Abstract
Acromegaly is associated with an enhanced mortality, with cardiovascular and respiratory complications representing not only the most frequent comorbidities but also two of the main causes of deaths, whereas a minor role is played by metabolic complications, and particularly diabetes mellitus. The most prevalent cardiovascular complications of acromegaly include a cardiomyopathy, characterized by cardiac hypertrophy and diastolic and systolic dysfunction together with arterial hypertension, cardiac rhythm disorders and valve diseases, as well as vascular endothelial dysfunction. Biochemical control of acromegaly significantly improves cardiovascular disease, albeit completely recovering to normal mainly in young patients with short disease duration. Respiratory complications, represented mainly by sleep-breathing disorders, particularly sleep apnea, and respiratory insufficiency, frequently occur at the early stage of the disease and, although their severity decreases with disease control, this improvement does not often change the indication for a specific therapy directed to improve respiratory function. Metabolic complications, including glucose and lipid disorders, are variably reported in acromegaly. Treatments of acromegaly may influence glucose metabolism, and the presence of diabetes mellitus in acromegaly may affect the choice of treatments, so that glucose homeostasis is worth being monitored during the entire course of the disease. Early diagnosis and prompt treatment of acromegaly, aimed at obtaining a strict control of hormone excess, are the best strategy to limit the development or reverse the complications and prevent the premature mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most common complications associated with acromegaly include cardiovascular, respiratory and metabolic comorbidities that are among the main clinical conditions responsible for the increase of mortality associated with the disease [1–5].
Cardiovascular disease represents the most prevalent comorbidity, accounting for up to 80% of complications, in patients with acromegaly, and has historically reported to contribute to nearly 50% of deaths [6]. However, according to a recent 20-year follow-up study [7], causes of death in patients with acromegaly progressively shifted from 44% cardiovascular and 28% neoplastic during the first decade, to 23% cardiovascular and 35% neoplastic during the second decade. Similarly, a retrospective study [8] has demonstrated that the most common cause of mortality in acromegaly was malignancy, followed by cardiovascular diseases, with no significant impact of metabolic disorders [8]. Therefore, nowadays, cardiovascular disease represents the most frequent comorbidity and still represents one of the most important cause of death in acromegaly. Cardiovascular disease associated with acromegaly is mainly characterized by a cardiac damage, represented by a typical cardiomyopathy, which progressively develops during the disease course, with a minor impact of vascular damage, which may worsen the cardiac disease and increase the cardiovascular risk associated with the disease. Systemic arterial hypertension affects approximately one-third of patients with acromegaly [2–4]. Acromegalic cardiomyopathy is characterized by concentric biventricular hypertrophy, mainly involving the left ventricle (LV), in 80%, with consequent diastolic dysfunction in 44% of patients with acromegaly [1–5], whereas rhythm disorders [9] and valve diseases [10] affect 48% and 75% of patients, respectively, and progressive systolic dysfunction occurs after a long period, followed by cardiac failure in about 10% of patients [3]. The combination of these cardiac complications configures the peculiar acromegalic cardiomyopathy [1–5].
Respiratory disorders represent the second relevant comorbidity in patients with acromegaly, accounting for up to 80% of complications and contribute to 25% of deaths with a respiratory mortality that appears to be three-fold higher than in normal population [4, 11–13]. The respiratory disorders associated with acromegaly are a consequence of anatomical and functional changes involving the entire respiratory system; these include sleep breathing disorders, mainly sleep apnea, with a prevalence of 20–80%, and respiratory insufficiency with a prevalence of 30–80% [4]. The respiratory disorders complicate the cardiovascular disease and increase the cardiovascular risk associated with acromegaly.
Metabolic complications, mainly disorders of glucose and lipid metabolism, are frequently associated with acromegaly and represent adjunctive risk factors for the increased cardiovascular mortality [4]. However, a recent study demonstrated that such metabolic complications have a negligible impact on mortality in acromegaly [8]. The disorders of glucose metabolism include diabetes mellitus (DM), impaired glucose tolerance (IGT) and impaired fasting glucose (IFG). The prevalence of these disorders of glucose homeostasis are still unclear, widely differing among studies and ranging from 19% to 56% for DM [4], from 6% to 45% for IGT [14–19] and from 7% to 22% for IFG [14, 16, 19, 20]. DM may develop early in patients with acromegaly and more than 20% of naïve patients may have DM at diagnosis of the disease [21, 22]. The disorders of lipid metabolism mainly include decrease in HDL-cholesterol, with a prevalence ranging from 33% and 40%, and hypertriglyceridemia [14, 16, 18], with a prevalence ranging from 39% to 47%, respectively [14, 16], whereas the incidence of hypercholesterolemia is similar to general population [4].
Disease control, represented by the normalization of hormone secretion, induced by either pituitary surgery or medical therapy, improves comorbidities and restores the mortality in the majority of cases achieving hormone control.
The current review discusses current and emerging pathophysiological, clinical and prognostic aspects of the most important comorbidities, including cardiovascular, respiratory and metabolic complications occurring in patients with acromegaly.
Cardiovascular complications
Acromegaly is associated with a typical cardiomyopathy, characterized by biventricular hypertrophy, mainly involving the LV, in 80%, and consequent diastolic dysfunction, in 44% of patients with active disease [1–5]; hypertension, valvulopathies, arrhythmias, and vascular endothelial dysfunction represent additional relevant cardiovascular complications, which, together with the respiratory and metabolic complications, contribute to the development of cardiac disease and the increase in cardiovascular risk in acromegaly. The pathogenesis of acromegalic cardiomyopathy includes either a direct action of GH and IGF-I excess on the heart, or indirect mechanisms by which GH and IGF-I excess induces hypertension and disorders of glucose and lipid metabolism, resulting in cardiac glucotoxicity and lipotoxicity and cardiac remodelling and hypertrophy [23, 24]. Evidence collected in animal and human models supported the role of GH and IGF-I in determining direct changes in cardiac muscle. GH and IGF-I receptors are expressed and IGF-I is synthesized directly in cardiomyocytes [25–27]. In animal models, GH and IGF-I increase myocardial contractility and induce a hypertrophic response of the heart [28–30] and GH stimulates cardiac myocytes to re-enter the cell cycle, increasing the number of cardiac myocytes [31]. The pathogenesis of acromegalic cardiomyopathy has been proposed to develop after three steps [4]. The early phase, which is reversible, is characterized by initial cardiac hypertrophy, with increase of heart rate and systolic output, altogether configuring the hyperkinetic syndrome [4, 32]. In the middle phase of untreated or uncontrolled disease, cardiac hypertrophy becomes more evident, and signs of diastolic dysfunction with the appearance of systolic dysfunction on effort [4]. In the end-stage of untreated or uncontrolled disease, cardiac damage may include systolic dysfunction at rest and heart failure until the development of dilative cardiomyopathy, which is not reversible even with the treatment of the disease [2, 4, 23]. At diagnosis, cardiac hypertrophy is a common feature in patients with acromegaly, mainly in those with a long disease history [30, 31]. Acromegalic heart has thickened walls but rarely enlarged chambers [33, 34]. At histology, the most relevant abnormalities are interstitial fibrosis, increased extra-cellular collagen deposition, myofibrillar derangement, and areas of monocyte necrosis and lympho-mononuclear infiltration, gradually impairing the whole organ architecture [35–38]. Different echocardiographic studies have confirmed histological findings, reporting cardiac fibrosis to be common in the acromegalic heart [39, 40], however, recently cardiac fibrosis has been found to be totally absent [39] or very rare [40] in patients with active acromegaly evaluated by cardiac magnetic resonance imaging. Coexistence of cardiovascular comorbidities, including hypertension, valvulopathy, arrhythmias, together with vascular endothelial dysfunction and disorders of glucose and lipid metabolism, may worsen cardiomyopathy [41].
Hypertension is one of the most common cardiovascular comorbidities in acromegaly, with an avarage prevalence of approximately 35%, ranging from 18% to 60%, according to a meta-analysis [42]. Pathogenic mechanisms responsible for hypertension in acromegaly are yet to be fully elucidated, but the chronic exposure to GH and IGF-I excess has been suggested to act directly in the kidneys by exerting a potential antidiuretic and antinatriuretic effect [43], or indirectly by leading to the expansion of plasma volume and increasing responsiveness to angiotensin action and consequently increasing peripheral resistance [42]. Additionally, insulin resistance associated with the disease, may stimulate renal sodium reabsorption, contributing to the increase in blood pressure and the development of hypertension in acromegaly [44].
Valvulopathy is a common feature of acromegalic cardiomyopathy. Cardiac valvulopathy affects 75% of patients at the time of diagnosis [10]. This complication is a consequence of the dysregulation of extracellular matrix and the deposition of collagen and mucopolysaccharides at the level of valvular leaflets [45, 46], promoting leaflet disarray, valve ring fragility and valve regurgitation, with mitral and aortic being the most frequently affected valves [10, 47, 48]. In addition, aortic ectasia, was more frequently found in patients with acromegaly compared with controls, with aortic diameter correlating with LV mass, and patients with aortic ectasia presenting with greater cardiac hypertrophy compared with patients without aortic ectasia [49–51].
Arrhythmias frequently characterize the acromegalic cardiomyopathy. Cardiac arrhythmias affects up to nearly 90% of patients with active disease [52, 53]. This complication is consequence of the interstitial fibrosis, myofibrillar derangement and cardiac hypertrophy, contributing to induce anatomical changes in cardiomyocytes possibly leading to abnormalities in cardiac conduction [9, 52]. Recently, a 24-h Holter and cardiac magnetic resonance study, reporting arrhythmias in up to 89% of patients with acromegaly, described different types of arrhythmias: isolated and paired ventricular ectopy was found in 71% and 21%, isolated and paired supraventricular ectopy in 89% and 39%, non-sustained ventricular tachycardia in 11% and non-sustained supraventricular tachycardia in 46% of patients, respectively, without clinically relevant arrhythmias [53]. Acromegaly may also be associated with a peculiar rhythm abnormality, namely LV dyssynchronicity, defined as the loss of the simultaneous peak contraction of corresponding cardiac segments, even independently from typical predictors of cardiovascular disease, therefore suggesting a potential direct effect of hormonal excess on cardiac synchronicity [54].
The most striking functional disturbance in acromegalic cardiomyopathy is the diastolic dysfunction, manifested by inadequate ventricular filling capacity, as mainly demonstrated by the decrease of early (E) to late or atrial (A) peak velocities ratio (E/A) and the prolongation of the isovolumetric relaxation time (IVRT) [4, 23]. LV hypertrophy rarely leads to systolic dysfunction until heart failure in approximately 10% of acromegalic patients [2, 4], particularly in the end-stage of acromegalic cardiomyopathy in patients with untreated or uncontrolled disease [4]. The relative risk to develop systolic dysfunction has been demonstrated to be higher in patients with acromegaly compared with control subjects [55].
