Abstract
Purpose
Thyrotropin-secreting pituitary adenomas (TSHomas) represent a rare subtype of pituitary tumors. Neurosurgery (NCH) is still considered the first-line therapy. In this study we aimed to investigate the outcome of different treatment modalities, including first line somatostatin analogs (SSA) treatment, with a specific focus on neurosurgery-related complications.
Methods
We retrospectively evaluated thirteen patients diagnosed for TSHomas (9 M; age range 27–61). Ten patients had a magnetic resonance evidence of macroadenoma, three with slight visual field impairment. In the majority of patients, thyroid ultrasonography showed the presence of goiter and/or increased gland vascularization. Median TSH value at diagnosis was 3.29 mU/L (normal ranges 0.2–4.2 mIU/L), with median fT4 2.52 ng/dL (0.9–1.7 ng/dL).
Results
Three patients (two microadenoma) were primarily treated with NCH and achieved disease remission, whereas ten patients (nine macroadenomas) were initially treated with SSA. Despite the optimal biochemical response observed during medical treatment in most patients (mean TSH decrease −72 %), only two stayed on medical therapy alone, achieving stable biochemical control at the end of the follow-up. The remaining patients (n = 7) underwent NCH later on during their clinical history, followed by radiotherapy or adjuvant SSA treatment in two cases. Noteworthy, five of them developed hypopituitarism. All patients reached a biochemical control, after a multimodal therapeutic approach.
Conclusions
Neurosurgery ultimately led to complete disease remission or to biochemical control in majority of patients, whereas resulting in a considerable percentage of post-operative complications (mainly hypopituitarism, 50 %). In the light of the optimal results unanimously reported for medical treatment with SSA, our experience suggests that a careful evaluation of risk/benefit ratio should be taken into consideration when directing the treatment approach in patients with TSHoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyrotropin-secreting adenomas (TSHomas) are a rare subtype of pituitary tumors, representing less than 2 % of all adenoma histotypes. However, very recently the first estimate of a national incidence of TSHomas, conducted in the Swedish population, suggested a significant increase (about threefold) in their incidence and prevalence, in agreement with reports on other type of pituitary adenomas [1]. TSHomas may result in a rare form of central hyperthyroidism, characterized by elevated circulating thyroid hormones (free-T3 and free-T4) in presence of inappropriately normal or high TSH levels. This entity has to be differentiated by the syndrome of central resistance to thyroid hormone (RTH) on the basis of clinical symptoms, specific biochemical parameters (e.g. α-subunit levels), pituitary magnetic resonance imaging (MRI), as well as dynamic tests (high T3 doses suppression test and/or TRH stimulation test). Misdiagnosis, or even just a delayed diagnosis, of patients with central hyperthyroidism may result in an inappropriate thyroidectomy, and/or permanent visual field defects and hypopituitarism due to the progressive enlargement of the undiagnosed pituitary tumor [2, 3].
TSHomas are usually benign lesions, which commonly present at diagnosis as macroadenomas (about 80 % of reported cases) with a largely positive immunostaining for TSH. However, they may co-secrete other anterior-pituitary hormones, such as growth hormone (GH) or prolactin (PRL) in 15 and 10 % of cases, respectively [1, 4].
To date, the standard therapeutic options include neurosurgery, medical therapy with somatostatin analogues (SSA) and/or dopamine agonists (DA), and radiotherapy [5, 6]. Surgery is still considered the first-line treatment, with an estimated cure rate around 30–40 %. These rather disappointing results are probably due to both the peculiar tumor tissue characteristics (reported by several neurosurgeons as hard and fibrous) and the frequent occurrence of local invasion of the cavernous sinus or other extrasellar structures observed in these patients. The same factors may also account for the reported high percentage of transient and/or permanent post-surgical complications observed as a result of difficult resection and dissection procedures [7].
On the other hand, TSHomas usually show a satisfactory response to medical treatment with SSA, which can induce biochemical control in about 80 % and tumor shrinkage in 30–40 % of patients [8, 9]. The peculiar and predominant expressions on tumor cell membrane of the somatostatin receptor subtype 2 (sst2) and 5 (sst5), preferential targets of the currently available SSA, represent the pathophysiological basis for the efficacy of SSA treatment in TSHomas [10]. Moreover, very recently the first case of a TSHoma patient “cured” by medical therapy with SSA monotherapy has been described [11].
