Abstract
This study examined the incidence of PTSD and psychiatric co-morbidity among women who experienced stillbirth and investigated the relationship between locus of control, trauma characteristics of stillbirth, posttraumatic cognitions, PTSD and co-morbid psychiatric symptoms following stillbirth. Fifty women recorded information on stillbirth experiences, and completed the Posttraumatic Stress Diagnostic Scale, General Health Questionnaire-28, Edinburgh Post-natal Depression Scale, Rotter’s Locus of Control Scale and the Posttraumatic Cognitions Inventory. 60, 28 and 12 % met the diagnostic criteria for probable full-PTSD, partial and no-PTSD respectively. Sixty-two percent and 54 % scored at or above the cutoff of the General Health Questionnaire-28 and postnatal depression respectively. Women who experienced stillbirth reported significantly more psychiatric co-morbid and post-natal depressive symptoms than the comparison group. Both groups were similar in locus of control. Women who experienced stillbirth reported negative cognitions about the self the most. After adjusting for postnatal depression, trauma characteristics were significantly correlated with Posttraumatic cognitions which, in turn, were significantly correlated with PTSD and psychiatric co-morbidity. Locus of control was not significantly correlated with psychological outcomes. Mediational analyses showed that negative cognitions about self mediated the relationship between trauma characteristics and psychiatric co-morbidity only. Women reported a high incidence of probable PTSD and co-morbid psychiatric symptoms following stillbirth. Stillbirth trauma characteristics influenced how they negatively perceived themselves. This then specifically influenced general psychological problems rather than PTSD symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttraumatic stress disorder following stillbirth (post-stillbirth PTSD) has been recognized in literature with the prevalent rates of 20 and 29 % for current and life-time PTSD. Psychiatric co-morbidities include depression and anxiety [1–4]. Risk factors include trauma characteristics: seeing or holding the stillborn infant [5], and a low level of social support [6–8]. Keeping mementos (e.g. a photograph) of the stillborn infant or attending the funeral did not relate to distress outcomes [4, 5].
In addition to trauma characteristics, according to a cognitive model of PTSD [9], individual vulnerability and negative appraisal cannot be neglected. Simply put, trauma characteristics and individual vulnerability create negative appraisals of the trauma which, in turn, trigger a sense of current threat accompanied by PTSD symptoms and co-morbid psychiatric responses. In other words, the relationship between individual vulnerability, trauma characteristics, PTSD symptoms and psychiatric co-morbidities is mediated by negative appraisals. This model, however, does not seem to emphasise personality traits as an individual vulnerability. Such neglect is surprising when personality traits have been shown to be intrinsic individual factors influencing biochemical processes and our perception of distress and illness [10, 11,12]. Also, the impact of personality traits on PTSD following unsuccessful pregnancy has been demonstrated [13].
Thus far, no systematic studies have looked at the link between locus of control, as a personality trait, post-stillbirth PTSD and psychiatric co-morbid symptoms. Briefly, according to Rotter [14], people with an internal locus of control tend to consider their own behaviour as being the cause of what happened to them. People with an external locus of control tend to think that control is out of their hands and that they are subject to fate, luck or other people. One study showed that women who lost infants through miscarriage blamed external sources (e.g. chance and powerful others) for their loss. Those with a previous experience of elective abortion tended to blame themselves (internal locus of control) for the miscarriage [15]. Locus of control would, in turn, be associated with post-stillbirth PTSD and co-morbid psychiatric symptoms. This is based on the link between internal and external attributions and distress among parents who lost infants through stillbirth, abortion and infant death [16].
The cognitive model of PTSD points to negative appraisals as a mediator for the relationship between individual vulnerability (locus of control in the current study), trauma characteristics and PTSD symptoms and psychiatric co-morbidity following stillbirth. To consider negative appraisals for the present study, we turn to posttraumatic cognitions characterized by negative self cognitions, negative world cognitions and self-blame [17]. The impact of posttraumatic cognitions on post-stillbirth PTSD and psychiatric co-morbidity has not been investigated. Meanwhile, they have been shown to predict PTSD symptoms following a range of other traumas [18]. Greater negative posttraumatic cognitions particularly about the self and the world were associated with greater PTSD and psychiatric co-morbid symptoms [19–23]. There was also a suggestion that these two negative cognitions mediated the severity of the trauma itself and PTSD symptoms [24].
Self-blame, on the other hand, has not been a consistent predictor to PTSD [20] and depression [21]. Among people who experienced different traumatic events, self-blame did not predict PTSD 3 months after the trauma [22]. That said, some studies have argued that self-blame was associated with a reduced risk of full-PTSD diagnosis and elevated PTSD symptoms [25] and with improvement in psychological adjustment [26].