Disease duration plays a pivotal role in the determination of acromegalic cardiomyopathy, since it is correlated with the prevalence of hypertension [55], DM [4, 56] and cardiac complications, including valvulopathy [10], arrhythmias [47, 48], diastolic and systolic dysfunction [55], suggesting a potential cumulative effect of the exposure to chronic hormone excess.
Vascular disease has been described in acromegaly, although it seems to exert a relatively minor role in the determination of cardiovascular disease. The most common vascular damage described in acromegaly is the vascular endothelial dysfunction; although endothelial dysfunction, together with oxidative stress, represents the main underlying mechanism of atherosclerosis, a clear-cut vascular atherosclerosis represents a controversial finding in acromegaly. In an animal model, a vessel-specific deterioration of endothelial function, initially caused by increased oxidative stress, has been ascribed directly to hormone excess [57]. In patients with acromegaly a decrease in nitric oxide, expression of an increased level of oxidative stress, has been reported [58, 59], as well as an increase of endothelin-1, a biomarker of endothelial dysfunction [60], confirming the presence of a predisposition to atherosclerosis [60]. The presence of endothelial dysfunction in acromegaly is testified by the evidence at the brachial artery that flow-mediated dilatation is decreased in patients as compared to controls [61]. Endothelial dysfunction has been found associated with a hypertrophic remodeling of the subcutaneous blood vessels from gluteal fat biopsies of acromegalic patients [62]. Moreover, aortic stiffness has been reported significantly higher, whereas aortic strain and distensibility significantly decreased in patients with active disease as compared to controls [63]. Interestingly, the study of the peripheral microcirculation showed a significantly lower capillary number and length and a significantly higher number of tortuous loops and meandering capillaries in patients as compared to controls [64]. Beyond the evidence of the vascular endothelial dysfunction, and the vascular remodelling and dysfunction, data on vascular atherosclerosis in acromegaly are controversial. Some studies have found an increased carotid intima-media thickness (IMT) in patients as compared to controls [65–67], whereas some other studies reported a similar prevalence of increased coronary or carotid IMT and atherosclerosis between patients and controls [68–70]. Noteworthy, the risk of atherosclerosis in acromegaly has been associated with the coexistence of different classical cardiovascular risk factors, such as smoking habits, sleep apnea, insulin resistance, dyslipidemia and obesity, rather than to the direct chronic exposure to hormone excess [70]. Figure 1 shows the impact of GH and IGF-I excess on the cardiovascular system in acromegaly.
Effects of GH and IGF-I excess on the cardiovascular system. Cardiac effects of GH and IGF-I hypersecretion (left) include cardiac hypertrophy, hyperkinetic syndrome, diastolic and systolic dysfunction, arrhythmias and valvulopathy. Moreover, hormonal excess leads to vascular endothelial dysfunction and increased intima media thickness (IMT), mainly of carotid and coronary arteries, so inducing a direct vascular damage (right). Additional risk factors, including systemic arterial hypertension, insulin resistance and disorders of glucose and lipid metabolism, further contribute to cardiovascular disease in acromegalic patients (middle)
Control of acromegaly, induced by either pituitary surgery or medical therapy with conventional somatostatin receptor ligands (SRL), or the GH-receptor antagonist pegvisomant (PEG) improves cardiac structure and performance [2–4, 71], as well vascular damage [72]. Successful surgery has been shown to significantly improve hypertension, cardiac hypertrophy, diastolic or systolic dysfunction [17], and endothelial dysfunction [73]. In patients receiving SRL, LV hypertrophy rapidly reduces following hormone normalization [18, 74–77], and the improvement in diastolic and systolic dysfunction occurs in those achieving hormone excess control [78]. Persistence of uncontrolled acromegaly has been reported associated with further impairment of cardiac performance [78], and recovery from LV hypertrophy or diastolic and systolic dysfunction seemed to depend not only on the correction of hormone excess but also on patient age [17, 70], disease duration [18, 70], and the control of metabolic comorbidities [18]. In fact, the achievement of disease control induced by 12-month SRL treatment has been shown to normalize LV mass in 100% of young and in 50% of middle-aged patients [18], and ejection fraction response at peak exercise in 80% of young and in 50% of middle-aged patients [18]. Twelve months first-line treatment with SRL or surgery induced similar improvement in LV hypertrophy and diastolic function, whereas systolic function was more evidently improved in patients treated with SRL than in patients treated by surgery [17]. First-line treatment with SRL for 5 years induces a significant improvement in the prevalence of hypertension, LV hypertrophy, diastolic and systolic dysfunction, arrhythmias and lipid profile [74], and a slight decrease in the prevalence of the impairment of glucose metabolism [75]. In patients resistant or poorly responders to SRL and converted to PEG monotherapy, IGF-I normalization results in the improvement of blood pressure in hypertensive patients [79], reduction of arrhythmias [80], and amelioration of vascular endothelial dysfunction at carotid and brachial arteries [81]. Long-term PEG monotherapy has been demonstrated to improve acromegalic cardiomyopathy, by decreasing cardiac hypertrophy and enhancing diastolic and systolic function [82]. Recent evidence has also demonstrated SRL and PEG combined treatment to exert a beneficial effect on acromegalic cardiomyopathy [83]. Long-term PEG addition to SRL has been found to improve cardiac mass and diastolic function in acromegalic patients resistant to SRL [83]. However, cardiovascular complications, mainly including LV hypertrophy [17], cardiac performance at exercise [18] and vascular endothelial dysfunction [72], may persist even after the achievement of disease control, particularly in 50% of middle-age patients and long disease duration [18], therefore straightening the importance of early diagnosis and prompt treatment of hormone excess, and monitoring cardiac structure and function even in patients cured from acromegaly.
In conclusion, acromegaly is associated with a typical cardiomyopathy, mainly characterized by cardiac hypertrophy and diastolic dysfunction, and more rarely systolic dysfunction; this cardiomyopathy with the different concomitant features, including valve disease and rhythm disorders, beyond vascular damage, are strictly associated with the disease duration. Stringent control of hormone excess induced by surgery and/or medical therapy is associated with a significant improvement in cardiac structure and performance in patients with acromegaly, demonstrating the crucial role of disease remission in the reversal or prevention of the development of a serious cardiac disease, although persistence of cardiomyopathy is possible in patients after cure, especially middle-aged, or elderly, patients with a long disease history.
Respiratory complications
Acromegaly is associated with relevant complications of the respiratory system. The respiratory complications associated with acromegaly mainly include sleep breathing disorders, generally represented by the sleep apnea, and respiratory insufficiency [84–108]. Table 1 shows the pathogenesis of sleep apnea and respiratory insufficiency in acromegaly.
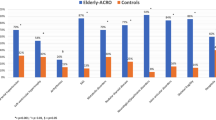
The anatomical changes affecting craniofacial bones and soft tissues, including the swelling of the tongue, the changes in the respiratory mucosa and cartilages, lung volume, and rib cage geometry, together with the alterations in muscle structure, the reduction in lung elasticity, and the increase in lung distensibility, are the main determinants of the respiratory complications associated with acromegaly. These alterations can be mostly ascribable to direct GH and IGF-I actions. Indeed, in both rodents and humans, GH and IGF-I have been shown to exert proliferative effects on lung and respiratory muscles [88–96], so promoting the increase in lung volume. Indeed, lung volume increase has been observed in up to 81% patients with acromegaly [84–86]. However, more importantly, small and upper airway narrowing was described in 35% and 26% of acromegalic patients, respectively [85–87]. This feature is the main determinant of sleep breathing disorders. Sleep apnea affects 20–80% of patients, and is a common cause of nocturnal snoring and daytime sleepiness [91, 97, 98]. Disease activity, elderly age and neck circumference have been reported to be independent predictors of sleep apnea syndrome in acromegaly [97]. In the general population, sleep apnea is known to predispose to hypertension and arrhythmias [99] suggesting that this might be also occur in patients with acromegaly. Sleep apnea is either classified as central, due to cessation of brain control of respiration, or as obstructive, due to narrowing of upper respiratory airways. Approximately one-third of patients with acromegaly develop central sleep apnea, that is associated with increased gain of the respiratory control system, in association with the obstructive sleep apnea [91]. GH and IGF-I excess have been reported as the main determinants of central sleep apnea in acromegaly [91]. However, acromegaly is predominantly associated with obstructive sleep apnea, ordinarily caused by macroglossia, pharyngeal soft tissue hypertrophy, and anatomical abnormalities of the pharynx lumen, which reduce the respiratory space. Patients may complain of apneic episodes, or hypopneic episodes [100]. Some studies have demonstrated a relationship between either the severity or the frequency of apneas and disease activity [101–103], disease duration [91], aging [91], and male gender [97]. The alteration of the structure and elasticity of the entire respiratory system lead to an impairment of pulmonary function until respiratory insufficiency. Respiratory insufficiency is less frequently investigated in acromegaly, but it seems to affect 30–80% of patients [87–89]. Most patients (70%) achieve subnormal respiratory muscle force, either during inspiratory or expiratory breathing [105]. Small and upper airway narrowing [85–87] and lung volume and capacity increase [94, 105] contribute to the pathogenesis of respiratory insufficiency. Indeed, acromegalic patients have increased amounts of lung tissue as well as nonaerated and poorly aerated areas, determining a loss of homogeneity of the respiratory system [100]. Moreover, the increased lung distensibility with normal diffusion capacity suggests that lung growth may result from an increase in alveolar size [94]. The inspiratory time is usually shorter and, consequently, the breathing frequency may increase [102]. Additional features of the acromegalic respiratory insufficiency include subclinical hypoxemia in 80% of patients [87], caused by the ventilation-perfusion ratio mismatching [87]; nocturnal hypoxemia have been also reported in 23% of patients [86]. For the aforementioned reasons, patients with acromegaly often achieve an inadequate response to ventilatory demand during exercise [4]. At anaerobic threshold and at maximal exercise, acromegalic subjects sustained a significantly decreased workload compared with control subjects [5], but this can be explained also considering a probable cardiac component. At the aerobic fitness, heart rate and perceived fatigue have been reported to be significantly higher, while maximum oxygen uptake and ventilation threshold at the maximal exercise were significantly lower than the predicted values in patients with acromegaly [108].
