Abstract
Hyperprolactinemia has been associated with impaired metabolism, including insulin resistance. However, the metabolic effects of elevated prolactin (PRL) levels are not completely clarified. The aim of this study was to obtain more insights of metabolic consequences in hyperprolactinemia patients. Fourteen consecutive patients, eight women and six men, aged 39.7 (±13.7) years with prolactinomas (median PRL 72 [49–131] μg/L in women and 1,260 [123–9,600] μg/L in men) were included. Anthropometric data and metabolic values were studied before and after 2 and 6 months on DA agonists (Bromocriptine [5.7 (±3.9) mg/day, n = 13] or Cabergoline [0.5 mg/week, n = 1]). Euglycemic hyperinsulinemic clamps were studied in six patients before and after 6 months of treatment. PRL normalized in all patients. Anthropometric data changed only in males with a significant decrease of median body weight (95.6 [80.7–110.1] to 83.4 [77.8–99.1] kg, P = 0.046), waist circumference and fat percentage after 6 months. LDL cholesterol was positively correlated to PRL at diagnosis (r = 0.62, P = 0.025) and decreased within 2 months (3.4 [±0.9] to 2.9 [±0.6] mmol/L, P = 0.003). Insulin, IGFBP-1 and total adiponectin levels did not change. Insulin sensitivity tended to improve after 6 months; M-value from 5.7 (±1.8) to 7.8 (±2.6) mg/kg/min, P = 0.083 and per cent improvement in M-value was correlated to per cent reduction in PRL levels (r = −0.85, P = 0.034). In conclusion, beneficial metabolic changes were seen in prolactinoma patients after treatment with DA agonists, underscoring the importance of an active treatment approach and to consider the metabolic profile in the clinical management of hyperprolactinemia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prolactin (PRL) is a multifunctional polypeptide hormone produced by the lactotrophs in the anterior pituitary as well as by different extrapituitary sites [1]. The main effect of PRL in humans is to regulate mammary gland development during pregnancy and to induce milk production. However, a wide variety of functions have been attributed to PRL [2].
For some years, PRL has attracted attention as a metabolic hormone. Hyperprolactinemia has been reported to be associated with abnormalities of carbohydrate and lipid metabolism [3]. In patients with elevated PRL levels reduced glucose tolerance and hyperinsulinemia have been demonstrated [4–6]. Moreover, increased insulin resistance using homeostasis model assessment (HOMA) index is described in patients with hyperprolactinemia [7, 8] and that insulin sensitivity index (ISI composite) is reduced in the hyperprolactinemic state, improving after normalization of PRL by dopamine (DA) agonist therapy [9]. Additionally, in a recent study hyperprolactinemic patients were more insulin resistant than controls, measured by a euglycemic hyperinsulinemic clamp [10]. Furthermore, treatment with Bromocriptine (BRC) in non-hyperprolactinemic obese humans or patients with diabetes mellitus (DM) type 2 improved lipid profile [11] and glycemic control [12], respectively.
Hyperprolactinemia has also been linked to hypercholesterolemia [13], with [14] or without [7] improvement after treatment with DA agonists. In humans, sustained hyperprolactinemia is often associated with weight gain and obesity [15, 16] with weight loss after normalization of PRL by DA agonists [15, 17], although some findings are conflicting and contradictory [7, 18]. The linkage between hyperprolactinemia and weight gain remains elusive; however, reduced central dopaminergic tone as a result of persistent hyperprolactinemia has been proposed as one possible mechanism [17]. Furthermore, endothelial dysfunction [9] and low-grade inflammation [7, 9] have been demonstrated in these patients. Thus, to some extent the metabolic consequences of hyperprolactinemia are similar to those of the metabolic syndrome. The aim of this study was to obtain more insight into the metabolic consequences of hyperprolactinemia by evaluating anthropometric data, blood lipids and insulin sensitivity before and after normalization of PRL by DA agonist therapy.
Patients and methods
Patients
Fifteen consecutive patients with newly diagnosed hyperprolactinemia, referred to the outpatient clinic at the Department of Endocrinology, Metabolism and Diabetology, Karolinska University Hospital, Stockholm, Sweden, were included in the study. One woman was excluded because of pregnancy. Thus, the final sample consisted of fourteen patients (eight women and six men). The study was approved by the Stockholm Regional Ethical Review Board and informed written consent was obtained from all patients.
