Abstract
Traumatic brain injury (TBI) is a very common occurrence in childhood, and can lead to devastating long term consequences. Recent research has focused on the potential endocrine consequences of TBI in adults. The research in children is less robust. This paper reviews current literature regarding TBI and possible hypothalamic and pituitary deficiencies in childhood. Acute endocrine changes are commonly found after TBI in pediatric patients, which can include changes in hypothalamic–pituitary–adrenal axis and antidiuretic hormone production and release. In the long term, both temporary and permanent alterations in pituitary function have been found. About 30% of children have hypopituitarism up to 5 years after injury. Growth hormone deficiency and disturbances in puberty are the most common, but children can also experience ACTH deficiency, diabetes insipidus, central hypothyroidism, and elevated prolactin. Every hormonal axis can be affected after TBI in children, although growth hormone deficiency and alterations in puberty are the most common. Because transient and permanent hypopituitarism is common after TBI, survivors should be screened serially for possible endocrine disturbances. These children should undergo routine surveillance at least 1 year after injury to ensure early detection of deficiencies in hormonal production in order to permit normal growth and development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the United States, pediatric traumatic brain injury (TBI) places a large burden on our health care system [1]. Average annual incidence of TBI rate is approximately 180–200 per 100,000 children [1]. In 2000, there were 70 hospitalizations per 100,000 children under age 18 years in the United States for TBI. The age group most affected is 15–17 years, followed by ages 0–4 years, with males affected more than females [2]. Poor developmental and functional outcomes persisted in 35% of affected children at 2 years post-injury [3]. Prospective evaluation identified that 40% of children still had an impaired quality of life (QOL) at 1 year after moderate to severe head injury [4]. TBI in children results in long-term health consequences, including altered growth and development [5]. Recently, there has been an increase in the number of publications about endocrine function after TBI in adults, leading to awareness that pituitary dysfunction is common after TBI [6–13]. In contrast, there is very little literature analyzing endocrine function after TBI in children.
Acute endocrine changes after traumatic brain injury, endocrine response to critical illness/injury
Significant injury to the hypothalamic–pituitary axis during head injury may complicate medical management in the period immediately after injury. In the first few days after injury, cortisol levels usually rise in response to the stress of injury and hospitalization. Admission cortisol levels in a person with an intact hypothalamic–pituitary axis obtained within a few hours of injury tend to correlate with injury severity scores and neurologic outcome, with lower cortisol levels in milder injury and the highest cortisol levels in the most severely injured [14, 15]. Thus, a low cortisol level obtained acutely in a severely injured patient may suggest secondary adrenal insufficiency (ACTH deficiency). In 80 adults followed prospectively in the first 9 days after TBI, there was a 53% incidence of adrenal insufficiency based on low cortisol levels, significantly associated with injury severity [16]. Children may differ in their response in the acute phase after TBI, but reports are limited. In 37 children studied on days 1, 3, and 7 after severe TBI, cortisol was elevated on day 1 then normal by day 3; however 46% had a low cortisol [17].
In adults evaluated acutely after injury, 80% had gonadotropin deficiency, 18% GH deficiency, 16% ACTH deficiency, 40% diabetes insipidus or SIADH, compared to long term deficiencies in 25% [18]. In contrast, another study found no cases of low cortisol levels at baseline in children after TBI [19]. Patients with moderate to severe head injury should have their adrenal status evaluated acutely after injury (serum cortisol within the first 12–24 h). Research in the ICU setting suggests that a random cortisol level of more than 25 μg/dl during the stressed state is necessary to prove adrenal sufficiency [20]. If children do not meet these criteria, it is important to treat short-term with stress doses of hydrocortisone or other steroid having mineralocorticoid and glucocorticoid effect. Steroids should be tapered quickly as the clinical picture improves. These children will require reassessment of their adrenal axis with stimulation testing approximately 1 month after discontinuing steroids.
Diabetes insipidus (DI) is uncommon, but when present nearly always occurs early in the acute phase after TBI. DI can present within hours to days after the injury. However, onset of DI may be delayed as long as 30 days after injury [20]. In a series of 19 children with brain-damage (12 with TBI), all with DI, only three patients survived, leading to the conclusion that DI may be a poor prognostic indicator [21]. Regardless, permanent DI is rarely reported after TBI in children.