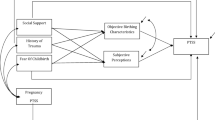
This study aimed to (1) re-affirm the incidence of probable PTSD and psychiatric co-morbidity among women who experienced stillbirth, and (2) investigate a model, informed by the preceding cognitive model of PTSD, depicting the interrelationship between locus of control (individual vulnerability), trauma characteristics of stillbirth, posttraumatic cognitions (negative appraisals), PTSD symptoms and co-morbid psychiatric symptoms following stillbirth. Therefore, for aim one, the hypothesis was:
-
H1: Women who had experienced stillbirth would report an incidence of probable PTSD comparable to that suggested in literature and a high level of co-morbid psychiatric symptoms.
For aim two, the hypotheses were:
-
H2: The trauma characteristics of holding the infant would be negatively associated with the severity of PTSD and co-morbid psychiatric symptoms; perceived lack of social support would be positively associated with the same outcomes, and keeping mementos and attending the funeral would not be associated with outcomes.
-
H3: Locus of control would be positively associated with the severity of PTSD and co-morbid psychiatric symptoms.
-
H4: Posttraumatic cognitions would mediate the relationship between trauma characteristics, the severity of PTSD and co-morbid psychiatric symptoms.
-
H5: Posttraumatic cognitions would mediate the relationship between locus of control and the severity of the same distress outcomes.
These are combined to form the path diagram shown in Fig. 1.
Method
Procedure
Two stillbirth support groups in the United Kingdom were contacted for the research. Upon their approval, the research was publicised on their newsletters and website. The inclusion criteria were listed as follows: (1) first time stillbirth, (2) spontaneous stillbirth after 24 week gestation based on United Kingdom stillbirth guidelines (NHS Choices), (3) no delivery of surviving twin, and (4) time of stillbirth at least 1 month prior to study. Fifty-four women responded but 4 were omitted on the grounds of not meeting the 24 week gestation. The rest were sent questionnaires with a letter explaining the purpose of the study, the ethical procedure, a consent form and a return address envelope. The questionnaires were those described in the measures section.
For comparison purposes, three mother and toddler groups in a local community in the United Kingdom were contacted. The organizers of the groups advertised the research in their weekly meetings with these criteria: (1) they had experienced a healthy birth and (2) had no previous experience of stillbirth, miscarriage, abortion, or neo-natal death. Fifty women volunteered and were sent the same questionnaires as the stillbirth group except the Posttraumatic Stress Diagnostic Scale and Posttraumatic Cognitions Inventory. A letter explaining the purpose of the study, the ethical procedure, a consent form and a return address envelope were also sent along with the questionnaires. The comparison data would help establish whether there was a greater incidence of psychiatric co-morbidity among women who experienced stillbirth than those who did not. Ethical approval from the University of Plymouth was granted for the study.
Measures
Demographic questionnaire
This questionnaire was composed of questions on age, marital status, ethnicity, educational level, and occupation for the stillbirth and comparison groups. For the stillbirth group, information on the number of children prior to and after stillbirth was recorded. It also recorded information on the gestation age, how long ago the stillbirth occurred and whether they experienced miscarriage, abortion and neo-natal death.
Stillbirth experience
Information was collected on trauma characteristics of stillbirth. Using a dichotomous scale (0 = no, 1 = yes), we recorded information on whether the women saw or held the baby following the stillbirth, whether they photographed or took another memento of the baby (e.g. footprint), whether they were given reasons for the stillbirth, whether they had a funeral or a cremation service for the baby, or whether they regularly visited the grave. We also collected data on whether they felt reluctant to have another baby, whether they were pregnant at the time of the study, whether they received support from partners, family members, or friends, or health professionals.
The Posttraumatic Stress Diagnostic Scale [27] was used to reach a diagnosis of probable PTSD focusing on the traumatic stillbirth experience. The PDS generates three sub-scales: re-experiencing, avoidance and hyperarousal. The reliability of the PDS scale is high (re-experience, Cronbach’s α = 0.78; avoidance, Cronbach’s α = 0.84; hyperarousal, Cronbach’s α = 0.84) and has shown good agreement with the Structured Clinical Interview for the DSM-III-R (SCID) (kappa = 0.65, agreement = 82 %, sensitivity = 0.89 and specificity = 0.75). On the basis of the current sample, Cronbach’s α for re-experiencing, avoidance and hyperarousal were 0.77, 0.82 and 0.90 respectively.
The General Health Questionnaire-28 [28] aims to estimate the likelihood of participants being diagnosed as suffering from general psychiatric morbidity at interview. The questionnaire yields four subscales which are somatic problems, anxiety, social dysfunction and depression. The GHQ-28 has shown a sensitivity value of 88 % at a specificity of 84.2 % and an overall misclassification rate of 14.5 %. Based on the current sample, Cronbach’s α for somatic problems, anxiety, social dysfunction and depression were 0.78, 0.90, 0.90 and 0.91 respectively.
Edinburgh Post-natal Depression Scale [29] is a 10–item scale measuring postnatal depression. Mothers who scored above 13 were likely to be suffering from depression of varying severity. With the cutoff scores of 12/13, the sensitivity and specificity scores were 75 and 84 respectively. Using the current sample, Cronbach’s α was 0.89 for the total score.
