Abstract
We examined the outpatient prescription pattern of psychotropic drugs used for the treatment of five major psychiatric diseases in Bahrain. Setting outpatient department of the main psychiatric hospital in Bahrain. Methods This was a retrospective, cross-sectional study in which we targeted randomly selected prescriptions (n = 992, 56.1% males, 43.9% females) from 1st of January until 31st of December, 2017. Main outcome measure the types of outpatient psychotropic drugs prescribed by the physicians. Results The pharmacotherapy of schizophrenia consisted of atypical anti-psychotics (92.8%), or typical anti-psychotics (17.8%). The anti-depressants used were: Selective-serotonin reuptake inhibiters (SSRIs) (41.6%), Serotonin-norepinephrine reuptake inhibiters (SNRIs) (34.5%), tricyclic anti-depressants (TCAs) (12.8%), and atypical anti-depressants (10.6%). Combination anti-depressants was employed in (12.4%) of cases. The pharmacotherapy for anxiety disorders was composed of benzodiazepines (59.5%), atypical anti-psychotics (45.2%), SSRIs (40.5%), SNRIs (28.6%), TCAs (14.3%), and anti-convulsants (16.7%) and atypical anti-psychotics (7.1). The medications prescribed for bipolar disorder were atypical anti-psychotics (78.6%), anti-convulsants (66.5%), benzodiazepines (27.7%), typical anti-psychotics (8.9%) and lithium (6.7%). Schizoaffective disorder patients received atypical anti-psychotics (97.3%), anti-convulsants (47.8%), benzodiazepines (27.4%), SNRIs (25.7%), SSRIs (15%), typical anti-psychotics (10.6%), atypical anti-depressants (10.6%) and TCAs (6.2%). A combination of antipsychotics and anti-depressants was employed in 33.6% and 4.7% of all subjects regardless of the diagnosis, respectively. Conclusions With a few exceptions, the pharmacotherapy of psychiatric diseases in Bahrain was in line with the latest recommendations. However, psychotropic polypharmacy was observed and calls for immediate attention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last few decades, the pharmacotherapy of most psychiatric disorders has been subjected to major changes, mainly due to the advent of newer drugs. Indeed, in most clinical settings, newly introduced psychotropic drugs, which possess higher efficacy and safety, have become first-line therapy in all cases. For example, due to their tolerability and better efficacy for treating negative symptoms of schizophrenia, atypical anti-psychotic drugs such as risperidone, olanzapine and aripiprazole are currently preferred over conventional ones like phenothiazine and haloperidol [1]. Indeed, Bret et al. studied the prescribing practices of antipsychotic drugs in a group of psychiatric hospitals in France and reported that atypical anti-psychotic drugs have largely replaced the conventional ones for the treatment of schizophrenia and mood disorders [2]. Likewise, selective serotonin reuptake inhibitors (SSRIs) and selective norepinephrine reuptake inhibitors (SNRIs) are now the drugs of first choice for treating major depressive illness, compared to the older anti-depressant medications such as tricyclic anti-depressants, which have universally become second-line drugs [3].
The introduction of more effective and tolerable psychotropic drugs has led to an increase in the rate of psychotropic polypharmacy, defined as the prescription of two or more psychotropic drug in combination [4]. Under certain clinical settings, the use of psychotropic drug combinations is sometimes justified, such as for the treatment of multiple psychiatric disorders such as the management of schizophrenia patients who suffer from comorbid depression [5]. However, in many cases, prescribing a combination of drugs for psychiatric patients could be irrational, and may result in serious adverse consequences which include in addition to the increased cost of therapy, increasing adverse drug reactions and the development of drug-drug interactions [6]. Brett et al., 2017 studied psychotropic polypharmacy in Australia between 2006 and 2015. The investigators reported that the rate of polypharmacy was 5.9–7.3% for antipsychotics, 2.1–3.7% for antidepressants and 4.3–2.9% for benzodiazepines [4].
Aim of the Study
In the present study, we aimed to explore the prescription pattern of major psychotropic drugs, which are used for the treatment of five major psychiatric disorders, namely, schizophrenia, major depression, anxiety disorders, bipolar disorder, and schizoaffective disorder. We ought to contrast the prescription trend of these medications to both the international guidelines and other countries. In addition, we aimed to investigate the rate of psychotropic polypharmacy in our sample of prescriptions classified by class. To the best of our knowledge, this study was the first to be conducted in Bahrain to explore this aspect of psychopharmacology.
