Abstract
While recent national discussions of the Affordable Care Act (ACA) made the introduction of mandated contraceptive coverage within health insurance policies seem like a novel idea, it is not new at all. Since the late 1990s, 29 states have mandated that insurance providers include prescription contraceptive supplies and, in some instances, associated contraceptive services in their coverage. We use state-level policy variation to generate both difference-in-differences and triple difference estimates to determine if women in states with state-level contraception supply or contraception supply and services insurance mandates experienced changes in their utilization of contraception and preventive health care services. We find a positive relationship between these policies and prescription contraception use for those with low educational attainment, but the results are not robust to a variety of specifications. Our results also show an increase in the consumption of preventive health services for women with low educational attainment as a result of these health insurance mandates. We conclude by discussing the implications for the ACA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to reproductive as well as other gender-specific differences, women’s consumption of preventive healthcare services is often greater than their male counterparts (Asch et al. 2006; DHHS 2001). Moreover, women often require a unique set of preventive healthcare services, especially as it relates to their reproductive health. This increased demand for preventive services causes increased out-of-pocket expenditures for women (Bertakis et al. 2000; Kjerulff et al. 2007). Often out-of-pocket expenditures manifest in the form of insurance copayments and deductibles, and there is evidence that even modest copayments deter women—especially low income women—from consuming preventive services such as pap tests, mammograms (Solanki et al. 2000; Trivedi et al. 2010), and contraception (Kaiser Family Foundation 1998).
Women use oral contraceptives for many health related purposes, the most common of which is to prevent unintended pregnancy (Jones 2011).Footnote 1 While there is an array of contraceptive methods from which women may chose, there is variation in the cost and efficacy among available contraceptive options currently approved by the Food and Drug Administration (FDA), which are summarized in Table 1. Over-the-counter (OTC) methods are less expensive but are also often less efficacious in preventing pregnancy than prescription-only methods, which include relatively expensive barrier methods, hormonal methods, implanted devices, and sterilization. Understanding this variation, may help inform the need and rationale for policy interventions, such as insurance subsidies, intended to promote greater access to and use of contraception.
One such policy intervention is the Affordable Care Act (ACA), which now requires many health insurance plans to offer an array of preventive healthcare services to women with no cost sharing. Inclusion of FDA approved contraceptive drugs and devices and annual well-woman visits are two of the seven key preventive services contained within the reform.Footnote 2 The inclusion of a contraception provision in the ACA has garnered substantial public debate. Despite recent, national attention, this policy concept is not a new one. Since the late 1990s, 29 states have mandated (either through statute or administrative ruling) that when an insurance plan covers prescription drugs, it must also similarly cover prescription contraception (sometimes referred to as “contraception equity”). Additionally, among those 29 states, 19 require insurance policies to cover contraceptive services, which includes examinations and other services related to contraceptive use. Thus, mandates may expand contraceptive coverage in two important ways—by adding prescription contraceptives to the array of prescriptions covered or by reducing women’s financial responsibility by requiring equitable coverage.
To date, the effects of these mandates and the resulting expanded coverage are unknown, and this gap in the literature serves as our primary motivation for this paper. Specifically, we ask if mandated contraception coverage within private health insurance policies (1) alters the likelihood of using a variety of contraceptive choices and (2) affects complementary health services utilization, e.g., pap tests or pelvic examinations which are often performed when prescribing contraception for women in the United States (Henderson et al. 2010). Investigating the effects of state-level private health insurance mandates could inform the national debate by providing some evidence for the effects one might expect following implementation of the ACA.
Importantly, there are two key differences between the state mandates we study in this paper and the contraceptive mandates written into the ACA that have implications for current policy debates. First, the state mandates apply only to individuals with private insurance with a prescription drug benefit.Footnote 3 Furthermore, self-insured employers are legally excluded from state-level mandates by the federal Employee Retirement Income Security Act (ERISA) of 1974 as are certain employers due to religious exemptions.Footnote 4 To get some sense of the number of self-insured policies, Fronstin (2012) reports that in 1998, when the first state contraceptive mandate was implemented, about 41 % of all employer provided insurance coverage was self-insured.Footnote 5 In contrast, the contraceptive mandates that are part of the ACA will affect more insurance policies, and, by extension, more policyholders. A recent report from the Urban Institute (Buettgens et al. 2011) estimates that the ACA will reduce the number of uninsured Americans by about 28 million. Thus, while the contraceptive mandates we study have the potential to affect many women, the ACA will likely affect more.
Second, state mandates allowed cost sharing so long as the policyholder’s out-of-pocket expenses did not exceed the out-of-pocket expense related to prescription drugs or devices in a similar drug class or formulary. In contrast, the ACA does not allow any cost sharing. All else equal, the lower cost for contraception due to the ACA may induce a greater behavioral response from those covered. To the extent that the state-level mandates are able to predict the effect of the ACA, the estimates from state-level mandates may be conservative estimates.
While the implications of mandating prescription coverage—either via state mandates or the ACA—might seem to automatically imply increased use, the actual behavioral response is difficult to predict. If a woman’s out-of-pocket cost of contraception is reduced via an insurance subsidy, then one would expect her to increase her consumption of prescription contraception. In particular, if the cost prohibited her from using her preferred method, then following the receipt of insurance coverage, she might change to another form of contraception. However, ambiguity surrounding the predicted effect of the mandates arises when one considers the population most likely to be affected. The policy only changes the cost of contraception for those with private insurance, and most private insurance is provided through an employer. Women with insurance obtained through employment, all else equal, are likely to have higher education levels relative to women who do not have insurance or who have publically provided insurance. If true, then women with private insurance are probably more likely to use more effective methods of contraception to control their fertility (Martinez et al. 2013). While this could mean privately insured women would be particularly responsive to a policy that lowers the cost of contraception, it may also imply that these policies crowd-out privately financed contraception, i.e., that the women most likely to be affected by this policy are already privately financing their contraception because they have a relatively high and inelastic demand for contraception. Under these circumstances, mandates would ease women’s contraceptive financial burden, but would not lead to a change in their contraceptive use. One might also see null findings for these contraceptive mandates if a large number of health insurance policies already covered many forms of contraception when states implemented these policies.Footnote 6
Many health services are also tied to contraceptive use. In order to obtain prescription contraception, women must first see a health care provider. Therefore, mandates could facilitate increased interaction between women and the health care system, potentially improving women’s health more generally. In particular, one might expect to see an increase in other preventive services such as annual well-woman visits, pap tests, pelvic examinations, and counseling around more general sexual health issues. If contraceptive mandates act as a conduit for women’s consumption of other preventive services, then this would be an additional benefit of the policy.
