due to efficacy of the newly prescribed medication. Effectiveness of the medication is perceivable and compelling evidence for consumers. This research documents the ability of consumers to assign value to medication-related experience and satisfaction constructs as perceived from their perspective. Satisfied consumers should be more adherent, thus enhancing the probability of positive therapeutic outcomes.
This new evidence suggests that treatment satisfaction is a significant contributor to intention to continue therapy and presumably, eventual positive therapeutic outcomes. Measuring satisfaction with treatment besides clinical endpoints would provide significant additional insights from a patient perspective and health plans could be evaluated based on performance with PRO scores.
References
Taylor, T. R. (2000). Understanding the choices that patients make, [Review] [52 refs]. Journal of the American Board of Family Practice, 13(2), 124–133.
Awad, A. G., & Voruganti, L. N. (1999). Quality of life and new antipsychotics in schizophrenia. Are patients better off? International Journal of Social Psychiatry, 45(4), 268–275.
Anderson, R. B., Hollenberg, N. K., & Williams, G. H. (1999). Physical symptoms distress index: A sensitive tool to evaluate the impact of pharmacological agents on quality of life. Archives of Internal Medicine, 159(7), 693–700.
Diamond, R. (1985). Drugs and the quality of life: The patient’s point of view. Journal of Clinical Psychiatry, 46(5 Pt 2), 29–35.
Atkinson, M. J., Sinha, A., Hass, S. L., et al. (2004). Validation of a general measure of treatment satisfaction—the treatment satisfaction questionnaire for medication (TSQM) using a national panel study of chronic disease. Health and Quality of Life Outcomes, 2:12.
Katz, J. N. (2001). Patient preferences and health disparities, [comment]. JAMA, 286(12), 1506–1509.
Golin, C. E., DiMatteo, M. R., & Gelberg, L. (1996). The role of patient participation in the doctor visit. Implications for adherence to diabetes care, [Review] [134 refs]. Diabetes Care, 19(10), 1153–1164.
Atkinson, M. J., Kumar, R., Cappelleri, J. C., & Hass, S. L. (2005). Hierarchical construct validity of the treatment satisfaction questionnaire for medication (TSQM version II) among outpatient pharmacy consumers. Value Health, 8 (Suppl 1), S9–S24.
Acquadro, C., Berzon, R., Dubois, D., et al. (2003). Incorporating the patient’s perspective into drug development and communication: An ad hoc task force report of the patient-reported outcomes (PRO) harmonization group meeting at the food and drug administration, February 16, 2001. Value in Health, 6(5), 522–531.
Chatterton, M. L., Scott-Lennox, J., Wu, A. W., & Scott, J. (1999). Quality of life and treatment satisfaction after the addition of lamivudine or lamivudine plus loviride to zidovudine-containing regimens in treatment-experienced patients with HIV infection. Pharmacoeconomics, 15(Suppl 1), 67–74.
Greil, W., Ludwig-Mayerhofer, W., Erazo, N., et al. (1997). Lithium vs carbamazepine in the maintenance treatment of schizoaffective disorder: A randomised study. European Archives of Psychiatry & Clinical Neuroscience, 247(1), 42–50.
Mathias, S. D., Warren, E. H., Colwell, H. H., & Sung, J. C. (2000). A new treatment satisfaction measure for asthmatics: A validation study. Quality of Life Research, 9(7), 873–882.
Ho, F. N., Mursch, J. D., Ong, B. S., & Perttula, B. (1997). Consumer satisfaction with OTC drugs: an analysis using the confirmation/disconfirmation model. Health Marketing Quarterly, 15(1), 103–117.
Baron-Epel, O., Dushenat, M., & Friedman, N. (2001). Evaluation of the consumer model: Relationship between patients’ expectations, perceptions and satisfaction with care. International Journal for Quality in Health Care, 13(4), 317–323.
Oliver, R. L. (1980). A cognitive model of the antecedents and consequences of satisfaction decisions. Journal of Marketing Research, 17(4), 460–409.
Smith, N. A., Ley, P., Seale, J. P., & Shaw, J. (1987). Health beliefs, satisfaction and compliance. Patient Education & Counseling, 10(3), 279–286.
Harris, L. E., Luft, F. C., Rudy, D. W., & Tierney, W. M. (1995). Correlates of health care satisfaction in inner-city patients with hypertension and chronic renal insufficiency. Social Science & Medicine, 41(12), 1639–1645.
Olson, J. C., & Dover, P. A. (1979). Disconfirmation of consumer expectations through product trial. Journal of Applied Psychology, 64(2), 179–189.
Ascher-Svanum, H., Rochford, S., Cisco, D., & Claveaux, A. (2001). Patient education about schizophrenia: Initial expectations and later satisfaction. Issues in Mental Health Nursing, 22(3), 325–333.
Froehlich, G. W., & Welch, H. G. (1996). Meeting walk-in patients’ expectations for testing. Effects on satisfaction. Journal of General Internal Medicine, 11(8), 470–474.
Shore, B. E., & Franks, P. (1986). Physician satisfaction with patient encounters. Reliability and validity of an encounter-specific questionnaire. Medical Care, 24(7), 580–589.
Schmidt, S., Muhlan, H., & Power, M. (2006). The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. Eur J Public Health, 16(4), 420–428.
Roe, C. M., McNamara, A. M., & Motheral, B. R. (2002). Gender- and age-related prescription drug use patterns. Annals of Pharmacotherapy, 36(1), 30–39.
State Health Facts Online: Health Coverage and the Uninsured. Kaiser Family Foundation.www.statehealthfacts.org. Retrieved October 2004. Internet Communication.
Gerth, W. C., McCarroll, K. A., Santanello, N. C., Vandormael, K., Zhang, Q., & Mannix, L. K. (2001). Patient satisfaction with rizatriptan versus other triptans: Direct head-to-head comparisons. International Journal of Clinical Practice, 55(8), 552–556.
Greil, W., Ludwig-Mayerhofer, W., Erazo, N., Engel, R. R., Czernik, A., Giedke, H., Muller-Oerlinghausen, B., Osterheider, M., Rudolf, G. A., Sauer, H., Tegeler, J., & Wetterling, T. (1997). Lithium vs carbamazepine in the maintenance treatment of schizoaffective disorder: A randomised study. European Archives of Psychiatry & Clinical Neuroscience, 247(1), 42–50.
Bech, P., Moses, R., & Gomis, R. (2003). The effect of prandial glucose regulation with repaglinide on treatment satisfaction, wellbeing and health status in patients with pharmacotherapy naive type 2 diabetes: a placebo-controlled, multicentre study. Quality of Life Research, 12(4), 413–425.
Andersen, R., & Aday, L. A. (1978). Access to medical care in the US: Realized and potential. Medical Care, 16(7), 533–546.
Acknowledgement
The authors wish to thank the participating pharmacists who recruited patients into the study: Frank Ackley, Roberta Armstrong, Jim Baxter, John Kaser, Frank Pawlicki, Michael Sanborn, Andrew Schandoyan, Mark Young, and Steve Zawisza. This research was supported by a grant from Pharmacia, Inc (now Pfizer).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, R.N., Kirking, D.M., Hass, S.L. et al. The association of consumer expectations, experiences and satisfaction with newly prescribed medications. Qual Life Res 16, 1127–1136 (2007). https://doi.org/10.1007/s11136-007-9222-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-007-9222-4