Abstract
In recent years, increased longevity of the Danish population has resulted in a growing segment with age-related and chronic health conditions. This, together with a general increase in the demand on the services of doctors, has augmented the role of pharmacies in the provision of healthcare services. In Denmark, a variety of pharmacy services has been developed, evaluated and implemented since the introduction of pharmaceutical care. The services are aimed at the person responsible for administering the medicine e.g. the patient themselves or care workers, thereby supporting medication safety. The services available have been developed, evaluated and implemented in collaboration between community pharmacies, the Danish Association of Pharmacies, the Danish College of Pharmacy Practice and international collaborators. In this commentary we present an overview of the available pharmacy service, the contents of each service, remuneration and the scientific evidence behind each service. The commentary covers: Inhaler Technique Assessment Service; New Medicines Service; Medication Review; and Medication Safety in Residential Facilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
In Denmark, pharmacy services are standardised and available from all pharmacies throughout the country. This ensures consistency and supports medication safety.
-
To further support pharmacy practice, manuals and supporting materials are made available by the Danish Association of Pharmacies in Denmark. Overall, this means that pharmacies around Denmark can provide the same services at consistent standards.
Introduction
Pharmaceutical Care, as defined by Hepler and Strand in 1990, has formed the foundation for professional services available at Danish community pharmacies. Today, patients without an appointment can walk into their local community pharmacy and receive counselling on safe and effective use of medication by a trained pharmacist or pharmacy technician [1].
In Denmark, 484 community pharmacies have a monopoly of practice and serve a population of 5.75 million people. The location and distribution of community pharmacies are state-regulated, securing extensive public accessibility with 80.7% of people living within five kilometres of a community pharmacy [2]. Staff at the pharmacy consist of pharmacists with a 5-year MSc-degree in pharmacy and Pharmacy technicians holding a three and a half-year Academy Profession degree. Pharmacists, like other healthcare professionals, have electronic access to patients prescribed medication through the Shared Medication Record. The level of trust between pharmacy staff and patients is high, with 83% of patients reporting satisfaction with advice and counselling [3]. Professional pharmacy services available have increased since the millennium and today include: smoking cessation, home delivery, automated dose dispensing, flu vaccination service, medication review, New Medicine Service (two different services) and Inhaler Technique Assessment Service—with only the two latter being remunerated by the government.
Aim
The aim of this commentary is to summarise the last 25 years’ research in pharmaceutical care in Denmark. This is done by reviewing the literature describing research and development behind some of the current pharmacy service programmes where the benefit for the patients’ safe and effective use of medicine has been considered greatest versus considerable barriers to implementation, i.e. resource use; Inhaler Technique Assessment Service, New Medicines Service, Medication Review and a programme to build medication safety in residential facilities.
Inhaler Technique Assessment Service (ITAS)
The current service is available to new or experienced patients using any kind of inhalation device. Since 2005 the pharmacies have been remunerated by the government for this service. The service, delivered by either a pharmacist or pharmacy technician, assesses the patient’s inhalation technique by demonstration and teach-back. The service is scheduled to take 10 min and aims to optimise the patient’s outcome of the treatment.
The development of ITAS was based on results from the programme, Therapeutic Outcomes Monitoring (TOM) [4]. The 1-year programme was established to improve drug therapy for asthma patients and developed by researchers from several countries through the Pharmaceutical Care Network Europe (PCNE) [5]. The programme involved the patients paying monthly visits to their community pharmacy where they received individual counselling on adherence, inhalation technique, therapeutic problems and coping with the disease and treatment [6, 7]. The pharmacist recorded the patient’s inhalation technique, peak expiratory flow rate and asthma symptoms. The patient kept a diary, which was monitored by the pharmacist along with discussion of daily experiences and challenges with the disease and possible solutions. Pharmacies are obliged to provide this service.