The Posttraumatic Cognitions Inventory [17] is a 36-item scale measuring trauma-related cognitions. It generates three sub-scales which are negative cognitions about self, negative cognitions about the world, and self-blame with Cronbach’s α of 0.97, 0.88 and 0.86 respectively. Using the current sample, Cronbach’s α were 0.95, 0.90 and 0.79 for the three sub-scales above.
Rotter’s Locus of Control Scale [14] measures the degree to which people believe that their own actions determine the rewards that they have obtained (internal locus of control) or that rewards in life are generally outside of their control. It consists of a 13-item forced-choice internal-external statement scale. Participants indicated their beliefs by choosing one of a pair of statements. Cronbach’s α ranged from 0.65 to 0.79. Test–retest reliabilities ranged from 0.49 for males (2 month interval) to 0.83 for females (1 month interval). On the basis of the present sample, the Cronbach’s score was 0.74.
Data analysis plan
Descriptive statistics were used to describe the trauma characteristics of stillbirth, the incidence of PTSD and posttraumatic cognitions. Chi square and t tests were used to compare the stillbirth and comparison groups in terms of demographic information, mean scores of postnatal depression, psychiatric co-morbidity and locus of control. Partial least squares (PLS) modelling was used to examine the hypothesized model. PLS has been used in recent PTSD research and described in detail e.g. [30–32]. Briefly, it can be used with modest sample sizes even for relatively complex models. One study used PLS modelling based on the sample size of 20 [33]. One criterion for estimating PLS sample sizes is ten times the largest number of structural paths going into a particular construct in the inner path model. The sample size for the current study met this criterion.
PLS generates outer and inner model estimates. The former examines the relationships between the latent variables and their observed indicators, while the latter examines the relationships between the independent and dependent latent variables. The indicators for the stillbirth trauma characteristics were formative while the others were reflective. Outer model estimates refer to the loadings or weights for each indicator and show how strongly it relates to the construct. Only reliable and valid indicators were used before looking at the linear relationship between constructs. For the constructs of postnatal depression and locus of control, three item and two item parcels were created as indicators respectively. Due to space constraint, the correlation matrix for the indicators used in the modelling was not shown but can be obtained upon request from the first author. Inner model estimates refer to the linear relationship between constructs by means of regression coefficients. PLS provides estimates of path coefficients in the model and tests whether these path coefficients differ significantly from zero using bootstrap resampling strategies. One thousand bootstrap samples were produced for this study. Mediational analyses were used based on the asymptotic and resampling strategies recommended by Preacher and Hayes [38].
Results
Fifty women who had experienced stillbirth participated in the study. With the given sample size of 50 and alpha set at 0.05, the study generated a power of 0.95 (critical F = 3.21). This was selected as a large effect size (f2 = 0.35) that would be important to detect, in the sense that any smaller effect would not be clinically or substantively significant. It was also assumed that this effect size was reasonable, in the sense that an effect of this magnitude could be anticipated in this field of research.
Compared with the 50 women who had not experienced stillbirth, the stillbirth group was significantly older. There were significant differences between the two groups in marital status and education. There was no significant difference in terms of income and almost all of the participants for both groups were of Caucasian origin (see Table 1).
Turning to the trauma characteristics of stillbirth, on average, gestation was 34 weeks (mean = 34.24, SD = 5.53) and stillbirth had occurred just over 3 and a half (mean = 44.76, SD = 33.16) years ago. Most women reported that during the stillbirth, they received support from spouse or partner (94 %), family members (82 %) and friends (94 %). A lesser proportion reported that they received support from midwives (52 %) and health visitors (32 %). Most women saw and/or held their dead infant (90 %), photographed their infant (94 %) and/or took their footprint and had a funeral (96 %) for them. A small proportion had a cremation service (16 %). Close to two-thirds of women visited the infant’s grave regularly (62 %). Less than a third were given a reason for the stillbirth (38 %). In terms of professional help, at the time of the study, less than 10 women were receiving medication from their family doctor, counselling or psychiatric intervention.
Focusing on aim one of the study, with regard to PTSD, 30 women (60 %) met the diagnostic criteria for probable full-PTSD; 14 (28 %) and 6 (12 %) women met the partial and no-PTSD criteria respectively. By partial, we mean those who met at least one symptom in each of the three PTSD symptom clusters [34].
