Abstract
Background Adherence to treatment is important to achieve target outcomes, particularly for those with type 2 diabetes. Pharmacists are well placed to enhance adherence, however evidence of the impact on clinical outcomes is not well known. Objective To determine the impact of an adherence support service on adherence scores and subsequent clinical biomarkers (HbA1c). Setting Community pharmacies providing a Medicines Use Review (MUR) Service in a New Zealand locality. Methods Records of patients receiving MURs between 2007 and 2012 were obtained from a single locality. Data extraction included: individual characteristics, the adherence score assigned at every consultation, pathology records. Patients receiving oral hypoglycaemic medications (n = 86) were included in the final analysis using generalised estimating equations to explore change in HbA1c over time, and whether this was related to the adherence score. Main Outcome Measures (a) change in adherence scores and (b) association between adherence sores and HbA1c. Results A total of 350 records were obtained, of those, 115 of 350 people had follow up MUR visit/s and could be analysed for changes in adherence. Most people (110/115) showed sustained or improved adherence scores with follow up visits. For those receiving oral hypoglycaemic medications (n = 86); where poor adherence scores were recorded, their HbA1c levels were higher and continued to increase by ~ 0.1% (1 mmol/mol) every 10 weeks, B = 0.11, p = 0.009. Conversely, those with high adherence scores showed an overall decrease in HbA1c levels. Conclusion MURs may positively influence medication adherence. This improved adherence shows a measurable decline in HbA1c levels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impacts on practice
-
In real world settings, pharmacist-led adherence support services can improve adherence scores for patients that remain in the programme.
-
The lack of adequate HbA1c testing (particularly sporadic in some people) may influence treatment or outcomes.
-
Increasing pharmacist access to patient laboratory results could allow more collaborative care to ensure regular testing is done to monitor treatment success.
Introduction
Improving adherence to appropriately prescribed medications enhances clinical outcomes [1, 2]. For this reason, many countries have implemented adherence support programmes to provide tailored, individualised strategies to help people improve adherence to medications [3]. Pharmacists have been at the centre of these programmes and work either with people alone or as part of a wider healthcare team, particularly liaising with general practitioners [4].
One widely implemented class of strategy involving pharmacists comprises a structured interview with a person to identify current adherence and identify individualised solutions to improve adherence. These pharmacist-led medication review programmes have different names depending on the country, however, the general format remains consistent. Examples include: Medication Therapy Management (MTM, United States of America), MedsCheck (Canada), Medicines Use Review, (MUR, United Kingdom) and Home Medication Review (HMR, Australia) [5,6,7,8]. These are more extensive interventions and can be conducted at various settings (i.e. patient homes, community pharmacy and via telephone). Within New Zealand (NZ), this service is called a Medication Use Review and Adherence Support Service (MUR). It aims to improve people’s understanding of and adherence to medicines; identifying and addressing factors linked to non-adherence behaviours, as well as minimising pharmaceutical waste [9]. This service is funded in some District Health Boards (DHBs) for patients that meet specific criteria, these criteria include: polypharmacy, multimorbidity, and other patient factors that would indicate that they would benefit from this intervention. Patients can self-refer, but the majority are referred from their general practitioner or practice nurse [10]. Accredited MUR pharmacists meet with patients face-to-face initially and determine a medication adherence “score” based on the framework adopted by the DHB funders. This score is measured on a scale of 1–4 (Question asked—How often do you miss a dose of this medication? 1—Always, 2—Often, 3—Seldom and 4—Never). Tailored adherence interventions are determined and health literacy regarding medications and medical conditions is enhanced through dialogue.
There have been several studies that have investigated the perceptions of those receiving these services and the wider health care team [11]. A previously published meta-analyses of pharmacist-led fee-for services medication reviews showed positive benefits in clinical outcomes including blood pressure and lipid levels [12]. It is often difficult to determine the direct benefits of adherence interventions in clinical outcomes as there can be a long period of time before therapeutic benefits are realised. Additionally, the benefits may be proportional to the degree of initial non-adherence and so gains may be at an individual level and harder to determine at a population level [13]. However, it may be possible to use a surrogate marker for improved outcomes, such a clinical biomarker, to determine whether improved adherence will have an improved clinical outcome.