Inclusion criteria were elevated PRL levels found on at least two occasions and magnetic resonance imaging of the hypothalamic-pituitary region confirming a prolactinoma. Exclusion criteria were combined hormone-producing pituitary tumors, secondary causes of hyperprolactinemia, pregnancy or patients on medication for hyperlipidemia and DM.
Baseline characteristics of the study subjects at diagnosis are presented in Table 1. Male patients had higher PRL levels (P = 0.004) and larger tumors than females. One woman was postmenopausal receiving low-dose estrogens at study entry. Her initially low gonadotrophins rose to normal postmenopausal levels after normalization of PRL. The other seven women were premenopausal: four of them were on hormonal contraceptives both at diagnosis and throughout the study period. In the other three women, two had secondary amenorrhea and one had oligomenorrhea. Two male patients had testosterone substitution already at referral to our clinic, which was kept unchanged during the study period. The other four men had hypogonadotrophic hypogonadism with testosterone levels below normal range together with low or normal levels of gonadotrophins. One male patient had secondary hypothyroidism at diagnosis and received substitution with 100 μg levothyroxine per day. This patient did not participate in the clamp and was excluded from the analysis of thyroid hormones and lipids. Apart from this, all patients were without medications and were non-smokers.
Study protocol
Patients were examined at base line (t0) and after 2 (t2) and 6 (t6) months of DA agonist therapy (BRC or Cabergoline [CAB]). Anthropometric data and laboratory measurements were studied at t0, t2 and t6. Blood samples were obtained in the morning after an overnight fast for measurements of hormones (PRL, TSH, fT4, testosterone, GH, IGF-I, IGF-binding protein-1 [IGFBP-1]), metabolic variables (glucose, hemoglobin A1c [HbA1c], insulin, C-peptide, lipid profile, leptin, adiponectin) and inflammatory markers (high sensitive CRP [hsCRP], tumor necrosis factor alpha [TNF-α]). Peripheral insulin sensitivity was determined using the euglycemic hyperinsulinemic clamp (clamp) technique at t0 and t6 in six patients (four women and two men). The other patients did not accept the clamp procedure for different reasons. We also assessed insulin resistance in all patients using HOMA and the insulin resistance index (HOMA-IR) was calculated (fasting plasma glucose [mmol/L] * fasting serum insulin [μU/mL]/22.5) [19]. To convert insulin from SI units to conventional unit values were divided by 6.945.
Thirteen patients were treated with BRC (mean dose 5.7 [±3.9] mg per day [range 1.25–15 mg]) and one patient was treated with CAB (0.5 mg per week) because of side effects of BRC. To normalize PRL the male patients required significantly higher doses of BRC than the females (8.5 [±4.1] mg vs. 3.2 [±1.2] mg) (P = 0.007).
Anthropometric data
Physical examination included measurements of height, weight, waist and hip. Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2). Waist and hip circumference were measured to calculate waist-hip ratio (WHR). Total body fat, fat free mass (FFM) and total body water were determined by bioelectrical impedance [20] using a body composition analyzer (Tanita, TBF-300).
Euglycemic hyperinsulinemic clamp
A clamp was performed according to De Fronzo et al. [21]. In brief, intravenous catheters were inserted into the right arm for substrate (insulin/glucose) infusion. A superficial dorsal hand vein was cannulated in retrograde fashion with a 21-gauge butterfly needle and kept patent by a slow saline infusion. The hand was kept warm by an electric device for intermittent sampling of arterialized venous blood. During the 120 min of the test, insulin (Actrapid [40 mU * m2(−1) * min−1], NovoNordisk A/S, Copenhagen, Denmark) was infused together with 20% dextrose (Fresenius Kabi, Stockholm, Sweden). The rate of dextrose infusion was adjusted to achieve a blood glucose level of 5.0 mmol/L based on arterialized samples withdrawn every 5th min from an ipsilateral dorsal hand vein (heated air box set at 55°C, University of Nottingham, U.K.). Whole-body insulin sensitivity (M-value) was calculated from the amount of glucose infused during the last 30 min of the clamp divided by body weight (kg) and period (min) and expressed as mg/kg/min.