Despite the well-recognized role of SSA in the control of hormone hypersecretion and related clinical symptoms, the use of SSA as a first line treatment for TSHomas has not been officially accepted yet. In this context, the relatively high-cost of long-term SSA treatment currently represents one of the main issues for a standardized first line approach with medical therapy in these tumors.
In this study, we retrospectively evaluated thirteen patients diagnosed for TSH-secreting pituitary adenomas, referred to two Italian and one French centers in the last 20 years. In order to weight the relative risk/benefit ratio in this cohort of patients, we aimed to investigate the outcome of different treatment modalities, with a specific focus on the most commonly reported treatment-related side effects and/or complications.
Subjects and methods
Subjects
A multicenter retrospective cohort design was used. The clinical data of thirteen patients diagnosed for TSHomas (from 1993 to 2011) at three referral centers for pituitary diseases were reviewed and analyzed. Partial data from three patients have been previously reported [12].
Diagnosis of TSH-secreting pituitary tumors was based on the combination of clinical findings (signs and symptoms of hyperthyroidism, tumor mass effect on the surrounding anatomical structures, e.g. visual field defects), biochemical evidence of measurable (normal or high) TSH levels contrasting with elevated serum free thyroid hormone levels, and the identification of a pituitary adenoma by MRI. Additional diagnostic tool (performed in five cases) was the evaluation of dynamic response of TSH to intravenous thyrotropin-releasing hormone (TRH) administration (TRH test). Somatostatin receptor scintigraphy was performed in one patient (Fig. 1).
111In-Pentetreotide scintigraphy (Octreoscan® with CT-SPECT acquisitions) in patient n. 12. An intense radiotracer uptake (arrows) is observed in correspondence of the sellar region in transversal, sagittal and coronal reconstructions. The physiological uptake of the radiotracer by the salivary glands and tonsils is evident, as well (arrowheads). Images have been recorded 24 h after i.v. injection of 185 MBq (5 mCi) of 111Indium, using the following setting for CT/SPECT scintigraphy: SPECT, 128 × 128 matrix, 32 pictures of 30 s/frame each gamma camera head; CT, dose efficacy 130 kV, 80mAs, slice thickness 3 mm
Data extracted from the clinical charts included general patients information (e.g. sex, age at diagnosis), latency time for diagnosis, laboratory studies (including dynamic tests), sellar MRI, visual field tests, surgical procedures, pituitary specimens immunohistochemistry, and results of medical therapy. Data concerning baseline evaluation of thyroid gland status (ultrasonography and/or labeled-iodine scintigraphy imaging, study of thyroid autoimmunity), and the assessment of global anterior pituitary function were collected and reported, as well.
Prior to SSA treatment, an acute octreotide test was carried out in three patients. A dose of 100 µg of octreotide was injected subcutaneously at 08:00, and blood samples for TSH (and fT4) were collected every hour for 6 h.
Patients underwent different treatment approaches including neurosurgery (transsphenoidal adenomectomy) or SSA therapy alone, SSA treatment prior neurosurgery, post-surgery radiotherapy and neo-adjuvant plus adjuvant SSA treatment.
In eleven patients, where long-term follow up data were available, we evaluated the outcome of the different treatment modalities and the treatment-related side effects and/or complications. These latter mainly consisted in the persistent impairment of anterior pituitary function (hypopituitarism).
Moreover, the prevalence of the surgery-related complications reported in our TSHoma cohort has been compared with an age-sex-tumor size matched group of 25 GH-secreting adenomas (GHomas). Detailed characteristics of this group, representing a consecutive series of the most recent operated GHomas registered in our records, are reported in Supplementary Table 1.
This retrospective study was conducted in accordance with the recommendations of the Declaration of Helsinki, and all patients provided an informed consent.
Magnetic resonance imaging
A 1.5-T MRI study of pituitary region with and without Gadolinium contrast enhancement (1.0 mmol/kg) was performed in all patients. The size and enhancement pattern of the adenomas were evaluated and independently reviewed by the neuroradiology staff of the three centers participating to the study.