Overall, we find weak evidence that women change their contraceptive consumption following the adoption of a contraception mandate: a positive effect that is not robust to a number of specifications. We do, however, find that women in states with mandates that cover contraceptive healthcare services are more likely to access services, such as pap tests and pelvic examinations. This paper proceeds in the following manner. In the “Literature Review” section, we overview the literature, and in the “State-Level Mandates” section, we provide detail about the health insurance mandates and the states that adopted them. Next, we describe our data in the “Data” section and our methods and empirical strategy in the “Methods” section. We present our results in the “Results” section and conclude in the “Discussion/Conclusion” section.
Literature Review
Much of the economic literature surrounding the topic of contraception investigates the relationship between improved access to contraception and contraceptive use.Footnote 7 This improved access may take the form of legalization, removing geographic barriers, educating consumers—especially young consumers, or lowering the price of contraception. This literature frequently shows that improved access to contraception leads to an increase in contraceptive use. Bailey (2006) uses variation in state consent laws to understand how the legalization of Enovid (the first birth control pill) changed the timing of births. She finds that legalization and the subsequent increased consumption of oral contraception led to delayed births and increased labor force participation. She notes that oral contraception (or “the pill”) was an attractive method of contraception in the 1960s because a woman could take the pill independent of her partner and long before she had intercourse. In addition, the pill was far more efficacious than other contraceptive methods available at the time. According to Cunningham et al. (2010), the pill remains one of the most efficacious forms of contraception (even when one factors in “typical” versus “perfect” use), and, therefore, one would expect improved access to prescription contraception to continue to be an attractive option for women seeking to control their fertility. Not all evidence points to an increase in contraceptive use with an increase in access, however. Recently, Joyce (2013a, b) has called some of the findings linking contraceptive access and increased use into question. He points out that the linkages, particularly between oral contraception and policy changes for minors’ access to this form of contraception are not robust due in part to the dearth of data on contraceptive use as well as the idiosyncratic data choices made by researchers.
A couple of studies use expansions of the Medicaid Family Planning Program to identify both effects on contraception and preventive health services consumption. Kearney and Levine (2009) employ the National Survey of Family Growth (NSFG) to assess the impact of state-level Medicaid family planning service expansions on contraceptive use and sexual frequency. They use demographic variables in the NSFG to help isolate the respondents most likely to be affected by the policy change. Following increased access to contraceptive supplies through Medicaid expansions, they find non-teen women increased their contraceptive use, while the estimates among teen women are imprecisely measured. Wherry (2013) asks if expansions of the family planning services component of Medicaid, which include preventive healthcare services, had any impact on the likelihood that women receive breast and cervical cancer screenings as well as tests for sexually transmitted infections among women. She uses data from the Behavioral Risk Factor Surveillance System from 1993 to 2009, and finds an increase in the likelihood of cervical cancer screening (approximately 19 %) and breast cancer screening (almost 15 %).
In a recent paper similar to ours, Bitler and Carpenter (2014) use a difference-in-differences model and the Behavioral Risk Factor Surveillance System (BRFSS) from 1988 to 2000 to investigate the relationship between insurance mandates for pap tests and utilization. They find that these mandates increase cervical cancer screening by about 1.5 % percentage points, with particularly strong effects for Hispanic and non-Hispanic white women.
More directly relevant, two recent studies ask about changes in contraceptive behaviors following the introduction of state-level private health insurance contraception mandates. Magnusson et al. (2012) show that privately insured women in contraceptive mandate states were more likely to use contraception consistently than women in nonmandate states using data from the 2006–2008 wave of the National Survey of Family Growth. Atkins and Bradford (2014) use the BRFSS surveys between 1998 and 2010 in their analysis. They restricted their sample to five states—two that implemented contraceptive mandates (Delaware and Iowa) and three that did not (Kentucky, Nebraska, and South Dakota)—that asked comprehensive information on family planning in the BRFSS during their study window. Atkins and Bradford first show that living in Delaware or Iowa after the insurance mandate was enacted is positively related to the likelihood of using an effective contraception method. Among those women who were using an effective method, living in Delaware or Iowa was positively associated with use of the pill, but unrelated to condoms or “other” prescription methods.
We build on this earlier literature and make several important contributions. First, like Magnusson et al. (2012), we use data from all states making our results more nationally representative. However, unlike Magnusson et al., we follow Atkins and Bradford, and use variation in the policy variable across time, i.e., before and after the contraceptive mandates, to identify policy effects. This helps us to account for pre-existing differences in the states and account for commonly experienced time shocks. In addition to incorporating some of the strengths of both studies, we add several new components. Neither previous study makes the distinction between states that mandate coverage of contraceptive supplies and states that mandate coverage of both supplies and services provided to accompany family planning (See next section for more detail). We argue that there are effectively two treatment groups among mandate states. Previous work lumps both treatment groups together. Because previous work does not make this distinction, neither investigated the impact these mandates had on preventive health services consumption. As we show below, these mandates have potentially important preventive health care benefits. In addition, we incorporate within state comparison groups into our analysis. If applied correctly, these comparisons remove potential bias from omitted variables that differ between mandate and nonmandate states.
State-Level Mandates
During the period we investigate in this study, 29 states have either a statute or administrative ruling requiring that private insurance policies that cover prescription drugs generally also cover prescription contraceptive drugs and devices that have been approved by the FDA.Footnote 8 The FDA approves both OTC contraception and methods requiring a prescription and/or administration by a healthcare professional. Although the mandates require insurance providers to cover the contraceptive methods approved by the FDA, policies will in practice cover a subset of the products in each category. For example, insurance companies subject to a mandate do not have to cover all oral contraceptives, but must cover a range of oral contraceptives and, consistent with contraceptive equity, policyholders cannot be billed more for their contraceptive prescription than another drug similarly situated in the prescription formulary.Footnote 9 These methods and relevant characteristics (i.e., likelihood of pregnancy with use, cost of contraception, cost of an initial exam, and if the method entails a service component beyond an annual exam) are summarized in Table 1. In reviewing Table 1, we see that the more efficacious methods are prescription methods. There are also notable cost differences. While prescription methods may be cost effective over time, they often require a larger upfront cost that may be prohibitive, especially among low-income women.