Endocrine studies in adults during the longer term after TBI
Overall, abnormalities in pituitary function occur in 23–69% of adults studied, 12 months or more after TBI [22]. The most common endocrinopathies in adults are growth hormone deficiency (GHD) and hypogonadism. However, central hypothyroidism (TSHD), adrenocorticotropin hormone (ACTH) deficiency (ACTHD), diabetes insipidus (DI), as well as prolactin elevation have also been reported. These deficiencies can occur either acutely after injury or develop slowly over time. The deficiencies can be transient or permanent. Most studies, but not all, report that the occurrence of pituitary deficiency is not correlated with severity of injury. Prevalence of different pituitary hormone deficiencies depends on the patients selected for study, definitions of deficiency, and choice of testing modality [23].
In young adults, Aimaretti et al. [24] studied 23 patients, ages 16–25 years, at 3 and 12 months after TBI. The incidence of pituitary abnormalities was 35% at 3 months and 30% at 12 months. Some abnormalities resolved by 12 months; however some patients had new pituitary deficiencies at 12 months. The most common pituitary abnormality was GHD, followed by hypogonadism.
Endocrine studies in children during the longer term after TBI
By comparison with reports in adults, little is known about endocrine function after TBI in children. Theoretically, pediatric patients may have an improved prognosis for neurologic recovery compared to adults with the same Glasgow Coma Scale (GCS) scores [25]. Many case reports after TBI in children have documented pituitary dysfunction, including precocious puberty. However, few studies have systematically evaluated the prevalence of endocrine dysfunction in children after TBI [19, 24, 26, 27]. Among retrospective studies [19, 24, 26], there is a 16–61% prevalence of hypopituitarism at 1–5 years after injury. A number of reviews and commentaries have discussed the need for prospective studies of hypothalamic-pituitary function after TBI in children [23, 28, 29].
Only two prospective studies in the pediatric age group have been published regarding endocrine abnormalities after TBI. Einaudi et al. [19] prospectively studied 30 children, average age of 9 years, at 0, 6, and 12 months after injury. At baseline, the incidence of endocrine dysfunction was 23%. At 6 months, the incidence was 4%, with one patient having ACTH deficiency. At 12 months, the incidence was 10% (n = 2). One patient had a new diagnosis of GHD, and the patient with ACTH deficiency was re-confirmed. Combined with the retrospective data from the same study, the incidence of some degree of hypopituitarism was 10.4% at 6 months after injury.
Kaulfers et al. [30] prospectively evaluated 31 children and adolescents for endocrine function after TBI. The incidence of any endocrinopathy in children who had moderate to severe head injury was 15% at 1 month after injury, 75% at 6 months, and 29% at 12 months after TBI. Interestingly, many of the endocrine abnormalities found in the first few months after injury resolved by 1 year. Abnormal menstruation was common in the first 6 months after injury in 22% of adolescent females, but all cases resolved by 1 year. Three children had water imbalance, but all were transient and resolved by 6 months. Eight children (33%) had elevated prolactin, but all had resolved by 12 months. One case of secondary adrenal insufficiency at 6 months had resolved by 12 months. Of the 13 children with thyroid abnormalities, all but two resolved by 12 months. Of 13% with GHD at 6 months, all but one resolved by 12 months. Thus, children need to have continued close endocrine surveillance until at least 1 year after TBI. At 12 months, abnormal pubertal development was most common. Other long lasting endocrine sequelae were GHD and central hypothyroidism. No risk factors were identified that could indicate which children would have endocrine abnormalities.
Thus the two studies with prospective data in the pediatric age range have shown an incidence of 30.3% [24] and 29% [30] pituitary deficiency at 1 year. These numbers are comparable to those reported for adults.
Recent meeting abstracts included three studies in the pediatric population after TBI showing a similar pattern of endocrine results. Bolado et al. (Spain) did cross-sectional study of 36 children after TBI. Of them, only 19% had severe injury (GCS < 9), 25% had moderate injury (GCS 9 to 13), while 55% had mild injury (concussion, GCS > 13). No abnormal endocrine findings were identified on simple screening, perhaps because so few had severe injury [31]. Aleksijevic et al. (Czech Republic) prospectively studied 58 children after TBI (23 with GCS < 8). During the first year after TBI, overall 15.5% had hormone deficiencies. Two had combined pituitary hormone deficiency, one had diabetes insipidus, three had GHD, one more had GHD with central hypothyroidism, one had precocious puberty, and two had hypogonadotropic hypogonadism [32]. Hewitt et al. (Australia) prospectively studied endocrine function during the first year after TBI in 49 children. GCS was more severe. Nearly half had deficiencies at 6 months and 10% had persistent deficiencies at 1 year [33]. Thus, endocrinopathies evolve over time after TBI. Temporary intervention during the first year after TBI may be beneficial with reevaluation at 1 year after injury.