Effectiveness of the service
In Denmark the programme was evaluated in a prospective controlled multicentre trial involving 500 adult patients (264 intervention patients and 236 control patients) and 31 pharmacies [6, 7]. For the intervention group, significant effects were found in asthma symptom status, overall health related quality of life (HRQoL) and asthma-related quality of life. There was a 23% improvement in asthma symptom status for intervention patients after twelve months compared with 10% for the control group. The study also showed positive, although not significant, effects on knowledge of asthma and medication, number of reported sick days, number of inhalation errors, drug use and number of drug therapy problems. During the study period, the drug therapy regimens changed towards consensus guidelines for the intervention group. The study demonstrated that an asthma service delivered by the community pharmacy is an effective strategy for improving the quality of drug therapy for asthma patients. Two evaluations on the use of ITAS implementation were performed. A mystery customer evaluation showed that pharmacies provided ITAS for 81% of patients using inhalation devices based on 1579 visits to 320 pharmacies [8]. Furthermore, data from three pharmacies and 95 patients showed that 60% of patients demonstrated suboptimal use of their inhalation device [9]. The effect of ITAS has been investigated in a Norwegian setting where an identical service is available. The evaluation included 405 patients and showed that the percentage of patients demonstrating an optimal inhalation technique increased from 8% at baseline to 52% when measured again after three months [10].
To secure uniformity and quality of the service, the Association of Danish Pharmacies has since created an individual mandatory certification programme.
Safe and effective use of medicines
Research on safe and effective use of medicines in Denmark has been performed since 2004 developing and testing a comprehensive adherence programme. The results from the programme have been part of the foundation for both New Medicines Services and Medication Review. The background and contents of Safe and Effective Use of Medicine has been described elsewhere [11], but in brief, consisted of four sessions with the patient at the community pharmacy over a period of up to 1 year. The patient received either a basic service or an extended service. Both services identified drug-related problems and, in collaboration with the patient, found individualised solutions to low adherence, lack of knowledge or other identified problems related to the patient’s medicine. The extended service was more time-consuming and elaborate, comprising a Medicine Use Review, clinical measurements, patient narratives and motivational interviewing.
Effectiveness of the service
The programme was evaluated in two randomised clinical trials targeting patients with type 2 diabetes and patients with hypertension [12, 13]. The study for type 2 diabetes included five pharmacies and 205 adult type 2 diabetes patients (39 basic intervention patients, 41 extended intervention patients and 125 control patients) using oral antidiabetic medicines and managed their medication themselves.
The intervention group testing the extended service reported significantly higher improvements for outcome measures in patient health, well-being, knowledge and satisfaction [13]. The study targeting hypertensive patients included five pharmacies and 563 adult hypertensive patients (120 basic intervention patients, 120 extended intervention patients and 323 control patients). For both the basic and extended intervention the number of patients with blood pressure exceeding recommended by clinical guidelines was reduced by more than 50% [12].
The programme was adjusted further and evaluated in two different settings. The first study was designed for adult hypertensive patients with specific focus on the patient’s adherence to treatment [14]. The study was designed as a formative evaluation and was a collaboration between The Danish Heart Foundation and 26 community pharmacies and included 290 adult heart patients. Recruited patients received a medication review with focus on adherence and a follow-up by phone 4–6 weeks after the initial session. The study showed that patients receiving the intervention obtained more knowledge about how to take their medication and improved their adherence. For patients experiencing side effects of medication, adherence improved significantly. Another important finding from this study was the recommendation that future studies should implement screening of patients to ensure those in most need received the service. Finally, the experience and knowledge from Safe and Effective use of Medicine was adapted to design a study targeting ethnic minorities [15]. The study was designed as a before and after evaluation and involved four municipalities and five community pharmacies. A total of 82 unemployed patients of non-western origin receiving social benefits was recruited. The patients received a medication review, patient education and follow-up for a total of four sessions. The results showed that several levels of adherence improved significantly over the course of the study (Intentional, self-regulation, unintentional and intentional, effect-related).
New medicines services
The New Medicines Service consists of two services. The services were founded on the experience from the comprehensive compliance programme Safe and Effective Use of Medicine. The first service, Adherence Service for New Medicine Users, was included in the counselling guidelines for Danish community pharmacies in January 2016. The service is aimed at patients diagnosed with a new chronic condition having started new medication within the last six months. The service is provided by pharmacists and consist of a counselling session and a follow-up by phone 2–4 weeks after the initial session. The counselling focuses on the patient’s new medicine and how the pharmacy can support the patient’s own medicine management by providing knowledge about the treatment, disease and thereby boost adherence. The second service, Adherence Service for Patients with Chronic Conditions With Signs of Low Adherence, launched in April 2018, is similar in structure to the first, the only difference being that the service is only available for patients who already have been in long-term treatment for more than 1 year and show signs of low adherence. Both services are remunerated by the government and both services have a combined length of 20 min. Pharmacies are obliged to provide these services.