Type 2 diabetes mellitus is a condition of growing international concern. The mainstay therapy for people with type 2 diabetes mellitus is oral hypoglycaemic medications. However, people often have suboptimal adherence to these medications. One study conducted in the US found that within 12 months of treatment initiation, 37% of people with type 2 diabetes mellitus discontinued using their oral hypoglycaemic agents [14]. In Europe, the CODE-2 study revealed that good glycaemic control was seen with only 28% of people with diabetes treated with hypoglycaemic agents [15]. This lack of adherence to oral hypoglycaemic medications has led to an estimated 1 billion US dollar rise in medical expenses due to poor glycaemic control [16, 17]. One study estimated that each 10% increase in adherence could reduce the total annual diabetes care cost by 8.6 to 28.9% [18].
HbA1c is a principal biomarker for glycaemic control in diabetes and can be used to monitor the management and glycaemic control of type 2 diabetes mellitus over time. HbA1c levels elevated by 1% (11 mmol/mol) may trigger a 10 to 20% rise in the magnitude of cardiovascular risk in people with diabetes [19]. The United Kingdom Prospective Diabetes Study has established that decreasing HbA1c is associated with decreased cardiovascular complications and lower mortality rates over time [20, 21]. Changes in HbA1c measurement can be used to determine the impact of adherence interventions in the people with type 2 diabetes mellitus as blood HbA1c levels reflect mean glycaemic control of the preceding 2–3 months [22]. The New Zealand Society for the Study of Diabetes not only recommends the use of HbA1c for the diagnosis of type 2 diabetes mellitus but also suggests 3-monthly follow up HbA1c testing to avoid/manage complications of diabetes [23]. HbA1c testing is recommended every 3 months in people with diabetes and twice yearly for people responding positively to the oral hypoglycaemic medication [24]. HbA1c targets differ for diagnosis and treatment of diabetes. During diagnostic screening HbA1c above 50 mmol/mol confirms the diabetes where as for the treatment of confirmed diabetes the HbA1c in range of 50–54 mmol/mol reflects very good glycaemic control, 55–64 mmol/mol is acceptable and above 65 mmol/mol falls into suboptimal control demanding for intensive therapy [25].
Some published clinical studies have supported the impact of pharmacist-led interventions on medication adherence [26, 27] and HbA1c levels [28, 29] in people with type 2 diabetes mellitus. However, again these were conducted under trial conditions. To our knowledge, there is scarce literature on the implementation and outcomes of an adherence support service when provided as “routine” or real world care. Therefore, the aim of this study is to retrospectively examine MUR records of the consultations provided in a single locality in New Zealand to determine if adherence support services provided as part of routine practice influence adherence and clinical outcomes, specifically HbA1c levels.
Aim of the study
The aim of this study is to retrospectively examine the MUR records of people receiving MURs as part of routine care to determine (a) if the MUR consultations resulted in a change in adherence scores, and (b) the association between adherence scores and HbA1c for those people taking oral hypoglycaemic medications.
Ethics approval
Ethical approval was obtained from the New Zealand Health and Disability Ethics Committee, (NXT/11/EXP/182).
Methods
Data collection
New Zealand is divided into 20 District Health Boards (DHBs), and while many core health services are funded at a national level, some services such as a pharmacist-led Medicines Use Review and Adherence Support Service (MUR) are funded only within specific DHBs. This study was conducted in one specific DHB that had a population of 226,530 people and funded the MUR service. As part of the MUR service, all consultations are documented and people sign a consent form to receive this service and for their records to be used in research to inform the evaluation of the service.
Following ethical approval, the pharmacies that provide this service were invited to participate in this study and those that chose to participate allowed the researchers’ access to all of the consultation files from 1 November 2007 to 31 Dec 2011. A total of 350 records were obtained from the MUR providers. Subsequent data extraction included demographic details: age, gender, ethnicity, MUR visits, and medication prescribed. Adherence scores were also extracted from the records, measured on the scale of 1–4 (Question asked—How often do you miss a dose of this medication? 1—Always, 2—Often, 3—Seldom and 4—Never). MUR providers have adopted this scoring system which was originally developed by the service’s funders. The diabetes biomarker data was collected separately from pathology records not available to the pharmacists.