Changes in endocrine function according to specific deficiency
In long-term follow-up of children after TBI, issues of anterior pituitary and/or hypothalamic deficiency gradually become important, especially with regard to growth and puberty. In multiple case reports of children after TBI, the months and years after head injury reveal poor growth, explicit GH deficiency, precocious puberty, or failure to enter or progress through puberty. Likewise, some adults experience chronic fatigue, loss of libido or amenorrhea, or overt gonadotropin deficiency [34]. Onset of these symptoms may be insidious and confused with the post-concussive syndrome. Pituitary dysfunction may go unrecognized and untreated in children after TBI, despite the integral nature of the pituitary’s function in growth and development [29]. It is crucial that medical providers recognize the relevance that a history of TBI may lead to pituitary dysfunction. Physicians must be diligent about regular height measurements and surveillance of pubertal development. If not, years may pass before a correct diagnosis is made and treatment started [33]. Without a high index of suspicion, some patients may never have their endocrine deficiencies identified.
Inconsistent methods of defining hypopituitarism contribute to the technical challenges in diagnosing children after TBI. For instance, some of the studies used baseline or basal hormonal testing, while others also used dynamic testing methods (stimulation tests). Different laboratory assays may also contribute to differences in outcomes for the diagnosis of hypopituitarism, for example for growth hormone [immunoradiometric assays (IRMA) vs. radioimmunoassays (RIA) versus enzyme-linked immunoassays (ELISA)] [35]. In addition, many drugs used in the acute or chronic stages of injury (i.e. anti-seizure medication, antidepressants, and antipsychotics) may interfere with neuroendocrine function and give artifactual results.
GH deficiency
Subtle GH deficiency (GHD) can be difficult to identify. Screening tests such as IGF-I and IGFBP3 can be helpful in excluding deficiency if the patient‘s results are above average for age. However, children with GHD can have IGF-I results either below normal limits or in the lower half of the normal range. GH stimulation tests identify children and adults who have clear-cut GHD, but may miss persons with more subtle disorders [36]. Overnight (12 h) spontaneous GH secretion has been found to be lower than normal in some children after cranial irradiation (another example of hypothalamic injury), and can indicate a subtle GH defect [37]. A 6 h sampling of GH levels, from 2,200 to 0400 h (normative results [38]), can accurately define a child’s ability to release GH, and is less invasive than the whole 12 h sampling period.
In adults and children, GHD is one of the most common endocrine abnormalities after TBI [22, 39, 42]. In adult patients evaluated at 1 year or more after TBI, the incidence of GHD is 2–33%. The wide range of results can be explained by differences in the type of testing used, different stimulating agents, and different cut-off criteria. Among retrospective studies in children after TBI, there is also a wide range of incidence of GHD at one or more years after TBI. Each study used a different method for GH testing. Among the prospective studies in children, Einaudi [19] reported one patient with GHD at 12 months (3%), Norwood [43] found that 16% of the children recruited from the pediatric TBI clinic had GHD, diagnosed after overnight sampling and an arginine/glucagon test. Nineteen percent of the children exhibited insufficient GH secretion in one or the other testing modality. Most studies used a single stimulation test or overnight hourly sampling to determine GHD, neither of which fulfills clinical standards for two stimulation tests revealing GHD. Auxology, but not growth velocity, was discussed in most articles. Unpublished data from Kaulfers reveals that 10 of 21 children were still growing during the study. In the first 6 months after the study, five of the ten children did not grow, while the average growth was 2 cm for the remaining five children (0.7–2.8 cm) in 6 months. In the following 6 months, the children grew an average of 3.7 cm (2.2–5.5 cm), and none of these children had low growth or thyroid hormone production. The children growing the fastest were having rapid puberty.
Children with low GH secretion had more rapid weight gain, had lower levels of free thyroxine, lower FSH levels, and males had lower testosterone levels. Kaulfers [30] found that 13% of children had a GH secretion defect at 6 months (using 6-h, every 20 min sampling at night). None of these had isolated deficiencies, and all patients had normal IGF-1. Consequently, at 12 months after TBI, only one child (5%) had GHD by low response to arginine clonidine stimulation testing. Regardless of method used, these studies show that GHD remains an important problem that requires clinical follow-up. In addition, these results suggest that GHD can be transient, or may persist in children after TBI. Children may need to be followed for longer than 12 months after TBI, as 1 year may be too early to see a decline in height velocity in children who are not yet at adult stature. It is important to correlate growth velocity to biochemical results.
Gonadotropin deficiency
Gonadotropin deficiency (GnRH-D) is one of the most common endocrinopathies after TBI. All of the prospective studies in adults show a higher prevalence acutely after injury than in the long-term, suggesting that hypogonadism may be a temporary adaptive response to injury [44], but may alternatively be permanent. Among the retrospective pediatric studies, Poomthavorn et al. [27] found that 4% of children had hypogonadism within the first year of injury, either transient or permanent. No new cases of hypogonadism were found more than 8 months after injury. Einaudi [19] found a 9% incidence of hypogonadism at one to 4 years after injury in children.