Hormone assays
Serum TSH, fT3 and fT4 levels were measured by means of ultra-sensitive chemiluminescence immunoassay (Roche Diagnostics, Mannheim, Germany). Normal ranges are 0.2–4.2 mIU/L for TSH, 2.0–4.4 pg/mL for fT3 and 0.9–1.7 ng/dL for fT4.
Criteria for remission
Patients with TSH-secreting adenomas were considered in remission when no residual tumor was detected on imaging follow-up, in presence of normalized or below normal TSH levels and normal free thyroxine levels (with or without thyroid hormone replacement therapy).
Diagnosis of post-surgical pituitary function impairment
Global anterior pituitary function was assessed after surgery in all patients by measurement of fasting serum GH, IGF-I, PRL, ACTH, cortisol, LH, FSH, estrogen (women) and testosterone (men). When the impaired secretion of one or more pituitary hormone was suspected, dedicated dynamic tests were performed. In detail, GH-deficiency was defined evaluating the GH response to GHRH + Arginine test [13], ACTH-deficiency by use of the CRH test [14]. Moreover, the presence of central hypogonadism was defined on the basis of clinical sign and symptoms (e.g. menstrual cycle history in pre-menopausal women), low basal testosterone or estrogen concentrations, in the presence of decreased or normal LH and FSH levels, followed by GnRH test [15].
Statistical analysis
SPSS for Windows 20.0 (SPSS Inc., Chicago, IL) was used for statistical analyses. Results are expressed as mean ± SD [or as median (range)] for quantitative variables, and as a percentage for qualitative variables. Differences between frequencies were evaluated by Chi square test. The comparison between TSH and free thyroid hormone levels at the beginning of the study and at the end of follow-up period was analyzed by the Mann–Whitney U test. Differences were taken to be statistically significant at p < 0.05.
Results
Baseline assessment
Our study group included nine male and four female patients, with a median age at diagnosis of 42 years (range, 27–61 years). Median latency time between onset of hyperthyroidism and diagnosis of pituitary adenoma was 4.5 months (range 2–36). Data from eleven patients were available for long-term follow up evaluation (date of the assessment of the surgical and biochemical outcome of the patients) (median 4.0 years; range 1.0–19).
MRI of the sellar region was suggestive for the presence of a pituitary adenoma in all cases. In line with previous reports in literature, ten out of thirteen patients had a macroadenoma, with extrasellar expansion in five (mostly suprasellar) and both suprasellar extension and left sphenoid sinus invasion in one case (patient n. 9 in the Tables).
Visual field defects were reported in three patients: one slight bitemporal hemianopia, one upper right temporal hemianopia and one upper left temporal hemianopia. Two patients (patient n. 8 and n. 10 in the Tables) had a normal visual field test despite the evidence of suprasellar invasion.
Thyroid gland imaging was performed by ultrasonography (US) in all subjects. Three patients had a multinodular goiter, four a diffuse goiter, one a single nodule, while three patients showed a diffuse enhanced parenchymal vascularization after color-doppler evaluation.
Four patients (n. 4, 8, 10 and 12 in the Tables) underwent thyroid scintigraphy [Technetium (Tc99m) Pertechnetate] as well, showing in one case intermediate and heterogeneous fixation and in three cases a diffuse increased uptake of the radiotracer, suggestive for an enhanced functional status of the gland. However, no patient included in our cohort underwent thyroidectomy, nor before the diagnosis of TSH-secreting adenoma neither during the follow-up period.
At baseline evaluation, TSH values were high or inadequately high in all patients (median 3.29 mU/L, range 1.25–13.24), with free T4 levels (median 2.52 ng/dl, range 1.82–3.87) borderline-high in four patients and suggestive for overt hyperthyroidism in the remaining nine.
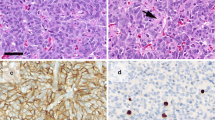
Moreover, none of our patients had biochemical evidence of co-secretion of other anterior pituitary hormones, despite the post-operative immunohistochemical evaluation showed a positive staining for GH in two tumor samples and for both GH and PRL in one case. As expected, all samples analyzed (n = 10) were diffusely positive for TSH immunostaining.
