Abstract
The weekly sustained-release recombinant human GH formulation LB03002, showed beneficial effects in GH-deficient (GHD) adults in a previous 26-week double-blind study. Prior studies of long-acting GH preparations in adults have only been conducted for 6 or 8 months, so the effects of longer-term use are unknown; this is important to address, as replacement is given for many years in GHD adults. This open-label, 26-week study extension evaluated longer-term safety and efficacy of LB03002 over 52 weeks in adults with GHD who had previously been randomized to GH, and provides additional safety and efficacy data over 26 weeks in the cohort who had previously been randomized to placebo. Of 147 adults with GHD who completed a preceding study, 136 patients continued in this open-label study to receive LB03002 over an additional 26 weeks. This represented a continuation of long-acting GH for 26 weeks in the cohort who took this medication in the prior study (LB03002 Throughout group), and describes the first use of long-acting GH in the cohort that was randomized to placebo in the prior study (Switched to LB03002 group). The LB03002 dose was adjusted according to serum insulin-like growth factor-I (IGF-I) levels. LB03002 treatment demonstrated mean significant decreases from baseline in fat mass (FM) for both 26 (Switched group, P = 0.001) and 52 weeks (Throughout group, P = 0.002) of 1.11 (1.95) kg and 1.06 (3.16) kg, respectively. Prolonged GH treatment was effective in sustaining the increase in lean body mass (LBM), serum IGF-I and IGFBP-3 levels achieved during the first 26 weeks. Long-term treatment with the sustained-release weekly GH preparation over both 26 and 52 weeks in adults with GHD demonstrated a sustained reduction of FM with a favorable safety profile. This study extends prior knowledge about long-acting GH because it reports the most prolonged treatment of adults with any long-acting GH preparation, thereby confirming the value and safety of such agents for long-term GH replacement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Growth Hormone (GH) formulations with different sustained-release mechanisms have been developed and tested in growing children [1, 2] and in adults [3, 4] with GH deficiency (GHD), although none has yet been approved for treatment of adult GHD. The longest reported duration of treatment with a long-acting GH preparation in adults has been only 6–8 months [3, 4]. A previous double-blind, placebo-controlled study with LB03002 over 26 weeks [5] demonstrated that adults with GHD can be effectively treated with GH replacement using a sustained-release formulation given once weekly. This open-label extension study was performed for an additional 26 weeks to obtain longer-term safety and efficacy data in those patients who voluntarily participated upon completion of double-blind study.
In this open-label study, the primary objective was to evaluate the long-term (1 year) safety of LB03002 in adults with GHD who were treated with this compound in the preceding double-blind study and then continued on LB03002 for an additional 26 weeks, providing information on a total of 1 year of treatment (the LB03002 “Throughout” group). In addition, the effect of LB03002 on pharmacodynamics (PD) parameters including IGF-I and IGFBP-3 and the various anthropometric parameters including FM, LBM, trunk fat, percentage trunk fat and percentage body fat between 6 and 12 months was investigated. Safety of LB03002 was assessed at 1 year from adverse events, injection site reactions, glucose homeostasis, and antibody development. Efficacy parameters, including FM, LBM, IGF-I, IGFBP-3 and IGF-I SDS, were also analyzed in patients who had been randomized to placebo during the preceding double-blind study, and were receiving LB03002 for 26 weeks for the first time in this extension study (the “Switched” to LB03002 group).