Biochemical assays
Serum PRL was measured using commercial chemiluminescence immunoassay (Beckman Coulter Unicel, DXI), normal range: 3–27 μg/L (women <50 years); 3–20 μg/L (women ≥50 years); 3–13 μg/L (men). The sera were not screened for macroprolactin due to the specificity of the PRL method. In-house RIAs were used for IGF-I and IGFBP-1 with individual serum samples from the different investigations in the same assay. IGF-I was measured after ethanol extraction and cryoprecipitation and using des (1–3) IGF-I as ligand [22]. The intra- and inter-assay CV were 4 and 11%, respectively. The standard deviation (SD) scores of IGF-I were calculated from the regression of healthy adult subjects [23]. The RIA for IGFBP-1 was performed according to Póvoa et al. [24] with intra- and inter-assays CV 3 and 10%, respectively. The geometrical means and 95% confidence interval (CI) of IGFBP-1 in 595 non diabetic middle-aged women and men are 41 (95% CI; 39–44) and 19 (95% CI; 18–20) μg/L, respectively [25]. Plasma total cholesterol, high-density lipoprotein (HDL) cholesterol and triglycerides were measured by automated colorimetric methods (UniCel DXC800, Beckman Coulter, Fullerton, CA, USA). Low-density lipoprotein (LDL) cholesterol was calculated according to the formula suggested by Friedewald et al. [26]. The upper normal limit in reference population for fasting total cholesterol was 6.1 mmol/L (<31 years), 6.9 mmol/L (<51 years) and 7.8 mmol/L (≥51 years); the corresponding values for LDL cholesterol were 4.3, 4.7 and 5.3 mmol/L, respectively. The normal range for fasting triglycerides was 0.45–2.6 mmol/L. Commercial kits were used for the following factors: S-insulin and S–C-peptide by electrochemiluminescence immunoassays (Roche Diagnostics GmbH, Mannheim) (reference range for fasting values 18-173 pmol/L and 0.25-1.0 nmol/L, respectively), S-total adiponectin and S-leptin by RIA kit (Millipore Corporation, Linco Research, Inc, USA), S-TNF-α by chemiluminescent immunometric assay (Immulite, Siemens, Gwynedd, Great Britain) and P-hsCRP by an automated immunoturbidimetric assay (Beckman Coulter, Fullerton, CA, USA) with the lower detection limit 0.2 mg/L and reference range <3.0 mg/L. HbA1c was measured by cat-ion exchange chromatography (MonoS column) with HPLC (Bio-Rad) (reference range 3.9–5.3%). S-TSH (reference range 0.4–3.5 mE/L), S-free T4 (reference range 8–14 pmol/L), S-testosterone (reference range in men, 10–30 nmol/L), P-glucose (reference range for fasting values 4.0–6.0 mmol/L) and S-GH were all measured using routine assays.
Statistical analysis
Normally distributed data are presented as mean (± SD), otherwise as median and range (min–max). Differences between women and men were analyzed with unpaired Student’s t test when data or log-transformed data were normally distributed. The Mann–Whitney rank sum test was used if the distribution was not normal. For comparison between repeated measurements in the same patients, one way repeated measures analysis of variance (ANOVA) was used and if significance followed by Tukey post-hoc test, in non normally distributed data Friedman ANOVA was used followed by Wilcoxon signed rank test. Correlation analyses were performed using linear regression with log-transformed data when required or Spearman Rank order correlation test. Per cent change in M-value was calculated as M-value ([t6-t0]/t0) * 100 and per cent change in S-PRL as S-PRL ([t6-t0]/t0) * 100. Statistical analyses were performed using Statistica StatSoft version 9.0 (Tulsa, OK, USA). A two-sided p-value < 0.05 was considered statistically significant.
Results
The main reduction of serum PRL occurred after 2 months of DA agonist treatment in both women and men (Fig. 1). Median PRL level in women decreased from 72 (49–131) to 11 (1.0–17) μg/L at 2 months (P = 0.012) and remained within normal range at 6 months, 9.3 (2.9–20) μg/L. In the six men, the corresponding values were 1,260 (123–9,600), 51 (3.8–77) and 11 (3.1–13) μg/L, respectively.
