Abstract
Background
Autoimmune hypophysitis (AH) is a rare autoimmune inflammatory disorder of pituitary gland.
Objective
To analyse clinical, hormonal, radiological features and management outcomes of AH.
Design
Retrospective analysis of patients with primary hypophysitis (where secondary causes of hypophysitis were ruled out) was carried out from 2006 to 2012. AH emerged as the most plausible aetiology and the diagnosis of exclusion.
Results
Twenty-four patients with AH (21 females and 3 males) were evaluated. They presented with symptoms of expanding sellar mass (83.3 %), symptoms of anterior pituitary hormone deficiencies (58.3 %), and diabetes insipidus (16.7 %). The anterior pituitary hormonal axes affected were cortisol (75 %), thyroid (58.33 %) and gonadotropin (50 %). All had sellar mass on magnetic resonance imaging, which was symmetrical (91.7 %) and homogenously enhancing (91.7 %). Stalk thickening, suprasellar extension, loss of posterior pituitary hyperintensity and parasellar T2 dark sign were seen in 87.5, 87.5, 71.5, and 50 % respectively. In addition to hormone replacement, five (20.83 %) patients underwent trans-sphenoidal surgery, fifteen (62.5 %) were watchfully monitored, while four cases (16.67 %) received steroid pulse therapy. On follow up imaging, the sellar mass regressed in all, while, stalk thickening was persistent in 13/19 (68.4 %) non-operated patients at median follow up of 1 year. Pituitary hormone axis recovery was seen in 10 (41.67 %) and was seen in cortisol 10/18 (55.5 %) followed by gonadotropin 5/12 (41.67 %) axis.
Conclusion
Characteristic radiology helps in diagnosis of AH even without tissue diagnosis. Non-operative treatment is the preferred treatment modality. Steroid pulse therapy potentially improves pituitary axis recovery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autoimmune hypophysitis (AH) is a rare autoimmune inflammatory disorder involving the pituitary gland. Since the first description by Goudie and Pinkerton in 1962, about 750 cases have been reported to date [1, 2]. Estimated incidence of AH is one in nine million per year [3, 4]. It occurs predominantly in young females, especially in the peripartum period. The classical presentation is symptoms of expanding sellar mass with or without varying degrees of hypopituitarism. The patients may have evidence of other associated autoimmune diseases [3]. Histopathology is required for a definitive diagnosis, but many cases have been managed solely on clinical grounds. The natural history of AH encompasses a wide spectrum which spans from coexistent characteristic clinical, hormonal and radiological features or clinical, hormonal features in presence of normal sellar imaging or just the characteristic imaging features in absence of symptoms and hormonal involvement. [5].
We present our experience with primary hypophysitis (PH) where the secondary causes were ruled out and the autoimmune aetiology remained as the diagnosis of exclusion. Our aim is to analyse clinical, hormonal, radiological features and management outcomes of these cases.
Methods
Patients with PH presenting to a tertiary care centre in western India between 2006 and 2012 were retrospectively analysed. Diagnosis of AH was histopathological or based on characteristic Magnetic resonance imaging (MRI) of the sellar mass and its regression on follow up in the non-operated cohort. Coexistent tuberculosis was ruled out by high resolution computed tomography (HRCT) chest, abdomen and pelvis. Normal serum angiotensin converting enzyme levels were documented to rule out sarcoidosis. Other differentials like Wegener’s granulomatosis and Langerhan’s cell histiocytosis were ruled out clinically. After ruling out the secondary causes, autoimmune aetiology was the diagnosis of exclusion.