Control of acromegaly, induced either by pituitary surgery or medical therapy, improves sleep breathing disorders [99, 100, 109–115]. Particularly, pituitary surgery has been reported to improve sleep apnea, irrespective of disease cure [110], albeit persisting in 25% of patients achieving hormone control [115]. However, although the positive correlation between central sleep apnea and disease activity implies that hormone excess control and disease remission may lead to the disappearance of central sleep apnea, previous studies reported the persistence of sleep apnea after pituitary surgery, presumably because of the persistence of the obstructive causes [109, 110]. Medical treatment with SRL or PEG has been demonstrated to dramatically influence the remisison of sleep apnea [99, 100, 111–114], mainly by decreasing the frequency of apneic and hypopneic episodes by 50% [112], improving the central component of sleep-breathing control [91], and reducing soft tissue swelling, particularly macroglossia [114]. After 24 weeks of treatment with lanreotide Autogel (LAN) [75], despite the improvement in hormone control of acromegaly, the apnea/hypopnea index score, used to indicate the severity of sleep apnea, was found to improve in 61%, to remain unchanged in 8.7%, or even to worsen in 30.4% of patients [75]. In a cohort of 12 patients medically treated with PEG for 6 months, both tongue volume and apnea-hypopnea index significantly decreased following hormone normalization [114]. In male patients, sleep apnea can be also exacerbated by concomitant testosterone deficiency [116], and in turn sleep breathing disorders may decrease testosterone levels in experimental models [117]. Testosterone treatment transiently worsens the severity of sleep apnea [118], therefore caution is recommended for its use in patients with severe untreated sleep apnea, although it does not represent an absolute contraindication to its use [119]. However, although sleep breathing disorders severity has been shown to decrease with acromegaly control, this decrease does not change the indication for positive airway pressure (PAP) therapy, the main treatment of sleep apnea [120–122]. Sleep apnea syndrome can persist after recovery of acromegaly [123]. Considering the negative prognostic significance of this respiratory disorder, polysomnography should be included as routine procedure in the work-up of acromegalic patients, and even repeated after disease remission, being mandatory in those patients considered at high risk, mainly elderly males, overweight, and diabetic patients [123]. Appropriate intensive treatment should be implemented to minimize the clinical impact of sleep apnea syndrome in acromegaly, and PAP therapy should not be delayed in acromegalic patients with sleep-breathing disorders [120–122]. Respiratory insufficiency partly improves after disease control. Following treatment with SRL lung volumes and distensibility have been found to decrease, with stable diffusion capacity [94]. The change in lung elastic properties are reflected by a significantly improvement in the response to the physical exercise after therapy. Workload and oxygen consumption at anaerobic threshold and at maximal exercise improved significantly after 24-h continuous octreotide infusion [5], suggesting that the sustained octreotide-induced hormone reduction may cause the significant improvement in work capacity at both anaerobic threshold and during maximal exercise [5]. After a 6-month treatment with octreotide-LAR (LAR) patients achieved an increase in ventilation threshold, as well as a decrease in perceived fatigue, although the maximal oxygen uptake during progressive treadmill test did not significantly increase [108].
In consideration of the relevant prevalence of sleep apnea in acromegaly, patients with sleep apnea might constitute a target group for the earlier detection of acromegaly. A recent multicentric prospective study [124] including 755 consecutive patients referred to tertiary French centres has revealed a diagnosis of acromegaly in 0.35% of patients with a confirmed diagnosis of obstructive sleep apnea syndrome. On the other hand, every acromegalic patient should have a careful clinical, and eventually laboratory assessment, for sleep apnea at the time of diagnosis, in collaboration with a respiratory physician [125].
In conclusion, acromegaly is associated with sleep apnea and respiratory insufficiency. The anatomical changes in the respiratory system induced by hormone excess are the main determinants of respiratory complications. Control of hormone excess induced by surgery and/or medical therapy is associated with the improvement of respiratory disorders. In particular, prompt and appropriate treatment of acromegaly may favour the resolution of respiratory disorders, when the rapid hormone control permit the reversal of soft tissue hypertrophy. Conversely, persistence of the respiratory disorders after disease remission may be consequence to residual and irreversible anatomical deformations.
Metabolic complications
Acromegaly is frequently associated with deterioration of glucose and lipid metabolism. The insulin resistance represents the main pathogenetic mechanism for glucose intolerance, DM and dyslipidemia, which are common features of acromegaly and represent risk factors for the increased cardiovascular morbidity and mortality [4, 8].
Glucose metabolism
The disorders of glucose metabolism associated with acromegaly include IGT, IFG and DM; these conditions are more frequently reported in patients with acromegaly than in the general population [4, 125, 126]. The prevalence of DM in acromegaly differs greatly among studies, ranging from 16% to 56% [4, 14, 126], and this variability is explained by heterogeneity of the study populations and differences in the criteria used for the diagnosis [22, 127, 128]. Similarly, the frequency of IGT [14–19, 21] and IFG [14, 16, 19, 120] ranges from 6% to 45% and from 7% to 22%, respectively. Despite its correlation with disease duration, DM may develop early in patients with acromegaly and more than 20% of naïve patients may have DM at diagnosis [22], potentially interfering with the feasibility of diagnostic tests for acromegaly. The direct action of GH are mainly diabetogenic by increasing lipolysis and inducing insulin resistance [129, 130], whereas the indirect actions of GH, via increased IGF-I, may in turn facilitate insulin action [4]. GH exerts an overall lipolytic effect, inducing the hydrolysis of triglycerides with formation of free fatty acids (FFA) from the adipose tissue; although the exact mechanism through which GH induces lipolysis has long been debated, evidence exists that GH can influence the sensitivity and/or the responsiveness of adipose tissue to agents regulating lipolysis, such as beta-adrenergic agents [4]. The increase in FFA production is one of the main responsible factor for the development of insulin resistance. Indeed, GH-induced insulin resistance is considered to be the major mechanism accounting for the disorders of glucose metabolism in patients with acromegaly, although impairment of pancreatic beta-cell function and insulin secretion has been also clearly implicated [21, 129, 131]. Chronic GH excess leads to insulin resistance both in liver and peripheral tissue, such as skeletal muscle and adipose tissue [130]. The consequence of insulin resistance is the occurrence of hyperinsulinemia and increased glucose turnover in the basal and post-absorptive states, which characterize acromegaly; the GH-dependent increase of gluconeogenesis in the liver, with consequent increase in glucose production, importantly contributes to the impairment of glucose tolerance and development of disorders in glucose metabolism [132]. In particular, the pathogenesis of insulin resistance is multifactorial. The GH-dependent increase of FFA production induces an impairment of insulin-stimulated glucose uptake, through the suppression of glucose transporters in adipose tissue [133]. Moreover, GH excess directly blocks insulin signaling, mainly through the inhibition of insulin-receptor substrate-1 and PI-3-kinase, involved in the stimulation of glucose transport in muscle and adipose tissue and in the inhibition of liver glucose production [131]. The impairment of pancreatic beta-cell function and insulin secretion is also a necessary step towards disorders of glucose metabolism in insulin-resistant patients with acromegaly [133]. Differently from GH, under physiologic conditions, IGF-I has been shown to improve glucose homeostasis and insulin requirements, directly stimulating glucose transport into the muscle through either IGF-I or insulin/IGF-I hybrid receptors [134]. However, chronic GH excess leading to insulin resistance largely overcome the possible beneficial effects of IGF-I excess on insulin sensitivity [4]. Acromegaly has been also associated with adipose tissue dysfunction, recently expressed with a gender-specific mathematical index, the visceral adiposity index (VAI), based on anthropometric and metabolic parameters, independently correlated with cardiometabolic risk in the general population [14, 16]. The association between VAI and insulin sensitivity confirms that adipose tissue dysfunction may be an important factor in determining insulin resistance and impairment of glucose metabolism in patients with acromegaly [16]. The impairment of glucose metabolism in acromegaly is associated with obesity [19, 126], elderly [19, 128, 135, 136], and family history of diabetes [19, 126], as in the general population. However, differently from the general population, women display more severe insulin resistance compared to men with acromegaly [16]. Figure 2 shows the metabolic effects of GH excess on the target organs.