Turning to psychiatric co-morbidity, women who experienced stillbirth reported more psychiatric co-morbid symptoms than the comparison group. In particular, they reported significantly more anxiety and depressive symptoms. Thirty-one (62 %) women who experienced stillbirth scored at or above the cutoff for GHQ-28, whilst 28 (56 %) of the comparison group scored or above the cutoff (odds ratio 1.28, 95 % CI 0.57–2.84, z = 0.61, ns). With regard to Post-natal depression, women who experienced stillbirth reported significantly more Post-natal depressive symptoms than the comparison group. Twenty-seven (54 %) women who experienced stillbirth scored at or above the cutoff for Edinburgh Post-natal Depression Scale whereas 9 (18 %) from the comparison group met the cutoff score. Odds ratio calculation suggested that women who experienced stillbirth were 5 times (odds ratio 5.34, 95 % CI 2.15–13.29, z = 3.60, p < 0.001) more likely to report postnatal depression than those from the comparison group. In terms of locus of control, there were no significant differences between groups. These women reported negative cognitions about the self the most followed by negative cognitions about the world. To a lesser degree, they blamed themselves for what happened.
To investigate aim two of the present study, partial least squares (PLS) modelling was carried out [35]. The correlations between constructs, composite reliability, average variance extracted, discriminant validity, communality and redundancy are shown in Table 2. The values of composite reliability and Cronbach’s alpha (except locus of control) were over the minimum threshold of 0.70 [36] indicating the reliability of these scales. The average variance extracted (AVE) for all constructs was above 0.50 indicating convergent validity of all the constructs. There was also evidence for satisfactory discriminant validity in that all the square root of AVE values were greater than the correlations between any of the paired constructs in the model.
The inner model results of the path coefficients for relationships between constructs were shown in the final PLS structural model depicted in Fig. 2. Prior to analysis, we examined whether demographic variables would serve as possible co-variates. The results showed that they were not significantly correlated with PTSD (age: r = −0.11, ns; marital status: rpb = 0.08, ns; educational level: rpb = −0.17, ns; income level: r = 0.03, ns) or psychiatric co-morbidity (age: r = −0.01, ns; marital status: rpb = 0.08, ns; educational level: rpb = 0.03, ns; income level: r = 0.12, ns). However, Post-natal depression was significantly correlated with PTSD (r = 0.66, p < 0.001) and psychiatric co-morbidity (r = 0.80, p < 0.001).
The results of the final PLS model with significant paths at 5 % or better (dotted arrows denote non-significant paths). Note: a = These are weight estimates. The rest are loadings. Time of stillbirth and receiving current professional help were the only valid formative indicators used for measuring trauma characteristics
Post-natal depression in the final PLS model analysis was controlled for. After controlling for the effects of Post-natal depression on PTSD (B = 0.45, SE = 0.12, t = 3.80, p < 0.01, 95 % CI 0.81–1.61, f2 = 0.75, a large effect) and psychiatric co-morbidity (B = 0.64, SE = 0.08, t = 7.49, p < 0.01, 95 % CI 1.73–2.69, f2 = 1.77, a large effect), trauma characteristics were significantly correlated with posttraumatic cognitions (B = 0.51, SE = 0.09, t = 5.61, p < 0.01, 95 % CI −0.64–0.07 f2 = 0.05, a small effect) which in turn were significantly correlated with PTSD (B = 0.25, SE = 0.10, t = 2.40, p < 0.05, 95 % CI 0.01–0.11, f2 = 0.14, close to a medium effect) and psychiatric co-morbidity (B = 0.23, SE = 0.09, t = 2.42, p < 0.05, 95 % CI 0.03–0.15, f2 = 0.20, a medium effect). The R2 values for the endogenous variables of posttraumatic cognitions, PTSD and psychiatric co-morbidity were 0.47, 0.50, and 0.76 respectively. These were moderate values except for 0.76 which was substantial. The average R2 was 0.29. Locus of control was not significantly correlated with psychological outcomes.
The GoF index was 0.47 which indicated an acceptable fit. One could conclude that the predictive relevance of this model was acceptable. Omission distance G = 30 blocks was used for the blindfolding analysis. The results showed that most of the blocks had high values for the communality index. This measured the quality of the measurement model for each block. They were over and above zero [37] and the average communality was 0.77. On the other hand, all the values for the redundancy index which measured the quality of the structural model for each endogenous block were lower, taking into account the measurement model. The average redundancy was 0.27.
The PLS results show that trauma characteristics influenced posttraumatic cognitions which, in turn, impacted on PTSD and psychiatric co-morbidity. In other words, posttraumatic cognitions mediated the relationship between trauma characteristics and psychological outcomes. To verify these mediational relationships, we used asymptotic and resampling strategies, recommended by Preacher and Hayes [38] for assessing indirect effects in multiple mediator models. For this analysis, we assessed posttraumatic cognitions as the mediators. These strategies would estimate the path coefficients in a mediator model and generate bootstrap confidence intervals (bias-corrected and accelerated) for testing total and specific indirect effects of X on Y through the mediators of posttraumatic cognitions. These strategies would control for the possible influence of covariates (postnatal depression) in the model. The bootstrap estimates were based on 1000 bootstrap samples. Point estimates and confidence intervals (95 %) were estimated for the indirect effects. The point estimate was considered to be significant when the confidence interval did not contain zero.