Table 1 also shows that prescription contraceptives include costs above the supply cost—what we refer to as “service” costs. The first service cost is that of the initial exam, which is necessary for a health care provider to prescribe medication. Depending on the type of contraceptive, this may be an annual exam or an exam that happens less frequently. According to Trussell et al. (2009), the Medicaid reimbursement rate for an initial gynecological exam is $40, but Davis and Carper (2009) use the medical expenditure panel survey (MEPS) and find the average cost for a gynecological office visit is $253. In addition, Table 1 indicates which contraceptive methods require additional services beyond the initial exam, such as insertion and administration.
To address the costs of these additional medical services, the majority (19 out of 29) of mandates also require insurance policies cover these related services. As an example, Arizona’s statute defines these services as the following:
“[O]utpatient contraceptive services” means consultations, examinations, procedures and medical services provided on an outpatient basis and related to the use of the United States food and drug prescription contraceptive methods to prevent unintended pregnancies. (Arizona Revised Statute 20-2329, 2003)
While each state created its own statute, the language concerning the services component is strikingly similar across states. The services component covers a wide range of health care expenses. Consultations and examinations includes medical consultations and advice regarding which method is best for the woman, pap tests and pelvic examinations to make sure the contraceptive device is safe and appropriate for a particular woman, and the administration or insertion of the contraception by a health care provider (often required for long-acting reversible contraception). Methods requiring this latter type of care are often more efficacious, and the services component may be especially valuable for women who prefer long-lasting reversible methods (injections, IUDs, implants) or methods that are meant to be permanent (sterilization). In many instances it would be hard for a woman to consume contraception without insurance coverage of the initial examination as well as the coverage of any administration or insertion costs. While most of the literature surrounding contraception cost and access has focused on the cost of the prescription, it seems highly likely that if the cost of contraception is prohibitive for many women, then the service fee is probably similarly prohibitive.
As previously explained, many women get a pap test or pelvic examination (outcomes that we include in our study) as a pre-cursor to their health care provider writing their contraception prescription. Supply and service mandates cover examinations and consultations related to contraceptive use, which would include these tests. In fact, one might view these services and contraception as complements since about 45 % of clinicians either always or usually require these examinations (Henderson et al. 2010). Therefore, insurance mandates, and, in particular, mandates that cover both supplies and services, could affect women’s health care consumption by encouraging women to switch from an OTC method to a prescription contraception method, encouraging women to switch to a prescription contraception method that requires a service beyond an examination (like an IUD), or encouraging women to retain their current contraceptive method but to begin to take advantage of pap tests or pelvic examinations that were previously cost prohibitive.
We also note that the contraceptive mandate legislation does not require women to actually consume contraception in order for her preventive health related services to be covered by her private insurance policy. Therefore, it is also possible that some women take advantage of the contraceptive service component of an insurance mandate without having to also consume contraceptive supplies. Thus, women, who in the past did not have insurance coverage for and therefore skipped or were not offered a pelvic exam, for instance, may now be more inclined to undertake the test or may be offered this test by the physician due to expanded insurance coverage.
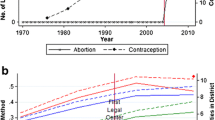
While we are interested in the effect of contraceptive mandates generally, we also recognize that there are two types of mandates which could be viewed as distinct policies. In our empirical strategy we will begin by looking at the overall effect of a state having either type of insurance mandate since there may be common effect regardless of the type of contraceptive mandate. However, we also disaggregate the mandates and define them as two distinct treatments recognizing that there may be a different relationship by mandate states. Table 2 classifies states by their mandate status—states without mandates (22 states, which includes DC), states mandating contraception supplies (10 states), and states mandating contraception supplies and related services (19 states)—and provides implementation dates for each state. One might ask if states with mandates have greater contraception coverage than states without the mandates. Work by Sonfield et al. (2004) compares contraceptive coverage among employer-provided insurance plans, and they find that insurance plans in states with mandates are 29–45 % percentage points more likely to include contraception coverage (their results are summarized in Fig. 1).Footnote 10 Of course, we do not know if this increased coverage is a response to mandates, if mandate states always had higher coverage, or if some other factor besides the mandates led to mandate states having higher coverage. Our work and identification strategy assumes that contraceptive coverage expanded after the mandates were enacted.Footnote 11
Do the Mandates Change Who has Private Insurance?
These mandates only affect women with private insurance, and therefore, it is important to determine what proportion of Americans have private health insurance. If this number is low, then one might not expect to see much of a policy effect simply because the number of women “treated” by the policy is quite small. Furthermore, the likelihood that someone has private health insurance may differ by education level. If high socioeconomic status women are the only individuals with private health insurance, for example, we may observe that women with private health insurance consume contraception at the same rates as before the mandate, they simply no longer have to pay for the contraception out-of-pocket, i.e., that there is no discernable contraception effect.
Figure 2 reports results from the March Current Population Survey (CPS) using data from 1989 through 2009 for all women aged 15–44 and for women by education level. These data show that a majority of women (68 %) have private health insurance regardless of their level of education. For women who have not completed high school, 53 % have private health insurance, and 61 % of high school graduates have private health insurance. For women with a college education, 87 % have private health insurance. Given the large proportion of women who are subject to the “treatment”, i.e., have private health insurance, we believe it reasonable to expect to identify health insurance mandate effects, should they exist.
We recognize that by selecting only women with private health insurance we are implicitly assuming that women do not purchase private health insurance coverage to take advantage of the contraception policy. As the cost of health insurance likely exceeds the cost of contraception, this assumption seems reasonable, but nevertheless, we employ an empirical test to examine our hypothesis. We used a state-level panel from 1989 through 2009 using data from the March CPS. We have a sample of women aged 15–44 in each year creating a total sample of over 780,000 women. We estimate the following linear probability model:
regressing an indicator for receipt of private health insurance on an indicator for women who reside in states with contraceptive supplies mandates (CS) and an indicator for women who reside in states with contraceptive supplies and services mandates (CSS). The vector X includes a set of indicators for race/ethnicity and a set for age as well as an indicator if the respondent was married; a linear measure of the individual’s educational attainment and number of children (0, 1, 2 or more); the state poverty rate; and the state unemployment rate. We also include state and time fixed effects, and show results both with and without linear state-time trends in Table 3.
