Abstract
Background Medication dispensing errors (MDEs) are frequent in community pharmacy practice. A definition of MDEs and scenarios representing MDE situations in Palestinian community pharmacy practice were not previously approached using formal consensus techniques. Objective This study was conducted to achieve consensus on a definition of MDEs and a wide range of scenarios that should or should not be considered as MDEs in Palestinian community pharmacy practice by a panel of community pharmacists. Setting Community pharmacy practice in Palestine. Method This was a descriptive study using the Delphi technique. A panel of fifty community pharmacists was recruited from different geographical locations of the West Bank of Palestine. A three round Delphi technique was followed to achieve consensus on a proposed definition of MDEs and 83 different scenarios representing potential MDEs using a nine-point scale. Main outcome measure Agreement or disagreement of a panel of community pharmacists on a proposed definition of MDEs and a series of scenarios representing potential MDEs. Results In the first Delphi round, views of key contact community pharmacists on MDEs were explored and situations representing potential MDEs were collected. In the second Delphi round, consensus was achieved to accept the proposed definition and to include 49 (59 %) of the 83 proposed scenarios as MDEs. In the third Delphi round, consensus was achieved to include further 13 (15.7 %) scenarios as MDEs, exclude 9 (10.8 %) scenarios and the rest of 12 (14.5 %) scenarios were considered equivocal based on the opinions of the panelists. Conclusion Consensus on a definition of MDEs and scenarios representing MDE situations in Palestinian community pharmacy practice was achieved using a formal consensus technique. The use of consensual definitions and scenarios representing MDE situations in community pharmacy practice might minimize methodological variations and their significant effects on the number and rate of MDEs reported in different studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Methodological variability in counting medication dispensing errors (MDEs) in community pharmacy practice might arise from situations for which there could be some debate as to whether or not they should be considered MDEs.
-
The use of consensual definitions and scenarios representing MDEs might be the way to forward in minimizing methodological variations in analyzing for MDEs in community pharmacy practice.
-
Consensual definitions and MDE situations permit direct comparisons between the numbers and rates of MDEs reported in different studies.
Introduction
Since the publication of the report “To Err is Human: Building a Safer Health System” by the Institute of Medicine in 2000, medication errors have become a center of attention for research in medicine and pharmacy [1]. Consequently, improving the safety of healthcare services and reducing medication errors have become a global priority [2]. Medication errors may occur at any stage during medication prescription, transcription, dispensing, administration or monitoring [3–6]. While the vast majority of previous studies have focused on medication errors occurring at the prescription and administration stages, the medication dispensing stage can be a source of harmful errors as well [2, 5, 7–10].
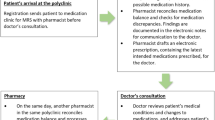
In Palestine, community pharmacies are often individually owned in a privately funded healthcare system where patients have to pay out of their pockets to purchase medications. Community pharmacies are operated by registered pharmacists. In routine community pharmacy practice, patients or their caregivers bring prescriptions to community pharmacies where pharmacists fill prescriptions and dispense medications accordingly. Generic substitution is a common practice that is often performed by the community pharmacists without consulting the prescriber. Like in many community pharmacy practice settings around the world, once a prescription was filled and a medication was dispensed to the patient further verifications to ensure the dispensing of correct medication are not performed [2, 9, 11]. Therefore, it is highly probable that errors made in the dispensing stage would reach the patient [12].
In community pharmacy practice, the processes of medication dispensing and patient counselling are the responsibility of community pharmacists and; therefore, MDEs are often made by pharmacists [13–15]. Data on prescription and dispensing volumes in the Palestinian market are not available. However, Khdour et al. [16] prospectively estimated the number of defined daily doses of non-steroidal anti-inflammatory drugs (NSAIDs) consumed per 1000 inhabitants per day in Palestinian mid-territories over a period of 3 months in 2011. The study showed that consumption was 61.3 % of that in the European countries. Conflicting reports were published on the rate of MDEs in different community pharmacy settings. In the UK, MDEs rates were reported in the range of 0.04–0.08 % in community practice [2, 17]. Franklin and O’Grady [9] reported content errors in 1.7 % and labelling errors in 1.6 % of dispensed items. In the US, dispensing error rates of up to 24 % in community pharmacies were reported [18, 19]. Flynn et al. [19] observed trained pharmacists in fifty pharmacies and reported an overall error rate of 1.7 % (range 0–12.8 %) in 4481 dispensed items. Regardless of the exact rate, even smaller figures are of extreme importance given that millions of medications are dispensed annually in community pharmacy practice and therefore presenting many opportunities for errors and harm to patients.
Variability in the number of dispensing errors or rates could be attributed to the variable number or rate of errors observed in each study. Variability could also be attributed to differences in what constituted a MDE situation in each study. Such methodological variations were shown to affect the error rates reported in observational studies investigating medication administration errors [20]. Obviously, using a definition of MDEs is a prerequisite step in assessing the incidence and prevalence of MDEs in different community pharmacy settings [9]. Accordingly, the number or rate of errors to be reported would differ depending on the number and type of situations considered as MDEs in each analysis. Clearly, studies that would include a larger number of MDE situations would report a larger number or rate of errors and vice versa [9, 21, 22]. In their review, James et al. [12] showed that different studies used different definitions of MDEs. These definitions were either developed by researchers or were taken from previous studies.