Patients and methods
Study design and patients
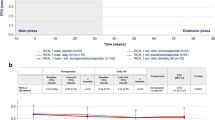
This was a 26-week open-label, multicenter study evaluating treatment with a sustained-release GH formulation in adult patients with confirmed GHD who had previously been enrolled in a 26-week placebo-controlled, double-blind study conducted in Europe and the US (Fig. 1) [5]. The study was carried out according to Good Clinical Practice guidelines and the Declaration of Helsinki, and with appropriate ethical approvals. A total of 147 adult GH-deficient patients had completed the 26 weeks of the preceding double-blind study. Of these, 136 adult patients signed written informed consent to continue participation in this open-label study to receive LB03002 for a further 26 weeks, including 43 who had received placebo during the preceding double-blind study. None of the 136 patients had developed an active malignancy or tumour growth or benign intracranial hypertension during the preceding 26 weeks study, which would have led to exclusion of such a patient in this extension phase. Eleven patients chose not to participate in this open-label study. The last visit of the double-blind study was considered as the Visit 0 for the open-label study. Patient visits were scheduled 4 ± 1 days after the drug administration.
Study drug administration and dose selection
The test product was supplied in powder form which, after reconstitution with medium chain triglyceride (MCT), produced a GH concentration of 10 mg/ml. The homogenous suspension was self administered subcutaneously by all patients using a 26-gauge needle. In this open-label study, all patients received the active medication (LB03002) for 26 weeks. To protect the blinding from the preceding study, all patients received transitional LB03002 doses between 1.0 and 3.0 mg per week for the first 3 weeks. This transient low-dose treatment for both groups was expected to result in IGF-I levels not significantly different between the two groups, preventing patient assignment to their previously blinded regimen in the preceding study from being revealed to the investigators, the patients or the study team. Thereafter, the dose of LB03002 was adjusted, if necessary, according to serum IGF-I levels measured during the scheduled visits. The dose of LB03002 was increased, maintained or decreased to achieve a target serum IGF-I concentration in a range between −0.5 and +1.5 standard deviation score (SDS) at 4 ± 1 days post-dosing, and with a minimum of +1 SDS increase from the baseline IGF-I SDS (prior to GH administration).
At each dose adjustment, the dose increment was 1.5 mg for female patients receiving oral estrogen or 1.0 mg for all other patients, and any dose decrement was 0.5 mg for all patients. The GH does was decreased if IGF-I SDS exceeded +2. The maximum dose per protocol was 7 mg/week, except for females taking oral estrogen who could potentially receive up to 10.5 mg/week. Individual study investigators adjusted the dose of LB03002 according to the IGF-I level at each regularly scheduled visit during the dose adjustment period. However, dose reductions or treatment interruptions could also be carried out at any time during the study, according to the clinical judgment of the investigator, based on side effects and/or abnormal laboratory findings including fasting glucose, insulin, and glycosylated hemoglobin (HbA1c) concentrations.
Replacement of other pituitary hormones
Throughout the study, temporary adjustment of glucocorticoid replacement therapy for adrenal insufficiency symptoms was allowed, as appropriate. Replacement therapy for other pituitary hormone insufficiencies was required to be adequate and stable throughout the study. For patients receiving estrogen therapy, the administration route was to remain the same throughout the study.
Efficacy assessments
For the group receiving the sustained-release GH for 52 weeks (“Throughout” group), baseline was defined as the Screening visit of the preceding double-blind study, and for the patients switched from placebo to LB03002 (“Switched” group), baseline was defined as the value at the Visit 0 of the open-label study, which was also the last visit of the double-blind study. At weeks 0 and 26 of this open-label study, fat mass (FM), lean body mass (LBM), percentage body fat, trunk fat, and percentage trunk fat were measured by dual-energy x-ray absorptiometry (DXA) at each investigational site, with quality control by means of phantom scans, and evaluated centrally (DXA Resource Group, Westborough, MA).
Serum concentrations of IGF-I and IGFBP-3 were determined at a central laboratory (Medizinische Klinik Innenstadt, Munich, Germany) using DPC Biermann Immulite chemiluminescence assays. All IGF-I and IGFBP-3 concentrations and SDS results were sent to the investigator immediately after completion of analysis to allow dose adjustments.