The detailed general and clinical characteristics of the patients included in the study are shown in Table 1.
Dynamic tests
The TSH response after intravenous injection of 200 μg TRH (TRH test) was evaluated in five patients (namely patient 1, 2, 7, 9 and 13 in the Tables). Four out of five (80 %) had absent response to TRH (TSH increase <2 mU/L), while one patient showed a normal response, defined as a TSH increase of >200 % of baseline or >5 mU/L [16].
Prior to treatment with SSA, an acute octreotide test was performed in three patients, as above described, with a significant TSH reduction observed in all patients, ranging from −62 to −81 % (basal vs. nadir).
Disease management and treatment outcome
As depicted in the flow diagram (Fig. 2), patients included in the study underwent different treatment approaches based on the treatment modalities available at the time of diagnosis and the individual patient characteristics (including patients compliance).
More in detail, two out of the three microadenoma patients underwent neurosurgery as first line therapy and achieved disease remission without evidence of any post-operative complication. The third patient harboring a microadenoma was primarily treated with SSA but was lost at follow-up before the first post-treatment examination. One patient with a small macroadenoma without signs of cavernous sinus invasion (enclosed tumor, patient n. 10), underwent first-line surgery resulting in complete tumor removal and biochemical control.
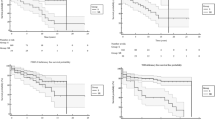
All other macroadenoma patients (n = 9) were treated with SSA as first-line. Two patients (n. 1 and 10 in the Tables) were considered non-responders to SSA treatment, failing to reach complete biochemical control, after at least 1 year of therapy. On the other hand, seven of the nine macroadenomas patients (78 %) showed an optimal biochemical response to SSA treatment (long-acting release formulations in 6 cases, short-acting subcutaneous in one) achieving significant reduction of both TSH and fT4 levels (Fig. 3a). Moreover, patient n. 8 showed an impressive tumor shrinkage after only 3 months of medical treatment, as already described in a previous study [12], while patient n. 6 showed a slight tumor shrinkage (21 % reduction of maximum diameter after 1 year SSA treatment), with a partial resolution of the visual field impairment.
Percent TSH and fT4 reduction versus baseline in patients responder to SSA treatment (a) and in all patients which concluded the study, at the end of follow-up (b). a In line with previous data from literature, patients showed a general good response to SSA treatment. In particular, seven out of nine patients even after short term treatment (at low doses) had a significant decrease of both TSH and fT4 (TSH −72 % ± 15; fT4 −38 % ± 24). b All patients reached the biochemical control at the end of follow-up (n = 11, two patients were lost at follow-up), despite the different therapeutic approaches, showing a significant decrease of both TSH and fT4 levels (TSH −73 % ± 16; fT4 −48 % ± 29). Percent TSH and fT4 decrease are expressed as mean ± standard deviation. Statistically relevant differences (p < 0.05) are reported in each graph
However, only two patients (n. 3 and 4 in the Tables) stayed on SSA therapy alone, showing complete biochemical control and stable tumor volume at the end of follow-up. Afterwards, the other five macroadenoma patients underwent neurosurgery, despite the normalization of biochemical parameters observed after short term (median 3 months) treatment with relatively low doses of SSA [octreotide s.c. 100 µg trice a day (n = 1), octreotide LAR 20 mg every 4 weeks (n = 2) or lanreotide autogel 60 mg every 4 weeks (n = 2)]. More in detail, the decision for neurosurgery in these five SSA good responder patients was driven by: presence of visual defects in two cases (patient n. 6 and 7), lack of compliance of patient n. 8 after four months therapy, decision for debulking surgery in agreement with the neurosurgeon for patient n. 9 (adenoma with left sphenoidal sinus invasion and tumor max diameter of 26 mm) and intent for curative surgery in patient n. 12 (small macroadenoma without sinus invasion).
In conclusion, of the seven patients that underwent surgery as second treatment option (the two SSA non-responders, plus the above described five patients showing good response to SSA), three achieved complete disease remission, one reached biochemical control in the presence of stable tumor remnant and one was lost at follow-up after the operation. Moreover, one patient needed post-surgery radiotherapy (patient n. 10) and one started adjuvant SSA treatment and achieved the biochemical control at the end of the follow-up period (Fig. 2).