Pituitary hormonal deficiencies were defined as follows:
Hypocortisolism was defined as 8 a.m. serum cortisol <137.5 nmol l−1 (5 μg dl−1) while the 8 a.m. serum cortisol levels >275.9 nmol l−1 (10 μg dl−1) were considered normal. Steroid supplement (prednisolone) was withheld for 48 h, prior to blood collection for 8 a.m. serum cortisol on follow up. Central hypothyroidism was defined as total thyroxine <57.91 nmol l−1 (4.5 μg dl−1) with TSH < 10 mIU l−1. Patients were considered to have secondary hypogonadism if the follicular stimulating hormone (FSH) and leutenising hormone (LH) levels were each less than 10 mIU ml−1 in women with oligo/amenorrhoea and in men with low-serum testosterone <10.4 nmol l−1 (<3.0 ng ml−1). The normal range for prolactin was 100–532 mU l−1 (5–25 ng ml−1) for females and 100–425 mU l−1 (5 > 20 ng ml−1) for males. The water deprivation test was done in patients with clinical suspicion of diabetes insipidus (DI). Serum osmolality >295 mosm kg−1 with corresponding urine osmolality <300 mosm kg−1 was considered to be suggestive of DI. Hormonal measurements were carried out by chemiluminescence assay (Advia Centaur CP). Intraassay and interassay coefficients of variation were less than 8 and 10 %, respectively, for all hormonal evaluation.
Dynamic stimulation testing could not be done for hormone deficiencies due to unavailability of pharmacological preparations of adrenocorticotrophic hormone (ACTH), TRH (thyrotropin releasing hormone), CRH (corticotrophin releasing hormone) in India. Evaluation for GH (growth hormone) axis was not done due to resource limited set up.
All patients underwent MRI of pituitary at our centre on a 1.5 T MR system (Sonata Vision; Siemens, Erlangen, Germany) using 8 channel circularly polarised head coil. All the images were reported by a single experienced radiologist in a predefined format.
It included
-
1)
Pituitary enlargement (symmetric or asymmetric),
-
2)
Pituitary enhancement pattern (homogeneous or heterogeneous),
-
3)
Thickened stalk (If the diameter of the pituitary stalk exceeded 3.5 mm at the level of the median eminence of the hypothalamus, the stalk was considered thick),
-
4)
Extension of sellar mass (suprasellar and/or parasellar),
-
5)
Posterior pituitary hyperintensity (PPHI) on T1-weighted images (identified/non identified),
-
6)
The dural tail (identified or not identified), and
-
7)
Parasellar signal intensity on T2-weighted images
Parasellar signal intensity on T2-weighted images was classified as ‘dark’, when it was isointense with bone cortex. If different signal intensities were detected in the parasellar areas, the lowest signal intensity was adopted [6, 7]. Gutenberg et al. have described a score to differentiate hypophysitis from pituitary adenoma. The points included are as follows (the scores are in the bracket): Age ≤30 year−1, Presence of relation to pregnancy (−4), Pituitary volume ≥6cm3 (+2), Medium or high gadolinium enhancement (−1), Heterogenous gadolinium enhancement (+1), Asymmetric sellar enlargement (+3), Loss of posterior pituitary bright spot (−2), Enlarged stalk size (−5), Presence of sphenoid mucosal thickening (+2). This score was calculated for our cohort of AH patients retrospectively [6].
Deficient hormone replacement and symptomatic treatment for headache was offered to all. Operative management included trans-sphenoidal surgery (TSS) by an experienced neurosurgeon (group 1). Non-operated cases were managed conservatively with watchful observation (group 2) or steroid pulse therapy (group 3). Steroid pulse therapy included intravenous methylprednisolone 1 gram/day for three consecutive days, followed by 1 mg/kg/day oral prednisolone for 4 weeks. Thereafter, the steroid dose was tapered by 5 mg/week.
Statistical analysis
Qualitative data was represented in form of frequency and percentage. Association between qualitative variables was assessed by Chi Square test with Continuity Correction for all 2 × 2 tables and Fisher’s Exact test for all 2 × 2 tables where p value of Chi Square test was not valid due to small counts. Adjacent row data of more than 2 × 2 tables was pooled and Chi Square test was reapplied in case more than 20.0 % cells had expected count less than 5.
Association between variables quoted in proportions was assessed by Chi square test for the comparison of two proportions. Quantitative data was represented using mean ± SD. Analysis of Quantitative data between the two groups was done using unpaired t-test. Results were graphically represented where deemed necessary. MedCalc V. 11.3.3.0 was used for analysis.