S-PRL levels at diagnosis and after 2 and 6 months of DA agonist therapy in women (a) and men (b) with prolactinomas. Dotted line indicates Case 4 (Fig. 1a)
Anthropometric variables
Data on body composition before and after DA agonist therapy are presented in Table 2. None of the women had a BMI ≥ 30 kg/m2 at diagnosis, whereas three out of six men were obese (BMI ≥ 30 kg/m2). However, no significant difference in BMI was observed between women and men (P = 0.228). No significant changes in anthropometric variables were observed in women after DA agonist treatment. In men no changes in body composition were demonstrated after 2 months, but after 6 months there was a significant decrease in body weight, BMI, waist circumference and body fat % (P < 0.05) (Table 2).
Hormonal and metabolic variables
The hormonal and metabolic levels are shown in Table 3. Apart from the patient with TSH deficiency, the thyroid hormone levels were within the normal range before and after treatment. Serum testosterone levels increased significantly after 6 months in the four men without testosterone replacement therapy (P = 0.002) (Table 3). Total IGF-I levels in relation to age were within normal range and did not change during therapy in the whole group. Leptin values decreased significantly after 6 months of DA agonist therapy only in men, which was probably due to the close positive correlation between percent change in leptin and body fat% (r = 0.89, P < 0.05).
A positive association between LDL cholesterol and serum PRL levels at diagnosis was demonstrated (r = 0.62, P = 0.025) (Fig. 2). Total and LDL cholesterol decreased significantly already after 2 months of DA agonist treatment. No correlations between LDL cholesterol and dose of BRC at 2 and 6 months, respectively, were seen (r = 0.02, P = 0.958 and r = 0.04, P = 0.901). Further, no detectable changes were observed in HDL cholesterol, triglycerides, hsCRP or TNF-α between the hyperprolactinemic and normalized state (Table 3).
The relation between P-LDL cholesterol and S-PRL in hyperprolactinemia patients at diagnosis (circle) and after 2 (filled triangle) and 6 (filled square) months of DA agonist therapy. The regression line for the correlation between P-LDL cholesterol and S-PRL at diagnosis (circle) is presented. The patient with diabetes mellitus at diagnosis is marked (DM)
IGFBP-1 and adiponectin levels were not altered during therapy in the whole sample or in men and women analyzed separately. There was no significant correlation between total adiponectin and PRL levels at diagnosis or after 2 and 6 months, respectively (r = −0.43, P = 0.123; r = −0.43, P = 0.122; r = 0.15, P = 0.599). Fasting glucose, HbA1c, insulin, C-peptide levels and HOMA-IR did not change after treatment (Table 3). After inclusion in the study, DM type 2 was diagnosed in one male patient with fP-glucose 12 mmol/L and HbA1c 8.2% which improved after 6 months (6.7 mmol/L and 5.6%, respectively), without glucose lowering treatment. This patient did not participate in the clamp.
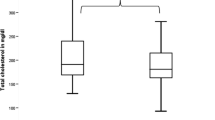
Insulin sensitivity determined by clamp
No obvious differences were observed between the six patients who accepted to perform the clamp and the whole patient group (Table 4). A tendency of improvement in insulin sensitivity after normalization of PRL by DA agonist therapy was demonstrated: the M-value at baseline was 5.7 (±1.8) and at 6 months 7.8 (±2.6) mg/kg/min, P = 0.083 (Fig. 3). All patients, except one female (case 4), improved their insulin sensitivity as assessed by the clamp. Per cent change in insulin sensitivity was correlated to per cent reduction in PRL levels at 6 months (r = −0.85, P = 0.034) (Fig 4). In the five patients treated with BRC who performed the clamp; percent change in insulin sensitivity was correlated to per cent reduction in PRL levels (r = −0.89, P = 0.042) but also to BRC dose (r = 0.92, P = 0.029), which, in addition, was associated with the reduction in PRL levels (r = −0.90, P = 0.035). No correlation was found between per cent change in M-value and adiponectin levels (r = 0.37, P = ns) or change in body fat% (r = −0.49, P = ns).
Discussion
In the present study of women and men with prolactinomas total and LDL cholesterol decreased significantly after reduction of PRL by DA agonist treatment. Furthermore, insulin sensitivity tended to improve and there was a correlation between improvement in insulin sensitivity and reduction in PRL levels.