Analysing the relationship between trauma characteristics and PTSD/psychiatric co-morbidity through posttraumatic cognitions, the results showed that the total and direct effects of trauma characteristics on PTSD were −0.06 (SE = 0.03, t = −1.95, ns) and −0.04 (SE = 0.03, t = −1.47, ns) respectively. The difference between the total and direct effects was the total non-significant indirect effect through posttraumatic cognitions with the effect of −0.01 (Boot SE = 0.01, Boot LL 95 % BCa CI = −0.06, Boot UL 95 % BCa CI = 0.00). The results also showed that the total and direct effects of trauma characteristics on psychiatric co-morbidity were −0.03 (SE = 0.04, t = −0.79, ns) and −0.00 (SE = 0.03, t = −0.16, ns) respectively. The difference between the total and direct effects was the total significant indirect effect through posttraumatic cognitions with the effect of −0.02 (Boot SE = 0.01, Boot LL 95 % BCa CI = −0.07. Boot UL 95 % BCa CI = −0.00). Further analysis showed that of all the domains of posttraumatic cognitions, the significant mediator lay in negative cognitions about self. Both negative cognitions about the world and self-blame did not contribute to the indirect effect above and beyond negative cognitions about self (Table 3).
Discussion
This study examined the incidence of probable PTSD and psychiatric co-morbidity among women who experienced stillbirth and a hypothesized model describing the interrelationship between locus of control, trauma characteristics of stillbirth, posttraumatic cognitions, PTSD and co-morbid psychiatric symptoms. Sixty percent met the diagnostic criteria for probable full-PTSD and 62 % scored at or above the cutoff of GHQ-28. Partial least squares modelling showed that after controlling for postnatal depression, trauma characteristics were significantly correlated with posttraumatic cognitions which, in turn, were significantly correlated with PTSD and psychiatric co-morbidity. However, mediational analysis showed that posttraumatic cognitions, in particular, negative cognitions about self, mediated the relationship between trauma characteristics and psychiatric co-morbidity only. Locus of control was not significantly correlated with psychological outcomes.
Our findings confirmed hypothesis one in that women who had experienced stillbirth reported a high incidence of probable PTSD and a high level of co-morbid psychiatric symptoms. However, the incidence of probable PTSD in our study was much higher than that of literature [4]. This could be due to the different measures used to collect information on PTSD. In Turton et al’s study, the PTSD-I interview was used whereas in our study, the Posttraumatic Stress Diagnostic Scale (PDS), a self-report measure, was used. Also, these measures were based on different diagnostic criteria (DSM-III-R and DSM-IV). It has been argued that changes in diagnostic criteria could result in changes in the prevalence rate of PTSD [39].
The difference in incidence could also be due to individual differences between our samples. For example, the mean age of Turton’s sample was 29.7 (range 20–46); ours was older (35.86) (range 27–48). There is evidence suggesting that women of different ages display different levels of PTSD following a life threatening illness [40]. Traumatized community samples also revealed different age-related patterns for PTSD along with other psychological distress [41]. In addition to age, 62 % of Turton’s sample were Caucasian while almost all of ours were. This could have affected the incidence of probable PTSD since the link between ethnicity and PTSD has been established [42].
The present results echoed literature suggesting that women who experience stillbirth report co-morbid psychiatric symptoms [1, 4]. The fact that PTSD and other psychological problems co-exist is expected, since PTSD is not a discrete psychological syndrome. Instead, it is expressed through other psychiatric symptoms [43, 44]. The correlation matrix confirmed the strong correlations between PTSD and psychiatric co-morbidity (see Table 2).
Our results did not confirm hypothesis two. Trauma characteristics did not relate significantly to the severity of PTSD and co-morbid psychiatric symptoms. However, according to the PLS results, before adjusting for postnatal depression, trauma characteristics were significantly correlated with PTSD (path coefficients = 0.31) and psychiatric co-morbidity (path coefficients = 0.33). After controlling for postnatal depression, they dropped to 0.12 and 0.10 respectively. This suggested that postnatal depression accounted for much of the variance of trauma characteristics. This does not mean that trauma characteristics as predisposing factors can be ignored [45]. Rather, for women who experienced stillbirth, the aftermath postnatal depression played a major role in influencing PTSD and psychiatric co-morbid symptoms alongside trauma characteristics.
Focusing on trauma characteristics and consistent with literature [4, 5], the results reveal that keeping mementos or attending the funeral were not significantly correlated with distress outcomes (mementos: PTSD, r = −0.02, psychiatric co-morbidity, r = −0.12; funeral: PTSD, r = −0.09, psychiatric co-morbidity, r = −0.09), nor with trauma characteristics (i.e. reasons given for stillbirth, visiting grave and cremation service). Contrary to literature [5], however, seeing or holding the infant did not correlate significantly with outcomes. This contradicted good-practice guidelines suggesting that seeing or holding the dead infant for stillbirth parents would be related to grief processing and the reduction of PTSD symptoms [46]. Our research also contradicted the relationship between holding the dead infant and elevated distress for parents [5].