In the first two columns, we report the association between the health insurance mandates and the likelihood that an individual has private health insurance only. In columns three and four, we include those individuals who have private health insurance combined with some form of public health insurance. The coefficient for supply states is positively related to the health insurance outcomes in all of the models, but the estimate is never statistically significant at the 0.05 level. With respect to the supply and service states, not only is the estimate statistically insignificant and small in every model, it is negative in in three of the four models. We interpret these results to imply that the assumption is certainly plausible for both type of states, but especially the contraceptive supplies and services states.Footnote 12
Another potential threat to our research design is that upon passage of contraceptive mandates, firms either self-insure or drop health insurance from their employee benefits in order to avoid compliance. Previous evidence by Gruber (1994) finds that few firms adjust in this way. Furthermore, such scenarios seem unlikely when one considers the cost of compliance relative to the alternatives. A DHHS (2012) brief provides a review of actuarial studies showing that the cost of adding contraceptive coverage does not add more than approximately 0.5 % to premiums and likely has cost savings beyond this due to averting unintended pregnancies.
Data
Our data regarding contraception use and preventive health services come from the National Survey of Family Growth (NSFG).Footnote 13 We use data from the 1995, 2002, and 2006–2010 survey waves, which contain 10,847, 7,643, and 12,279 female respondents respectively, effectively creating a repeated cross-section with varying intervals between observations. Since some groups are oversampled, we employ sampling weights to produce representative statistics. State identifiers are suppressed in the public use files, but identifiers are available to researchers approved by the National Center for Health Statistics via a Census Research Data Center.
The NSFG asks several questions that allow us to measure changes in women’s contraceptive consumption. The survey asks women what method of contraception (condoms, oral contraceptives, injectables, natural family planning, etc.) they used during their last sexual intercourse act.Footnote 14 Women are allowed to select up to four types of contraception (for example, a woman might use birth control pills to protect against pregnancy and a condom to protect against STD/Is). We used this information to construct several outcome variables, which all take the form of dummy variables. As a woman can employ multiple forms of contraception during intercourse, the contraceptive use variables are not mutually exclusive. The first is a variable equal to one if a woman uses a contraceptive method that relies on OTC methods (such as condoms or spermicides) or natural methods (such as the calendar method, rhythm method, or withdrawal method) and zero otherwise. The next is a variable equal to one if a woman uses a method that requires a prescription but does not require an additional health service (such as oral contraception and other hormonal methods like patches) and zero otherwise. We also constructed a variable equal to one if a woman uses a contraceptive method that would require a health service (such as IUD implantation, a diaphragm fitting, etc.) and zero otherwise. Next, we created a variable which combines the latter two variables and thus is equal to one if a woman uses any type of prescription contraception and zero otherwise. Women who were not sexually active are included in the models, largely because they may consume contraception, particularly oral contraception, for reasons other than pregnancy prevention. We do not want to ignore the potential for these mandates to affect these women.
In addition, the survey asks women about their consumption of sexual health services. We are interested in three measures of sexual health—as we believe women who are seeking prescription contraception are likely to obtain these services during their annual exam (a frequent pre-cursor to contraception). In particular, the NSFG asks women if they had a pap test, pelvic exam, and/or a test for a venereal disease or sexually transmitted infection (STD/I) within the last 12 months.Footnote 15 As before, with each of the three services we create three distinct variables equal to one if the woman had the service and zero otherwise.
Finally, the survey also collects a range of individual level demographic variables. We are able to control for the respondent’s age,Footnote 16 and we created indicator variables to control for her religion (no religion stated, protestant, Catholic, and other religious preference), education (less than high school, high school or GED, some college, and college or college and beyond), race (white, non-Hispanic, black, non-Hispanic, other, non-Hispanic, and Hispanic), and marital status (married, single, a collapsed category of separated, divorced and widowed). We also controlled for state level income and postpartum duration Medicaid eligibility expansions updated from Kearney and Levine (2009). Finally, the data identifies the respondent’s insurance status, which we use for sample selection and treatment assignment in our models. Respondents are asked a series of questions to identify what type of, if any, health insurance they had in the past 12 months. Approximately 5–8 % of respondents fell into more than one insurance category, for example they were covered by both Medicaid and private insurance in the past 12 months. In our main results, these respondents are treated as privately insured. As a sensitivity check, we also dropped those who stated they were covered by more than one type of insurance, and the results are unchanged.
We used three sources to collect the state mandate variable: the Guttmacher Institute, the National Council of State Legislatures (NCSL), and a review of each state statute (retrieved through WestLaw). The Guttmacher Institute classifies each state mandate as a “supplies” mandate or a “supplies and services” mandate. Our own reading of the statutes almost always agreed with the Guttmacher Institute’s interpretation of the statute.Footnote 17 The main benefit of consulting the state statutes was to collect the “effective” date of the policies. While statutes were enacted in a given year, many states allowed insurers 6 months to a year before they were required to cover contraceptive supplies or services. We consider this latter date to be the effective date. We consider women in mandate states whose date of interview occurs after the effective date to be “treated” by the mandate.
Methods
To estimate the effect of the mandates on women’s contraceptive consumption and consumption of health care services, we use a difference-in-differences (DD) model. We start by estimating the effect of a state having a contraception mandate. Women in non-mandate states serve as a comparison group. In our DD models, we only include women with private insurance, as these are the women most likely to be affected by the policy change. The DD model will reveal the mean difference in the probability that women with private health insurance in mandate states will use a particular contraception or consume a particular health service relative to women with private health insurance in states without a mandate. Our regression model can be expressed as follows:
where Y is equal to one of the outcome variables previously described (either her contraceptive method or health care service consumption), α s is a state fixed effect, and θ t is a time fixed effect, which is characterized by the survey year. The vector X represents a set of control variables, including the respondent’s age, race, religion, marital status, and if her state has passed a Medicaid eligibility expansion.Footnote 18 We also report results with (λ s * survey year) and without state level linear time trends, in order to show the difference between our baseline and preferred (with trends) model.Footnote 19 The model with trends identifies the post mandate effect using residual variation after one controls for the state-specific trend in the outcome. As such, this is potentially a more stringent requirement when identifying the mandate estimates. We run models for all contraceptive outcomes and all health service outcomes for our sample of privately insured women.