Hypercholesterolemia has been linked to patients with hyperprolactinemia [13]. In a recent study total and LDL cholesterol were higher in patients with prolactinomas than controls [27], while in other studies no differences in lipoprotein profile have been reported [7, 9]. Treatment with BRC in obese non-diabetic women [11] and in patients with DM type 2 [12] has been shown to reduce both PRL and total cholesterol, while another study showed no changes in total cholesterol in patients with DM type 2 after BRC therapy [28]. In our cohort, LDL cholesterol correlated positively to PRL levels at diagnosis and total and LDL cholesterol decreased significantly already after 2 months on DA agonists. The reduction in LDL cholesterol was seen in women despite no change in weight and was evident in men before their weight loss. Furthermore, we found no correlation between reduction in LDL cholesterol and BRC dosage. Hypogonadism could be a confounding factor considering the levels of LDL cholesterol, but the majority of our female patients were on hormonal contraceptives from study start without any change in this medication during the study. In the four men without testosterone replacement the increase in testosterone levels were not clinically significant until after 6 months of treatment. Our results, may suggest a direct relation between LDL cholesterol and PRL levels. Its homologue GH induces the expression of hepatic LDL receptors, which is accompanied by a decrease in serum cholesterol [29] and it can be speculated that PRL may act in a similar way as GH in the liver.
In the present study, only six of the 14 patients participated in the clamp, reducing the power in this part of the study. However, five of these six patients showed a considerable improvement of peripheral insulin sensitivity. The woman in whom the M-value did not increase (case 4), had only slightly elevated PRL levels at diagnosis (49 μg/L) and also the highest PRL level within normal range at 6 months (20 μg/L). A significant correlation was found between per cent increase in M-value and reduction in PRL levels as well as to BRC dosage, which in turn correlated to decrease in PRL levels. Thus, the improvement in insulin sensitivity could be attributed to the decrease in PRL levels, BRC treatment, or a combination of these factors. In a previous study, BRC treatment of non-diabetic females did not change plasma insulin levels or the ability of insulin to mediate glucose disposal [11]. In contrast, in a clamp study of obese type 2 diabetics, BRC therapy improved insulin sensitivity [28]. Recently, insulin sensitivity, evaluated by clamp, was shown to be significantly lower in 16 hyperprolactinemia patients than controls [10] and in another study that HOMA-IR improved after DA agonist treatment [30]. Results from clamp studies evaluating insulin sensitivity in prolactinoma patients after DA agonist therapy has not been published before.
PRL has been shown to inhibit secretion of adiponectin from human adipose tissue in vitro [31] and suppression of adiponectin levels may be one factor that increases insulin resistance in hyperprolactinemic patients [32]. However, neither PRL levels nor the improvement in insulin sensitivity was correlated to total adiponectin levels in our study. Similar to adiponectin, IGFBP-1 levels did not change during DA agonist therapy, indicating no alterations in hepatic insulin sensitivity [33]. We did not find any changes in glucose, HbA1c, insulin or C-peptide levels after DA agonist treatment in the whole patient group. However, the patient with DM type 2 displayed a dramatic improvement with a decrease in HbA1c from 8.2 to 5.6% during BRC treatment and diet information.
Hyperprolactinemia has also been associated with elevated hsCRP, with reduction after treatment with DA agonists [7, 9]. In contrast, we found no change in hsCRP levels between the hyperprolactinemic and normalized state. Furthermore, there was no change in the pro-inflammatory cytokine TNF-α levels after DA agonist treatment, supporting the view that hyperprolactinemia, at least in this study, does not induce low-grade inflammation.
In agreement with others, we found that weight gain and obesity in our hyperprolactinemic patients were predominantly seen in men [16, 17]; after treatment, only the men demonstrated a reduction of weight, waist circumference and body fat%. In the current study, a control group was not established since our aim was to evaluate metabolic variables in patients before and after treatment, and thus we used the patients as their own controls. To compare with a healthy control group would probably not have helped us in defining the effects of PRL vs. other factors on metabolism.