Noteworthy, this latter patient (n. 9 in the Tables) showed a significant shrinkage of the tumor remnant, which become almost undetectable at MRI evaluation during post-surgical SSA treatment. However, after 1-year drug withdrawal, in parallel with a slight increase of both TSH and fT4 levels, the remnant tumor displayed a volume increase (back to the first post-surgical imaging), and SSA therapy was, therefore, successfully re-started.
Despite the different therapeutic approaches, all patients reached biochemical control at the end of follow-up showing a significant reduction of both TSH and fT4 levels (Fig. 3b).
Post-surgical complications rate
As above mentioned, ten patients underwent neurosurgery during their clinical history.
Five out of ten patients were diagnosed during the follow-up period (median 4 years) for partial anterior hypopituitarism (three isolated ACTH-deficiency, one GH-deficiency associated with central hypogonadism and one GH-deficiency in presence of central hypothyroidism). Noteworthy, none of these patients had impairment of anterior pituitary function (other than TSH secretion) at baseline assessment. Moreover, one patient (n. 7 in the Tables) experienced a severe post-operative CSF rhinorrhea that required a second operation and prolonged hospitalization.
Notably, out of the four patients that did not experience any post-surgical complication, two were harboring a microadenoma and achieved complete disease remission, while other two patients had a macroadenoma, were treated with SSA before surgery, and still showed a tumor remnant after the surgical procedure. On the other hand, the four macroadenoma patients which achieved complete disease remission after surgery (biochemical control as well as no residual tumor at MRI) all showed a partial anterior hypopituitarism at the end of the follow-up (Table 2).
When compared with an age-sex-tumor size matched group of 25 GHomas (see Supplementary Table), we observed that the percentage of patients developing post-surgical hypopituitarism was significantly higher in the TSHoma group (5/10, 50 % vs. 3/25, 12 %; Chi square p value: 0.016).
Discussion
TSH-secreting pituitary adenomas represent a rare cause of central hyperthyroidism. The key step for a proper diagnosis is the evidence of a pituitary adenoma on MRI combined with normal or inappropriately high TSH concentrations in presence of elevated free-thyroid hormone levels [2]. The autonomous TSH production may often result in an enlarged thyroid volume, thus increasing the risk of misdiagnosis (primary vs. secondary hyperthyroidism) in absence of appropriate and careful clinical evaluation. Nowadays, the latency between the first reported symptoms and the correct diagnosis of TSHoma has been significantly shortened. This is clear when comparing the percentage of patients which underwent thyroidectomy or radio-iodine therapy before TSHoma diagnosis in the old series (up to 40–60 %) [7, 16], with the more recent reports (<20 %) [17, 18]. In line with this observation, none of the patient included in our study underwent thyroidectomy or radio-iodine therapy. Indeed, our cohort shows a relatively short “latency time to diagnosis” (median 4.5 months).
In this context, some authors speculated about a possible correlation between a long latency time to diagnosis and the high prevalence of macroadenomas observed in TSHoma series [4, 19]. However, the critical analysis of the data reported in literature so far seems not to support this hypothesis. Indeed, most of the studies published to date (and the current study as well), report a percentage of macroadenomas ranging from 70 to 90 %, with a latency time to diagnosis varying from 4.5 months to 9 years. The only study reporting a higher percentage of microadenomas (55 %) [18] is associated with a mean latency time to diagnosis of more than 3 years (39 months), not significantly shorter compared to what observed in other studies reporting a higher prevalence of macroadenomas [4, 17, 20].
The first-line therapeutic approach for TSHomas is still considered neurosurgery (namely transsphenoidal adenomectomy), followed by medical therapy with SSAs and/or radiotherapy. The cure rate of the single surgical procedure ranges between 25 to 58 % in majority of the reported series [4, 5, 7, 16, 21], with an average success rate of 40 % [2]. These quite unsatisfactory results are likely related to the peculiar tumor characteristics, which often present as large macroadenomas with tendency to local invasion and extrasellar extension. Moreover, the ‘typical’ fibrous and hard tumor consistency reported for TSHomas, get the surgical procedure even more complicated [19].