Ethics Approval
Prior to conducting this study, ethical approval was obtained from the Research and Ethics Committee at the Arabian Gulf University (approval number: E013-PI-10/17). Approval was also acquired from the Secondary Healthcare Research Committee at the Ministry of Health in Bahrain (approval number: SHCRC17042018). Data was collected retrospectively by analyzing outpatient prescriptions made by physicians at the target hospital. No patient interviewing was conducted as part of this investigation. Because the research was retrospective in nature, no informed consent was necessary, and the approving committees approved the waiver.
Methods
The Psychiatric Hospital, which was established in 1932, is the national center in Bahrain that provides secondary and tertiary psychiatric services for about 1.3 million people who live in the country. Currently, the hospital contains 269 beds for inpatient care, in addition to several service units. Those service units include general adult psychiatry, drug and alcohol detoxification and rehabilitation, child and adolescent psychiatry, community psychiatric services, old age psychiatry services, intellectual disability services, forensic psychiatry, general adult liaison psychiatry, anxiety clinic and marital counseling clinic.
In order to be dispensed to patients, prescriptions made by physicians at the outpatient clinics of the target hospital, are sent electronically to the pharmacy, which is located within the same building. All prescription orders are saved in an electronic system that belongs to the Ministry of Health, called “I-Seha”. The prescriptions contain various information such as patient’s age, gender, diagnoses, source of prescription, prescriber’s name, and a list of medications prescribed to the patient.
This was a retrospective, cross-sectional study, which targeted a sample of outpatient prescriptions issued by the outpatient clinics of the Psychiatric Hospital in Bahrain. A randomly-selected sample of outpatient prescriptions from within the target hospital, received electronically by the pharmacy department from 1st of January until the 31st of December, 2017, were included in the current study. The target year was divided into 4 seasons: Spring (March 1 to May 31), summer (June 1 to August 31), autumn (September 1 to November 30), and winter (December 1 to February 28). In. In each season, one random month was selected. All prescriptions made over one randomly selected week of the selected month were analyzed. Out of the prescriptions, which were retrieved for analysis, only those, which were issued for patients diagnosed with the following psychiatric disorders, were included in the study: Schizophrenia, depression, anxiety disorders, bipolar disorder, and schizoaffective disorder. All the diagnoses were made against the International Classification of Diseases Version 10 (ICD-10) criteria. The selected prescriptions were examined for patient’s characteristics such as age, gender, and diagnosis. In addition, the type of psychotropic medications, which were included in the prescription orders were analyzed.
The data collected in this study was analyzed by using the Statistical Package for the Social Sciences (SPSS), Version 25 (IBM Corp., Chicago, Illinois, USA). Simple descriptive statistics were utilized to analyze the results.
Results
The number of prescriptions, which were analyzed during the current study, was (992) (Table 1). The majority of subjects were adults (69.9%), whereas the rest were children, aged less than 18 years (30.1%). According to gender, (56.1%) of the selected patients were males, and (43.9%) were females. Based on the diagnosis stated in the prescription, the most common was schizophrenia (39%), followed by depression (22.8%), bipolar disorder (22.6%), schizoaffective disorder (11.4%), and anxiety disorder (4.2%) (Table 2).
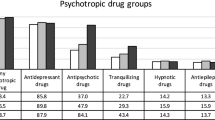
Irrespective of the diagnosis, the most commonly prescribed psychotropic drugs were atypical anti-psychotics (78.7%), anti-convulsants (32.1%), benzodiazepines (29.6%), SNRIs (19.7%), SSRIs (19%), typical anti-psychotics (11.5%), atypical anti-depressants (6.8%), tricyclic anti-depressants (6.3%), and lithium (1.8%). Almost one-third of the target subjects received a combination of anti-psychotic drugs (33.6%) compared to (4.7%) only, who were treated with more than one anti-depressant drug.
The prescriptions were further analyzed for the psychotropic drug selection according to the patient’s diagnosis. Regarding the patients who were diagnosed to have schizophrenia, the most frequently prescribed drugs, were atypical anti-psychotics (92.8%) and typical anti-psychotics (17.8%). In addition, (50.1%) of those subjects received a combination of anti-psychotic agents. For patients with major depression, the most commonly prescribed anti-depressants were SSRIs (41.6%), SNRI (34.5%), TCAs (12.8%), and atypical anti-depressants (10.6%). Moreover, it was observed that a combination of anti-depressant agents was employed in (12.4%) of cases.