In conclusion, total and LDL cholesterol decreased significantly after treatment with DA agonists in patients with hyperprolactinemia and improvement in insulin sensitivity correlated to the decrease in PRL levels. Our results may indicate a direct relation between LDL cholesterol and PRL, however the reasons for the metabolic changes seen in prolactinoma patients after treatment are complex and probably due to several factors. Our findings in a limited group of patients have to be confirmed in larger prospective studies, but underscore the importance of normalizing PRL levels in hyperprolactinemia patients as well as to evaluate and follow-up the metabolic status. Furthermore, it might be important to consider the metabolic profile, when not treating patients with asymptomatic hyperprolactinemia or in connection with discontinuation of DA agonist treatment, for example in postmenopausal women.
References
Ben-Jonathan N, Mershon JL, Allen DL, Steinmetz RW (1996) Extrapituitary prolactin: distribution, regulation, functions, and clinical aspects. Endocr Rev 17:639–669
Bole-Feysot C, Goffin V, Edery M, Binart N, Kelly PA (1998) Prolactin (PRL) and its receptor: actions, signal transduction pathways and phenotypes observed in PRL receptor knockout mice. Endocr Rev 19:225–268
Ben-Jonathan N, Hugo ER, Brandebourg TD, LaPensee CR (2006) Focus on prolactin as a metabolic hormone. Trends Endocrinol Metab 17:110–116
Landgraf R, Landraf-Leurs MM, Weissmann A, Horl R, von Werder K, Scriba PC (1977) Prolactin: a diabetogenic hormone. Diabetologia 13:99–104
Johnston DG, Alberti KG, Nattrass M, Burrin JM, Blesa-Malpica G, Hall K, Hall R (1980) Hyperinsulinaemia in hyperprolactinaemic women. Clin Endocrinol (Oxf) 13:361–368
Schernthaner G, Prager R, Punzengruber C, Luger A (1985) Severe hyperprolactinemia is associated with decreased insulin binding in vitro and insulin resistance in vivo. Diabetologia 28:138–142
Serri O, Li L, Mamputu JC, Beauchamp MC, Maingrette F, Renier G (2006) The influences of hyperprolactinemia and obesity on cardiovascular risk markers: effects of cabergoline therapy. Clin Endocrinol (Oxf) 64:366–370
Tuzcu A, Bahceci M, Dursun M, Turgut C, Bahceci S (2003) Insulin sensitivity and hyperprolactinemia. J Endocrinol Invest 26:341–346
Yavuz D, Deyneli O, Akpinar I, Yildiz E, Gozu H, Sezgin O, Haklar G, Akalin S (2003) Endothelial function, insulin sensitivity and inflammatory markers in hyperprolactinemic pre-menopausal women. Eur J Endocrinol 149:187–193
Tuzcu A, Yalaki S, Arikan S, Gokalp D, Bahcec M, Tuzcu S (2009) Evaluation of insulin sensitivity in hyperprolactinemic subjects by euglycemic hyperinsulinemic clamp technique. Pituitary 12:330–334
Kamath V, Jones CN, Yip JC, Varasteh BB, Cincotta AH, Reaven GM, Chen YD (1997) Effects of a quick-release form of bromocriptine (Ergoset) on fasting and postprandial plasma glucose, insulin, lipid, and lipoprotein concentrations in obese nondiabetic hyperinsulinemic women. Diabetes Care 20:1697–1701
Cincotta AH, Meier AH, Cincotta M Jr (1999) Bromocriptine improves glycemic control and serum lipid profile in obese Type 2 diabetic subjects: a new approach in the treatment of diabetes. Expert Opin Investig Drugs 8:1683–1707
Pelkonen R, Nikkila EA, Grahne B (1982) Serum lipids, post heparin plasma lipase activities and glucose tolerance in patients with prolactinoma. Clin Endocrinol (Oxf) 16:383–390
Fahy U, Hopton MI, Hartog M, Bolton CH, Hull MG (1999) The lipoprotein profile of women with hyperprolactinemic amenorrhoea. Hum Reprod 14:285–287
Greenman Y, Tordjman K, Stern N (1998) Increased body weight associated with prolactin secreting pituitary adenomas: weight loss with normalization of prolactin levels. Clin Endocrinol (Oxf) 48:547–553
Schmid C, Goede DL, Hauser RS, Brandle M (2006) Increased prevalence of high Body Mass Index in patients presenting with pituitary tumours: severe obesity in patients with macroprolactinoma. Swiss Med Wkly 136:254–258