We were also interested in disaggregating the mandates to reflect that that two potential treatment groups exist: women who reside in states with contraceptive supplies (CS) mandates and women who reside in states with contraceptive supplies and services (CSS) mandates. After investigating the effect of any mandate, we then run the following regression model:
The coefficients for CS and CSS are difference-in-differences (DD) estimates, and as before women in states without a mandate are the reference group, and all other parameters are the same as those in Eq. 3. Descriptive statistics for the sample of privately insured women can be found in Table 4.
Because women with low educational attainment may have larger behavioral responses than women with high educational attainment due to the relatively high cost of prescription contraception and preventive health services, we also disaggregate our estimates by women’s educational attainment. We define women with low educational attainment as those whose highest level of educational attainment is a high school diploma or equivalency or less. High educational attainment women completed some college, have a college degree, or completed some graduate-level education.
While comparing women with private health insurance in states with a mandate to women in states without a mandate can be informative, an appropriate within state control group would be ideal as it would potentially reduce omitted variable bias that could arise from other state policies or other health care initiatives that affect all women within the same state. We selected women that do not have private insurance as our within state control group, and also estimate a difference-in-difference-in-differences model (DDD). This model asks if the difference in the outcome among privately insured and non-privately insured women in mandate states is any different from the difference in the outcome among privately insured and non-privately insured women in non-mandate states. The identification in this model is conditioned on the validity of women without private insurance serving as an appropriate counterfactual for women with private insurance. For example, states with contraception mandates may have public health care campaigns that encourage all women to increase their preventive health care. Observing an increase in preventive health care among women in these states may not be due to the health insurance mandates but instead due to the public messages. By comparing women within the same state, any differences observed within state cannot be due to the intrastate message effects or any other factors common to women within the same state. As before, we begin by assessing the impact of an aggregate measure of the contraceptive mandate, then investigate if the type of mandate affects contraceptive or preventive care consumption. In all models, we cluster the standard error at the state level to correct for serial correlation.
Results
Contraceptive Outcomes
We first describe how the mandates affect women’s choice of contraception. In particular, we ask if the mandates changed the probability women use OTC methods, prescription methods that do not require a service (mainly hormonal methods), prescription methods that do require a service, or any type of prescription method.
The top panel of Table 5 provides results from a model with and without state specific linear time trends. Among all privately insured women, having any mandate does not appear to have an effect on contraceptive use.Footnote 20 The estimates imply small changes, and all are statistically insignificant. We then disaggregate the mandates to understand if this effect is dependent on the type of mandate available to a woman. Overall, the results are the same with one exception: women with private health insurance are 3 % percentage points less likely to use OTC methods than women in non-mandate states after the mandates were implemented. This difference is statistically significant at the 0.05 level. One would expect this reduction in OTC methods, assuming a constant level of contraceptive use, would translate into increases in prescription methods that are covered. While coefficient estimates for prescription methods (those not requiring and those requiring a service) are positive, neither model yields a significant estimate.
The lower panel of Table 5 disaggregates respondents into low (less than or equal to high school completion) and high levels (more education than high school completion) of education. As before, we start by looking at the effect of a state having either type of mandate, and these results suggest that women with low educational attainment are more responsive to the contraceptive mandates when compared to women with higher levels of education. Following the implementation of the contraceptive mandates, there was an eight percentage point increase in the use of prescription contraceptive methods, and this estimate is statistically significant. We observe no change in the contraceptive behavior of women with high educational attainment.
When we disaggregate the “treatment” into CS and CSS states, we find a statistically significant three percentage point reduction in the use of OTC/natural methods in the CSS states among those with low levels of education. This change was accompanied by increases in the use of prescription contraception, but none of these estimates is statistically significant. We also show that the positive estimate for prescription contraception among low education women is driven by those in CS states, who are approximately 15 percentage points more likely to use a contraceptive method which requires a prescription. Moreover, this change seems to be isolated to an increase in pill or hormonal methods, or methods that do not require an additional service component.
As explained earlier, we are concerned that the DD models suffer from bias due to factors that are different between mandate and nonmandate states that are not accounted for in our models. Next, we employ a DDD model, which utilizes within state variation to identify mandate effects, and our results pertaining to contraceptive use can be found in Table 6.Footnote 21 Interestingly, once we compare the changes for women with private insurance in mandate versus nonmandate states to women without private insurance, we do not find a statistically significant change in the use of contraceptive outcome methods, regardless of type of mandate. Disaggregating the models by women’s educational attainment does not reveal different responses either, and in particular the effects from the DD model among women with low educational attainment in CS states disappear. This result suggests that women without private insurance in CS states also increased their prescription contraceptive use. In summary, we do not find consistent evidence of a contraception effect created by these private insurance contraceptive mandates.
Health Services Outcomes
We also investigate if the mandates led to an increase in health care utilization, and in particular, we observe if there were changes in the likelihood that a woman received a pap test, pelvic exam, or STI/D test in the past 12 months. As before, we start by presenting results from our DD model and then move into results from the DDD model.
Table 7 shows our findings from the DD model. Overall in the top panel, we do not observe a statistically significant change in health care utilization following a mandate once we control for state-specific time trends, although all of the estimates for CSS states are positive. Once we separate the sample into low education and high education women, we do find a positive estimate for the pap test outcome that, while statistically insignificant at the 0.05 level, is measured with some precision. Once we disaggregate the treatments, we continue to observe positive estimates for the pap test, but none is statistically significant. The other coefficient estimates for the education subgroups are also statistically insignificant and usually much smaller in magnitude.
When we estimate the DDD model (results presented in top panel of Table 8), we see no significant change in health service consumption following the adoption of any mandate—though we note the coefficients are all positive. Upon disaggregating the mandate states, we see that women in CS mandate states do not increase their health services consumption following the mandate. The coefficients are both small and insignificant. This result is expected, as the CS mandate does not alter the cost of services in any meaningful way. In contrast, women in CSS states do alter their health services consumption. We observe a 10.4 percentage point increase in pap tests (a 15.9 % increase over the sample mean), and an 8.1 percentage point increase in pelvic examinations (a 12.8 % increase over the sample mean).