Effectiveness of the service
The service for newly diagnosed patients was evaluated by endpoint questionnaires (n = 56 patients) and semi-structured interviews (n = 6) [16]. Approximately 85% of patients who responded reported being satisfied with the programme. The programme helped patients start well using their new medicine; increased their knowledge of the effects; educated them on correct use of the medication; gave them a feeling of safety and helped develop good medication intake habits.
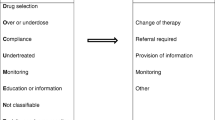
Medication review
The current Medication Review pharmacy service was launched in 2005 and is offered at the community pharmacy or as part of a clinical service to nursing homes or other residential facilities. The review is carried out by a pharmacist in collaboration with the patient or nursing staff. Data is sourced from the patient’s digital list of prescribed medication with all other data collected from the patient or carer such as actual drug use, over-the-counter drugs, vitamins and minerals and results from blood tests etc. Focus of the review is to optimise the patient’s medical treatment by identifying and solving drug related problems. Suggestions are summarised in agreement with the patient and communicated to the patient’s general practitioner, preferably by the patient. The service is estimated to last 75 min. If relevant, a follow-up of the review can be offered. The Medication Review pharmacy service is not remunerated, and pharmacies are not obliged to provide this service. However, in recent years more pharmacies throughout Denmark have established contractual agreements with municipalities to deliver medication reviews at e.g. nursing homes. To support and secure the uniformity and quality of the service, the Association of Danish Pharmacies has since created an individual mandatory certification programme.
The background for the current medication review service is founded on data and experience from several programmes; The Therapeutic Outcome Monitoring programme, Safe and Effective Use of Medicines, and the Pharmaceutical Care model [5,6,7, 10, 12,13,14].
Effectiveness of the service
A medication review was part of the Therapeutic Outcome Monitoring (TOM) programme [5, 6] and the comprehensive compliance programme Safe and Effective use of Medicines [7, 10]. In the TOM project there was a sharp decline in the number of DRPs [5]. In the Safe and Effective Use of Medicines for ethnic minorities study, there was an 8.4% decrease in the number of patients with potential adherence problems [10]. Also, a large multi-centre study was carried out in seven European countries testing the pharmaceutical care model on elderly patients [17]. The study included 190 community pharmacies and 2454 home-dwelling patients (1290 intervention patients and 1164 control patients) over 65 years of age using at least four prescription medicines. The study found no overall significant differences between intervention and control groups for HRQoL or hospitalisations, but patients’ satisfaction with the service in general was significantly increased over time when compared with the start of the study and the control group. However, the Danish contribution to the study based on data from 28 community pharmacies and 523 patients (254 intervention patients and 269 control patients) reported a significant improvement for two domains of the HRQoL and a significant reduction in hospitalisation [17]. Another study, based on patient data from the large European multi-centre study, analysed the impact of the pharmaceutical care model on drug-drug interactions in elderly [18]. Data from six countries and 1601 elderly patients was included. The study identified 1324 potential drug-drug interactions corresponding to 0.83 interactions per patient.
Building capacity on medication-safety at residential facilities
An educational programme service for staff at residential care facilities to ensure medication safety has been available since 2005 [19]. The programme is delivered by a pharmacist or pharmacist technician at the local community pharmacy and is tailored for the specific needs of the residential facility. The programme can cover three main areas; disease and medicines; quality, safety, communication and coordination; and skills, knowledge and competencies according to the national qualification framework for lifelong learning.
The educational programme was developed through a task-and-learning analysis based on official guidelines and interviews with management and staff from residential facilities. The programme consists of a seven-day basic programme for all participants and an additional 2 days for participants whose responsibilities related especially to medicines. The delivery and cost are agreed between the pharmacy and the residential facility.