Doknic M, Pekic S, Zarkovic M, Medic-Stojanoska M, Dieguez C, Casanueva F, Popovic V (2002) Dopaminergic tone and obesity: an insight from prolactinomas treated with bromocriptine. Eur J Endocrinol 147:77–84
Delgrange E, Donckier J, Maiter D (1999) Hyperprolactinaemia as a reversible cause of weight gain in male patients? Clin Endocrinol (Oxf) 50:271
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI (1985) Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 41:810–817
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
Bang P, Eriksson U, Sara V, Wivall IL, Hall K (1991) Comparison of acid ethanol extraction and acid gel filtration prior to IGF-I and IGF-II radioimmunoassays: improvement of determinations in acid ethanol extracts by the use of truncated IGF-I as radioligand. Acta Endocrinol (Copenh) 124:620–629
Hilding A, Hall K, Wivall-Helleryd IL, Saaf M, Melin AL, Thoren M (1999) Serum levels of insulin-like growth factor I in 152 patients with growth hormone deficiency, aged 19–82 years, in relation to those in healthy subjects. J Clin Endocrinol Metab 84:2013–2019
Povoa G, Roovete A, Hall K (1984) Cross-reaction of serum somatomedin-binding protein in a radioimmunoassay developed for somatomedin-binding protein isolated from human amniotic fluid. Acta Endocrinol (Copenh) 107:563–570
Lewitt MS, Hilding A, Brismar K, Efendic S, Ostenson CG, Hall K (2010) IGF-binding protein 1 and abdominal obesity in the development of type 2 diabetes in women. Eur J Endocrinol 163:233–242
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Erem C, Kocak M, Nuhoglu I, Yilmaz M, Ucuncu O (2009) Blood coagulation, fibrinolysis and lipid profile in patients with prolactinoma. Clin Endocrinol (Oxf) Dec 18. [Epub ahead of print]
Pijl H, Ohashi S, Matsuda M, Miyazaki Y, Mahankali A, Kumar V, Pipek R, Iozzo P, Lancaster JL, Cincotta AH, DeFronzo RA (2000) Bromocriptine: a novel approach to the treatment of type 2 diabetes. Diabetes Care 23:1154–1161
Rudling M, Norstedt G, Olivecrona H, Reihner E, Gustafsson JA, Angelin B (1992) Importance of growth hormone for the induction of hepatic low density lipoprotein receptors. Proc Natl Acad Sci USA 89:6983–6987
Dos Santos Silva CM, Barbosa FR, Lima GA, Warszawski L, Fontes R, Domingues RC, Gadelha MR (2010) BMI and metabolic profile in patients with prolactinoma before and after treatment with dopamine agonists. Obesity (Silver Spring) 17(9):1783–1788
Nilsson L, Binart N, Bohlooly YM, Bramnert M, Egecioglu E, Kindblom J, Kelly PA, Kopchick JJ, Ormandy CJ, Ling C, Billig H (2005) Prolactin and growth hormone regulate adiponectin secretion and receptor expression in adipose tissue. Biochem Biophys Res Commun 331:1120–1126
Brandebourg T, Hugo E, Ben-Jonathan N (2007) Adipocyte prolactin: regulation of release and putative functions. Diabetes Obes Metab 9:464–476
Kotronen A, Lewitt M, Hall K, Brismar K, Yki-Jarvinen H (2008) Insulin-like growth factor binding protein 1 as a novel specific marker of hepatic insulin sensitivity. J Clin Endocrinol Metab 93:4867–4872
Acknowledgments
We gratefully acknowledge RNs Ulrika Sjöstedt, Anette Härström, Agneta Hilding, Christina Häll and Lotta Larsson for taking excellent care of the patients and Inga-Lena Wivall-Helleryd for skilful technical assistance. This work was supported by grants from the Swedish Society of Medicine (2007-19869), Elin Danielsson foundation and Bert von Kantzows foundation.
Conflict of interest
The authors have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berinder, K., Nyström, T., Höybye, C. et al. Insulin sensitivity and lipid profile in prolactinoma patients before and after normalization of prolactin by dopamine agonist therapy. Pituitary 14, 199–207 (2011). https://doi.org/10.1007/s11102-010-0277-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-010-0277-9