Among the prospective pediatric studies, Einaudi [19] did not find any cases of hypogonadism at 1 year after injury. Kaulfers [30] also showed that hypogonadism is usually transient. One patient clinically presented with hypogonadism within 1 month of injury, and by 3 months he had recovered. Female patients with abnormal menstruation had recovered by 1 year after injury. One new case of GnRH-D was evident at 1 year, highlighting the need for these children to be closely monitored for at least 1 year after injury. It is impossible to diagnose a prepubertal child with hypogonadism, therefore follow-up for longer than 1 year may be necessary, as many children may not be old enough yet to be identified with delayed puberty.
Precocious puberty
Precocious puberty (PP) after TBI, as opposed to hypogonadism, is a phenomenon that is unique to children. PP may go unrecognized and untreated in children after TBI. There are several case reports of PP in children after TBI. Among the retrospective pediatric studies, Poomthavorn et al. [27] identified one child (2%) with PP 4 years after TBI. Einaudi et al. [19] found one child (5%) with PP at 5 years after injury. Prospectively, Kaulfers [30] found a high incidence of rapid and/or precocious puberty in children after TBI. Among children younger than 10 years, 43% had signs of PP by 6 months. Overall, four children (16%) had a rapid tempo of puberty by 6 months after injury, and all of them continued to progress in puberty at the 12 month visit. Two of them required therapy to slow down the progression of puberty. It is thought that the brain injury interferes with the inhibition of gonadotropin release. Gonadotropin release is normally kept low by negative feedback in the prepubertal years. The mechanism may involve TBI causing the loss of neural inhibitory influence of gamma-aminobutyric acid (GABA) on the gonadotropin releasing hormone (GnRH) pulse generator, or loss of inhibitory effects on the N-methyl-d-aspartate (NMDA) receptors resulting from the hypothalamic-pituitary injury [45, 46]. This process is similar to what is found clinically in populations of children with a history of meningitis, hydrocephalus, brain tumors, or encephalopathy.
ACTH deficiency
Another persistent endocrinopathy seen long-term after TBI in children is ACTH deficiency (ACTH-D). A wide range of incidence results from different criteria and a variety of tests used to make the diagnosis. However, when using an ACTH stimulation test (250 mcg cortrosyn), there was only a 7% incidence of ACTH-D. Results are less consistent among different studies when basal cortisol levels are used, than when low-dose ACTH test is used to make the diagnosis of secondary adrenal insufficiency after TBI [31]. A low-dose ACTH stimulation test (1 mcg/m2, with peak cortisol obtained at 20–30 min) can be used to evaluate for hypothalamic or pituitary adrenal insufficiency [47]. Kaulfers [30] found no cases of low basal cortisol levels before 6 months, using strict criteria for diagnosis (cortisol <5 mcg/dl). Basal cortisol concentrations did not correlate well with the peak cortisol response to low-dose ACTH stimulation test at the 6 month visit. At that time, one patient had a low basal cortisol (3.3 mcg/dl) but a normal stimulated cortisol level (26.3 mcg/dl), and another patient had a normal basal cortisol (11.9 mcg/dl) but an abnormal stimulated cortisol (18.1 mcg/dl). A large metanalysis of ACTH testing looked at 13 studies, and the mean basal cortisol in patients without adrenal insufficiency was 13 μg/dl. After low-dose stimulation with cortrosyn, cortisol levels over 22 μg/dl were consistent with adrenal sufficiency [47].
Among retrospective studies, Poomthavorn et al. [27] showed results similar to Kaulfers et al. [30]. Only one of 15 patients tested had a low basal cortisol level, and that patient had a normal stimulated cortisol level on a low-dose ACTH stimulation test [27]. Niederland et al. [26] performed insulin tolerance tests on 26 children after TBI, and found that their stimulated cortisol levels were lower than in healthy controls. Einaudi et al. [19], in their prospective cohort, reported two patients with low basal cortisol levels at 6 months after injury, only one of whom failed a glucagon stimulation test. ACTH-D was confirmed in that patient at the 12 month visit. Each pediatric study has used a different standard for diagnosis of ACTH deficiency, thus it is difficult to draw conclusions about the true incidence. However, each study found only a few patients with persistent adrenal insufficiency. Therefore, even though ACTH deficiency is possible and life-threatening, it is not as common as GHD or GnRH deficiency in children after TBI.