In our opinion, all these negative factors do not only influence the cure/remission rate of the surgical procedure, but could also have a role on the onset of intra- and post-operative complications (such as bleeding, liquorrhea, diabetes insipidus and, mainly, hypopituitarism).
Clarke and colleagues conducted a retrospective analysis reviewing the surgical outcome of 20 TSHoma patients which underwent neurosurgery at Mayo Clinic (out of >5,000 adenomas available in their clinical reports). Together with a surgical remission rate of 50 % (10/20), they described the occurrence of post-surgical pan- or anterior hypopituitarism in 30 % of patients (6/20) [7]. Moreover, in a previous study from a NIH series by Brucker-Davis et al., out of 25 TSHoma patients with a surgical remission rate of 35 %, the authors reported three deaths and a number of postoperative complications, such as cerebrospinal leak, pan-hypopituitarism, transient or permanent diabetes insipidus and isolated persistent central hypothyroidism. On the contrary, in a recent study conducted by Malchiodi and colleagues, reporting a case series referred from two centers in Milan (Italy), 23/68 patients (34 %) were cured after first surgery, with an unexpected extremely low rate (9 %) of new pituitary deficiencies after surgery. An explanation for these discrepancy can be the rate of pituitary deficiencies observed at baseline evaluation in the Milan cohort (nearly 13 %), with a disclosed underestimation for GH-deficiency, that was not tested in 66 % of patients.
Finally, a very recent paper published by Kirkman et al. [22], retrospectively evaluating 38 TSHoma patients, again reported a high rate of post-surgical hypopituitarism. More in detail, after a mean follow-up of 6.7 years, the authors showed that 16 % of patients required thyroxine replacement, 22 % testosterone replacement, 28 % hydrocortisone, 3 % desmopressin and another 3 % growth hormone [22].
In the light of these conflicting results, the major challenge in understanding the exact rate of surgery-related complications in TSHomas is due to the fact that none of these studies primarily focused on this specific outcome, and often the post-surgical evaluation of anterior pituitary axis (other than the pituitary-thyroid axis) is not adequately performed or described.
In line with the findings of Clarke, Bruker-Davis and Kirkman, in our series we observed a high percentage of post-surgical complications (60 %, 5/10 partial anterior hypopituitarism, plus one case of severe CSF rhinorrhea), associated with a relatively high cure rate after surgery (55 %, alone or in combination with short-term neo-adjuvant SSA treatment). However, it should be also emphasized that all the patients reported in the present series were referred to skilled, expert pituitary neurosurgeons, working in a multidisciplinary team and operating more than 30 pituitary tumors per year.
The occurrence of post-surgical complications (in particular postoperative endocrine dysfunctions) in the TSHoma patients described in our cohort was significantly higher compared with an age–sex–tumor size matched control group of GHomas (12 % of post-operative complication rate) extracted from our clinical records. Noteworthy, the results from our control group are in line with previously reported data describing the post-surgical complication rate in large series of GHomas (about 10 %) [23].
The finding of a high rate of post-surgical hypopituitarism in TSHomas, despite coming from a small cohort of patients and, therefore, requiring further confirmation possibly through bigger International multi-centric studies, further raises the question of the right management of TSHomas and the role of SSA in their treatment algorithm [2]. Indeed, a number of studies have recently pointed out the role of SSA treatment as a valuable first line treatment in selected TSHoma patients [11, 17], similarly to what already stated for GH-secreting adenomas in the last published disease management guidelines [24]. Moreover, the reported response rate to SSA in TSHomas, considering both the biochemical response (about 90 % cases being controlled) and the tumor shrinkage rate (30–40 %), seems to be even superior when compared to the results reported for SSA treatment in acromegaly [2, 25].
In this light, it is noteworthy that the satisfactory results of SSA treatment (7/9 good responders, 2 cases of tumor shrinkage) reported in the present study have been achieved after short time treatment (3 months median), without any attempt of dose titration, except for the two patients that declined surgery and stayed on SSA monotherapy. However, these latter patients achieved a complete biochemical control, in presence of stable tumor mass, at the end of follow-up.