The bottom panel of Table 8 provides nuance to this finding. The increases in preventive health care services appears to be concentrated among women who have low levels of education and who have private health insurance. Given that these services can be expensive, it is not unexpected that we see the beneficial impacts of this program among low socioeconomic status women. As we do not see a corresponding change in the women’s contraceptive choice, these results suggest that low socioeconomic status women who are were already consuming contraception are now able to add preventive health services to their health care routine. Additionally, we find no change in STD/I testing regardless of socioeconomic status. Perhaps this is not surprising: those women at highest risk of STD/Is are young, may not have private health insurance, struggle financially (Gonzalez et al. 2009, Laumann and Youm 1999), and often do not have access to quality sexual or health services (Eng and Butler 1997), all of which imply low access to employer provided health insurance.
As we compare the DDD coefficient estimates to the DD estimates, we do not see an appreciably different estimate for the pap test outcome, with the exception that the DD coefficient was not statistically significant at the 0.05 level. Both the DD results and the DDD models show an increase in the likelihood of a pap test following the contraceptive mandates among low education women. For the pelvic exam outcome, the DD models indicate women in states with and without mandates had similar patterns of health service consumption, regardless of the mandate type. In contrast, our DDD models demonstrate a relative increase in health service consumption of low education women in CSS. The difference in the result is clearly driven by a relative decline in pelvic exam consumption by women without private insurance in CSS states.
Discussion/Conclusion
The ACA has generated considerable discussion among policymakers, and mandated contraception coverage has been one of the biggest sources of concern within the public debates of the ACA. Given the acrimony over this feature of the legislation, one might think that the mandated contraceptive coverage was an idea legislators were considering for the first time; however, mandated contraception coverage is not a new policy at all. Since the 1990s, 29 states have implemented policies that require health care providers cover contraception in their health care insurance policies that include other prescription drug benefits. Our objective in this paper was to estimate the impact of these health insurance mandates on contraceptive use and preventive health care among American women. We also believe the results from this policy analysis should inform the debates surrounding the contraceptive coverage in the ACA.
Using three different panels of the NSFG, we have a couple of findings related to the contraception outcome First, our results consistently show that these health insurance mandates have no statistically discernible effect on the contraceptive behavior of women with high education levels. Second, we find some evidence that contraceptive mandates may have lowered the use of OTC/natural methods for low-education women in CSS states and increased the use of oral contraception or other hormonal methods for low-education women. However, these results only surfaced in the DD models. When we compared the trends for the contraceptive use of privately insured women to the trends for women without private insurance, they were very similar. In sum, we do not find a robust contraception effect in our data.
A number of plausible explanations for this finding exist. First, these state mandates did not apply to self-insured private insurance, which constitutes a large proportion of employer sponsored plans. In addition, evidence from Sonfield et al. (2004) suggests that many private health insurance policies already covered contraception when many of the mandates were implemented, which limits the impact of the mandates regardless of a woman’s socioeconomic status or educational attainment. Second, women may have maintained their contraceptive practices after the implementation of this policy, but simply stopped paying for them out-of-pocket and used their health insurance policy to fund their consumption. The fact that we see no evidence in the DD or DDD models for women with high education levels is consistent with this explanation. Our data do not let us track individual-level contraception use or forms of payment for the contraception. Future work utilizing individual level data on type of contraception and method of payment may provide important insights into this issue.
We do find evidence that women with low educational attainment who are in states with mandates that require coverage of both contraceptive supplies and as well as supplemental preventive healthcare services became more likely to obtain preventive healthcare services. It is possible that women with low educational attainment may particularly benefit from contraceptive mandates because they may have lower incomes, making the insurance subsidy more beneficial for them. Also, we expect that on average women with lower educational attainment have less comprehensive private insurance coverage, which are precisely the plans that would have needed to expand their coverage following the adoption of the mandates.
In particular, we find an increase in pap tests among women with low educational attainment in both the DD models and the DDD models, although the estimate are only statistically significant in the DDD models. We also find a statistically significant increase in pelvic exams among low-education women in CSS states in the DDD models. Specifically, we find a nearly 16 % increase in the likelihood that women with private insurance received a pap test and 13 % increase in the likelihood of a pelvic exam in the past year for women with low education levels. While large, these estimates are similar to those reported by Wherry (2013) in her study of Medicaid expansions for the same time period.
While informative, this study does have several limitations. We would have benefitted from a data source with greater variation across time in contraception use and preventive health care services. We utilize the changes across three different cohorts of the NSFG to identify effects, but annual variation from a period, such as from 1995 to 2010, would have been preferable. With more variation to explain, our point estimates would likely have been more precise and our contraception results potentially more robust. Furthermore, we could have tested the validity of our research design by comparing trends between the comparison and treatment groups in the period prior to the implementation of the contraceptive mandates. To the best of our knowledge, the NSFG is the only data source with samples that allow one to explicitly track contraception use and identify the respondents’ state of residence over the observation window when contraceptive mandates were being implemented. Other researchers have commented on the lack of data on contraception use over time (Bailey et al. 2013; Joyce 2013a). We would also have preferred to test for differences by race. The small sample sizes by race particularly once disaggregated by education level within states made these separate analyses untenable.
Despite these limitations, we do find evidence that mandating that private health insurance policies cover contraception and health care services likely increased women’s consumption of preventive health care. Our findings have implications for the ACA, especially since the contraception mandate in the ACA includes provisions for women’s preventive health care that are most similar to the contraceptive mandates in the CSS states. First, the ACA mandates coverage of all FDA approved contraceptive methods, cervical cancer testing, as well as a large number of other preventive health screenings. Accordingly, one may observe a general increase in women’s health. Second, since the ACA expands coverage to a large number of uninsured Americans, primarily in the lower portion of the income distribution (Buettgens et al. 2011), one might find large improvements in population health since this is similar to the population that appeared to benefit from the state contraception mandates. Finally, while we did not observe this phenomenon in our data, it is plausible that these contraceptive mandates changed the funding source for contraception for high socioeconomic status women. Instead of these women paying for prescription contraception and the affiliated services out-of-pocket, their private health insurance policies may now fund their contraception. In the future, researchers with more detailed data on contraception payment might seek to observe if there has been a change in the funding source for prescription contraception among high socioeconomic status women. The ACA could have generated prescription equity across the income distribution.
Notes
Fifty-six percent of oral contraceptive users also cite non-contraceptive health benefits as a reason for use (Jones 2011).
The other main preventive services included in the legislation are screening for gestational diabetes, Human Pappilomavirus DNA testing, domestic violence screening and counseling, HIV screening and counseling for sexually transmitted infections and diseases, and breastfeeding supplies.
This provision does not likely exclude many plans from the mandate. A 2011 Department of Labor report estimates that almost all plans include prescription medications in their insurance plans.