Central hypothyroidism
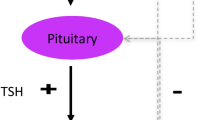
Disturbances in thyroid function are commonly observed acutely after brain injury, characteristic of a state of non-thyroidal illness, including low triiodothyronine (T3) and low T4, usually with a normal level of TSH [48]. Kaulfers [30] found that 21% had a low Free T4 at baseline, and 24% at 3 months. Einaudi [19] found similar results; 23% of children transiently had low Free T3 acutely after injury. Interestingly, Kaulfers [30] found that 11% had an elevated TSH at baseline after injury. The suggested mechanism of central hypothyroidism with elevated TSH is abnormal glycosylation of the TSH alpha and beta subunits, thus the TSH secreted is not biologically active [49, 50].
A sensitive method for confirming central hypothyroidism (TSH-D) requires recognition of the circadian pattern of TSH secretion [50]. Many patients with TSH-D maintain normal TSH concentrations and iodothyronine concentrations that are just below the normal range or in the lowest third of the normal range [50]. A significant rise in TSH occurs at night in normal children and adults, which is termed the TSH surge [51]. The nocturnal surge is blunted in patients with TSH-D, leading to Free T4 in the lowest third of the normal range [52].
Failure to recognize and treat TSH-D can result in less than optimal overall state of health and poor growth. In a prior report of children with short stature, an incidence of approximately 13 per 100 short children had a blunted TSH surge associated with low or low–normal Free T4 in the absence of any other pituitary hormone disturbance. The incidence was 33% of children with height shorter than −2 SD who had a Free T4 in the lowest third of the normal range. These children showed a significant increase in growth velocity during levothyroxine therapy compared to the growth response of children who had a normal TSH surge who were otherwise clinically similar [52]. Another model of central nervous system injury to the hypothalamus is cranial irradiation. TSH surge was found to be abnormal in 43% of referred poorly growing childhood cancer survivors [53].
The TSH surge test was used to diagnose central hypothyroidism after TBI [29]. An abnormal TSH surge was identified in 46% of the patients at 6 months after TBI, and most (72%) of them had a Free T4 in the lowest third of the normal range. Many of these cases would have been missed by only checking a Free T4 and TSH level. The TSH surge continued to be abnormal in 10% of the patients at 12 months. Thus, central hypothyroidism can be a transient or persistent deficiency. Pediatric TBI studies found an incidence of TSH deficiency at 1 year after injury (5–12%) similar to that observed in adult TBI studies (2–22%) [19, 24, 26, 27].
Hyperprolactinemia
Elevated prolactin (PRL) reflects probable pituitary stalk injury. Hyperprolactinemia may occur after hypothalamic or pituitary injury in both adults and children. Hyperprolactinemia is usually transient and resolves within the first year after injury. Two retrospective studies in children each reported one child with elevated PRL at 1–2 years post-injury [26, 27]. Both children had PRL elevation associated with other pituitary deficiencies. There were no reports in the pediatric literature of elevated PRL at more than 2 years after injury. Either PRL was not evaluated at 2 years or was transient after head injury. Kaulfers [30] found that PRL elevation was one of the most common abnormalities observed at both three and 6 months after injury, even after eliminating those patients on medications that cause hyperprolactinemia [30]. However, all cases resolved by 12 months after injury.
Diabetes insipidus
In prospective studies of children [21], there was a 4.3% incidence of diabetes insipidus (DI) at 12 months post-injury. Kaulfers [30] found 10% to have transient DI, but no permanent cases of DI. Among retrospective studies in children, only one found transient DI in one patient, and permanent DI in another who had a pituitary stalk transection [27]. Persistent DI appears to be a potential but rare phenomenon in children post-TBI.
Predictors of endocrinopathies
The prevalence of endocrinopathies at 12 months was not correlated with severity of injury as measured by the Glasgow Coma Score (GCS). In addition, CT or MRI findings after TBI were not associated with presence of endocrinopathies at 12 months [30]. Patients with persistent endocrinopathies at 1 year reported a higher incidence of mood disturbances and altered appetite than those without hormone deficiencies [30, 42]. Thus, if children report fatigue, cold intolerance, poor growth, altered puberty, mood disturbances, or altered appetite control after TBI, they should be considered for an endocrine evaluation, as some deficiencies can be subtle.
Time course of changes in endocrine function over time after TBI
In survivors, endocrine deficiencies after pediatric TBI may present acutely or manifest slowly over subsequent months or years. These deficiencies can have a profound impact on a child’s ongoing development and long-term recovery. In case reports of pituitary deficiencies after head injury in children, most were not diagnosed until years after the initial injury, leading to unrecognized poor growth and/or altered puberty [23]. Acquired GHD in childhood can impair adult height if there is a delay in diagnosis and treatment [54]. Consistent with adult literature, the most common endocrinopathies after TBI in children are GHD and hypogonadism [29]. Hypogonadism may not be apparent in prepubertal age children and would require a high index of suspicion in early adolescence. In addition, children may develop precocious puberty.