Results
Twenty-four patients (21 females and 3 male) with AH, diagnosed over 6 years (2006–2012), were analysed. All female patients were in the reproductive age group except for one postmenopausal woman. One patient presented in pregnancy (second trimester) and none presented in postpartum period (till 1 year after delivery). The median age at presentation was 31.5 ± 9.57 years (females: 32 ± 9.9 years, males: 23 ± 4.04 years) and the range being 16–55 years. The median duration from onset of symptoms to diagnosis was 10 weeks (range 1–72 weeks).
The symptoms like headache and vomiting, attributable to an expanding sellar mass were present in 20 (83.3 %) patients. Additionally, cranial nerve palsies (VI nerve in two and III nerve in one) were observed. One patient had left sided temporal visual field cut off. In one case unilateral visual loss was explained by optic neuritis.
The symptoms of anterior pituitary hormone deficiency at presentation were seen in 14 (58.3 %) patients. The classical symptoms of hypothyroidism were seen in three and that of hypocortisolism in one. Out of the 19 females (excluding one pregnant and one postmenopausal patient), menstrual irregularity was present in 10 patients. Galactorrhoea was seen in three (12.5 %) patients. Four (16.7 %) patients presented with DI. Two of them had isolated DI at presentation. The unmasking of DI was not seen in any of the patients after correction of cortisol and thyroid deficiencies. Besides these four, one patient who underwent TSS had post operative permanent DI.
The commonest anterior pituitary deficiency was cortisol axis in 18 (75 %) followed by thyroid 14 (58.33 %) and gonadotropin 12 (50 %) axes. Hyperprolactinaemia was seen in ten (41.67 %) cases ranging from 636 mU l−1 (30 ng ml−1) to 1590 mU l−1 (75 ng ml−1). Decreased prolactin levels were observed in three (12.5 %) patients. Out of three patients with galactorrhoea, only one had hyperprolactinemia. In patients with thyroid axis involvement, TSH values ranged from 0.04 to 1.2 mIU l−1. In patients with gonadotropin deficiency, FSH values ranged from 0.41 to 6.1 mIU ml−1 and LH values ranged from 0.129 to 5.1 mIU ml−1. Baseline MRI Imaging was available in all the patients while serial imaging was available in 22 of 24 patients. Serial imaging was not available in two patients, but both of them had undergone TSS and the diagnosis was proven on histopathology. Table 1 shows the imaging features in our cohort. Figure 1 shows serial MRI pituitary (at baseline and after steroid pulse therapy) of a 16 year female who had acute presentation with VI nerve palsy. Figure 2 shows the parasellar T2 dark sign. On application of clinical and radiological score described by Gutenberg et al. to our series, the median score was -8 while the range was −1 to −13.
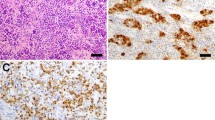
Typical MRI features in AH. 16 year female presented with headache and right VI nerve palsy. At baseline the contrast enhanced coronal a and sagital b MRI showed homogenously enhancing sellar mass with suprasellar extension and thick stalk (arrow). Patient was treated with steroid pulse therapy and after 1 month, the contrast enhanced coronal c and saggital d MRI showed significant reduction in sellar mass and suprasellar extension
Deficient hormone replacement and symptomatic treatment for headache was offered to all. Five (20.8 %) patients underwent TSS (group 1). Fifteen (62.5 %) patients were managed conservatively with watchful observation (group 2) while steroid pulse therapy was given in four (16.7 %) patients (group 3). In group 1, one had atypical radiological features with VI nerve palsy, while the other had evidence of pituitary apoplexy. The rest three patients had typical radiological features of AH and were referred to us postoperatively. Infiltration with lymphocytes and plasma cells with occasional lymphoid follicles were demonstrated in the histopathology of all operated patients. In group 3, the indication of steroid pulse therapy was cranial nerve palsies in two patients and proximity of the sellar mass to optic chiasm in one. One patient received steroid pulses because of associated optic neuritis. No adverse effects were observed in patients who were given steroids.