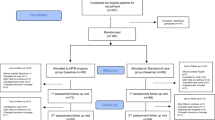
The MUR and pathology data were merged to allow longitudinal tracking of individuals. The first MUR visit date was considered as reference and the final analysis was for a time period of ± 52 weeks from first MUR. As MUR services are provided to people with any chronic conditions, each person’s records were scrutinized to determine whether that had sufficient documentation to determine that they had type 2 diabetes mellitus and that they had complete data for analysis. This process is shown in Fig. 1 and indicates that 88 people had type 2 diabetes mellitus, of which 86 people were included in the final analysis.
Data analysis
Data were analysed descriptively with Microsoft Excel and inferentially using IBM SPSS Statistics version 23. This study used two different approaches for data analysis to address the two aims. First, to determine the impact of follow-up visits on the adherence scores the first MUR visit date was considered as reference and follow-up visit adherence scores were compared with that of the first one (115/350 records). Secondly, generalised estimating equations (GEEs) were used to explore change in HbA1c over time, and whether this was related to the adherence score given by the pharmacist in the first MUR (88/350 records). GEEs are a generalised linear model (similar to ANOVA and mixed models), but are particularly robust in situations where the number of measurements per participant, and the timing of these measurements, are not standard [30], in this case the timing of the HbA1c measurements. HbA1c was the dependent variable, with observations nested within persons (which served as a random factor). Adherence was scored so that 4 (complete adherence) was the reference level, with contrasts for 3, as well as 2 and 1 combined (there were only two people estimated as having level 1 adherence). Adherence was a fixed factor, and the time of the HbA1c testing was included as a continuous covariate. An autoregressive (AR1) covariance structure was used to model the relationship between successive HbA1c scores within each person.
To determine the pattern of HbA1c testing frequency and the adherence to the testing guidelines, the number of HbA1c tests for a person was calculated for each year. These were then grouped according to whether they matched the guidelines every year of testing (i.e. tested every 3 months), where none of the years had sufficient testing, or “mixed” where some years adequate testing was done.
Results
Only 115 out of 350 people had follow up MUR visits. Table 1 summarises the changes in MUR adherence scores as compared to first MUR visit. 27 (71%) people collectively with MUR scores 1 & 2 showed improvement in follow up MUR visit scores when compared with their first visit score. 63 (82%) people collectively with MUR scores 3 & 4 sustained their first visit score over follow up visits and 9 (18%) people with MUR score 3 improved to MUR score 4.
There were 88 people who met the inclusion criteria with type 2 diabetes mellitus, who had HbA1c, adherence score & prescribed oral hypoglycaemic medication(s). Those 88 people ranged in age from 25 to 94, consisted of 50 female and 38 male patients, 46 people were of Māori descent and the remainder were of European descent. Only 86 people had pathology results available for the duration of ± 52 weeks from their first MUR consultation. The people with the lowest MUR adherence score (1 & 2 combined) had average HbA1c levels over ~ 1% (11 mmol/mol) higher than those with MUR score 4 (the reference category), B = 10.5, p = 0.014, but there was no difference between people with MUR score 3 & MUR score 4, B = 0.7, p = 0.8. There was a marginal trend for a slight decrease with time of HbA1c levels, B = −0.04, p = 0.08, but this was qualified by an interaction between adherence level and time. Specifically, as Fig. 2 shows the people with lowest MUR adherence scores (1 & 2 combined) had HbA1c scores that increased by ~ 0.1% (1 mmol/mol) every 10 weeks, B = 0.11, p = 0.009. In contrast, people with MUR score 3 and MUR score 4 trend down over time, but those with MUR score (1 & 2) start high and continue trending up with time.