There can be considerable difficulty discriminating post-TBI behavior and endocrine deficiency from typical adolescent behaviors. After TBI there can be fatigue and impaired executive function. The effects of having puberty earlier than peers can also present significant clinical challenges.
Recommendations
Based on the publications in adults after TBI, a consensus conference recommended systematic endocrine screening of all patients after moderate to severe TBI [13] (see Table 1). Those found to have hormone deficiencies benefit from appropriate hormonal replacement [13]. Regarding patients after milder injury such as concussion, there are limited data and no recommendations have been published for screening of endocrine function.
The current review shows that endocrine dysfunction in children after TBI is common, can evolve after injury, and can be persistent (see Table 2). Every child with a moderate or severe head injury should undergo routine endocrine surveillance until at least 1 year after injury, even if there were no findings at 6 months (see Table 1). Most, but not all, endocrine abnormalities resolve by 1 year after TBI. New endocrinopathies may be identified at 6 and even 12 months after injury in children. Overall, 84% of pediatric patients had an endocrine disruption. Most were transient and isolated, while 38% of the endocrine deficiencies were persistent.
Further studies in children are warranted to better describe the natural progression of endocrine function after TBI. Attention to diagnosis and therapy of endocrine abnormalities early after TBI may improve QOL and speed of recovery from post-trauma sequelae. We recommend on-going endocrine surveillance at both 6 and 12 months after TBI to document resolution of temporary abnormalities and to ensure early intervention for persistent or late-occurring endocrinopathies.
References
Bruns J Jr, Hauser WA (2003) The epidemiology of traumatic brain injury: a review. Epilepsia 44(suppl 10):2–10
Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA (2006) Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics 118:483–492
Keenan HT, Runyan DK, Nocera M (2006) Longitudinal follow-up of families and young children with traumatic brain injury. Pediatrics 117:1291–1297
McCarthy ML, MacKenzie EJ, Durbin DR, Aitken ME, Jaffe KM, Paidas CN et al (2006) Health-related quality of life during the first year after traumatic brain injury. Arch Pediatr Adolesc Med 160:252–260
Acerini CL, Tasker RC (2008) Neuroendocrine consequences of traumatic brain injury. J Pediatr Endocrinol Metab 21:611–619
Popovic V, Pekic S, Pavlovic D, Maric N, Jasovic-Gasic M, Djurovic B et al (2004) Hypopituitarism as a consequence of traumatic brain injury (TBI) and its possible relation with cognitive disabilities and mental distress. J Endocrinol Invest 27:1048–1054
Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A (2007) Hypothalamopituitary dysfunction following traumatic brain injury, aneurysmal subarachnoid hemorrhage: a systematic review. JAMA 298:1429–1438
Agha A, Phillips J, Thompson CJ (2007) Hypopituitarism following traumatic brain injury (TBI). Br J Neurosurg 21:210–216
Bushnik T, Englander J, Katznelson L (2007) Fatigue after TBI: association with neuroendocrine abnormalities. Brain Inj 21:559–566
Tanrverdi F, De Bellis A, Bizzarro A, Sinisi AA, Bellastella G, Pane E, Bellastella A, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2008) Antipituitary antibodies after traumatic brain injury: is head trauma-induced pituitary dysfunction associated with autoimmunity? Eur J Endocrinol 159:7–13
Pavlovic D, Pekic S, Stojanovic M, Zivkovic V, Djurovic B, Jovanovic V, Miljic N, Medic-Stojanoska M, Doknic M, Miljic D, Djurovic M, Casanueva F, Popovic V (2010) Chronic cognitive sequelae after traumatic brain injury are not related to growth hormone deficiency in adults. Eur J Neurol 17:696–702
Berg C, Oeffner A, Schumm-Draeger PM, Badorrek F, Brabant G, Gerbert B, Bornstein S, Zimmermann A, Weber M, Broecker-Preuss M, Mann K, Herrmann BL (2010) Prevalence of anterior pituitary dysfunction in patients following traumatic brain injury in a German multi-centre screening program. Exp Clin Endocrinol Diabetes 118:139–144