In group 1, the symptoms of expanding sellar mass subsided immediately post surgery, while they subsided within a week of steroid pulse therapy (group 3), and with a median duration of 1 month in group 2. The commonest axis recovered was cortisol in 10/18(55.5 %) followed by gonadotropin 5/12(41.67 %). The thyroid axis recovered in 1/14 (7.14 %) and DI remained persitent. On follow up, 70.8 % patients required long term hormonal replacement with at least one anterior pituitary hormonal substitution while 29.2 % had complete recovery of anterior pituitary functions. Table 2 shows the hormone axis recovery at median duration of 8 months after presentation in the three groups.
On serial imaging, in 19 patients who were not operated (group 2 + group 3), pituitary mass regressed in all in median duration of 1.5 years (range: 1 month to 3 years). Persistent stalk thickening was seen in 13 (68.4 %). Two (10.5 %) patients had near normal MRI findings and four (21 %) had empty sella with thinning of stalk.
Discussion
Hypophysitis can be classified as primary or secondary depending on the aetiology. Secondary hypophysitis can be due to local lesions (granulomas, craniopharyngioma, Rathke’s cleft cysts, and pituitary adenomas) or systemic diseases (sarcoidosis, Wegener’s granulomatosis, Langerhans cell histiocytosis, tuberculosis). Histopathologically, hypophysitis can be lymphocytic (autoimmune), granulomatous, xanthomatous, necrotising, IgG4 plasmacytic and mixed. Based on the anatomic location of pituitary involvement it can be classified as adenohypophysitis, infundibuloneurohypophysitis, panhypophysitis [1, 8] In our cohort, five patients had histopathological proof of the diagnosis and four others had responded to steroids and thus pointing towards autoimmune aetiology. In remaining 15 cases, the secondary causes with local pathology are unlikely as MRI at baseline did not show any associated pathology and we have documented the regression of the mass on follow up MRI. None of these patients had any evidence of systemic pathology at baseline or even at median duration of follow up of 1.5 years and had regression of sellar mass without intervention. So, after excluding the other underlying aetiologies of hypophysitis, AH remains as the diagnosis of exclusion.
This study analysed 24 patients with AH presenting to our institute from 2006 to 2012. In the same period, our institute managed 100 new patients with Cushing’s disease. Considering the incidence of Cushing’s disease as 1 case/million/year [9], the incidence of AH can be extrapolated as 2.4 in ten million. This figure is very close to the reported incidence (one in nine million) of AH in literature. Considering the natural history of AH, which can recover spontaneously or lead to empty sella, a considerable number of cases will be remaining undiagnosed, so under reported.
Caturegli et al. [3] has described 492 patients of AH, published between 1962 and 2008. Table 3 compares our series with this data. The age of presentation and female:male ratio was similar, but the literature described the strong association with pregnancy was lacking in our cohort. The frequencies of symptoms at presentation and hormonal axis involvement were similar to that reported in the literature. In our study, dynamic stimulation tests were not done, so the axis involvement and recovery pattern in our cohort and the literature though similar, may not be comparable. However, as described by Yip et al. recently, 8 a.m. serum cortisol cut off of <128 nmol l−1 (4.63 μg dl−1) is sufficient for predicting a post-ACTH value <550 nmol l−1 (19.93 μg dl−1), and 8 a.m. serum cortisol levels of >243 nmol l−1 (8.8 μg dl−1) and >266 nmol/L (9.64 μg dl−1) predict peak post-ACTH values of >500 (18.12 μg dl−1) and >550 nmol l−1 (19.93 μg dl−1) respectively, obviating the need for dynamic testing. So, we deduce that the definition of involvement and recovery of cortisol axis with basal cortisol values may be appropriate [10]. Moreover, ACTH values were not measured but low cortisol value in presence of sellar mass (and in absence of hyperpigmentation and absence of clinical features of mineralocorticoid deficiency) points towards secondary adrenal insufficiency.