At present, the extent to which the ACA will allow for religious exemptions is unclear due to pending legal actions in various federal courts.
We note, however, that while a plan may be legally excluded from the mandate, there may be pressure to cover contraception supplies and related services if competing policies within the state are extending this coverage (Sonfield and Gold 2004).
We were not able to find direct evidence regarding how many policies covered prescription contraception prior to mandate adoption. Sonfield et al. (2004) find that 86 % of health insurance providers who responded to their survey reported covering the five most common forms of prescription contraception in their policies when asked in 2002. Unfortunately, these data were collected after several states had implemented the mandates, and the survey had a very low response rate (53 %).
We recognize that other disciplines, namely sociology and psychology, also research questions concerning contraceptive use and access. We examine the economic literature because it is most similar to the current study.
The mandate was issued via an administrative ruling in Michigan and an attorney general opinion in Montana. In both states, the ruling found that failing to cover contraception differentially affected women, as only women can become pregnant. The rulings argue failure to cover contraception violates women’s civil rights under Title VII.
Some mandates expressly exclude coverage of abortifacients, making coverage an option for the insurance plan but not required by law. No abortifacient is listed as a contraceptive option in our data.
Sonfield et al. (2004) detail the difficulty they had fielding their study. They report a response rate of 53 % once they made several accommodations to the data collection.
We are not aware of a data set that would allow us to formally test this assumption.
The lack of evidence for policy endogeneity in states with a mandate to cover both supplies and services is particularly relevant given that our strongest results are seen in the states that cover both.
More information about the NSFG can be found on the CDC’s website: http://www.cdc.gov/nchs/nsfg/about_nsfg.htm.
The NSFG does not specify the timing of the last sex act. For the majority of respondents, those who were interviewed before a mandate change or well after a mandate change, or who resided in a nonmandate state, this should not create a problem for our results. There were seven states that implemented a mandate near the time of the NSFG interviews: Michigan, Montana, New Jersey, Oregon, Texas, Washington, and Wisconsin. To the extent that respondents from these states may have been classified as being in the “treatment group” (i.e., in post period) when they had their last sex act in the pre period, our results will be attenuated.
Other outcomes, such as breast exams, were asked in various surveys but none was asked continuously making them impractical for our analyses.
We also run model where we drop the women 19 years of age and younger. For a variety of reasons, these women may not take-up the mandates (for example, they may be on their parent’s insurance or may be unaware of mandates). Estimates from these models are nearly identical to the results presented in the paper.
One exception is the classification of Missouri. We do not consider Missouri to be a mandate state, but the Guttmacher Institute and National College of State Legislatures does. We regard a state to be a mandate state when the mandate achieves contraceptive equity, which occurs when any plan covering prescription drugs must also cover prescription contraceptives. However, Missouri’s mandate only applies to policies that cover obstetrical and gynecological benefits AND pharmaceutical coverage. While nearly all plans include pharmaceutical coverage, fewer than 60 % included obstetrical and gynecological benefits in 2010 (Department of Labor 2011). Our decision to categorize Missouri as a control state likely attenuates our treatment effect.
Bitler and Carpenter’s recent work (2014) on mandated pap test coverage suggests that we might also want to control for the implementation of this policy. We carefully compared the start and stop times for the pap test mandates to the contraceptive mandates in all states and the District of Columbia. Twenty-four states never implemented a pap test mandate and 10 states that did implement a pap test mandate, did not implement a contraceptive mandate. These 34 states should not affect our results. In states that implemented both policies, 15 implemented the pap test mandate at least four years before the contraceptive mandates, thus the pap test mandate contributes to the pre period for our models only. One state, Colorado implemented changes after the window of our study. Only one state, Texas, implemented both mandates and the pap test mandate occurred after the contraceptive mandate. Observations from this one state are a potential source of bias, albeit small, for our results.
The state specific trends control for linear trends in the dependent variable. We use linear trends as we do not have enough time periods to include quadratic or other non-linear forms.
While we would prefer to estimate these models by race/ethnicity, due to very small subgroups, we are only able to perform these analyses for all racial groups combined.
We do not include state-specific time trends in the DDD models. This specification did not converge in our models. We did however, run DD models with state-specific time trends for those with private insurance and those without private insurance. We used the difference in mandate coefficients as an approximation for the DDD results. All DDD approximations were similar to the coefficient reported.
References
Arizona revised statutes title 20—insurance§ 20-2329 prescription contraceptive drugs and devices; definition. (2003). Justia Law. Retrieved February 23, 2014 from http://law.justia.com/codes/arizona/2013/title-20/section-20-2329.
Asch, S. M., Kerr, E. A., Keesey, J., Adams, J. L., Setodji, C. M., Malik, S., & McGlynn, E. A. (2006). Who is at greatest risk for receiving poor-quality health care? New England Journal of Medicine, 354(11), 1147–1156.
Atkins, D. N., & Bradford, W. D. (2014). Changes in state prescription contraception mandates for insurers: The effect of women’s contraceptive use. Perspectives on Sexual and Reproductive Health, 46(1), 23–29.
Bailey, M. J. (2006). More power to the pill: The impact of contraceptive freedom on women’s life cycle labor supply. The Quarterly Journal of Economics, 121(1), 289–320.
Bailey, M. J., Guldi, M., & Hershbein, B. J. (2013). Further evidence on the internal validity of the early legal access research design. Journal of Policy Analysis and Management, 32(4), 899–904.
Bertakis, K. D., Azari, R., Helms, L. J., Callahan, E. J., & Robbins, J. A. (2000). Gender differences in the utilization of health care services. The Journal of Family Practice, 49(2), 147–152.
Bitler, M. P. & Carpenter, C. S. (2014). The effects of state cervical cancer insurance mandates on pap test rates. Unpublished manuscript.
Buettgens, M., Holahan, J., & Carroll, C. (2011). Health reform across states: Increased insurance coverage and federal spending on the exchange and Medicaid. Retrieved September 17, 2014, from http://www.urban.org/uploadedpdf/412310-Health-Reform-Across-the-States.pdf.