Regarding the pharmacotherapy of patients who suffered from anxiety disorders, the majority of cases were managed by using benzodiazepines (59.5%), followed by atypical anti-psychotics (45.2%), SSRIs (40.5%), SNRIs (28.6%), anti-convulsants (16.7%), TCAs (14.3%), and typical anti-psychotic drugs (7.1%). For bipolar disorder patients, most of them were treated by using atypical anti-psychotic medications (78.6%), followed by anti-convulsants (66.5%), benzodiazepines (27.7%), typical anti-psychotics (8.9%) and lithium (6.7%). Lastly, nearly all patients who were diagnosed with schizoaffective disorder were managed by atypical anti-psychotic drugs (97.3%), followed by anti-convulsants (47.8%), benzodiazepines (27.4%), SNRIs (25.7%), SSRIs (15%), typical anti-psychotics, (10.6%), atypical anti-depressants (10.6%), TCAs (6.2%), and lithium (0.9%). It was noted that (44.2%) of those subjects were managed by using a combination of anti-psychotic drugs compared to (4.4%) who were prescribed more than one anti-depressant.
Discussion
The current study was carried out to describe the types of psychotropic drugs, which are used for treating five major psychiatric disorders in Bahrain, namely schizophrenia, major depression, bipolar disorder, anxiety disorders and schizoaffective disorder. The research team targeted a cohort of (992) prescription orders that were issued by the outpatient department of the central psychiatric hospital in the Kingdom. Our data showed that, with a few exceptions, pharmacotherapy of those psychiatric diseases generally followed the international guidelines. However, a relatively high rate of psychotropic polypharmacy was observed which merit further attention.
Our data showed that the most commonly diagnosed psychiatric disorder in our sample was schizophrenia followed by major depression and bipolar disorder, both of which had about an equal prevalence, whereas anxiety disorders were the least common. The prevalence of these psychiatric diseases seems to be dissimilar in different geographical locations. Indeed, in contrast to our findings, Baxter et al. conducted a systematic review on the prevalence of mental conditions in China and India and noticed that major depression followed by anxiety disorders were the most prevalent whereas schizophrenia was the least common [7].
Our findings revealed that the most commonly prescribed anti-psychotic drugs for treating patients who suffered from schizophrenia were atypical agents. These observations were in line with the international trend of using the newer atypical anti-psychotics at the expense of the conventional ones, largely due to their safety, tolerability and ability to control negative symptoms of schizophrenia. Recently, there has been a significant debate about efficacy of the atypical anti-psychotic drugs. Lewis et al., conducted a randomized clinical trial on (227) subjects, to study the clinical and cost-effectiveness of typical and atypical anti-psychotic drugs. Except for participants who received clozapine, the investigators reported that, following twelve months of therapy, typical anti-psychotics were not inferior to the newer agents in relation to participant’s quality of life, symptoms, or cost of therapy [8]. Clearly, our data showed that the newer anti-psychotic drugs were the drugs of first choice for the prescribers. However, based on the latest evidence, this clinical choice needs to be reconsidered in the light of the debate on their efficacy and associated cost of therapy.
The drug selection for the treatment of major depression followed the most recent recommendations. Indeed, SSRIs were the first-line drugs, followed by SNRIs. Two-thirds of the major depression subjects received one of these two drug groups. Comparatively, older TCAs and atypical anti-depressants were selected in a small percentage of patients. Although SSRIs were the most commonly selected drugs by the psychiatrists in our sample, there has been a discussion on the practice of using SSRIs as first-line drugs for major depression. Cipriani et al., conducted systematic review about the efficacy and tolerability of different anti-depressant medications and reported that SSRIs were associated with the best outcome in terms of efficacy and adverse effects profile [9]. In contrast to these findings, Machado et al., conducted a meta-analysis to compare the remission rate and adverse reactions of the various anti-depressant drug groups [10]. The investigators concluded that SNRIs were associated with the highest response rate followed by TCAs and then SSRIs. Due to the ongoing debate about the selection of first-line drugs for depression, we believe that physicians choices were generally acceptable.