Metabolic effects of growth hormone (GH) excess on the target organs. GH plays an overall lipolytic effect leading to increased release of free fatty acids from adipose tissue and reducing the glucose uptake; impairment of pancreatic beta-cell function has been also clearly implicated. The increased gluconeogenesis in the liver importantly contributes to the impairment in glucose tolerance. Moreover, GH excess can directly decrease the activity of lipoprotein lipase increasing triglycerides levels and impact the lipoprotein metabolism, increasing plasma levels of Lp-a, Apo A-I, and Apo E
Control of acromegaly induced by surgical treatment improves both glucose tolerance and prevalence of DM [14, 17], whereas medical therapies exert different effects on glucose metabolism [135, 137–148]. Particularly, after surgery insulin secretion and sensitivity were shown both to improve [17, 149] and normalization of glucose homeostasis occurred in 23–58% of patients with preexisting DM [129]. Conversely, medical treatment of acromegaly may variably influence glucose metabolism. SRL themselves exert different hormone effects on pancreatic beta-cells, insulin secretion and glucose homeostasis [140]. Generally, SRL treatment improves insulin resistance by decreasing GH levels, and may lead to restoration of normal glucose tolerance, but hyperglycemia or even hypoglycemia have been documented [140]. In particular, discordant data are reported on the effect of SRL treatment on glucose tolerance in acromegalic patients [14, 19, 135, 138–144], taking into account that the studies performed are heterogeneous in terms of glucose parameters and duration of follow-up, and most of studies did not evaluate glucose metabolism as main clinical end-point. Nowadays, the available SRL include conventional SRL (LAR and LAN), preferentially acting via the subtype receptor SSTR2, and displaying lower affinity for SSTR5, and pasireotide (PAS), a second-generation SRL, which targets multiple receptor subtypes with a binding affinity 40-fold higher for SSTR5, and twofold lower for SSTR2 [145]. These two classes of SRL have different effects on glucose metabolism. Conventional SRL is widely demonstrated to reduce insulin resistance, but to almost similarly impair insulin and glucagon secretion by the interaction with SSTR2 [146, 147, 150, 151], also inhibiting gastrointestinal glucose absorption and hepatic glucose production. Conventional SRL were initially suspected to worsen glucose tolerance in acromegaly due to the important suppression of insulin production [152]. However, a subsequent study suggested that glucose tolerance was only modestly altered by conventional SRL therapy [153]. On the other hand, the progressive improvement of insulin resistance induced by conventional SRL may likely counterbalance its inhibitory effect on insulin secretion, mainly occurring at the beginning of treatment [74, 137, 154], so that glucose tolerance was found to improve during long-term treatment [74, 137]. A recent meta-analysis [140] evaluating the clinical impact of conventional SRL therapy on glucose metabolism demonstrated that conventional SRL significantly decrease serum insulin levels, according to the experimental evidence of the inhibition of insulin secretion [155], without a consistent change of fasting plasma glucose and serum glycated haemoglobin (HbA1c). In patients with pre-existing glucose abnormalities, conventional SRL have been found to worsen or to improve glucose profile in 25% and 29% of patients, respectively, with 46% of them maintaining the same glucose tolerance status [140]. Interestingly, high-dose LAR therapy has been demonstrated not to affect glucose metabolism in most patients, and the worsening of glucose metabolic status has been found to occur in close relation with persistently lack of disease control [144]. Differently from conventional SRL, the pathophysiological effects of PAS on glucose metabolism are yet to be completely elucidated. A recent study in healthy volunteers [156] has demonstrated that PAS suppresses predominantly insulin secretion, simultaneously with a relatively lower inhibition in glucagon secretion, and a concomitant inhibition in the secretion of incretins, such as glucagon-like peptide 1 (GLP-1), and glucose-dependent insulinotropic polypeptide (GIP), from the pancreas [156]. The peculiar binding affinity profile to SSTRs of PAS could explain the effects of PAS on insulin and glucagon secretion [156]. Indeed, PAS has the highest binding affinity for SSTR5, which is known to have a predominant role in regulating insulin secretion [157] and a lower affinity for SSTR2, which is the main mediator of glucagon secretion [157]; this may account for the more pronounced suppression of insulin and more modest suppression of glucagon induced by PAS, and may explain why the strongly reduction of insulin/glucagon ratio may induce a more important imbalance in glucose homeostasis with development of DM. The decrease in incretin levels induced by PAS through pancreatic SSTR5 receptors [158] contribute to explain the stronger suppression of insulin secretion, and the stronger impairment of glucose homeostasis associated with PAS compared with the conventional SRL. Differently from conventional SRL, the experience about the use of long-acting PAS in acromegaly is limited to recent phase 3 clinical trials [145, 159] and no data are nowadays available about the use of this compound in routine clinical practice, since this drug was only recently approved in Europe for the treatment of acromegaly patients with inadequate response to surgery and conventional SRL, and in USA for the treatment of patients with acromegaly who have had an inadequate response to surgery and/or for whom surgery is not an option [160]. Both clinical trials documented PAS to induce hyperglycemia-related adverse events more frequently than conventional SRL [145, 159]. Particularly, in patients with inadequately controlled acromegaly at the maximum dose of conventional SRL and switched to PAS [159] all grade hyperglycemia-related adverse events have been reported to occur in 67% and 61% of patients treated with PAS 40 and 60 mg, and in 30% of patients on conventional SRL, and DM in 21%, 26% and 8%, respectively. However, hyperglycemia resolved within 3 months to near-normal levels in patients who crossed over from PAS to LAR [145], suggesting that this effect was reversible. Interestingly, PAS-induced hyperglycaemia has been found to be not related to disease control but to baseline glucose tolerance status and fasting glucose levels: patients with baseline FG > 100 mg/dL experienced higher values of fasting glucose and HbA1c during PAS therapy, and 25% of patients initiated antidiabetic medication [161]. Therefore, the results of these studies suggest that an accurate metabolic assessment should be performed before starting treatment with PAS, and in patients with poorly controlled DM antidiabetic treatment should be optimized before treatment is started. In general, considering the variable effect on glucose metabolism, a monitoring of glucose profile is important during treatment of either conventional or second-generation SRL. Figure 3 shows the different effect of conventional SRL and PAS on insulin and glucagon secretion.
Different effect of conventional SRL (a) and pasireotide (b) on insulin and glucagon secretion. SSTR2 and SSTR5 have an important role in glucose regulation; in particular conventional SRL suppress the secretion of insulin and glucagon due to the interaction with SSTR2. The greater binding affinity of pasireotide for SSTR5 compared to SSTR2 could determine an altered regulation of insulin and glucagon. Indeed, pasireotide has the highest binding affinity for SSTR5, which is known to have an important role in mediating insulin secretion. By contrast, glucagon secretion is mainly mediated by SSTR2, and this may account for the more modest suppressive effect of pasireotide on glucagon secretion
In patients resistant to SRL, PEG monotherapy has been demonstrated to improve insulin sensitivity likely by blocking GH action at the receptor level and its effect on insulin resistance [148, 162–169]. It remains unclear whether the favourable outcome on glucose homeostasis during PEG is dependent on specific drug effects or may derive from improved hormone control and/or removal of inhibitory effects of SRL on insulin secretion [168, 169]. Several studies demonstrated that PEG monotherapy induced a significant decrease in fasting glucose and HbA1c levels [162–165, 168] also in patients with IGT and DM. A positive impact of PEG on peripheral insulin sensitivity has been also demonstrated [163, 166, 167]. However, it was recently reported that short-term PEG administration in healthy subjects can suppress lipolysis without significant changes in either glucose and insulin metabolism [170]. Moreover, it has been speculated that PEG treatment in acromegaly is subject to tissue-specific differences in a dose-dependent manner, and it seems possible that the peripheral suppression of GH activity is achieved prior to normalization of hepatic IGF-I production [171]. Despite disease control, disorders in glucose metabolism may persist [141]. IGT and DM have been found to persist in 10% and 20%, respectively, of patients definitively cured, and in 39% and 36%, respectively, of those achieving disease control [141].
Due to the frequent occurrence of impairment of glucose metabolism in acromegaly, patients with disorders of glucose metabolism might constitute a target group for the earlier detection of the disease. Interestingly, a recent study in 2270 patients with DM or glucose intolerance investigated the frequency of acromegaly in order to estimate its prevalence in the general population [172]. Frequency was estimated as greater as 480 cases per million adults, suggesting that the prevalence of acromegaly is still underestimated [172].
In conclusion, the impairment of glucose metabolism is frequent in patients with acromegaly. Hormone levels, increased body mass index, age and family history of DM represent the main determinants of deterioration of glucose metabolism. Surgical treatment appears to improve both glucose tolerance and DM prevalence. Conversely, medical treatment may variably influence glucose metabolism, often affecting the choice of treatment. Glucose homeostasis is worth being monitored in all patients during SRL therapy, in particular when PAS is used, regardless of the pre-existing metabolic abnormalities especially in those with uncontrolled disease.
Lipid metabolism
The disorders of lipid metabolism associated with acromegaly mainly include hypertriglyceridemia and decrease of HDL-cholesterol [4]. Indeed, whereas the prevalence of hypercholesterolemia in patients with acromegaly is similar to that in the general population [4], the prevalence of hypertriglyceridemia is three-times higher than that of the general population, and ranges from 33% and 40% of patients [14, 16, 17], being similar in both genders [16], whereas the prevalence of low HDL-cholesterol ranges from 39% to 47% [14, 16] and it is higher in postmenopausal women than in men [16]. Moreover, acromegaly is also associated with alteration of the lipoprotein metabolism, particularly with an increase of circulating levels of Lp-a, Apo A-I, and Apo E, involved in the transport of triglycerides and cholesterol, as well as small dense LDL particles, possibly as a consequence of insulin resistance [173], so contributing to the development of vascular damage [173]. Indeed, infiltration and retention of Apo B containing lipoproteins (LDL, VLDL, and Apo E remnants) in the artery wall is a critical initiating event that sparks an inflammatory response and promotes the development of atherosclerosis [174]. Arterial injury causes vascular endothelial dysfunction promoting modification of Apo B containing lipoproteins and infiltration of monocytes into the subendothelial space [174]. Altogether, these mechanisms increase the cardiovascular risk.
GH exerts direct and indirect effects, throught IGF-I, on lipid metabolism. Specifically, although GH excess induces an enhancement of lipolysis, with a consequent increase in the release of FFA from adipose tissue, which are responsible for the development of insulin resistance [4, 131, 175], GH excess may also directly decrease the activity of lipoprotein lipase (LPL), which might induce a reduction of the uptake of triglycerides in adipose tissue, increasing circulating triglycerides levels [132]. Conversely, the decrease in HDL-cholesterol seems to be related to IGF-I excess, since an independent negative relationship of IGF-I with lecithin-cholesterol acyl transferase, able to esterify free cholesterol in HDL, has been demonstrated [176]. It is noteworthy that hypertriglyceridemia in acromegalic patients seems to be not related to body weight, basal GH levels, insulin concentrations or glucose tolerance, but to the compensatory hyperinsulinemia [130]. Conversely, HDL-cholesterol levels seems to be related to IGF-I levels and gender [16, 176].
Control of acromegaly, induced by either pituitary surgery or medical therapy improves dyslipidemia [4, 177]. A significant improvement in triglycerides and HDL-cholesterol levels was reported in patients treated with both surgery or conventional SRL [14]. However, hypertriglyceridemia and low HDL levels persisted in 12.4% and 24% of patients respectively despite disease control [14]. Differently, variable results were observed on lipid metabolism after PEG treatment. Some studies have reported an increase in total and LDL-cholesterol with unchanged triglyceride and a significant decline in Lp-a levels [178, 179], whereas other studies [180–182] reported no change in lipid fractions during PEG treatment. However, the mechanism whereby PEG can act on lipid profile is still unknown [178–182].
In conclusion, acromegaly is associated with disorders of lipid metabolism, mainly including hypertriglyceridemia and decrease in HDL-cholesterol. Hormone control induced by surgery and/or SRL is associated with a significant improvement in lipid metabolism, demonstrating the crucial role of disease remission in the reversal of dyslipidemia in acromegaly. However, further studies are still required to establish the impact and mechanisms of PEG on lipid metabolism.
General conclusions
Acromegaly is associated with an increased mortality compared to the general population, with cardiovascular and respiratory diseases representing two of the most important cause of death, whereas metabolic complications play a minor role in determining mortality. Early diagnosis and prompt treatment are the best way to limit morbidity and mortality in acromegaly. Appropriate and effective treatment of acromegaly should be started early to obtain a strict hormone control since beneficial effects on comorbidities and mortality can be seen in patients achieving disease control. In particular, stringent control of hormone excess is associated with the significant improvement in cardiac hypertrophy, as well as diastolic and systolic function, demonstrating that biochemical control leads to an overall improvement in cardiac structure and performance in patients with acromegaly. However, cardiovascular disease can persist after disease control, mainly in elderly patients with long disease duration. Moreover, hormone control of acromegaly, albeit decreasing the severity of respiratory disorders, does not recover sleep apnea in the totality of patients, and sleep apnea can persist after complete recovery of acromegaly, mainly in elderly male patients with long disease duration, requiring specific therapy despite hormone normalization. The effects of disease control on metabolic complications are variable. Surgery improves both glucose tolerance, DM and dyslipidemia. Medical therapy improves lipid metabolism and may variably impact glucose metabolism and DM prevalence, also influencing the choice of treatments. Therefore, an adequate monitoring of glucose homeostasis is recommended in all patients during SRL therapy, particularly in those receiving PAS. In general, despite complete hormone normalization, disease control cannot recover systemic complications in the totality of acromegalic patients. Close dialogue among endocrinologists and specialists involved in the management of acromegalic patients is of extreme importance for the optimal care of these patients.