Of the 88 people that had laboratory data, 41 did not receive adequate monitoring (HbA1c measured every 12 weeks), 40 had mixed monitoring where some years had adequate monitoring and other years had reduced monitoring, and only 7 received the level of monitoring recommended in the guidelines. During the course of this study, we found 27 people of the original 350 that had elevated HbA1c levels in their pathology data, but no oral hypoglycaemic agent prescribed during the period in which data was available.
Discussion
Most people that had a low adherence score at their first MUR visit showed an improvement in their adherence scores after subsequent follow up visits. This may indicate that MUR can enhance medication adherence. However, given that only 115 of the original 350 people had a follow up visit this needs to be further studied. Particularly, the identification of the reasons for non-follow up for the majority of people.
An important finding of this study is that, those people with high adherence (MUR score 3/4) had decreasing HbA1c levels which fell within the defined acceptable range [25]. Conversely, those people who had poor adherence (MUR score 1/2) continued to show an increase in HbA1c level with time. This indicates the potential impact of increased adherence on disease progression and further the potential of this type of service in improving adherence and subsequently HbA1c. As discussed in the introduction many countries are recognising the importance of improving medication adherence and have initiated services to improve adherence. These services have had a very little evaluation of their impact in a real world population. However, it has been noted in other studies that targeted education to people regarding their diabetes has shown a direct impact in improving HbA1c [31]. One aspect of the MUR consultation is indeed education and so this aligns with others findings. Further, other studies have also indicated the importance and impact of a comprehensive care package for people with diabetes and that targeted care will enhance achievement of glycaemic targets [32, 33].
At the time these MUR consultations were conducted the pharmacist had no access to any pathology data. Recently, within New Zealand, there has been a change in the sharing of health information held by individuals. This has increased the access that pharmacists have to laboratory results for people under their care [34]. Laboratory data/medical records shared with pharmacist may be advantageous to improve safety and avoid medication errors [35,36,37,38,39]. This may allow the pharmacist to speak with the people directly about the importance of monitoring treatment efficacy or via the prescriber in a more collaborative care model. This is important as often prescribers may be unaware of non-adherence and people may not feel comfortable disclosing it [40]. A closer working relationship between pharmacists and prescribers will have positive outcomes for people with diabetes and multimorbidity [41, 42].
One surprising finding was the identification of a group of people who had significantly elevated HbA1c levels and no treatment with oral hypoglycaemic initiated during the period of this study. Again a multidisciplinary approach and shared records which include prescribing, dispensing and laboratory results may allow closer monitoring. In this study very few people received testing as frequently as suggested in the guidelines.
This is an area worthy of further investigation as to whether the prescribers are not requesting the tests, or whether people are not actioning the requests.
There are some limitations to this study. As the study relied on secondary data, not all information was available for all people. This also means that only people that were offered and accepted an MUR were included in this study. The adherence score given by the pharmacist is a non-validated tool and provides only an “estimation” of the individuals’ adherence as judged by the pharmacist conducting the MUR. The influence of MUR on change in adherence score could only be shown in 115/350 patients which limits the interpretation. As mentioned above, there needs to be further research into why the remainder of patients did not have follow up visits. This study found that there was sporadic and less than recommended testing of HbA1c, this also is an area for further research. It is important to note in this piece of work that the pharmacists conducting the MUR services did not have access to people’s pathology results and therefore are unaware which people they are working with are achieving reductions in their HbA1c levels. Further, they are unable to recommend treatment initiation for people with elevated laboratory results because they are not aware that HbA1c is elevated.
This study has investigated the impact of a structured adherence service when offered in a “real life” setting and indicates that for those patients who have follow-up visits, adherence may be improved. Importantly the impact of this adherence on clinical outcomes such as HbA1c has been shown.
Conclusion
Pharmacists performing an adherence support service may positively influence medication adherence. Patients with high adherence scores show a decline in measured HbA1c; conversely the people who are poorly adherent, have an increasing HbA1c.
References
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14.
Sabate E, editor. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organization. 2003. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1. Accessed 02 Nov 2017.