We also studied the doctor’s drug selection for managing anxiety disorders. Our data reported that most cases were managed by using benzodiazepines (59.5%), followed by anti-psychotics (45.2%), SSRIs (40.5%), and SNRIs (28.6%). These data are in line with the results of the meta-analysis of Gomez et al., who concluded that based on the latest evidence, BZSs were the most effective treatment option for generalized anxiety disorder compared to SSRIs and SNRIs which showed less satisfactory response [11]. In accordance with these data, Reinhold et al. studied the efficacy of the different drug groups for treating generalized anxiety disorder and concluded that BZs are considered first-line therapy [12]. We observed a high rate of using anti-psychotic drugs for anxiety disorder cases. Veale et al., conducted a systematic review and meta-analysis to study the role of atypical anti-psychotics in SSRI-resistant anxiety disorder and reported that the newer anti-psychotics are effective [13]. Our data showed that drug selection for anxiety disorders is in line with the latest evidence that BZS are the most effective group of drugs for this condition.
For bipolar disorder, most patients were treated by atypical anti-psychotic medications (78.6%), anti-convulsants (66.5%) and benzodiazepines (27.7%). A small proportion of patients were maintained on lithium (6.7%). Regarding the atypical antipsychotic drugs, NICE guidelines recommended olanzapine as part of the first-line treatment for moderate to severe bipolar depression; and also, for mania, hypomania and rapid cyclers. Other studies, however, revealed that anticonvulsant agents had higher efficacy than lithium while anti-psychotic drugs were ranked the least effective for treating bipolar disorder [14]. The high rate of prescribing benzodiazepines for these patients was also noticed. This approach has been discouraged as evidenced by recent studies largely because the initiation of BZs resulted in dependence in a large percentage of users [15].
Our findings on the drug therapy for schizoaffective disorder showed that almost all cases were treated by atypical anti-psychotics, followed by anti-convulsants, BZs and SSRIs. In contrast to schizophrenia and major depression, clear guidelines for the pharmacotherapy of schizoaffective disorder are not developed yet. Most clinicians recommend using anti-psychotic medications for this condition both for acute and chronic therapy [16]. The combination of anti-psychotics with an anti-depressant is also recommended for this condition [17].
Almost half of the schizophrenia patients received a combination of anti-psychotic drugs. This phenomenon was significantly more common in males (40%) than females (25.3%) (p < 0.001). Although it was more common in younger subjects, no significant difference was noticed based on participant’s age (p > 0.05). In addition, one-third of all patients regardless of the diagnosis were maintained on a combination of anti-psychotic drugs. The observed prevalence of anti-psychotic polypharmacy in our study is significantly higher than what was previously reported by Fontanella et al., who reported a rate of using a combination of anti-psychotic therapy that reached 24.9% [18]. Similar to our data, however, the authors found a positive association between the rate of using a combination of anti-psychotics and younger age and male gender. The use of combination anti-psychotics was also high in schizoaffective disorder (44.2%) and bipolar disorder (28.6%). Comparatively, major depression cases who received more than one anti-depressant was (12.4%), a rate which was lower than what has recently been reported by Rhee et al., who showed that 22.7% of depression cases were on combination anti-depressants [19]. Psychotropic polypharmacy is serious and should be avoided since it can result in serious adverse outcomes to the patients [20].
There are several strengths, which are pertinent to this study. Firstly, we analyzed a relatively large number of prescriptions. This adequate sample size allowed the research team to make conclusions on the research questions with confidence. Secondly, we explored the psychotropic drug therapy for the most common five psychiatric diseases rather than limiting our investigation to one disease. This gave the investigators a broader view of the choice of the psychopharmacotherapy in Bahrain. On the other hand, this study had certain limitations. Firstly, all the data was collected from one hospital rather than collecting information on drug prescribing from different centers. Because in Bahrain only one psychiatric hospital exists, this limitation could not be addressed. Secondly, investigating the prescription trend of psychotropic medications inpatients was not performed. Rather our study was limited to the outpatient prescribing patterns.
Conclusion
In this study, we investigated the selection of drug therapy for five major psychiatric disorders at the outpatient clinics which belong to the central psychiatric hospital in Bahrain. With a few exceptions, the pharmacotherapy of those diseases was in line with the latest guidelines. However, psychotropic polypharmacy was observed in a significant percentage of cases and calls for immediate attention.
References
Trifirò G, Spina E, Brignoli O, Sessa E, Caputi AP, Mazzaglia G. Antipsychotic prescribing pattern among Italian general practitioners: a population-based study during the years 1999-2002. Eur J Clin Pharmacol. 2005;61(1):47–53.