Ghigo E, Masel B, Aimaretti G, Leon-Carrion J, Casanueva FF, Dominguez-Morales MR et al (2005) Consensus guidelines on screening for hypopituitarism following traumatic brain injury. Brain Inj 19:711–724
Barton RN, Stoner HB, Watson SM (1987) Relationships among plasma cortisol, adrenocorticotrophin, and severity of injury in recently injured patients. J Trauma 27:384–392
Woolf PD, Cox C, Kelly M, Nichols D, McDonald JV, Hamill RW (1990) The adrenocortical response to brain injury: correlation with the severity of neurologic dysfunction, effects of intoxication, and patient outcome. Alcohol Clin Exp Res 14:917–921
Cohan P, Wang C, McArthur DL, Cook SW, Dusick JR, Armin B et al (2005) Acute secondary adrenal insufficiency after traumatic brain injury: a prospective study. Crit Care Med 33:2358–2366
Srinivas R, Brown SD, Chang YF, Garcia-Fillion P, Adelson PD (2010) Endocrine function in children acutely following severe traumatic brain injury. Childs Nerv Syst 26:647–653
Behan LA, Phillips J, Thompson CJ, Agha A (2008) Neuroendocrine disorders after traumatic brain injury. J Neurol Neurosurg Psychiatry 79:753–759
Einaudi S, Matarazzo P, Peretta P, Grossetti R, Giordano F, Altare F et al (2006) Hypothalamo-hypophysial dysfunction after traumatic brain injury in children, adolescents: a preliminary retrospective and prospective study. J Pediatr Endocrinol Metab 19:691–703
Morares RB, Czepielewski M, Friedman G, de Borba EL (2011) Diagnosis of adrenal failure in critically ill patients. Arq Bras Endocrinol Metab 55:295–302
Barzilay Z, Somekh E (1998) Diabetes insipidus in severely brain damaged children. J Med 19:47–64
Tanriverdi F, Senyurek H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2006) High risk of hypopituitarism after traumatic brain injury: a prospective investigation of anterior pituitary function in the acute phase and 12 months after trauma. J Clin Endocrinol Metab 91:2105–2111
Kokshoorn NE, Wassenaar MJE, Biermasz NR, Roelfsema F, Smit JWA, Romijn JA, Pereira AM (2010) Hypopituitarism following traumatic brain injury: prevalence is affected by the use of different dynamic tests and different normal values. Eur J Endocrinol 162:11–18
Aimaretti G, Ambrosio MR, Di Somma C, Gasperi M, Cannavo S, Scaroni C et al (2005) Hypopituitarism induced by traumatic brain injury in the transition phase. J Endocrinol Invest 28:984–989
Bruce DA, Schut L, Bruno LA, Wood JH, Sutton LN (1978) Outcome following severe head injuries in children. J Neurosurg 48:679–688
Niederland T, Makovi H, Gal V, Andreka B, Abraham CS, Kovacs J (2007) Abnormalities of pituitary function after traumatic brain injury in children. J Neurotrauma 24:119–127
Poomthavorn P, Maixner W, Zacharin M (2008) Pituitary function in paediatric survivors of severe traumatic brain injury. Arch Dis Child 93:133–137
Medic-Stojanoska M, Pekic S, Curic N, Djilas-Ivanovic D, Popovic V (2007) Evolving hypopituitarism as a consequence of traumatic brain injury (TBI) in childhood—call for attention. Endocrine 31:268–271
Acerini CL, Tasker RC (2007) Endocrine sequelae of traumatic brain injury in childhood. Horm Res 68(Suppl 5):14–17
Kaulfers AM, Backeljauw PF, Reifschneider K, Blum S, Michaud L, Weiss M, Rose SR (2010) Endocrine dysfunction following traumatic brain injury in children. J Pediatr 157:894–899
Bolado GG, Estebanez M, Arizkeuren EM, Calcena AA, Esteves AR, Vela A, Rica I (2011) Assessment of pituitary function after traumatic brain injury in childhood. Abstract P2-d1-680: European Society for Pediatric Endocrinology (ESPE), Glasgow
Aleksijevic D, Zapletalova J, Krahulik D, Klaskova E, Widermann J, Mihal V (2011) Endocrine dysfunction after traumatic brain injury in children and adolescents (a single centre prospective study). Abstract P2-d1-732: European Society for Pediatric Endocrinology (ESPE), Glasgow
Hewitt J, Pitkin J, Corbin V, Maixner W, Zacharin M (2011) Endocrine sequelae of traumatic brain injury in children: a prospective study. Abstract P1-d3-347: European Society for Pediatric Endocrinology (ESPE), Glasgow