Safety assessments
Safety was evaluated from adverse events, glucose homeostasis, thyroid hormone status, and screening for antibodies against GH and Saccharomyces cerevisiae at Screening, inclusion visits and endpoint visits. Glucose homeostasis was assessed from concentrations of fasting glucose, fasting insulin, and HbA1c; fasting glucose and insulin were assessed at each scheduled visit 4 ± 1 days after GH administration. Thyroid function was assessed by measurement of free triiodothyronine (T3), free thyroxine (T4), and thyroid stimulating hormone (TSH) concentrations. Anti-hGH antibodies were quantified by a radio-precipitation assay, however neither blocking or neutralizing capacity was assessed. Because the GH protein used in the administered product, LB03002, was derived from S. cerevisiae, anti-yeast antibodies were determined by a solid-phase enzyme immunoassay system. Local tolerability to the study drug was assessed by both the investigators and the patients as injection site reactions.
Statistical analysis
In accordance with the open-label study design, no confirmatory treatment comparisons were planned. The focus was on assessing safety and efficacy over a continuous year of treatment within the group of patients randomized to LB03002 from the Screening of the previously-reported double-blind study. Separately, safety and efficacy were evaluated in an additional cohort of patients taking LB03002 for the first time, namely, the group of patients switched from placebo at the end of the double-blind study to GH replacement with LB03002. Continuous data were assessed by summary statistics, with values shown as mean ± standard deviation (SD), and categorical data summarized as counts and percentages. Only paired t tests for within-group changes were analyzed.
Results
A total of 136 patients were evaluated; 93 of them were patients who had been on LB03002 treatment Throughout (i.e. during the preceding double-blind study as well as the open-label phase, for a total of 52 weeks). The remaining 43 patients had been on placebo in the initial study, and were switched to LB03002 treatment during the optional open-label phase, for a total of 26 weeks of GH replacement. Of the 136 total patients, 129 completed the open-label study, 89 in the Throughout group and 40 in the Switched group. As shown in Table 1, there were no evident differences between the two treatment groups in distribution of baseline demographic characteristics as well as clinical diagnoses. Overall, there were more patients with AO GHD (72.1 %) than CO GHD (27.9 %), and 56.6 % of the patients were male.
The average ± SD weekly dose of LB03002 over the 26 weeks of this open-label study was 3.45 ± 1.26 mg (range 1.0–6.9 mg) in the Throughout group, and 3.38 ± 1.16 mg (range 1.3–5.9 mg) in the Switched group.
Treatment with LB03002 for both 52 and 26 weeks was effective in producing notable increases in serum IGF-I levels and in IGFBP-3 levels. These increases were indicative of a change from Baseline within each treatment group, overall and for all subgroups (P < 0.05). Comparison of the placebo patients in the double-blind study against when they were switched to LB03002 in the open-label study, showed changes in IGF-I, IGFBP-3, and IGF-I SDS between the two study phases with P < 0.001. Patients in the Switched group had a mean increase in IGF-I in the placebo phase of 0.29 ng/mL (26.50) compared to a mean increase of 101.60 ng/mL (72.35) in this open-label study. Switched patients had a mean decrease of 1.35 (5.65) in IGF-I SDS during the placebo phase, compared to a mean increase of 4.62 (5.14) once they were stable on long-acting GH replacement. (Fig. 2)
Changes in DXA body composition are presented in Table 2. Baseline, GH-untreated, mean FM values for the Throughout (Screening of double-blind study) and the Switched groups (Visit 0 of open-label study) were comparable: 27.8 ± 8.8 kg and 27.4 ± 10.9 kg. While no significant change in FM had been seen in the placebo group during the double-blind study (0.37 ± 2.25 kg), when Switched to LB03002 these patients experienced a change in FM of −1.11 ± 1.95 kg (P = 0.005) over the 26-week open-label period, comparable to the decrease from baseline of 1.06 ± 3.15 kg (P = 0.002) seen in the Throughout group during the total period of 52 weeks of administration. There was no further FM decrease in the Throughout group during their second 26 week of GH therapy (Table 2). The changes in trunk fat during the same periods of LB03002 administration were −0.99 ± 1.80 kg (P < 0.001) in the Throughout group and −0.91 ± 1.20 kg (P < 0.001) in the Switched group.