In conclusion, the results of the present study and the analysis of the (few) data available in literature to date, lay for a high rate of post-surgical complications in TSH-secreting adenomas. If confirmed in larger studies, this finding, together with the well-recognized efficacy of SSA treatment, should drive us to re-consider the role of SSA in the management of TSHomas.
Indeed, the risk for a life-long hormone replacement therapy, with its impact on patient quality of life, should be carefully weighted when directing the treatment approach in TSHoma patients.
References
Onnestam L, Berinder K, Burman P, Dahlqvist P, Engstrom BE, Wahlberg J, Nystrom HF (2013) National incidence and prevalence of TSH-secreting pituitary adenomas in Sweden. J Clin Endocrinol Metab 98(2):626–635. doi:10.1210/jc.2012-3362
Beck-Peccoz P, Persani L, Mannavola D, Campi I (2009) Pituitary tumours: TSH-secreting adenomas. Best Pract Res Clin Endocrinol Metab 23(5):597–606. doi:10.1016/j.beem.2009.05.006
Refetoff S (1993) Resistance to thyroid hormone. Clin Lab Med 13(3):563–581
Socin HV, Chanson P, Delemer B, Tabarin A, Rohmer V, Mockel J, Stevenaert A, Beckers A (2003) The changing spectrum of TSH-secreting pituitary adenomas: diagnosis and management in 43 patients. Eur J Endocrinol 148(4):433–442
Losa M, Giovanelli M, Persani L, Mortini P, Faglia G, Beck-Peccoz P (1996) Criteria of cure and follow-up of central hyperthyroidism due to thyrotropin-secreting pituitary adenomas. J Clin Endocrinol Metab 81(8):3084–3090
Beck-Peccoz P (2011) Treatment of central hypothyroidism. Clin Endocrinol (Oxf) 74(6):671–672. doi:10.1111/j.1365-2265.2011.04037.x
Clarke MJ, Erickson D, Castro MR, Atkinson JL (2008) Thyroid-stimulating hormone pituitary adenomas. J Neurosurg 109(1):17–22. doi:10.3171/JNS/2008/109/7/0017
Caron P, Arlot S, Bauters C, Chanson P, Kuhn JM, Pugeat M, Marechaud R, Teutsch C, Vidal E, Sassano P (2001) Efficacy of the long-acting octreotide formulation (octreotide-LAR) in patients with thyrotropin-secreting pituitary adenomas. J Clin Endocrinol Metab 86(6):2849–2853
Beck-Peccoz P, Persani L (2002) Medical management of thyrotropin-secreting pituitary adenomas. Pituitary 5(2):83–88
Gatto F, Barbieri F, Castelletti L, Arvigo M, Pattarozzi A, Annunziata F, Saveanu A, Minuto F, Castellan L, Zona G, Florio T, Ferone D (2011) In vivo and in vitro response to octreotide LAR in a TSH-secreting adenoma: characterization of somatostatin receptor expression and role of subtype 5. Pituitary 14(2):141–147. doi:10.1007/s11102-010-0271-2
Fliers E, van Furth WR, Bisschop PH (2012) Cure of a thyrotrophin (TSH)-secreting pituitary adenoma by medical therapy. Clin Endocrinol (Oxf) 77(5):788–790. doi:10.1111/j.1365-2265.2012.04405.x
Gatto F, Barbieri F, Gatti M, Wurth R, Schulz S, Ravetti JL, Zona G, Culler MD, Saveanu A, Giusti M, Minuto F, Hofland LJ, Ferone D, Florio T (2012) Balance between somatostatin and D2 receptor expression drives TSH-secreting adenoma response to somatostatin analogues and dopastatins. Clin Endocrinol 76(3):407–414. doi:10.1111/j.1365-2265.2011.04200.x
Colao A, Cotta OR, Ferone D, Torre ML, Ferrau F, Di Somma C, Boschetti M, Teti C, Savanelli MC, Alibrandi A, Trimarchi F, Cannavo S (2013) Role of pituitary dysfunction on cardiovascular risk in primary empty sella patients. Clin Endocrinol (Oxf) 79(2):211–216. doi:10.1111/cen.12122