References
Melmed S, Colao A, Barkan A, Molitch M, Grossman AB, Kleimberg D, Clemmons D, Chanson P, Laws E, Schlechte J, Vance ML, Ho K, Giustina A (2009) Guidelines for acromegaly management: an update. J Clin Endocrinol Metab 94:1509–1517
Clayton RN (2003) Cardiovascular function in acromegaly. Endocr Rev 24:272–274
Melmed S (2006) Medical progress: acromegaly. New Engl J Med 355:2558–2573
Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis and management. Endocr Rev 25:102–152
Giustina A, Boni E, Romanelli G, Grassi V, Giustina G (1995) Cardiopulmonary performance during exercise in acromegaly, and the effects of acute suppression of growth hormone hypersecretion with octreotide. Am J Cardiol 75:1042–1047
Holdaway IM, Rajasoorya RC, Gamble GD (2004) Factors influencing mortality in acromegaly. J Clin Endocrinol Metab 89(2):667–674
Ritvonen E, Löyttyniemi E, Jaatinen P, Ebeling T, Moilanen L, Nuutila P, Kauppinen-Mäkelin R, Schalin-Jäntti C (2015) Mortality in acromegaly: a 20-year follow-up study. Endocr Relat Cancer 23(6):469–480
Mercado M, Gonzalez B, Vargas G, Ramirez C, de los Monteros AL, Sosa E, Jervis P, Roldan P, Mendoza V, López-Félix B, Guinto G (2014) Successful mortality reduction and control of comorbidities in patients with acromegaly followed at a highly specialized multidisciplinary clinic. J Clin Endocrinol Metab 99(12):4438–4446
Kahaly G, Olshausen KV, Mohr-Kahaly S, Erbel R, Boor S, Beyer J, Meyer J (1992) Arrhythmia profile in acromegaly. Eur Heart J 13(1):51–56
Colao A, Spinelli L, Marzullo P, Pivonello R, Petretta M, Di Somma C, Vitale G, Bonaduce D, Lombardi, G (2003) High prevalence of cardiac valve disease in acromegaly: an observational, analytical, case-control study. J Clin Endocrinol Metab 88(7):3196–3201
Alexander L, Appleton D, Hall R, Ross WM, Wilkinson R (1980) Epidemiology of acromegaly in the Newcastle region. Clin Endocrinol 12:71–79
Nabarro JDN (1987) Acromegaly. Clin Endocrinol 26:481–512
Bengtsson BA, Eden S, Ernest I, Oden A, Sjögren B (1988) Epidemiology and long-term survival in acromegaly: a study of 166 cases diagnosed between 1955 and 1984. Acta Med Scand 223:327–335
Giordano C, Ciresi A, Amato MC et al (2012) Clinical and metabolic effects of first-line treatment with somatostatin analogues or surgery in acromegaly: a retrospective and comparative study. Pituitary 15(4):539–551
Kreze A, Kreze-Spirova E, Mikulecky M (2001) Risk factors for glucose intolerance in active acromegaly. Braz J Med Biol Res 34:1429–1433
Ciresi A, Amato MC, Pivonello R et al (2013) The metabolic profile in active acromegaly is gender-specific. J Clin Endocrinol Metab 98(1):E51–E59
Colao A, Pivonello R, Galderisi M, Cappabianca P, Auriemma RS, Galdiero M, Cavallo LM, Esposito F, Lombardi G (2008) Impact of treating acromegaly first with surgery or somatostatin analogs on cardiomyopathy. J Clin Endocrinol Metab 93(7):2639–2646
Colao A, Marzullo P, Cuocolo A, Spinelli L, Pivonello R, Bonaduce D, Salvatore M, Lombardi G (2003) Reversal of acromegalic cardiomyopathy in young but not in middle-aged patients after 12 months of treatment with the depot long-acting somatostatin analogue octreotide. Clin Endocrinol 58:169–176
Espinosa-de-los-Monteros AL, González B, Vargas G et al (2011) Clinical and biochemical characteristics of acromegalic patients with different abnormalities in glucose metabolism. Pituitary 14:231–235
Portocarrero-Ortiz LA, Vergara-Lopez A, Vidrio-Velazquez M et al (2016) The Mexican Acromegaly Registry: clinical and biochemical characteristics at diagnosis and therapeutic outcomes. J Clin Endocrinol Metab 101(11):3997–4004
Kasayama S, Otsuki M, Takagi M et al (2000) Impaired beta-cell function in the presence of reduced insulin sensitivity determines glucose tolerance status in acromegalic patients. Clin Endocrinol 52:549–555
Fieffe S, Morange I, Petrossians P et al (2011) Diabetes in acromegaly, prevalence, risk factors, and evolution: data from the French Acromegaly Registry. Eur J Endocrinol 164(6):877–884
Colao A, Marzullo P, Di Somma C, Lombardi, G (2001) Growth hormone and the heart. Clin Endocrinol 54:137–154
Isgaard J, Tivesten A, Friberg P, Bengtsson BA (1999) The role of the GH/IGF-I axis for the cardiac function and structure. Horm Metab Res 31:50–54
Isgaard J, Nilsson A, Vickman K, Isaksson, OGP (1989) Growth hormone regulates the level of insulin-like growth factor-ImRNAin rats skeletal muscle. J Endocrinol 120:107–112
Delafontaine P (1995) Insulin-like growth factor I and its binding proteins in the cardiovascular system. Cardiovasc Res 30:825–834
Han VK, D’Ercole AJ, Lund PK (1987) Cellular localization of somatomedin (insulin-like growth factor) messenger RNA in the human fetus. Science 236:193–197
Cittadini A, Stromer H, Katz SE, Clark R, Moses AC, Morgan JP, Douglas PS (1996) Differential cardiac effects of growth hormone and insulin-like growth factor-I in the rat. A combined in vivo and in vitro evaluation. Circulation 93:800–809
Lu C, Schwartzbauer G, Sperling MA, Devaskar SU, Thamotharan S, Robbins PD, McTiernan CF, Liu JL, Jiang J, Frank SJ, Menon RK (2001) Demonstration of direct effects of growth hormone on neonatal cardiomyocytes. J Biol Chem 276:22892–22900
Vetter U, Kupferschmid C, Lang D, Pents S (1988) Insulin-like growth factors and insulin increase the contractility of neonatal rat cardiocytes in vitro. Basic Res Cardiol 83:647–654
Brüel A, Christoffersen TE, Nyengaard JR (2007) Growth hormone increases the proliferation of existing cardiac myocytes and the total number of cardiac myocytes in the rat heart. Cardiovasc Res 76(3):400–408
Thuesen L, Christensen SE, Weeke J, Orskov H, Henningsen P (1988) A hyperkinetic heart in uncomplicated active acromegaly. Explanation of hypertension in acromegalic patients? Acta Med Scand 223:337–343
Vitale G, Pivonello R, Galderisi M, D’Errico A, Spinelli L, Lupoli G, Lombardi G, Colao A (2001) Cardiovascular complications in acromegaly: methods of assessment. Pituitary 4(4):251–257
Lombardi G, Colao A, Marzullo P, Ferone D, Longobardi S, Esposito V, Merola B (1997) Is growth hormone bad for your heart? Cardiovascular impact of GH deficiency and of acromegaly. J Endocrinol 155:S33
Courville C, Mason VR (1938) The heart in acromegaly. Arch Int Med 61:704
Hejtmancik MR, Bradfield JY, Herrmann GR (1951) Acromegaly and the heart: a clinical and pathologic study. Ann Intern Med 34:1445
Lie JT, Grossman SJ (1980) Pathology of the heart in acromegaly: anatomic findings in 27 autopsied patients. Am Heart J 100:41
Hayward RP, Emanuel RW, Nabarro, J.D.N. (1987) Acromegalic heart disease: influence of treatment of the acromegaly on the heart. Q J Med 62:41
Bogazzi F, Lombardi M, Strata E, Aquaro G, Di Bello V, Cosci C, Sardella C, Talini E, Martino E (2008) High prevalence of cardiac hypertophy without detectable signs of fibrosis in patients with untreated active acromegaly: an in vivo study using magnetic resonance imaging. Clin Endocrinol 68(3):361–368
dos Santos Silva CM, Gottlieb I, Volschan I, Kasuki L, Warszawski L, Balarini Lima GA, Xavier SS, Pedrosa RC, Neto LV, Gadelha MR (2015) Low frequency of cardiomyopathy using cardiac magnetic resonance imaging in an acromegaly contemporary cohort. J Clin Endocrinol Metab 100(12):4447–4455
Colao A, Baldelli R, Marzullo P, Ferretti E, Ferone D, Gargiulo P, Petretta M, Tamburrano G, Lombardi G, Liuzzi A (2000) Systemic hypertension and impaired glucose tolerance are independently correlated to the severity of the acromegalic cardiomyopathy. J Clin Endocrinol Metab 85:193–199
Bondanelli M, Ambrosio MR, degli Uberti EC (2001) Pathogenesis and prevalence of hypertension in acromegaly. Pituitary 4(4):239–249
Feld S, Hirschgerg R (1996) Growth Hormone, the insulin-like growth factor system, and the kidney. J Clin Endocrinol Metab 5:423–480
Hansen TK, Møller J, Thomsen K, Frandsen E, Dall R, Jørgensen JO, Christiansen JS (2001) Effects of growth hormone on renal tubular handling of sodium in healthy humans. Am J Physiol Endocrinol Metab 281(6):E1326–E1332
Rabkin E, Aikawa M, Stone JR, Fukumoto Y, Libby P, Schoen FJ (2001) Activated myofibroblasts express catabolic enzymes and mediate matrix re- modeling in myxomatous heart valves. Circulation 104:2525–2253
Feelders RA, Savelkoul HF, de Herder WW, Hooijkaas H, Lamberts SW (2002) The cytokine network in acromegaly before and after pituitary surgery: growth hormone excess is associated with a reversible shift to the T-helper 1 cytokine response. Program of the 84th Annual Meeting of The Endocrine Society, San Francisco, CA, p 76 (Abstract OR8-5)
Pereira AM, van Thiel SW, Lindner JR, Roelfsema F, van der Wall EE, Morreau H, Smit JW, Romijn JA, Bax JJ (2004) Increased prevalence of regurgitant valvular heart disease in acromegaly. J Clin Endocrinol Metab 89:71–75
van der Klaauw AA, Bax JJ, Roelfsema F, Bleeker GB, Holman ER, Corssmit EP, van der Wall EE, Smit JW, Romijn JA, Pereira AM (2006) Uncontrolled acromegaly is associated with progressive mitral valvular regurgitation. Growth Horm IGF Res 16:101–107
Colao A, Grasso LF (2011) Aortic root ectasia in patients with acromegaly: an emerging complication. Clin Endocrinol 75(4):420–421