Cranial nerve palsy was present in 12.5 % patients in our series (III nerve palsy in one and VI nerve palsy in two). In the literature, III, IV or VI cranial nerve palsy due to expansion of sellar mass has been reported in 3.7 % patients [1]. One of our patients had optic neuritis. Optic neuritis associated with AH may be explained by the close anatomic relationship between the optic nerves and sella, with spread of local inflammation to adjacent structures. Association of optic neuritis with AH is seldom reported in the literature [11, 12].
Our center had earlier published a retrospective analysis of cases diagnosed from 1988 to 2006 where the imaging modality used was computerised tomography (CT scan) in most of the patients. With improved imaging techniques over time, the current study provides more insight in the imaging of AH [13]. Hypophysitis can be differentiated from pitutary adenoma (PA) on MRI. Hypophysitis is a symmetrical, intensely and homogenously enhancing mass, with thickened stalk, loss of PPHI and intact sellar floor. PA is asymmetrical, heterogeneously enhancing mass with possible parasellar extension, displaced stalk, preserved PPHI and breach of sellar floor. With the score described by Gutenberg et al. value of <1 favours the diagnosis of hypophysitis with sensitivity of 92 %, and specificity of 99 %. When applied to our series, the median score was -8 while the range was −1 to −13. So, all the patients were correctly identified as AH. The radiology provided a strong proof to rule out the differential of PA in our cohort.
Parasellar T2 dark sign was seen in 50 % of the patients. In our patient who had ‘figure of 8’ appearance of the sellar mass, resembling pituitary adenoma, this sign was the pointer towards diagnosis of AH and helped us manage this patient with steroid pulse therapy rather than subjecting her to TSS. Nakata et al. first described this T2 dark sign. They compared 20 AH and 22 pituitary adenoma cases, and the sensitivity and specificity of this sign were 0.35 and 1.00 respectively to differentiate between these two entities. The possible explanation for this sign is the inflammatory and fibrotic changes in parasellar areas and in cavernous sinuses. The parasellar T2 dark sign may not be seen at initial imaging but may appear on follow up. So the sensitivity varies depending on the interval between imaging and the disease onset [6]. There was evidence of pituitary apoplexy on MRI, in one of the patients and she was operated due to atypical radiology. The presence of apoplexy with AH is scarcely reported in the literature [14, 15]. In non-operated patients, persistent stalk thickening i.e. thick stalk even as the sellar mass regressed, was seen in 68.4 % patients at median duration of 1.5 years. So, we postulate that persistent stalk thickening even in the absence of sellar mass may point towards diagnosis of AH, retrospectively.
TSS has been the most common treatment modality for AH so far, and it provides providing histopathological diagnosis as well. Only 21 % of our patients were treated with surgery as against 64 % of the 372 cases described by Caturegli. (p = 0.0001) still outcomes were comparable. With better understanding of the natural history of the disease and improvement in imaging technique and characterisation of specific imaging features of AH, the diagnostic yield is much higher even in the absence of tissue diagnosis. Thus, surgery can be avoided in AH, both from diagnostic as well as from therapeutic point of view.
Kristof et al. [16] performed the first prospective trial of glucocorticoid use in nine patients with AH. Pulse methylprednisolone (120 mg/day for 2 weeks) improved pituitary function in 44 % patients. Lupi et al. [17] reviewed outcomes of medical management in AH. Pituitary biopsy was available in 22.7 % patients only. Improvement of anterior pituitary function was seen in 50 % of patients treated with steroid pulse therapy. Though these reviews have demonstrated the efficacy of steroid pulse therapy in reversing the anterior pituitary axes involvement, occurrence of spontaneous recovery could have been a confounder. Our cohort is unique to have group 2, which gives insight in the natural history of disease. In non-operated patients from our cohort, the patients managed by watchful monitoring (group 2) had dismal results compared to those receiving steroid pulse therapy (group3) in terms of reversal of hypopituitarism. But the statistical significance could not be achieved due to small numbers. Thus, the evidence from literature as well as our observation suggests that the rate of recovery of hypopituitarism is better with steroid therapy than that without it. Larger randomised control study with loner follow up would be required to analyse the efficacy of steroid pulse therapy.