Kokshoorn NE, Romijn JA, Roelfsema F, Rambach AH, Smit JW, Biermasz NR, Pereira AM (2012) The use of an early postoperative CRH test to assess adrenal function after transsphenoidal surgery for pituitary adenomas. Pituitary 15(3):436–444. doi:10.1007/s11102-011-0344-x
Lieberman SA, Oberoi AL, Gilkison CR, Masel BE, Urban RJ (2001) Prevalence of neuroendocrine dysfunction in patients recovering from traumatic brain injury. J Clin Endocrinol Metab 86(6):2752–2756. doi:10.1210/jcem.86.6.7592
Brucker-Davis F, Oldfield EH, Skarulis MC, Doppman JL, Weintraub BD (1999) Thyrotropin-secreting pituitary tumors: diagnostic criteria, thyroid hormone sensitivity, and treatment outcome in 25 patients followed at the National Institutes of Health. J Clin Endocrinol Metab 84(2):476–486
van Varsseveld NC, Bisschop PH, Biermasz NR, Pereira AM, Fliers E, Drent ML (2013) A long-term follow-up study of eighteen patients with thyrotrophin-secreting pituitary adenomas. Clin Endocrinol (Oxf). doi:10.1111/cen.12290
Macchia E, Gasperi M, Lombardi M, Morselli L, Pinchera A, Acerbi G, Rossi G, Martino E (2009) Clinical aspects and therapeutic outcome in thyrotropin-secreting pituitary adenomas: a single center experience. J Endocrinol Invest 32(9):773–779. doi:10.3275/6479
Sanno N, Teramoto A, Osamura RY (2000) Long-term surgical outcome in 16 patients with thyrotropin pituitary adenoma. J Neurosurg 93(2):194–200. doi:10.3171/jns.2000.93.2.0194
Ness-Abramof R, Ishay A, Harel G, Sylvetzky N, Baron E, Greenman Y, Shimon I (2007) TSH-secreting pituitary adenomas: follow-up of 11 cases and review of the literature. Pituitary 10(3):307–310. doi:10.1007/s11102-007-0020-3
Malchiodi E, Profka E, Ferrante E, Sala E, Verrua E, Campi I, Lania AG, Arosio M, Locatelli M, Mortini P, Losa M, Motti E, Beck-Peccoz P, Spada A, Mantovani G (2014) Thyrotropin-secreting pituitary adenomas: outcome of pituitary surgery and irradiation. J Clin Endocrinol Metab, jc20134376. doi:10.1210/jc.2013-4376
Kirkman MA, Jaunmuktane Z, Brandner S, Khan AA, Powell M, Baldeweg SE (2014) Active and silent thyroid-stimulating hormone-expressing pituitary adenomas: presenting symptoms, treatment, outcomes, and recurrence. World Neurosurg. doi:10.1016/j.wneu.2014.03.031
Gondim JA, Almeida JP, Albuquerque LA, Schops M, Gomes E, Ferraz T, Sobreira W, Kretzmann MT (2011) Endoscopic endonasal approach for pituitary adenoma: surgical complications in 301 patients. Pituitary 14(2):174–183. doi:10.1007/s11102-010-0280-1
Melmed S, Colao A, Barkan A, Molitch M, Grossman AB, Kleinberg D, Clemmons D, Chanson P, Laws E, Schlechte J, Vance ML, Ho K, Giustina A (2009) Acromegaly Consensus, G.: Guidelines for acromegaly management: an update. J Clin Endocrinol Metab 94(5):1509–1517. doi:10.1210/jc.2008-2421
Colao A, Auriemma RS, Lombardi G, Pivonello R (2011) Resistance to somatostatin analogs in acromegaly. Endocr Rev 32(2):247–271. doi:10.1210/er.2010-0002
Acknowledgments
The authors did not receive any specific funding for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gatto, F., Grasso, L.F., Nazzari, E. et al. Clinical outcome and evidence of high rate post-surgical anterior hypopituitarism in a cohort of TSH-secreting adenoma patients: Might somatostatin analogs have a role as first-line therapy?. Pituitary 18, 583–591 (2015). https://doi.org/10.1007/s11102-014-0611-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0611-8