Casini AF, Neto LV, Fontes R, França RF, Xavier SS, Gadelha MR (2011) Aortic root ectasia in patients with acromegaly: experience at a single center. Clin Endocrinol 75:495–500
van der Klaauw AA, Bax JJ, Smit JW, Holman ER, Delgado V, Bleeker GB, Biermasz NR, Roelfsema, .F, Romijn JA, Pereira AM (2008) Increased aortic root diameters in patients with acromegaly. Eur J Endocrinol 159:97–103
Vitale G, Pivonello R, Lombardi G, Colao A (2004) Cardiac abnormalities in acromegaly. Pathophysiology and implications for management. Treat Endocrinol 3(5):309–318
Warszawski L, Kasuki L, Sá R, Dos Santos Silva CM, Volschan I, Gottlieb I, Pedrosa RC, Gadelha MR (2016) Low frequency of cardiac arrhythmias and lack of structural heart disease in medically-naïve acromegaly patients: a prospective study at baseline and after 1 year of somatostatin analogs treatment. Pituitary 19(6):582–589
Kırış A, Erem C, Turan OE, Civan N, Kırış G, Nuhoğlu I, Ilter A, Ersöz HO, Kutlu M (2013) Left ventricular synchronicity is impaired in patients with active acromegaly. Endocr 44:200–206
Colao A, Pivonello R, Grasso LF, Auriemma RS, Galdiero M, Savastano S, Lombardi G (2011) Determinants of cardiac disease in newly diagnosed patients with acromegaly: results of a 10 year survey study. Eur J Endocrinol 165(5):713–721
Jayasena C, Comninos A, Clarke H, Donaldson M, Meeran K, Dhillo W (2011) The effects of long term GH and IGF-I exposure on the development of cardiovascular, cerebrovascular and metabolic co-morbidities in treated patients with acromegaly. Clin Endocrinol 75:220–225
Andersson IJ, Johansson ME, Wickman A, Bohlooly-Y M, Klintland N, Caidahl K, Gustafsson M, Borén J, Gan LM, Bergström G (2006) Endothelial dysfunction in growth hormone transgenic mice. Clin Sci 110(2):217–225
Anagnostis P, Efstathiadou ZA, Gougoura S, Polyzos SA, Karathanasi E, Dritsa P, Kita M, Koukoulis GN (2013) Oxidative stress and reduced antioxidative status, along with endothelial dysfunction in acromegaly. Horm Metab Res 45(4):314–318
Ronconi V, Giacchetti G, Mariniello B, Camilletti A, Mantero F, Boscaro M, Vignini A, Mazzanti L (2005) Reduced nitric oxide levels in acromegaly: cardiovascular implications. Blood Press 14(4):227–232
Kirilov G, Zacharieva S, Alexandrov AS, Lozanov V, Mitev V (2009) Increased plasma endothelin level as an endothelial marker of cardiovascular risk in patients with active acromegaly: a comparison with plasma homocysteine. Methods Find Exp Clin Pharmacol 31(7):457–461
Baykan M, Erem C, Gedikli O, Hacihasanoglu A, Erdogan T, Kocak M, Kaplan S, Korkmaz L, Celik S (2009) Impairment in flow-mediated vasodilatation of the brachial artery in acromegaly. Med Princ Pract 18(3):228–232
Paisley AN, Izzard AS, Gemmell I, Cruickshank K, Trainer PJ, Heagerty AM (2009) Small vessel remodeling and impaired endothelial-dependent dilatation in subcutaneous resistance arteries from patients with acromegaly. J Clin Endocrinol Metab 94(4):1111–1117
Topaloglu O, Sayki Arslan M, Turak O, Ginis Z, Sahin M, Cebeci M, Ucan B, Cakir E, Karbek B, Ozbek M, Cakal E, Delibasi T (2014) Three noninvasive methods in the evaluation of subclinical cardiovascular disease in patients with acromegaly: epicardial fat thickness, aortic stiffness and serum cell adhesion molecules. Clin Endocrinol 80(5): 726–734
Schiavon F, Maffei P, Martini C, De Carlo E, Fais C, Todesco S, Sicolo N (1999) Morphologic study of microcirculation in acromegaly by capillaroscopy. J Clin Endocrinol Metab 84:3151–3155
Brevetti G, Marzullo P, Silvestro A, Pivonello R, Oliva G, di Somma C, Lombardi G, Colao A (2002) Early vascular alterations in acromegaly. J Clin Endocrinol Metab 87:3174–3179
Colao A, Spiezia S, Cerbone G, Pivonello R, Marzullo P, Ferone D, Di Somma C, Assanti AP, Lombardi G (2001) Increased arterial intima-media thickness by B-M mode echodoppler ultrasonography in acromegaly. Clin Endocrinol 54:515–524
Kartal I, Oflaz H, Pamukçu B, Meriç M, Aral F, Ozbey N, Alagöl F (2010) Investigation of early atherosclerotic changes in acromegalic patients. Int J Clin Pract 64:39–44
Paisley AN, Banerjee M, Rezai M, Schofield RE, Balakrishnannair S, Herbert A, Lawrance JA, Trainer PJ, Cruickshank JK (2011) Changes in arterial stiffness but not carotid intimal thickness in acromegaly. J Clin Endocrinol Metab 96:1486–1492
Bogazzi F, Battolla L, Spinelli C, Rossi G, Gavioli S, Di Bello V, Cosci C, Sardella C, Volterrani D, Talini E, Pepe P, Falaschi F, Mariani G, Martino, E (2007) Risk factors for development of coronary heart disease in patients with acromegaly: a five-year prospective study. J Clin Endocrinol Metab 92:4271–4277
Akutsu H, Kreutzer J, Wasmeier G, Ropers D, Rost C, Möhlig M, Wallaschofski H, Buchfelder M, Schöfl C (2010) Acromegaly per se does not increase the risk for coronary artery disease. Eur J Endocrinol 162:879–886
Colao A, Cuocolo A, Marzullo P, Nicolai E, Ferone D, Della Morte AM, Pivonello R, Salvatore M, Lombardi G (2001) Is the acromegalic cardiomyopathy reversible? Effect of 5-year normalization of growth hormone and insulin-like growth factor levels on cardiac performance. J Clin Endocrinol Metab 86:1551–1557
Akgul E, Tokgozoglu SL, Erbas T, Kabakci G, Aytemir K, Haznedaroglu I, Oto A, Kes SS (2010) Evaluation of the impact of treatment on endothelial function and cardiac performance in acromegaly. Echocardiography 27(8):990–996
Sakai H, Tsuchiya K, Nakayama C, Iwashima F, Izumiyama H, Doi M, Yoshimoto T, Tsujino M, Yamada S, Hirata Y (2008) Improvement of endothelial dysfunction in acromegaly after transsphenoidal surgery. Endocr J 55(5):853–859
Colao A, Auriemma RS, Galdiero M, Lombardi G, Pivonello R (2009) Effects of initial therapy for five years with somatostatin analogs for acromegaly on growth hormone and insulin-like growth factor-I levels, tumor shrinkage, and cardiovascular disease: a prospective study. J Clin Endocrinol Metab 94(10):3746–3756
Annamalai AK, Webb A, Kandasamy N, Elkhawad M, Moir S, Khan F, Maki-Petaja K, Gayton EL, Strey CH, O’Toole S, Ariyaratnam S, Halsall DJ, Chaudhry AN, Berman L, Scoffings DJ, Antoun NM, Dutka DP, Wilkinson IB, Shneerson JM, Pickard JD, Simpson HL, Gurnell M (2013) A comprehensive study of clinical, biochemical, radiological, vascular, cardiac, and sleep parameters in an unselected cohort of patients with acromegaly undergoing presurgical somatostatin receptor ligand therapy. J Clin Endocrinol Metab 98(3):1040–1050
Colao A, Marzullo P, Ferone D, Spinelli L, Cuocolo A, Bonaduce D, Salvatore M, Boerlin V, Lancranjan I, Lombardi G (2000) Cardiovascular effects of depot long-acting somatostatin analog Sandostatin LAR in acromegaly. J Clin Endocrinol Metab 86:3132–3140
Giustina A, Casanueva FF, Cavagnini F, Chanson P, Clemmons D, Frohman LA, Gaillard R, Ho K, Jaquet P, Kleinberg DL, Lamberts SW, Lombardi G, Sheppard M, Strasburger CJ, Vance ML, Wass JA, Melmed S; The Pituitary Society and the European Neuroendocrine Association (2003) Diagnosis and treatment of acromegaly complications. J Endocrinol Invest 26:1242–1247
Colao A, Cuocolo A, Marzullo P, Nicolai E, Ferone D, Florimonte L, Salvatore M, Lombardi G (1999) Effects of one-year treatment with octreotide on cardiac performance in patients with acromegaly. J Clin Endocrinol Metab 84:17–23
Colao A, Pivonello R, Auriemma RS, De Martino MC, Bidlingmaier M, Briganti F, Tortora F, Burman P, Kourides IA, Strasburger CJ, Lombardi G (2006) Efficacy of 12-month treatment with the GH receptor antagonist pegvisomant in patients with acromegaly resistant to long-term, high-dose somatostatin analog treatment: effect on IGF-I levels, tumor mass, hypertension and glucose tolerance. Eur J Endocrinol 154(3):467–477
Auriemma RS, Pivonello R, De Martino MC, Cudemo G, Grasso LF, Galdiero M, Perone Y, Colao, A (2012) Treatment with GH receptor antagonist in acromegaly: effect on cardiac arrhythmias. Eur J Endocrinol 168(1):15–22
De Martino MC, Auriemma RS, Brevetti G, Vitale G, Schiano V, Galdiero M, Grasso L, Lombardi G, Colao A, Pivonello R (2010) The treatment with growth hormone receptor antagonist in acromegaly: effect on vascular structure and function in patients resistant to somatostatin analogues. J Endocrinol Invest 33(9):663–670
Pivonello R, Galderisi M, Auriemma RS, De Martino MC, Galdiero M, Ciccarelli A, D’Errico A, Kourides I, Burman P, Lombardi G, Colao, A (2007) Treatment with growth hormone receptor antagonist in acromegaly: effect on cardiac structure and performance. J Clin Encocrinol Metab 92(2):476–482
Auriemma RS, Grasso LF, Galdiero M, Galderisi M, Pivonello C, Simeoli C, De Martino MC, Ferrigno R, Negri M, de Angelis C, Pivonello R, Colao A (2016) Effects of long-term combined treatment with somatostatin analogues and pegvisomant on cardiac structure and performance in acromegaly. Endocrine (Epub ahead of print)
Harrison BD, Millhouse KA, Harrington M, Nabarro JD (1978) Lung function in acromegaly. Q J Med 47:517–532
Evans CC, Hipkin LJ, Murray GM (1977) Pulmonary function in acromegaly. Thorax 22:322–327
Trotman-Dickenson B, Weetman AP, Hughes JM (1991) Upper airflow obstruction and pulmonary function in acromegaly: relationship to disease activity. Q J Med 79:527–538
Luboshitzky R, Barzilai D (1980) Hypoxemia and pulmonary function in acromegaly. Am Rev Respir Dis 121:471–475