Effectiveness of the service
The educational programme was evaluated using a quantitative baseline and endpoint evaluation based on data from 75 participants from 14 residential facilities representing five different, rural and urban municipalities [20]. They were interviewed about their knowledge, skills and competence regarding medicines and perceived need of further training. Most of the respondents were social workers (48%) with an average work experience in residential facilities of 10.2 years. Positive effects were reported for improvements in staff motivation and confidence, perceived ability to safely handle residents’ medication, safety culture, patient empowerment and communication skills.
A qualitative study based on ten semi-structured interviews with residential care facility staff members, five semi-structured interviews with residential care facility managers and five open-ended questionnaires with community pharmacists was carried out to explore the experiences of the staff, managers and community pharmacists [21]. The analysis showed that community pharmacists provide a resource to engage in educational programmes. As educators, the community pharmacists were successful in their role as experts in medicine. After the project, improved collaboration was reported between the residential facilities and their local community pharmacy.
Discussion
The pharmacy services described in this commentary have all been founded on scientific evidence. Research programmes have been conducted in collaboration between Danish community pharmacies, the Association of Danish Pharmacies, The Danish College of Pharmacy Practice and international collaborators such as Pharmaceutical Care Network Europe. Barriers and facilitators for implementation of pharmacy services have been identified and linked primarily to financial constraint [22]. Remunerated services have a high degree of uptake as pharmacies are obliged to provide the services. Medication Review and Educational Programme to Build Capacity on Medication-Safety at Residential Facilities are not remunerated, and pharmacies are not obliged to provide the service, with uptake dependent on local agreements.
For all services, manuals and supporting materials are made available by the Danish Association of Pharmacies.
In an international context, when compared to data from the International Pharmaceutical Federation and the Pharmaceutical Group of the European Union, pharmacy services available from Danish community pharmacies resemble services available in Western Europe and North America. Three services are remunerated by the government; Inhalation Technique Assessment service and the two New Medicines Services. More recently, pharmacies have been obliged to make repeat dispensing for a limited number of medications available since July 2019, the service being remunerated partly by the government and partly by third party payment from the patient.
Future needs for pharmacies could include more active involvement in identifying inappropriate drug use and facilitation of deprescribing. Also, communication with patients is generally taking place at the pharmacy, whereas study of the use of virtual communication could lead to new and better ways to reach patient groups that rarely visit the pharmacy.
Overall, for pharmacies to fulfil the full potential of providing pharmaceutical care, stronger bonds must be established between pharmacies and other healthcare professionals, from general practices and hospitals to nursing homes and elderly care. This will enable the pharmacy to follow and help patients navigate an otherwise complex healthcare system.
Conclusion
This commentary has demonstrated that Danish community pharmacies can deliver professional services that help support medication safety and prevent disease through implementation of the intended and rational use of medicines. The development of professional pharmacy services in Denmark has been built upon scientific evidence, ensuring that the benefits intended for patients and society are realised. The community pharmacies, as part of the healthcare system, play a key role in delivering professional pharmacy services and secures this support for patients through wide availability of counselling services.
References
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43.
The Association of Danish Pharmacies. Øget geografisk tilgængelighed til apoteket. 2018. https://www.apotekerforeningen.dk/-/media/apotekerforeningen/analysertilgaengelighed/19-12-2018-konkurrence-ventetid-aabningstid-tilgaengelighed.pdf. Accessed 3 Oct 2019.
The Association of Danish Pharmacies. Høj tilfredshed med apotekernes tilgængelighed og rådgivning. 2014. https://www.apotekerforeningen.dk/nyheder/nyhedsbreve/2014/09042014_hoj_tilfredshed_raadgivning. Accessed 28 Sept 2019.
Grainger-Rousseau T-J, Miralles MA, Hepler CD, Segal R, Doty RE, Ben-Joseph R. Therapeutic outcomes monitoring: application of pharmaceutical care guidelines to community pharmacy. J Am Pharm Assoc. 1997;37(6):647–61.
Pharmaceutical Care Network Europe (PCNE). Pharmaceutical Care Network Europe. www.pcne.org. Accessed 28 Sep 2019.