Baseline mean LBM values prior to GH replacement in the Throughout group were higher than those in the Switched group (49.32 ± 13.50 vs. 47.16 ± 11.98 kg; P < 0.001). While no significant change in LBM had occurred during the double-blind study in the placebo group (0.87 ± 2.26 kg), after the Switch to LB03002, an increase of 1.64 ± 1.88 kg (P < 0.001) was seen in these patients. For patients in the Throughout group, the total gain in LBM after 52 weeks was 2.22 ± 2.90 kg (P < 0.001).
Safety
Adverse events
Of the 136 patients who entered the study extension, 129 (94.8 %) completed 26 weeks of LB03002 treatment. Discontinuation was due to adverse events for one patient in the Throughout group (asthenia) and two patients in the Switched group (peripheral edema and dysgeusia). Four patients discontinued due to withdrawal of informed consent. No patient died and there were no reports of an adverse event related to tumor or cancer during this open-label study. Overall, 62 patients (66.0 %) in the Throughout group experienced 225 events and 27 patients (64.3 %) in the Switched group experienced 135 events. The most frequently reported treatment-emergent adverse events in the Throughout and Switched groups were: nasopharyngitis 10.6 and 14.3 %, respectively, arthralgia 7.4 and 7.1 %, peripheral edema 5.3 and 16.7 %, and headache 3.2 and 21.4 %.
Injection site reactions
Injection site reactions were reported in 19.1 % of the Throughout group and in 28.6 % of the Switched group. Local injection site reactions were neither treatment nor dose limiting and were similar between the Throughout and Switched groups in terms of frequency and severity, primarily classified as mild to moderate in severity. The majority of patients subjectively assessed discomfort at injection site as none (70.2 % in the Throughout group and 66.7 % in the Switched group). Overall, injection of study medication was relatively well tolerated by the patients as assessed by the investigators and patients themselves.
Glucose homeostasis
There were no statistically significant changes from baseline to endpoint in mean fasting glucose, fasting insulin or HbA1c concentrations in either the Throughout group or the Switched group. Diabetes mellitus (defined as fasting glucose > 126 mg/dL) was reported for 3 patients (3.2 %) in the Throughout group and 2 patients (4.8 %) in the Switched group based on the lab result that met the definition of diabetes as stated above. Of the 3 patients in the Throughout group with treatment-emergent diabetes mellitus, 2 had onset during the double-blind study and 1 had onset during this open-label study [5, 6]. Impaired fasting glucose (defined as fasting glucose >100 mg/dl [>5.6 mmol/l]) occurred in 32 patients (34.0 %) in the Throughout and 10 (23.8 %) in the Switched group, although nearly 40 % of these patients only had a single elevated value and did not have documentation of persistent impaired fasting glucose level. However, in patients with impaired fasting glucose level, disturbance of glucose homeostasis was present prior to LB03002 treatment, and 8 (25.8 %) patients in the Switched group experienced improvement of fasting glucose level while receiving LB03002 during the open-label study. Any abnormalities in glucose homeostasis were easily manageable and did not lead to the need for any dose modification.
Antibody assessments
In the Throughout group, 3 out of 4 patients who tested positive for antibodies against hGH during the double-blind phase were still positive at the end of this open-label study. No patients in the Switched group developed antibodies against hGH. In the Throughout group, 2 patients were positive for antibodies to S. cerevisiae at both baseline and end of study. In the Switched group, no patients were positive for S. cerevisiae antibodies either at baseline or at the end of the study. No differences in efficacy and safety were noted for patients with positive antibody tests to hGH or to S. cerevisiae when compared with the remainder of the cohort.