Lobie PE, Garcia-Aragon J, Wang BS, Baumback WR, Waters MJ (1992) Cellular localization of the growth hormone binding protein in the rat. Endocrinology 130:3057–3065
Zogopoulos G, Figueiredo R, Jenab A, Ali Z, Lefebvre Y, Goodyer CG (1996) Expression of exon 3-retaining and -deleted human growth hormone receptor messenger ribonucleic acid isoforms during development. J Clin Endocrinol Metab 81:775–782
Hill DJ, Riley SC, Bassett NS, Waters MJ (1992) Localization of the growth hormone receptor, identified by immunocytochemistry, in second trimester human fetal tissues and in placenta throughout gestation. J Clin Endocrinol Metab 75:646–650
Grunstein RR, Ho KY, Sullivan CE (1991) Sleep apnea in acromegaly. Ann Intern Med 115:527–532
Rom WN, Basset P, Fells GA, Nukiwa T, Trapnell BC, Crystal RG (1988) Alveolar macrophages release an insulin-like growth factor I-type molecule. J Clin Invest 82:1685–1693
Camilo GB, Carvalho AR, Machado DC, Mogami R, Kasuki L, Gadelha MR, Melo PL, Lopes AJ (2015) Correlations between forced oscillation technique parameters and pulmonary densitovolumetry values in patients with acromegaly. Braz J Med Biol Res 48(10):877–885
Garcia-Rio F, Pino JM, Diez JJ, Ruiz A, Villasante C, Villamor J (2001) Reduction of lung distensibility in acromegaly after suppression of growth hormone hypersecretion. Am J Respir Crit Care Med 164:852–857
Noveral JP, Bhala A, Hintz RL, Grunstein MM, Cohen P (1994) Insulin-like growth factor axis in airway smooth muscle cells. Am J Physiol 267:L761–L765
Rich CB, Ewton DZ, Martin BM, Florini JR, Bashir M, Rosenbloom J, Foster JA (1992) IGF-I regulation of elastogenesis: comparison of aortic and lung cells. Am J Physiol 263:L276–L282
Weiss V, Sonka K, Pretl M, Dostalova S, Klozar J, Rambousek P, Marek J, Haas T (2000) Prevalence of the sleep apnea syndrome in acromegaly population. J Endocrinol Invest 23:515–519
Dostalova S, Sonka K, Smahel Z, Weiss V, Marek J, Horinek D (2001) Craniofacial abnormalities and their relevance for sleep apnea syndrome aetiopathogenesis in acromegaly. Eur J Endocrinol 144:491–497
Ip, MSM, Tan KCB, Peh WCG, Lam KSL (2001) Effect of Sandostatin LAR on sleep apnoea in acromegaly: correlation with computerized tomographic cephalometry and hormonal activity. Clin Endocrinol 55:477–483
Chemla D, Attal P, Maione L, Veyer AS, Mroue G, Baud D, Salenave S, Kamenicky P, Bobin S, Chanson P (2014) Impact of successful treatment of acromegaly on overnight heart rate variability and sleep apnea. J Clin Endocrinol Metab 99(8):2925–2931
Isono S, Saeki N, Tanaka A, Nishino T (1999) Collapsibility of passive pharynx in patients with acromegaly. Am J Respir Crit Care Med 160:64–68
Morewood DJ, Belchetz PE, Evans CC, Whitehouse GH (1986) The extrathoracic airway in acromegaly. Clin Radiol 37:243–246
Perks WH, Horrocks PM, Cooper RA, Bradbury S, Allen A, Baldock N, Prowse K, van’t Hoff W (1980) Sleep apnoea in acromegaly. Br Med J 280:894–897
Hart TB, Radow SK, Blackard WG, Tucker HS, Cooper KR (1985) Sleep apnea in active acromegaly. Arch Intern Med 145:865–866
Iandelli I, Gorini M, Duranti R, Bassi F, Misuri G, Pacini F, Rosi E, Scano G (1997) Respiratory muscle function and control of breathing in patients with acromegaly. Eur Respir J 10:977–982
Colao A, Spinelli L, Cuocolo A, Spiezia S, Bonaduce D, Salvatore M, Lombardi G (2002) Cardiovascular consequences of early-onset growth hormone excess. J Clin Endocrinol Metab 87:3097–3104
Colao A, Cuocolo A, Marzullo P, Nicolai E, Ferone D, Della Morte AM, Petretta M, Salvatore M, Lombardi G (1999) Impact of patient’s age and disease duration on cardiac performance in acromegaly: A radionuclide angiography study. J Clin Endocrinol Metab 84:1518–1523
Thomas SG, Woodhouse LJ, Pagura SM, Ezzat S (2002) Ventilation threshold as a measure of impaired physical performance in adults with growth hormone excess. Clin Endocrinol 56:351–358
Pekkarinen T, Partinen M, Pelkonen R, Ivanainen M (1987) Sleep apnoea and daytime sleepiness in acromegaly: relationship to endocrinological factors. Clin Endocrinol 27:649–654
Pelttari L, Polo O, Rauhala E, Vuoriluoto J, Aitasalo K, Hyyppa MT, Kronholm E, Irjala K, Viikari J (1995) Nocturnal breathing abnormalities in acromegaly after adenomectomy. Clin Endocrinol 43:175–182
Rosenow F, Reuter S, Deuss U, Szelies B, Hilgers RD, Winkelmann W, Heiss WD (1996) Sleep apnoea in treated acromegaly: relative frequency and predisposing factors. Clin Endocrinol 45:563–569
Chanson P, Timsit J, Benoit O, Augendre B, Moulonguet M, Guillausseau PG, Warnet A, Lubetzki J (1986) Rapid improvement of sleep apnoea of acromegaly after short term treatment with somatostatin analogue SMS 201–995. Lancet 1:1270–1271
Grunstein RR, Ho KK, Sullivan CE (1994) Effect of octreotide, a somatostatin analog, on sleep apnea in patients with acromegaly. Ann Intern Med 121(7):478–483
Berg C, Wessendorf TE, Mortsch F, Forsting M, Teschler H, Weischer T, Mann K, Saller B, Herrmann BL (2009) Influence of disease control with pegvisomant on sleep apnoea and tongue volume in patients with active acromegaly. Eur J Endocrinol 161(6):829–835
Sze L, Schmid C, Bloch KE, Bernays R, Brändle M (2007) Effect of transsphenoidal surgery on sleep apnoea in acromegaly. Eur J Endocrinol 156(3):321–329
Barrett-Connor E, Dam TT, Stone K, Harrison SL, Redline S, Orwoll E, Osteoporotic Fractures in Men Study Group (2008) The association of testosterone levels with overall sleep quality, sleep architecture, and sleep-disordered breathing. J Clin Endocrinol Metab 93(7):2602–2609
Oh MM, Kim JW, Jin MH, Kim JJ, Moon du G (2012) Influence of paradoxical sleep deprivation and sleep recovery on testosterone level in rats of different ages. Asian J Androl 14:330–334
Killick R, Wang D, Hoyos CM et al (2013) The effects of testosterone on ventilatory responses in men with obstructive sleep apnoea: a randomised, placebo-controlled trial. J Sleep Res 22:331–336
Wittert G (2014) The relationship between sleep disorders and testosterone. Curr Opin Endocrinol Diabetes Obes 21(3):239–243
Akkoyunlu ME, Ilhan MM, Bayram M, Taşan E, Yakar F, Ozçelik HK, Karakose F, Kart L (2013) Does hormonal control obviate positive airway pressure therapy in acromegaly with sleep-disordered breathing? Respir Med 107(11):1803–1809
De Menis E, Giustina A, Colao A, Degli Uberti E, Ghigo E, Minuto F, Bogazzi F, Drigo R, Cattaneo A, Aimaretti G, COM.E.T.A. Italian Study Group (2011) Assessment of the awareness and management of sleep apnea syndrome in acromegaly. The COM.E.TA (Comorbidities Evaluation and Treatment in Acromegaly) Italian Study Group. J Endocrinol Invest 34(1):60–64
Attal P, Chanson P (2010) Endocrine aspects of obstructive sleep apnea. J Clin Endocrinol Metab 95(2):483–495
Davi’ MV, Dalle Carbonare L, Giustina A, Ferrari M, Frigo A, Lo Cascio V, Francia, G (2008) Sleep apnoea syndrome is highly prevalent in acromegaly and only partially reversible after biochemical control of the disease. Eur J Endocrinol 159(5):533–540
Galerneau LM, Pépin JL, Borel AL, Chabre O, Sapene M, Stach B, Girey-Rannaud J, Arnol N, Tamisier R, Caron P, Scientific council and investigators of the French national sleep apnoea registry (OSFP) (2016) Acromegaly in sleep apnoea patients: a large observational study of 755 patients. Eur Respir J 48(5):1489–1492
Melmed S, Casanueva FF, Klibanski A, Bronstein MD, Chanson P, Lamberts SW, Strasburger CJ, Wass JA, Giustina A (2013) A consensus on the diagnosis and treatment of acromegaly complications. Pituitary 16(3):294–302
Alexopoulou O, Bex M, Kamenicky P et al (2014) Prevalence and risk factors of impaired glucose tolerance and diabetes mellitus at diagnosis of acromegaly: a study in 148 patients. Pituitary 17(1):81–89
Reid TJ, Post KD, Bruce JN et al (2010) Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clin Endocrinol 72(2):203–208
Arosio M, Reimondo G, Malchiodi E et al (2012) Predictors of morbidity and mortality in acromegaly: an Italian survey. Eur J Endocrinol 167(2):189–198
Clemmons DR (2002) Roles of insulin-like growth factor-I and growth hormone in mediating insulin resistance in acromegaly. Pituitary 5(3):181–183
Møller N, Jørgensen JO (2009) Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr Rev 30(2):152–177
Frara S, Maffezzoni F, Mazziotti G, Giustina A (2016) Current and emerging aspects of diabetes mellitus in acromegaly. Trends Endocrinol Metab 27(7):470–483
Dal J, List EO, Jørgensen JO, Berryman DE (2016) Glucose and fat metabolism in acromegaly: from mice models to patient care. Neuroendocrinology 103(1):96–105
Kasayama S, Otsuki M, Takagi M et al (2000) Impaired-cell function in the presence of reduced insulin sensitivity determines glucose tolerance status in acromegalic patients. Clin Endocrinol 52:549–555
Drogan D, Schulze MB, Boeing H, Pischon T (2016) Insulin-like growth factor 1 and insulin-like growth factor-binding protein 3 in relation to the risk of type 2 diabetes mellitus: results from the epic-potsdam study. Am J Epidemiol 183(6):553–560
Fieffe S, Morange I, Petrossians P et al (2011) Diabetes in acromegaly, prevalence, risk factors, and evolution: data from the French Acromegaly Registry. Eur J Endocrinol 164:877–884