Anti pituitary antibodies are known to be associated with AH. Antipituitary antibodies measured with immunoblotting technique had sensitivity and specificity of 64 and 86 % in predicting histologically proven AH [3]. They are known to be present in various other autoimmune conditions and in healthy subjects too. Anti pituitary antibody as well as other autoimmune markers were not measured in our cohort is a limitation of our study. Presence of other associated autoimmune disease is reported in the literature (around 18 %) [1], only associated autoimmune manifestation in our cohort was presence of optic neuritis in one patient.
Conclusion
AH can be diagnosed with characteristic radiology, even without tissue diagnosis. Non-operative management is the treatment of choice. Steroid pulse therapy potentially improves the pituitary axis recovery.
References
Caturegli P, Newschaffer C, Olivi Al et al (2005) Autoimmune Hypophysitis. Endocr Rev 26:599–614
Caturegli P, Iwama S (2013) From Japan with love: another Tessera in the hypophysitis mosaic. J Clin Endocrinol Metab 98:1865–1868
Caturegli P, Lupi I, Landek-Salgadoa M et al (2008) Pituitary autoimmunity: 30 years later. Autoimmun Rev 7:631–637
Rivera J (2006) Lymphocytic hypophysitis: disease spectrum and approach to diagnosis and therapy. Pituitary 9:35–45
Hattori Y, Tahara S, Ishii Y, Kitamura T et al (2013) A case of IgG4-related hypophysitis without pituitary insufficiency. J Clin Endocrinol Metab 98:1808–1811
Nakata Y, Sato N, Masumoto T, Mori et al (2010) Parasellar T2 dark sign on MR imaging in patients with lymphocytic hypophysitis. Am J Neuroradiol 31:1944–1950
Gutenberg A, Larsen J, Lupi I et al (2009) A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. Am J Neuroradiol 30:1766–1772
Leporati P, Melissa A, Salgado L et al (2011) IgG4-related hypophysitis: a new addition to the hypophysitis spectrum. J Clin Endocrinol Metab 96:1971–1980
Bertagna X, Guignat L, Groussin L, Bertherat J (2009) Cushing’s disease. Best Pract Res Clin Endocrinol Metab 23:607–623
Yip CE, Stewart SA, Imran F et al (2013) The role of morning basal serum cortisol in assessment of hypothalamic pituitary-adrenal axis. Clin Invest Med 36:E216
Abdullah AM, Ganesh A, l-Zuhaibi S et al (2009) Lymphocytic infundibulo-neurohypophysitis: an unusual cause of recurrent optic neuropathy in a child. J AAPOS 13:207–209
Zoeller G, Benveniste R, Farhadi F et al (2012) Lymphocytic hypophysitis in a patient presenting with sequential episodes of optic neuritis. Pituitary 15:101–105
Menon SK, Sarathi V, Bandgar TR et al (2009) Autoimmune hypophysitis: a single centre experience. Singapore Med J 50:1080–1084
Fujimaki T, Hotta S, Mochizuki et al (2005) Pituitary apoplexy as a consequence of lymphocytic adenohypophysitis in a pregnant woman: a case report. Neurol Res 27:399–402
Minakshi B, Alok S, Hillol KP (2005) Lymphocytic hypophysitis presenting as pituitary apoplexy in a male. Neurl India 53:363–364
Kristof R, Roost D, Klingmuller D et al (1999) Lymphocytic hypophysitis: non-invasive diagnosis and treatment by high dose methylprednisolone pulse therapy? J Neurol Neurosurg Psychiatry 67:398–402
Lupi II, Manetti L, Raffaelli V et al (2011) Diagnosis and treatment of autoimmune hypophysitis: a short review. J Endocrinol Invest 34:e245–e252
Acknowledgments
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of all the contributors, I will act and guarantor and will correspond with the journal from this point onward.
Rights and permissions
About this article
Cite this article
Khare, S., Jagtap, V.S., Budyal, S.R. et al. Primary (autoimmune) hypophysitis: a single centre experience. Pituitary 18, 16–22 (2015). https://doi.org/10.1007/s11102-013-0550-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-013-0550-9