Discussion
We examined the long-term use of a new sustained-release GH formulation, LB03002, demonstrating a favorable safety profile and sustained body composition changes over 52 weeks of treatment. In the initial double-blind, placebo-controlled study, we had previously shown that with LB03002 administration once per week, IGF-I concentrations normalized with the dosing algorithm used [5] and that 26 weeks of treatment was effective and safe. This report extends prior knowledge about long-acting GH because it represents the most prolonged treatment of adults with any long-acting GH preparation, thereby confirming the value and safety of such agents for GH replacement. In addition, efficacy and safety were established in an additional cohort of patients treated for 26 weeks (the Switched from Placebo group), thereby expanding the number of adults who have experienced a favorable outcome with a long-acting GH preparation.
The beneficial changes in body composition, including total FM, percentage trunk fat and LBM seen with LB03002 in the Throughout group during the double-blind study were maintained over the 26-week additional period and remained statistically significant at the 52-week endpoint. The Switched group, who received LB03002 for the first time in this extension study, also experienced a significant decrease in fat mass, further confirming the efficacy of this compound over 26 weeks in another cohort of adult patients.
In this open-label uncontrolled study representing the longest duration of treatment of any long-acting GH compound, the safety of 1 year of sustained-release rhGH was demonstrated. There were no unexpected safety concerns with 52 weeks of LB03002 administration, and there were no deaths, tumors or malignancies reported during the study. In the Throughout group, the overall incidence of AEs was similar between the open-label study and double-blind study. The number of patients who discontinued due to an AE (one patient [1.1 %] in the Throughout group and two patients [4.8 %] in the Switched group) was also low. Potential safety concerns of GH treatment are related to fluid retention, glucose metabolism and interaction with other hormones. The incidence of AEs related to these did not increase with longer-term use between 26 and 52 weeks.
Most injection site reactions were mild or moderate in severity. A higher percentage of patients experienced injection site reactions in the Switched group than the Throughout group. More patients in the Throughout group experienced injection site reactions during the double-blind study compared to the open-label extension study. These two findings suggest that patients develop tolerance to injection site reactions with continued administration of LB03002.
The percentage of patients with at least one treatment-emergent adverse event was similar in the Throughout group (66.0 %) and in the Switched group (64.3 %), and the rate of TEAEs in the Switched group was similar to what the Throughout group had experienced in their first 26 weeks treatment with LB03002 [5]. Thus, long-term treatment with LB03002 for 52 weeks showed a good safety profile and was well tolerated in adult patients with GHD, consistent with daily GH studies [7, 8].
The effect of sustained-release GH administration on glucose control was carefully monitored. The number of patients with glucose homeostasis dysfunction was similar to that observed in the double-blind study. Overall, the rate of diabetes mellitus reported in the Throughout and the Switched groups were similar to rates reported in two other daily GH treatment studies in adults [4, 9]. Interestingly, several patients had laboratory results indicating improvement or resolution of their previous insulin resistance with continued or new exposure to GH. The prolonged glycemic safety profile after LB03002 treatment did not indicate any additional risk, and was in line with the daily injection study using the same GH molecule [10].
Anti-GH antibodies persisted in 3 patients in the Throughout group, and were not detected in any Switched patients. The rate of 3 % in the first group was comparable to that seen in the double-blind study [5] and also consistent with other daily injectable somatropin preparations [10, 11]. The GH protein of LB03002 is produced in yeast, and the genetic modification of the yeast cells and the purification of the GH molecule may produce a spectrum of proteins different from that of naturally occurring S. cerevisiae antigens. Positive antibody titers were observed in patients at both baseline and during treatment, suggesting that these findings were not specific for the LB03002 derived proteins [12, 13].
In conclusion, GH replacement in adult patients with GHD can be successfully carried out using a sustained-release formulation given once-weekly over a prolonged period of 52 weeks. The once-weekly formulation, LB03002, showed significant and sustained effects at a relatively low dose over 52-week treatment when compared to 26-week treatment in the double-blind study [5], and demonstrated a reassuring safety profile. In the Switched group, GH treatment for 26 weeks demonstrated similar results to the first 26 weeks of the double-blind study in the Throughout group patients, confirming the benefit of long-acting GH in an additional cohort of adult patients. This study extends prior knowledge about long-acting GH by reporting the most prolonged treatment of adults with any long-acting GH preparation, thereby confirming the value and safety of such compounds.