Cunningham, F. G., Leveno, K. J., Bloom, S. L., Hauth, J. C., Rouse, D. J., & Spong, C. Y. (2010). Williams obstetrics. New York: McGraw-Hill Medical. Planned Parenthood website: http://www.plannedparenthood.org/health-topics/birth-control-4211.htm
Davis, K. E., & Carper, K. (2009). Statistical briefing #381: “Use and Expenses for office-based physician visits by specialty, 2009: Estimates for the U.S. civilian noninstitutionalized population.” Retrieved September 9, 2014, from http://meps.ahrq.gov/data_files/publications/st381/stat381.shtml.
Department of Health and Human Services. (2001). Utilization of ambulatory medical care by women: United States, 1997–1998. In Vital and health statistics. Atlanta, GA: National Center for Health Statistics, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Retrieved March 10, 2012, from http://www.cdc.gov/nchs/data/series/sr_13/sr13_149.pdf.
Department of Health and Human Services. (2012). ASPE issue brief: The cost of covering contraceptives through health insurance. Retrieved March 10, 2012, from http://aspe.hhs.gov/health/reports/2012/contraceptives/ib.shtml.
Department of Labor. (2011). Selected medical benefits: A report from the department of labor to the department of health and human services. Retrieved August 4, 2014, from http://www.bls.gov/ncs/ebs/sp/selmedbensreport.pdf.
Eng, T. R. & Butler, W. T. (1997). The hidden epidemic: Confronting sexually transmitted diseases. Editors Committee of Prevention and Control of Sexually Transmitted Diseases, Institute of Medicine. Washington, DC: National Academies Press.
Fronstin, P. (2012). Self-insured health plans: State variation and recent trends by firm size. Notes. Employee Benefit Research Institute. Retrieved September 17, 2014, from http://www.ebri.org/pdf/notespdf/EBRI_Notes_11_Nov-12.Slf-Insrd1.pdf.
Gonzalez, J. S., Hendriksen, E. S., Collins, E. M., Durán, R. E., & Safren, S. A. (2009). Latinos and HIV/AIDS: Examining factors related to disparity and identifying opportunities for psychosocial intervention research. AIDS and Behavior, 13(3), 582–602.
Gruber, J. (1994). State mandated benefits and employer-provided health insurance. Journal of Public Economics, 55(3), 433–464.
Henderson, J. T., Sawaya, G. F., Blum, M., Stratton, L., & Harper, C. C. (2010). Pelvic examinations and access to oral hormonal contraception. Obstetrics and Gynecology, 116(6), 1257–1264.
Jones, R. K. (2011). Beyond birth control: The overlooked benefits of oral contraceptive pills. New York: Guttmacher Institute.
Joyce, T. (2013a). How important was the pill to women’s economic well-being? If Roe v Wade were overturned, how might society change? Journal of Policy Analysis and Management, 32(4), 879–887.
Joyce, T. (2013b). If only policy analysis were so easy. Journal of Policy Analysis and Management, 32(4), 897–899.
Kaiser Family Foundation. (1998). Americans support requiring insurers to cover contraceptives, even if premiums rise. Retrieved November 3, 2012, from http://www.kff.org/womenshealth/1404-insurance.cfm.
Kearney, M. S., & Levine, P. B. (2009). Subsidized contraception, fertility, and sexual behavior. The Review of Economics and Statistics, 91(1), 137–151.
Kjerulff, K. H., Frick, K. D., Rhoades, J. A., & Hollenbeak, C. S. (2007). The cost of being a woman: a national study of health care utilization and expenditures for female-specific conditions. Women’s Health Issues: official publication of the Jacobs Institute of Women’s Health, 17(1), 13–21.
Laumann, E. O., & Youm, Y. (1999). Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: A network explanation. Sexually Transmitted Diseases, 26(5), 250–261.
Magnusson, B. M., Sabik, L., Chapman, D. A., Masho, S., Lafata, J. E., Bradley, C. J., & Lapane, K. L. (2012). Contraceptive insurance mandates and consistent contraceptive use among privately insured women. Medical Care, 50(7), 562–568.
Martinez, G., Chandra. A., Febo-Vazquez, I., & Mosher, W. (2013). Use of family planning and related medical services among women aged 15–44 in the United States: National survey of family growth, 2006–2010. National Health Statistics Report; no. 68. Hyattsville, MD: National Center for Health Statistics.
Solanki, G., Schauffler, H. H., & Miller, L. S. (2000). The direct and indirect effects of cost-sharing on the use of preventive services. Health Services Research, 34(6), 1331–1350.
Sonfield, A., & Gold, R. B. (2004). New study documents major strides in drive for contraceptive coverage. The Guttmacher Report on Public Policy, 7, 4–6.
Sonfield, A., Gold, R. B., Frost, J. J., & Darroch, J. E. (2004). US insurance coverage of contraceptives and the impact of contraceptive coverage mandates, 2002. Perspectives on Sexual and Reproductive Health, 36(2), 72–79.
Trivedi, A. N., Moloo, H., & Mor, V. (2010). Increased ambulatory care copayments and hospitalizations among the elderly. New England Journal of Medicine, 362(4), 320–328.
Trussell, J., Lalla, A. M., Doan, Q. V., Reyes, E., Pinto, L., & Gricar, J. (2009). Cost effectiveness of contraceptives in the United States. Contraception, 79(1), 5–14. doi:10.1016/j.contraception.2008.08.003
Wherry, L. R. (2013). Medicaid family planning expansions and related preventive care. American Journal of Public Health, 103(9), 1577–1578.
Acknowledgments
We thank Ted Joyce and participants at the 2012 APPAM Fall Conference, the Center for Policy Research Seminar Series at Syracuse University, and the Cornell Population Center/Aging Studies Institute Encore Conference for their helpful comments on earlier versions of this paper. We also thank Melissa Kearney for sharing her data on Medicaid waivers. Emily Cardon and Lincoln Groves provided excellent research assistance. A portion of this research was carried out at a U.S. Census Bureau Research Data Center facility in Ithaca, NY. We thank Warren Brown, Andrew Green, and Evan Buntrock at the NYCRDC and Nataliya Kravets at NCHS for their help with these confidential data. These results have been screened by the National Center of Health Statistics (NCHS) to avoid revealing confidential data. The results and conclusions of the paper are those of the authors and do not indicate concurrence by the Census Bureau or NCHS.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raissian, K.M., Lopoo, L.M. Mandating Prescription Contraception Coverage: Effects on Contraception Consumption and Preventive Health Services. Popul Res Policy Rev 34, 481–510 (2015). https://doi.org/10.1007/s11113-014-9353-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11113-014-9353-6