Bret P, Bret MC, Queuille E. Prescribing patterns of antipsychotics in 13 French psychiatric hospitals. Encephale. 2009;35(2):129–38.
DeFilippis M, Wagner KD. Management of treatment-resistant depression in children and adolescents. Paediatr Drugs. 2014;16(5):353–61.
Brett J, Daniels B, Karanges EA, Buckley NA, Schneider C, Nassir A, et al. Psychotropic polypharmacy in Australia, 2006 to 2015: a descriptive cohort study. Br J Clin Pharmacol. 2017;83(11):2581–8.
Grüber L, Falkai P, Hasan A. Depressive symptoms in schizophrenia. Fortschr Neurol Psychiatr. 2015;83(4):238–46.
Tanaka E, Hisawa S. Clinically significant pharmacokinetic drug interactions with psychoactive drugs: antidepressants and antipsychotics and the cytochrome P450 system. J Clin Pharm Ther. 1999;24(1):7–16.
Baxter AJ, Charlson FJ, Cheng HG, Shidhaye R, Ferrari AJ, Whiteford HA. Prevalence of mental, neurological, and substance use disorders in China and India: a systematic analysis. Lancet Psychiatry. 2016;3(9):832–41.
Lewis SW, Davies L, Jones PB, Barnes TR, Murray RM, Kerwin R, et al. Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technol Assess. 2006;10(17):iii-iv, ix-xi, 1-165.
Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009 28;373(9665):746–58.
Machado M, Iskedjian M, Ruiz I, Einarson TR. Remission, dropouts, and adverse drug reaction rates in major depressive disorder: a meta-analysis of head-to-head trials. Curr Med Res Opin. 2006;22(9):1825–37.
Gomez AF, Barthel AL, Hofmann SG. Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: a meta-analytic review. Expert Opin Pharmacother. 2018;19(8):883–94.
Reinhold JA, Rickels K. Pharmacological treatment for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother. 2015;16(11):1669–81.
Veale D, Miles S, Smallcombe N, Ghezai H, Goldacre B, Hodsoll J. Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and meta-analysis. BMC Psychiatry. 2014;14:317.
Yee CS, Hawken ER, Baldessarini RJ, Vázquez GH. Maintenance pharmacological treatment of juvenile bipolar disorder: review and meta-analyses. Int J Neuropsychopharmacol. 2019;22(8):531–40.
Wingård L, Taipale H, Reutfors J, Westerlund A, Bodén R, Tiihonen J, et al. Initiation and long-term use of benzodiazepines and Z-drugs in bipolar disorder. Bipolar Disord. 2018;20(7):634–46.
Azorin JM, Kaladjian A, Fakra E. Current issues on schizoaffective disorder. Encephale. 2005;31(3):359–65.
Danileviciūte V. Schizoaffective disorder: clinical symptoms and present-day approach to treatment. Medicina (Kaunas). 2002;38(11):1057–65.
Fontanella CA, Hiance-Steelesmith DL, Guirgis H, Campo JV. Trends in and predictors of long-term antipsychotic Polypharmacy use among Ohio Medicaid patients with schizophrenia, 2008-2014. Psychiatr Serv. 2018;69(9):1015–20.
Rhee TG, Rosenheck RA. Psychotropic polypharmacy reconsidered: between-class polypharmacy in the context of multimorbidity in the treatment of depressive disorders. J Affect Disord. 2019;252:450–7.
Nørgaard A, Jensen-Dahm C, Gasse C, Hansen ES, Waldemar G. Psychotropic Polypharmacy in patients with dementia: prevalence and predictors. J Alzheimers Dis. 2017;56(2):707–16.
Acknowledgements
We would like to thank the pharmacy staff at the Psychiatric Hospital in Bahrain for their cooperation with the investigators. Special thanks to Dr. Amer Almarabheh for his help with the statistical analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare that they have no conflicts of interest.
Human Participants and Informed Consent
This research did not involve human participants and or animals. Since the study was retrospective no informed consent form was needed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tayem, Y.I., Jahrami, H.A., Ali, M.K. et al. Ambulatory Pharmacotherapy of Five Psychiatric Disorders in Bahrain: a Descriptive Study. Psychiatr Q 91, 289–298 (2020). https://doi.org/10.1007/s11126-019-09705-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-019-09705-5