References
Rosenfeld RG, Bakker B (2008) Compliance and persistence in pediatric and adult patients receiving growth hormone therapy. Endocr Pract 14:143–154
Reiter EO, Attie KM, Moshang T Jr, Silverman BL, Kemp SE, Neuwirth RB, Ford KM, Saenger P, Genentech Inc.-Alkermes Inc. Collaborative Study Group (2001) A multicenter study of the efficacy and safety of sustained release GH in the treatment of naive pediatric patients with GH deficiency. J Clin Endocrinol Metab 86:4700–4706
Cook DM, Biller BM, Vance ML, Hoffman AR, Phillips LS, Ford KM, Benziger DP, Illeperuma A, Blethen SL, Attie KM, Dao LN, Reimann JD, Fielder PJ (2002) The pharmacokinetic and pharmacodynamic characteristics of a long-acting growth hormone (GH) preparation (Nutropin depot) in GH deficient adults. J Clin Endocrinol Metab 87:4508–4514
Hoffman AR, Biller BMK, Cook D, Baptista J, Silverman BL, Dao L, Attie KM, Fielder P, Maneatis T, Lippe B, Genentech Adult Growth Hormone Deficiency Study Group (2005) Efficacy of a long-acting growth hormone (GH) preparation in patients with adult GH deficiency. J Clin Endocrinol Metab 90:6431–6440
Biller BMK, Ji H-J, Ahn H, Savoy C, Siepl EC, Popovic V, Coculescu M, Roemmler J, Gavrila C, Cook DM, Strasburger CJ (2011) Effects of once-weekly sustained-release growth hormone: double-blind, placebo-controlled study in adult growth hormone deficiency. J Clin Endocrinol Metab 96(6):1718–1726. doi:10.1210/jc.2010-2819
American Diabetes Association (2010) Standards of medical care in diabetes-2010. Diabetes Care 33(Suppl 1):S11–S61
Spielhagen C, Schwahn C, Moller K, Friedrich N, Kohlmann T, Moock J, Koltowska-Haggstrom M, Nauck M, Buchfelder M, Wallaschofski H (2011) The benefit of long-term growth hormone (GH) replacement therapy in hypopituitary adults with GH deficiency: results of the German KIMS database. Growth Horm IGF Res 21:1–10
Svensson J, Bengtsson BA (2009) Safety aspects of GH replacement. Eur J Endocrinol 161(Suppl 1):S65–S74
Hoffman AR, Strasburger CJ, Zagar A, Blum WF, Kehely A, Hartman ML, T002 Study Group (2004) Efficacy and tolerability of an individualized dosing regimen for adult growth hormone replacement therapy in comparison with fixed body weight-based dosing. J Clin Endocrinol Metab 89:3224–3233
Peterkova V, Arslanoglu I, Bolshova-Zukovskaya E, Romer T, Zdravkovic D, Kratzsch J, Ji HJ, Savoy C, Saenger P (2007) A randomized, double-blind study to assess the efficacy and safety of Valtropin, a biosimilar growth hormone, in children with growth hormone deficiency. Horm Res 68:288–293
Pirazolli P, Cacciari E, Mandini M, Cicognani A, Zucchini S, Sganga T, Capelli M (1995) Follow-up of antibodies to growth hormone in 210 growth hormone-deficient children treated with different commercial preparations. Acta Pediatr 84:1233–1236
Riente L, Chimenti D, Pratesi F, Sedie AD, Tommasi S, Tommasi C, Bombardieri S, Migliorini P (2004) Antibodies to tissue transglutaminase and Saccharomyces cerevisiae in ankylosing spondylitis and psoriatic arthritis. J Rheumatol 31:920–924
Walker LJ, Aldhous MC, Drummond HE, Smith BR, Nimmo ER, Arnott ID, Satsangi J (2004) Anti-Saccharomyces cerevisiae antibodies (ASCA) in Crohn’s disease are associated with disease severity but not NOD2/CARD15 mutations. Clin Exp Immunol 135:490–496
Acknowledgments
Jointly by LG Life Sciences, Ltd., Korea, and Biopartners GmbH, Switzerland. We thank the late Mircea Popa, Medical Center Sana, Bucharest, Romania, who significantly contributed to the study. His associate Catalin Gavrila continued his work in this study and co-authors this manuscript. We acknowledge the significant contributions by Jin Hwa Lee, Songmi Lee, Leah Suh, Karin Sulzer, and John Kim.