Agha A, Thompson CJ (2005) High risk of hypogonadism after traumatic brain injury: clinical implications. Pituitary 8:245–249
Popii V, Baumann G (2004) Laboratory measurement of growth hormone. Clin Chim Acta 350:1–16
Romshe CA, Zipf WB, Miser A, Miser J, Sotos JF, Newton WA (1984) Evaluation of growth hormone release and human growth hormone treatment in children with cranial irradiation-associated short stature. J Pediatr 104:177–181
Blatt J, Bercu BB, Gillin JC, Mendelson WB, Poplack DG (1984) Reduced pulsatile growth hormone secretion in children after therapy for acute lymphoblastic leukemia. J Pediatr 104:182–186
Rose SR, Municchi G (1999) Six-hour and four-hour nocturnal sampling for growth hormone. J Pediatr Endocrinol Metab 12:167–173
Bondanelli M, Ambrosio MR, Cavazzini L, Bertocchi A, Zatelli MC, Carli A et al (2007) Anterior pituitary function may predict functional and cognitive outcome in patients with traumatic brain injury undergoing rehabilitation. J Neurotrauma 24:1687–1697
Klose M, Juul A, Struck J, Morgenthaler NG, Kosteljanetz M, Feldt-Rasmussen U (2007) Acute and long-term pituitary insufficiency in traumatic brain injury: a prospective single-centre study. Clin Endocrinol (Oxf) 67:598–606
Schneider HJ, Schneider M, Saller B, Petersenn S, Uhr M, Husemann B et al (2006) Prevalence of anterior pituitary insufficiency 3 and 12 months after traumatic brain injury. Eur J Endocrinol 154:259–265
Bavisetty S, McArthur DL, Dusick JR, Wang C, Cohan P, Boscardin WJ et al (2008) Chronic hypopituitarism after traumatic brain injury: risk assessment and relationship to outcome. Neurosurgery 62:1080–1093 (discussion 1093-4)
Norwood KW, DeBoer MD, Gurka MJ, Kuperminc MN, Rogol AD, Blackman JA, Wamstad JB, Buck ML, Patrick PD (2010) Traumatic brain injury in children and adolescents: surveillance for pituitary dysfunction. Clin Pediatr 49:1044–1049
Behan LA, Agha A (2007) Endocrine consequences of adult traumatic brain injury. Horm Res 68(Suppl 5):18–21
Grumbach MM (2002) The neuroendocrinology of human puberty revisited. Horm Res 57(Suppl 2):2–14
Bourguignon JP, Gérard A, Purnelle G, Czajkowski V, Yamanaka C, Lemaître M, Rigo JM, Moonen G, Franchimont P (1997) Duality of glutamatergic and GABAergic control of pulsatile GnRH secretion by rat hypothalamic explants: II. Reduced NR2C- and GABAA-receptor-mediated inhibition at initiation of sexual maturation. J Neuroendocrinol 9(3):193–199
Kazlauskaite R, Evans AT, Villabona CV, Abdu TA, Ambrosi B, Atkinson AB et al (2008) Corticotropin tests for hypothalamic–pituitary–adrenal insufficiency: a metaanalysis. J Clin Endocrinol Metab 93:4245–4253
Chiolero RL, Lemarchand-Beraud T, Schutz Y, de Tribolet N, Bayer-Berger M, Freeman J (1988) Thyroid function in severely traumatized patients with or without head injury. Acta Endocrinol (Copenh) 117:80–86
Faglia G, Bitensky L, Pinchera A, Ferrari C, Paracchi A, Beck-Peccoz P et al (1979) Thyrotropin secretion in patients with central hypothyroidism: evidence for reduced biological activity of immunoreactive thyrotropin. J Clin Endocrinol Metab 48:989–998
Rose SR (2010) Improved diagnosis of mild hypothyroidism using time-of-day normal ranges for thyrotropin. J Pediatr 157:662–667
Rose SR, Nisula BC (1989) Circadian variation of thyrotropin in childhood. J Clin Endocrinol Metab 68:1086–1090
Rose SR (1995) Isolated central hypothyroidism in short stature. Pediatr Res 38:967–973
Rose SR (2001) Cranial irradiation and central hypothyroidism. Trends Endocrinol Metab 12(3):97–104
Casanueva FF, Leal A, Koltowska-Haggstrom M, Jonsson P, Goth MI (2005) Traumatic brain injury as a relevant cause of growth hormone deficiency in adults: a KIMS-based study. Arch Phys Med Rehabil 86:463–468
Acknowledgments
This review would not have been possible without the diligent efforts of our colleagues Anne-Marie Kaulfers, Samantha Blum, Tammy Weis, Linda Michaud, and Kathi Makoroff.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rose, S.R., Auble, B.A. Endocrine changes after pediatric traumatic brain injury. Pituitary 15, 267–275 (2012). https://doi.org/10.1007/s11102-011-0360-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-011-0360-x