Arguably, the focus should be on memory sharing, rather than creating memory through holding the dead infant or keeping mementos. Memory sharing has been associated with PTSD symptoms [8]. This is not surprising given that sharing memories with others can be seen as part of the grieving process, helping the mother to come to terms with the loss, adjust her ambiguous identity (both the mother and not the mother) and integrate the experience of birth into the her life narrative. This kind of memory sharing likely involves processing the emotion associated with the memories rather than simply creating memories per se [8]. This is equivalent to a form of emotional processing therapy through which women articulate the disorganized trauma memory by sharing with others and consequently turn it into an organized and much reduced fragmented memory. This in turn was negatively associated with outcomes [47–49].
The current results did not support hypotheses three and five pertaining to the role of locus of control. We will return to hypothesis four later. Locus of control was not significantly correlated with PTSD and psychiatric co-morbidity before and after the adjustment of postnatal depression. Thus, the lack of mediational effect via posttraumatic cognitions for locus of control was expected. Whether women tended to interpret their own behaviour or fate or bad luck as being responsible for the stillbirth seemed to have little impact on distress outcomes. This contradicted findings on women who experienced miscarriage, stillbirth, abortion and infant death [15, 16] as well as those who experienced birth trauma [50].
Perhaps the main issue for these women is not about feeling responsible for the stillbirth or not (due to fate). Rather, what concerned them might be how they felt in terms of their ability to exercise control over events in their lives. In other words, it might be about powerlessness which is a dominant feature of a traumatized self [51]. Powerlessness or loss of control over their reproductive life has been highlighted among women who experienced pregnancy loss [15]. Such feelings of powerlessness over events tend to lead to a magnification of the severity of threats, anxiety and distress leading to impaired functioning [52, 53]. Had we measured women’s feelings of powerlessness instead of locus of control, the results might have been different.
Our results partly confirmed hypothesis four. After controlling for postnatal depression, posttraumatic cognitions (negative cognitions about self in particular) mediated the relationship between trauma characteristics and psychiatric co-morbid symptoms but not PTSD. In the light of the cognitive model of PTSD, the way these women processed the trauma was influenced by trauma characteristics but not individual vulnerability (their perception of whether events happened outside or within their control). They consequently created negative appraisals characterized especially in terms of negative cognitions about themselves which, in turn, specifically affected co-morbid psychiatric symptoms. On the other hand, negative cognitions about themselves did not carry the influence of stillbirth experience onto PTSD severity. Stillbirth experience affected PTSD independently of traumatic cognitions about oneself. This result that negative cognitions about self exerted the most direct influence on PTSD symptoms has added to existing literature [26].
It is noteworthy that self-blame was not a mediator for distress outcomes. This would not be surprising for some researchers [20–22]. One needs to be cautious, however, of coming to a conclusion about the role of self-blame. It was not that self-blame was not associated with PTSD or psychiatric co-morbidity, but rather that it was correlated significantly with both distress outcomes (PTSD, r = 0.39; psychiatric co-morbidity, r = 0.35). In other words, as discussed earlier, self-blame influenced distress outcomes independently of stillbirth experiences.
There were limitations in the present study. Firstly, although the sample size was acceptable for the current study, a bigger sample size could have made a difference to the results. Secondly, there was a sample bias since they were self-selected. Prior to the study, these women might have been somewhat symptomatic due to the fact that they sought help by providing support to each other. They might also have used this research as an opportunity to make sense of their experience. A sample bias could have affected the way they responded to the questionnaires. On the contrary, there might be other women who had a high degree of PTSD and therefore exhibited avoidance behaviour by avoiding the study. Finally, data on previous traumatic life events was not collected. As a result, we could not comment on whether PTSD from other traumas influenced the results. The impact of past trauma on outcomes is plausible given that 1 to 12 % of the general population have had PTSD at some point in their life [54]. Also, the impact of past trauma (e.g. sexual) on the mental health of women expecting their first baby has been demonstrated [55].
To conclude, following stillbirth, women reported PTSD and co-morbid psychiatric symptoms. Stillbirth trauma characteristics influenced the way in which they negatively perceived themselves which had an impact on general psychological problems rather than PTSD symptoms. These reactions cannot be understood independently of the effect of postnatal depression.
References
Engelhard IM, van den Hout MA, Arntz A.: Posttraumatic stress disorder after pregnancy loss. General Hospital Psychiatry 23:62–66, 2001.
Giannandrea SAM, Cerulli C, Anson E, Chaudron LH.: Increased risk for postpartum psychiatric disorders among women with past pregnancy loss. Journal of Women’s Health 22:760–768, 2013.
Turton P, Evans C, Hughes P.: Long-term psychosocial sequelae of stillbirth: Phase II of a nested case-control cohort study. Archives of Women’s Mental Health 12:35–41, 2009.
Turton P, Hughes P, Evans CDH, Fainman D.: Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. The British Journal of Psychiatry 178:556–560, 2001.