In addition to the authors, this clinical trial was conducted by the following investigators: Anton Luger, M.D. (University of Vienna, Vienna, Austria); Josef Marek, M.D. (Vseobecna Fakultni Nemocnice, Praha, Czech Republic); Jan Cap, M.D. (Fakultni Nemocnice Hradec Kralove, Hradec Kralove, Czech Republic); Zdnek Frysak, M.D. (Fakultni Nemocnice Olomouc, Olomouc, Czech Republic); Philippe Chanson, M.D. (Centre Hospitalier Universitaire de Bicêtre, Paris, France); Francoise Borson-Chazot, M.D. (Hôpital Neurocardiologique Fédération d’Endocrinologie, Lyon, France); Georges Weryha, M.D. (Centre Hospitalier Universitaire de Nancy, Nancy, France); Michael Faust, M.D. (Klinikum der Universität zu Köln, Cologne, Germany); Roland Pfäffle, M.D. (Universitätsklinikum Leipzig, Leipzig, Germany); Jochen Schopohl, M.D. (Universitätsklinikum München, München, Germany); Harald Lahner, M.D. (Essen, Germany); Slawomir Mucha, M.D. (Independent Public Clinical Hospital, Sterlinga, Poland); Eusebie Zbranca, M.D. (Clinica de Endocrinologie, Iasi, Romania); Ioana Zosin, M.D. (Spitalul Clinic Judetean de Urgenta, Timisoara, Romania); Jan Podoba, M.D. (Interna Klinika FNsP, Bratislava, Slovakia); Felipe Casanueva, M.D. (Hospital Médico-Quirúrgico de Conxo, Santiago, Spain); Susan Webb, M.D. (Hospital de la Santa Creu i Sant Pau, Barcelona, Spain); Manel Puig, M.D. (Hospital Clinic I Provincial, Barcelona, Spain); Gudmundur Johannsson, M.D. (Universitetssjukhuset Göteborg, Göteborg, Sweden); Charlotte Höybye, M.D. (Karolinska Universitetssjukhuset Solna, Stockholm, Sweden); Richard Ross, M.D. (Royal Hallamshire Hospital, Sheffield, UK); Laurence Katznelson, M.D. (Stanford University Medical Center, Stanford, CA); David Kleinberg, M.D. (New York University School of Medicine, New York, NY) and Amir Hamrahian, M.D. (Cleveleand, OH).
Conflict of interest
H.J.J. and H.A. are employees of LG Life Sciences, Ltd.; C.S. and E.C.S. are employees of Biopartners, GmbH.; B.M.K.B. and C.J.S. received consulting fees from LG Life Sciences, Ltd., Korea, and Biopartners, GmbH, Switzerland.; V.P., M.C., J.R., C.G., and D.M.C. have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical trial identifier: NCT00596037.
Rights and permissions
About this article
Cite this article
Biller, B.M.K., Ji, HJ., Ahn, H. et al. 12-Month effects of once-weekly sustained-release growth hormone treatment in adults with GH deficiency. Pituitary 16, 311–318 (2013). https://doi.org/10.1007/s11102-012-0422-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-012-0422-8