Ganguli A, Clewell J, Shillingto AC. The impact of patient support programs on adherence, clinical, humanistic, and economic patient outcomes: a targeted systematic review. Patient Prefer Adherence. 2016;10:711–25.
Tan EC, Stewart K, Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm. 2014;10(4):608–22.
Clyne W, Blenkinsopp A, Seal R. A guide to medication review. 2008. http://www.sefap.org/media/upload/arxius/formacion/aula_fap_2010/bibliografia/guide_medication_review_2008.pdf. Accessed 02 Nov 2017.
American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model. 2008. http://www.pharmacist.com/sites/default/files/files/core_elements_of_an_mtm_practice.pdf. Accessed 02 Nov 2017.
Ontario Ministry of Health and Long-Term Care. MedsCheck. 2011. http://www.health.gov.on.ca/en/pro/programs/drugs/medscheck/medscheck_original.aspx. Accessed 02 Nov 2017.
Pharmaceutical Society of Australia Ltd. Guidelines for pharmacists providing Home Medicines Review (HMR) services. https://www.psa.org.au/download/practice-guidelines/home-medicines-review-services.pdf. Accessed 02 Nov 2017.
Pharmaceutical Society of New Zealand Inc. New Zealand National Pharmacist Services Framework. 2014. https://www.psnz.org.nz/Folder?Action=View%20File&Folder_id=86&File=PSNZPharmacistServicesFramework2014FINAL.pdf. Accessed 02 Nov 2017.
Lee E, Braund R, Tordoff J. Examining the first year of medicines use review services provided by pharmacists in New Zealand: 2008. N Z Med J. 2009;22(1293):26–35.
Supper I, Catala O, Lustman M, Chemla C, Bourgueil Y, Letrilliart L. Interprofessional collaboration in primary health care: a review of facilitators and barriers perceived by involved actors. J Public Health (Oxf). 2015;37(4):716–27.
Hatah E, Braund R, Tordoff J, Duffull SB. A systematic review and meta-analysis of pharmacist-led fee-for-services medication review. Br J Clin Pharmacol. 2014;77(1):102–15.
Hugtenburg JG, Timmers L, Elders PJ, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Person Prefer Adherence. 2013;10(7):675–82.
Hertz RP, Unger AN, Lustik MB. Adherence with pharmacotherapy for type 2 diabetes: a retrospective cohort study of adults with employer-sponsored health insurance. Clin Ther. 2005;27(7):1064–73.
Liebl A, Neiss A, Spannheimer A, Reitberger U, Wieseler B, Stammer H, et al. Complications, co-morbidity, and blood glucose control in type 2 diabetes mellitus people in Germany—results from the CODE-2 study. Exp Clin Endocrinol Diabetes. 2002;110:10–6.
Egede LE, Gebregziabher M, Dismuke CE, Lynch CP, Axon RN, Zhao Y, et al. Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care. 2012;35(12):2533–9.
Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in people with diabetes. Diabetes Care. 2004;27(12):2800–5.
Balkrishnan R, Rajagopalan R, Camacho FT, Huston SA, Murray FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003;25(11):2958–71.
Khaw KT. Elevated HbA1c level: a risk factor for cardiovascular disease mortality in people with chronic heart failure? Nat Clin Pract Endocrinol Metab. 2009;5(3):130–1.
Chan WB, Tong PCY, Chow CC, So WY, Ng MCY, Ma RCW, et al. Triglyceride predicts cardiovascular mortality and its relationship with glycaemia and obesity in Chinese type 2 diabetic people. Diabetes Metab Res Rev. 2005;21(2):183–8.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in people with type 2 diabetes (UKPDS 33. Lancet. 1998;352(9131):837–53.
Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan DM, Peterson CM. Tests of glycemia in diabetes. Diabetes Care. 2004;27(1):S91–3.
New Zealand Society for the Study of Diabetes: NZSSD position statement on screening and type 2 diabetes. 2011. http://www.nzssd.org.nz/HbA1c/1.%20NZSSD%20position%20statement%20on%20screening%20for%20type%202%20diabetes%20final%20Sept%202011.pdf. Accessed 02 Nov 2017.
Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan DM, Peterson CM. Tests of glycemia in diabetes. Diabetes Care. 2004;27(7):1761–73.
Braatvedt GD, Cundy T, Crooke M, Florkowski C, Mann JI, Lunt H, Jackson R, Orr-Walker B, Kenealy T, Drury PL. Understanding the new HbA1c units for the diagnosis of Type 2 diabetes. N Z Med J. 2012;125(1362):70–80.
Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–9.
Ayadurai S, Hattingh HL, Tee LB, Md Said SN. A Narrative review of diabetes intervention studies to explore diabetes care opportunities for pharmacists. J Diabetes Res. 2016; Article Id 5897452:1–11.
Butt M, Mhd Ali A, Bakry MM, Mustafa N. Impact of a pharmacist led diabetes mellitus intervention on HbA1c, medication adherence and quality of life: a randomised controlled study. Saudi Pharm J. 2016;24(1):40–8.
Korcegez EI, Sancar M, Demirkan K. Effect of a pharmacist-led program on improving outcomes in patients with type 2 diabetes mellitus from Northern Cyprus: a randomized controlled trial. J Manag Care Spec Pharm. 2017;23(5):573–82.
Wang M. Generalized estimating equations in longitudinal data analysis: a review and recent developments. Adv Stat. 2014; 2014, Article ID 303728. https://doi.org/10.1155/2014/303728.
Hörnsten A, Stenlund H, Lundman B, Sandström H. Improvements in HbA1c remain after 5 years–a follow up of an educational intervention focusing on patients’ personal understandings of type 2 diabetes. Diabetes Res Clin Pract. 2008;81(1):50–5.
Tien KJ, Hung HC, Hsiao JY, Hsu SC, Hsin SC, Shin SJ, et al. Effectiveness of comprehensive diabetes care program in Taiwanese with type 2 diabetes. Diabetes Res Clin Pract. 2008;79(2):276–83.
Welch G, Garb J, Zagarins S, Lendel I, Gabbay RA. Nurse diabetes case management interventions and blood glucose control: results of a meta-analysis. Diabetes Res Clin Pract. 2010;88(1):1–6.
Sharing health information—the way of the future published by New Zealand Ministry of Health. http://www.health.govt.nz/system/files/documents/topic_sheets/sharing-health-information-flyer.pdf. Accessed 02 Nov 2017.
Harrop A. The value of laboratory values: a community pharmacy perspective. Can Pharm J CPJ. 2015;148(3):115–7.
Gernant SA, Zillich AJ, Snyder ME. Access to medical records’ impact on community pharmacist-delivered medication therapy management: a pilot from the medication safety research network of Indiana (Rx-SafeNet). J Pharm Pract. 2017;1:897190017735422.
Leung WY, So WY, Tong PC, Chan NN, Chan JC. Effects of structured care by a pharmacist-diabetes specialist team in patients with type 2 diabetic nephropathy. Am J Med. 2005;118(12):1414.
Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11(4):253–60.
ISMP. Adjust Pradaxa dose for renal impairment. 2011. www.ismp.org/newsletters/ambulatory/archives/2011102_1.asp. Accessed 2 Nov 2017.
British Columbia Pharmacy Association (BCPhA) Clinical Service Proposal, Medication Adherence Services, Canada. 2013. http://studyres.com/doc/23992964/medication-adherence-services. Accessed 02 Nov 2017.
Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. BMJ. 2015;20(350):h176.
Shawn McFarland M, Wallace JP, Parra J, Baker J. Evaluation of patient satisfaction with diabetes management provided by clinical pharmacists in the patient-centered medical home. Patient. 2014;7(1):115–21.
Acknowledgements
We would like to thank the MUR coordinator and the community pharmacists who participated in this study and helped us with the data collections.
Funding
Mangesh D. Kharjul was supported by a School of Pharmacy PhD stipend.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kharjul, M., Braund, R. & Green, J. The influence of pharmacist-led adherence support on glycaemic control in people with type 2 diabetes. Int J Clin Pharm 40, 354–359 (2018). https://doi.org/10.1007/s11096-018-0606-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0606-z