Hughes P, Turton P, Hopper E, Evans CDH.: Assessment of guidelines for good practice in psychosocial care of mothers after stillbirth: A cohort study. Lancet 360:114–18, 2002.
Cacciatore J.: Effects of support groups on post traumatic stress responses in women experiencing stillbirth. OMEGA. 55:71–90, 2007.
Cacciatore J, Schnebly S, Froen JF.: The effects of social support on maternal anxiety and depression after stillbirth. Health and Social Care in the Community 17:167–176, 2009.
Crawley R, Lomax S, Ayers S.: Recovering from stillbirth: the effects of making and sharing memories on maternal mental health. Journal of Reproductive and Infant Psychology 31:195–207, 2013.
Ehlers A, Clark DM.: A cognitive model of posttraumatic stress disorder. Behaviour Research Therapy 38:319–45, 2000.
Costa PT, McCrae RR. Personality: Another ‘hidden factor’ in stress research. Psychological Inquiry 1:22–24, 1990.
Clark LA, Watson D, Mineka S.: Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 103:103–116, 1994.
Miller MW.: Personality and the etiology and expression of PTSD: A three-factor model perspective. Clinical Psychology: Science and Practice 10:373–393, 2003.
Engelhard IM, van den Hout MA, Schouten EGW.: Neuroticism and low educational level predict the risk of posttraumatic stress disorder in women after miscarriage or stillbirth. General Hospital Psychiatry 28:414–417, 2006.
Rotter JB.: Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs 80:1–23, 1966.
Klock SC, Chang G, Hiley A, Hill J.: Psychological distress among women with recurrent spontaneous abortion. Psychosomatics 38:503–507, 1997.
Jind L.: Parents’ adjustment to late abortion, stillbirth or infant death: The role of causal attributions. Scandinavian Journal of Psychology 44:383–394, 2003.
Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM.: The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment 11:303–314, 1999.
Lancaster SL, Rodriguez BF, Weston R.: Path analysis examination of a cognitive model of PTSD. Behaviour Research and Therapy. 49:194–201, 2011.
Belsher BE, Ruzek JI, Bongar B, Cordova MJ.: Social constraints, posttraumatic cognitions, and posttraumatic stress disorder in treatment-seeking trauma survivors: Evidence for a social-cognitive processing model. Psychological Trauma: Theory, Research, Practice and Policy 4:386–391, 2012.
Cieslak R, Benight CC, Lehman VC.: Coping self-efficacy mediates the effects of negative cognitions on posttraumatic distress. Behaviour Research and Therapy 46:788–798, 2008.
Daie-Gabai A, Aderka IM, Allon-Schindel I, Foa EB, Gilboa-Schechtman E.: Posttraumatic cognitions inventory (PTCI): Psychometric properties and gender differences in an Israeli sample. Journal of Anxiety Disorders 25:266–271, 2011.
Su YJ, Chen SH.: A three-month prospective investigation of negative cognitions in predicting posttraumatic stress symptoms. The mediating role of traumatic memory quality. Chinese Journal of Psychology 50:167–186, 2008.
Blain LM, Galovski TE, Elwood LS, Meriac JP.: How does the posttraumatic cognitions inventory fit in a four-factor posttraumatic stress disorder world? An initial analysis. Psychological Trauma: Theory, Research, Practice and Policy 5:513–520, 2013.
Nixon RDV, Nishith P.: September 11 attacks: Prior interpersonal trauma, dysfunctional cognitions and trauma response in a Midwestern University Sample. Violence and Victims 20:471–480, 2005.
Startup M, Makgekgenene L, Webster R.: The role of self-blame for trauma as assessed by posttraumatic cognitions inventory (PTCI): A self-protective cognition? Behaviour Research and Therapy 45:395–403, 2007.
O’Donnell ML, Elliott P, Wolfgang BJ, Creamer M.: Posttraumatic appraisals in the development and persistence of posttraumatic stress symptoms. Journal of Traumatic Stress 20:173–182, 2007.
Foa EB, Cashman L, Jaycox L, Perry K.: The validation of a self-report measure of posttraumatic stress disorder. The posttraumatic diagnostic scale. Psychological Assessment 9:445–451, 1997.
Goldberg D, Hillier V.: A scaled version of the general health questionnaire. Psychological Medicine 9:139–145, 1979.
Cox JL, Holden JM, Sagovsky R.: Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry. 150:782–786, 1987.
Carpenter L, Chung MC.: Childhood trauma in obsessive compulsive disorder: The roles of alexithymia and attachment. Psychology and Psychotherapy: Theory, Research and Practice 84:367–388, 2011.
Chung MC, Dennis I, Berger Z, Jones R, Rudd H.: Posttraumatic stress disorder following myocardial infarction: Personality, coping and trauma exposure characteristics. International Journal of Psychiatry in Medicine 42:393–419, 2011.
Hunkin V, Chung MC.: Chronic idiopathic urticaria, psychological co-morbidity and posttraumatic stress: The impact of alexithymia and repression. Psychiatric Quarterly 83:431–447, 2012.