Herborg H, Soendergaard B, Froekjaer B, Fonnesbaek L, Jorgensen L, Hepler CD, et al. Improving drug therapy for patients with asthma–part 1: patient outcomes. J Am Pharm Assoc (Wash). 2001;41(4):539–50.
Herborg H, Soendergaard B, Jorgensen T, Fonnesbaek L, Hepler CD, Holst H, et al. Improving drug therapy for patients with asthma-part 2: use of antiasthma medications. J Am Pharm Assoc (Wash). 2001;41(4):551–9.
Fonnesbæk L, Bolvig T, Gustafsen I. Tjek på inhalation-landsdækkende pseudokunmdeundersøgelse [In Danish]. Pharmakon, Danish College of Pharmacy Practice. 2007.
Klinke B, Fonnesbæk L. Tjek på inhalation-afprøvning af ydelsen [Inhaler technique service–testing the service. Evaluation report. In Danish]. Evalueringsrapport Danmarks Farmaceutiske Universitet og Pharmakon. 2005.
Ruud KW, Ronningen SW, Faksvag PK, Ariansen H, Hovland R. Evaluation of a structured pharmacist-led inhalation technique assessment service for patients with asthma and COPD in Norwegian pharmacies. Patient Educ Couns. 2018;101(10):1828–37.
Herborg H, Haugbølle LS, Sørensen L, Rossing C, Dam P. Developing a generic, individualised adherence programme for chronic medication users. Pharm Pract (Internet). 2008;6(3):148–57.
Dam P, Herborg H, Rossing C, Sørensen L. Sikker og effektiv medicinbrug for brugere af blodtryksmedicin [In Danish]. Pharmakon, Danish College of Pharmacy Practice. 2007.
Kjeldsen LJ, Bjerrum L, Dam P, Larsen BO, Rossing C, Sondergaard B, et al. Safe and effective use of medicines for patients with type 2 diabetes—a randomized controlled trial of two interventions delivered by local pharmacies. Res Soc Adm Pharm: RSAP. 2015;11(1):47–62.
Rossing C, Agergaard M, El-Souri M, Pultz K. Evaluering af Medicingennemgang med compliancerettet rådgivning—en rådgivningsydelse til hjertepatienter [In Danish]. Pharmakon, Danish College of Pharmacy Practice. 2010.
Dam P, El-Souri M, Herborg H, Nørgaard LS, Rossing C, Sodemann M, et al. Safe and effective use of medicines for ethnic minorities–a pharmacist-delivered counseling program that improves adherence. J Pharma Care Health Syst. 2015;2(128):2376.
Kaae S, Dam P, Rossing C. Evaluation of a pharmacy service helping patients to get a good start in taking their new medications for chronic diseases. Res Soc Adm Pharm. 2016;12(3):486–95.
Bernsten C, Bjorkman I, Caramona M, Crealey G, Frokjaer B, Grundberger E, et al. Improving the well-being of elderly patients via community pharmacy-based provision of pharmaceutical care: a multicentre study in seven European countries. Drugs Aging. 2001;18(1):63–77.
Björkman IK, Fastbom J, Schmidt IK, Bernsten CB. Drug–Drug Interactions in the Elderly. Ann Pharmacother. 2002;36(11):1675–81.
Danish Evaluation Institute. Referencing the Danish qualifications framework for lifelong learning to the European qualifications framework. Copenhagen: Danish Agency for Universities and Internationalisation; 2011.
Mygind A, El-Souri M, Rossing C, Thomsen LA. Development and perceived effects of an educational programme on quality and safety in medication handling in residential facilities. Int J Pharm Pract. 2018;26(2):165–73.
Mygind A, El-Souri M, Pultz K, Rossing C, Thomsen LA. Community pharmacists as educators in Danish residential facilities: a qualitative study. Int J Pharm Pract. 2017;25(4):282–91.
Rossing C, Hansen E, Krass I. Barriers and facilitators in pharmaceutical care: perceptions and experiences among Danish community pharmacists. J Soc Adm Pharm. 2002;19(2):55–64.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abrahamsen, B., Burghle, A.H. & Rossing, C. Pharmaceutical care services available in Danish community pharmacies. Int J Clin Pharm 42, 315–320 (2020). https://doi.org/10.1007/s11096-020-00985-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-00985-7