Dreval AV, Trigolosova IV, Misnikova IV et al (2014) Prevalence of diabetes mellitus in patients with acromegaly. Endocr Connect 3:93–98
Colao A, Auriemma RS, Galdiero M et al (2009 Feb) Impact of somatostatin analogues versus surgery on glucose metabolism in acromegaly: results of a 5-year observational, open, prospective study. J Clin Endocrinol Metab 94(2):528–537
Grasso LF, Auriemma RS, Pivonello R, Colao A (2015) Adverse events associated with somatostatin analogs in acromegaly. Expert Opin Drug Saf 14(8):1213–1226
Caron P, Morange-Ramos I, Cogne M, Jaquet P (1997) Three year follow up of acromegalic patients treated with intramuscular slow-release lanreotide. J Clin Endocrinol Metab 82(1):18–22
Mazziotti G, Floriani I, Bonadonna S et al (2009) Effects of somatostatin analogues on glucose homeostasis: a metaanalysis of acromegaly studies. J Clin Endocrinol Metab 94(5):1500–1508
Jonas C, Maiter D, Alexopoulou O (2016) Evolution of glucose tolerance after treatment of acromegaly: a study in 57 patients. Horm Metab Res 48(5):299–305
Valea A, Carsote M, Ghervan C, Georgescu C (2015) Glycemic profile in patients with acromegaly treated with somatostatin analogue. J Med Life 8 Spec Issue:82–86
Pereira AM, Biermasz NR, Roelfsema F, Romijn JA (2005) Pharmacologic therapies for acromegaly: a review of their effects on glucose metabolism and insulin resistance. Treat Endocrinol 4(1):43–53
Mazziotti G, Porcelli T, Bogazzi F et al (2011 Mar) Effect of high dose octreotide LAR on glucose metabolism in patients with acromegaly inadequately controlled by conventional somatostatin analog therapy. Eur J Endocrinol 164(3):341–347
Colao A, Bronstein MD, Freda P et al (2014) Pasireotide versus octreotide in acromegaly: a head-to-head superiority study. J Clin Endocrinol Metab 99(3):791–799
Ho KK, Jenkins AB, Furler SM et al (1992) Impact of octreotide, a long-acting somatostatin analogue, on glucose tolerance and insulin sensitivity in acromegaly. Clin Endocrinol 36(3):271–279
Colao A (2012) Improvement of cardiac parameters in patients with acromegaly treated with medical therapies. Pituitary 15(1):50–58
Higham CE, Rowles S, Russell-Jones D et al (2009) Pegvisomant improves insulin sensitivity and reduces overnight free fatty acid concentrations in patients with acromegaly. J Clin Endocrinol Metab 94(7):2459–2463
Kinoshita Y et al (2011) Impaired glucose metabolism in Japanese patients with acromegaly is restored after successful pituitary surgery in pancreatic b-cell function is preserved. Eur J Endocrinol 164:467–473
Singh V, Brendel MD, Zacharias S et al (2007) Characterization of somatostatin receptor subtype-specific regulation of insulin and glucagon secretion: an in vitro study on isolated human pancreatic islets. J Clin Endocrinol Metab 92(2):673–680
Braun M (2014) The somatostatin receptor in human pancreatic β-cells. Vitam Horm 95:165–193
Lamberts SW, Uitterlinden P, Verschoor L et al (1985) Long-term treatment of acromegaly with the somatostatin analogue SMS 201–995. N Engl J Med 313(25):1576–1580
Breidert M, Pinzer T, Wildbrett J et al (1995) Long-term effect of octreotide in acromegaly on insulin resistance. Horm Metab Res 27(5):226–230
Ronchi CL, Varca V, Beck-Peccoz P et al (2006) Comparison between six-year therapy with long-acting somatostatin analogues and successful surgery in acromegaly: effects on cardiovascular risk factors. J Clin Endocrinol Metab 91(1):121–128
Steffin B, Gutt B, Bidlingmaier M et al (2006) Effects of the long-acting somatostatin analogue Lanreotide Autogel on glucose tolerance and insulin resistance in acromegaly. Eur J Endocrinol 155(1):73–78
Henry RR, Ciaraldi TP, Armstrong D, Burke P, Ligueros-Saylan M, Mudaliar S (2013) Hyperglycemia associated with pasireotide: results from a mechanistic study in healthy volunteers. J Clin Endocrinol Metab 98(8):3446–3453
Zambre Y, Ling Z, Chen MC, Hou X et al (1999) Inhibition of human pancreatic islet insulin release by receptor-selective somatostatin analogs directed to somatostatin receptor subtype 5. Biochem Pharmacol 57(10):1159–1164
Chisholm C, Greenberg GR (2002) Somatostatin-28 regulates GLP-1 secretion via somatostatin receptor subtype 5 in rat intestinal cultures. Am J Physiol Endocrinol Metab 283(2):E311–E317
Gadelha MR, Bronstein MD, Brue T et al (2014) Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controller acromegaly (PAOLA): a randomised, phase 3 trial. Lancet Diabetes Endocrinol 2(11):875–884
Grasso LF, Pivonello R, Colao A (2013) Investigational therapies for acromegaly. Expert Opin Investig Drugs 22(8):955–963
Schmid HA, Brue T, Colao A et al (2016) Effect of pasireotide on glucose- and growth hormone-related biomarkers in patients with inadequately controlled acromegaly. Endocr 53(1):210–219
Schreiber I, Buchfelder M, Droste M et al (2007) Treatment of acromegaly with the GH receptor antagonist Pegvisomant in clinical practice: safety and efficacy evaluation from the German Pegvisomant Observational Study. Eur J Endocrinol 156:75–82
Drake WM, Rowles SV, Roberts ME et al (2003) Insulin sensitivity and glucose tolerance improve in patients with acromegaly converted from depot octreotide to Pegvisomant. Eur J Endocrinol 149:521–527
Barkan AL, Burman P, Clemmons DR et al (2005) Glucose homeostasis and safety in patients with acromegaly converted from long-acting octreotide to Pegvisomant. J Clin Endocrinol Metab 90:5684–5691
Ghigo E, Biller BM, Colao A et al (2009) Comparison of Pegvisomant and long-acting octreotide in patients with acromegaly naïve to radiation and medical therapy. J Endocrinol Invest 32:924–933
Lindberg-Larsen R, Møller N, Schmitz O et al (2007) The impact of Pegvisomant treatment on substrate metabolism and insulin sensitivity in patients with acromegaly. J Clin Endocrinol Metab 92:1724–1728
Higham CE, Rowles S, Russell-Jones D et al (2009) Pegvisomant improves insulin sensitivity and reduces overnight free fatty acid concentrations in patients with acromegaly. J Clin Endocrinol Metab 94:2459–2463
Rose DR, Clemmons DR (2002) Growth hormone receptor antagonist improves insulin resistance in acromegaly. Growth Horm IGF Res 12:418–424
Trainer PJ, Ezzat S, D’Souza GA et al (2009) A randomized, controlled, multicentre trial comparing Pegvisomant alone with combination therapy of Pegvisomant and long-acting octreotide in patients with acromegaly. Clin Endocrinol 71:549–557
Moller L, Norrelund H, Jessen N et al (2009) Impact of growth hormone receptor blockade on substrate metabolism during fasting in healthy subjects. J Clin Endocrinol Metab 94(11):4524–4532
Kokshoorn NE, Biermasz NR, Roelfsema F et al (2011) GH replacement therapy in elderly GH-deficient patients: a systematic review. Eur J Endocrinol 164(5):657–665
Rosario PW (2011) Frequency of acromegaly in adults with diabetes or glucose intolerance and estimated prevalence in the general population. Pituitary 14(3):217–221
Wildbrett J, Hanefeld M, Fucker K et al (1997) Anomalies of lipoprotein pattern and fibrinolysis in acromegalic patients: relation to growth hormone levels and insulin–like growth factor I. Exp Clin Endocrinol Diabetes 105:331–335
Linton MF, Yancey PG, Davies SS, Jerome WGJ, Linton EF, Vickers KC (2000–2015) The role of lipids and lipoproteins in atherosclerosis. In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A (eds) Source Endotext [Internet]. MDText.com, Inc., South Dartmouth
Chaves VE, Júnior FM, Bertolini GL (2013) The metabolic effects of growth hormone in adipose tissue. Endocr 44(2):293–302
Beentjes JA, van Tol A, Sluiter WJ, Dullaart RP (2000) Low plasma lecithin: cholesterol acyltransferase and lipid transfer protein activities in growth hormone deficient and acromegalic men: role in altered high density lipoproteins. Atherosclerosis 153:491–498
Delaroudis SP, Efstathiadou ZA, Koukoulis GN et al (2008) Amelioration of cardiovascular risk factors with partial biochemical control of acromegaly. Clin Endocrinol 69(2):279–284
Giustina A, Ambrosio MR, Beck Peccoz P et al (2014) Use of pegvisomant in acromegaly. An Italian Society of Endocrinology guideline. J Endocrinol Invest 37(10):1017–1030
Parkinson C, Drake WM, Wieringa G et al (2002) Serum lipoprotein changes following IGF-I normalization using a growth hormone receptor antagonist in acromegaly. Clin Endocrinol 56(3): 303–311
Sesmilo G, Fairfield WP, Katznelson L et al (2002) Cardiovascular risk factors in acromegaly before and after normalization of serum IGF-I levels with the GH antagonist pegvisomant. J Clin Endocrinol Metab 87(4):1692–1699
Berg C, Petersenn S, Lahner H et al (2010) Cardiovascular risk factors in patients with uncontrolled and long-term acromegaly: comparison with matched data from the general population and the effect of disease control. J Clin Endocrinol Metab 2010;95:3648–3656
Hodish I, Barkan A (2008) Long-term effects of Pegvisomant in patients with acromegaly. Nat Clin Pract Endocrinol Metab 4:324–332
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pivonello, R., Auriemma, R.S., Grasso, L.F.S. et al. Complications of acromegaly: cardiovascular, respiratory and metabolic comorbidities. Pituitary 20, 46–62 (2017). https://doi.org/10.1007/s11102-017-0797-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0797-7