Chin WW, Newsted PR: Structural Equation Modelling Analysis with Small Samples Using Partial Least Squares. In: Hoyle R, (ed) Statistical Strategies for Small Sample Research. London, Sage, pp. 307–341, 1999.
Stein MB, Walker JR, Hazen AL, Forde DR.: Full and partial posttraumatic stress disorder: findings from a community survey. American Journal of Psychiatry 154:1114–11149, 1997.
Chin WW: PLS-Graph User’s Guide. Houston.: Bauer College of Business: University of Houston, 2001.
Nunnally JC, Bernstein IH: Psychometric Theory. New York, McCraw-Hill, 1994.
Fornell C, Cha J: Partial least squares. In: Bagozzi RP (Ed) Advanced Methods of Marketing Research. Cambridge, Basil Blackwell, pp. 52–78, 1994.
Preacher KJ, Hayes AF.: Asymptotic and resamplying strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40:879–891, 2008.
Calhoun PS, Hertzberg JS, Kirby AC, Dennis MF, Hair LP, Dedert EA, et al. The effect of draft DSM-V criteria on posttraumatic stress disorder prevalence. Depression and Anxiety 29:1032–1042, 2012.
Mosher CE, Danoff-Burg S.: A review of age differences in psychological adjustment to breast cancer. Journal of Psychosocial Oncology 23:101–114, 2005.
Scott SB.:A lifespan perspective on terrorism: Age differences in trajectories of response to 9/11. Developmental Psychology 49:986–998, 2013.
Macdonald A, Greene CJ, Torres JG, Frueh BC, Morland LA.: Concordance between clinician-assessed and self-reported symptoms of posttraumatic stress disorder across three ethnoracial groups. Psychological Trauma: Theory, Research, Practice, and Policy 5:201–208, 2013.
Miller MW, Kaloupek DG, Dillon AL, Keane TM.: Externalizing and internalizing subtypes of combat related PTSD: A replication and extension using the PSY-5 scales. Journal of Abnormal Psychology. 112:636–45, 2004.
Keane TM, Brief DJ, Pratt EM, Miller MW. Assessment of PTSD and its comorbidities in adults. In: Friedman MJ, Keane TM, Resick PA (Eds): Handbook of PTSD. New York, The Guilford Press, pp. 279–305, 2007.
Briere J: Psychological Assessment of Adult Posttraumatic Stress. Washington, DC: American Psychological Association, 2004.
Gravensteen IK, Helgadόttir LB, Jacobsen EM, Rådestad I, Sandset PM, Ekeberg O.: Women’s Experiences in Relation to Stillbirth and Risk Factors for Long-Term Post-Traumatic Stress Symptoms: A Retrospective Study. BMJ Open 3. doi:10.1136/bmjopen-2013-003323.
Amir N, Stafford J, Freshman MS, Foa FB.: Relationship between trauma narratives and trauma pathology. Journal of Traumatic Stress. 11:385–392, 1998.
Foa EB, Meadows EA: Psychosocial Treatments for Post-Traumatic Stress Disorder: A Critical Review. In: J.Spence, J.M.Darley, D.J.Foss (Eds) Psychosocial Treatments for Post-Traumatic Stress Disorder: A Critical Review. Palo Alto, CA: Annual Reviews, pp. 449–480, 1997.
Foa EB, Riggs DS. Posttraumatic Stress Disorder In Rape Victims. In: J.Oldham MBR, Tasman A (Eds) American Psychiatric Press Review of Psychiatry. Washington, DC, American Psychiatric Press, pp. 285–309, 1993.
Soet JE, Brack GA, DiIorio C.: Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth: Issues in Perinatal Care 30:36–46, 2003.
Brewin CR (Ed): Posttraumatic Stress Disorder: Malady or Myth? New Haven: Yale University Press, 2003.
Bandura A (Ed): Self-Efficacy. New York, W.H.Freeman & Company, 1997.
Benight CC, Bandura A.: Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy 42:1129–1148, 2004.
Norris FH, Slone LB. The Epidemiology of Trauma and PTSD. In: Friedman MJ, Keane TM, Resick PA (Eds): Handbook of PTSD. New York, The Guilford Press, pp. 78–98, 2007.
Hamama L, Rauch SAM, Sperlich M, Defever E, Seng JS.: Previous experience of spontaneous or elective abortion and risk for posttraumatic stress and depression during subsequent pregnancy. Depression and Anxiety 27:699–707, 2010.
Acknowledgments
We thank the women in this study for their participation which made this study possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicting interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was sought from patients before they commenced the study. Ethical approval for the present study was granted by the research committee at the University of Plymouth.
Rights and permissions
About this article
Cite this article
Chung, M.C., Reed, J. Posttraumatic Stress Disorder Following Stillbirth: Trauma Characteristics, Locus of Control, Posttraumatic Cognitions. Psychiatr Q 88, 307–321 (2017). https://doi.org/10.1007/s11126-016-9446-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-016-9446-y