Lately, formal consensus techniques were used to develop definitions of different types of medication errors like prescribing errors [22, 23] and medication administration errors [5]. Franklin and O’Grady [9] used a formal consensus technique to achieve consensus on a definition of MDEs and 26 situations representing potential MDEs by a panel composed of 16 healthcare professionals with backgrounds in primary care, community pharmacy and/or the study of dispensing errors in the UK. However, it is not known if a similar definition can be accepted to be applied in Palestinian community pharmacy practice by community pharmacists. Similarly, there is a need to explore a wider range of potential MDE situations than those included in the study by Franklin and O’Grady. Currently, it is not known what would be considered as MDEs in Palestinian community pharmacy practice. For example, some legislations permit generic substitutions while under other laws they are not permitted. It is also believed that using consensual scenarios representing MDEs would impart validity to the error numbers and rates to be reported in future epidemiology studies investigating the incidence and prevalence of MDEs in Palestinian community pharmacy practice. A thorough understanding of MDE situations might help in changing community pharmacists’ behavior leading to errors.
Aim of the study
This study was conducted to achieve consensus on a definition of MDEs occurring in community pharmacy practice by a panel of community pharmacists using a formal consensus technique. The formal consensus technique was also used to achieve consensus on a wide range of situations representing potential MDEs in Palestinian community pharmacy practice.
Ethics approval
The protocol and ethics of this study were approved by the Institutional Review Board (IRB) Committee of An-Najah National University. All panelists invited to participate in this study gave verbal consent before taking part in the study. To protect the participants from any consequences, data were made anonymous before analyses. Views and opinions of each panelist were considered equally and each panelist remained anonymous to the remainder of the panelists during the Delphi rounds.
Methods
Panel of community pharmacists
We used purposive sampling to recruit panelists for this study. Personal contacts in the field were used to identify potential panelists from different geographical regions of the West Bank of Palestine. Nomination was based on qualifications and experience in the field of community pharmacy. Upon nomination, researchers approached the nominees and invited them to participate in the present study. Researchers explained the objectives and the design of the study to the nominees. The nomination criteria were as follows: (1) possession of a basic or advanced degree in pharmacy, (2) licensed to practice pharmacy in Palestine, (3) at least 5 years of practicing experience in a community pharmacy setting and as prior knowledge of the topic being investigated is highly recommended for panelists and (4) knowledge of MDEs. A total of fifty community pharmacists were invited to take part in this study. No financial incentives were offered to panelists during this study.
The Delphi technique
In this study, the Delphi technique was chosen as the most appropriate method to develop and achieve consensus on a proposed definition of MDEs and scenarios representing MDE situations [24, 25]. The Delphi technique has emerged as a valuable method of developing and achieving consensus on subjects with limited or inconclusive definitions [25]. This technique provides anonymity to the panelists, possibility to include panelists from different geographical locations, less costly and more practical than other commonly used methods like focus groups and ensures immunity against individual domination of the discussion [26, 27].
The Delphi technique is an iterative process which is executed in rounds. In the first round, views and opinions are generated [25]. These views and opinions are presented to a panel in subsequent rounds in which panelists indicate the extent of their agreement or disagreement with these views and opinions. To decrease the number of rounds needed to achieve consensus, panelists are provided with statistical summaries and comments generated in the previous round and asked to reconsider their prior agreements or disagreements in view of the opinions of other panelists [24].
Literature search
Prior to the first Delphi round, a literature search was performed to identify different definitions of MDEs used in previous studies. The majority of these definitions are summarized in a review by James et al. [12]. One of these definitions was developed by Franklin and O’Grady [9] using the Delphi technique. Consensus on this definition was achieved by a two round Delphi techniques using a panel of 16 panelists from the UK. In this study, we decided to use similar definition and explore if this definition would be accepted to be applied in Palestinian community pharmacy practice by a larger panel of community pharmacists from Palestine. In this definition a MDE was described as “any unintended deviation from an interpretable written prescription or medication order in terms of content and labelling in addition to any unintended deviation from professional or regulatory references, or guidelines affecting dispensing procedures” [9].
A comprehensive literature search was performed also to identify types of MDEs used in previous analyses [1, 2, 6–9, 12, 13, 17–19, 28–31]. All types of MDEs included or excluded in previous studies were identified. Other types of medication errors like prescribing and administration errors were also searched [5, 22, 23].
First Delphi round
In the first Delphi round, ten key contact community pharmacists were interviewed. The key contacts were asked to describe all situations they believed represented potential MDEs. Potential MDE situations found in the literature together with situations mentioned by the ten key contacts were formulated into a series of various scenarios. Some scenarios were based on other types of medication errors like prescribing and administration errors. These scenarios were included into a questionnaire. The questionnaire was piloted with five pharmacists who were not included in the Delphi process. Based on the feedback from the pilot, some scenarios were modified to help understanding.
Second Delphi round
In the second Delphi round, the questionnaire was handed to the fifty panelists. The questionnaire was of three parts. In the first part, panelists were asked to provide their demographic details. The second part included the proposed definition of MDEs. Panelists were asked to indicate the extent to which they agree or disagree with the proposed definition on a nine-point scale, where a score of 1 indicated total disagreement with the definition and a score of 9 indicated total agreement with the definition. Finally, the third part included a series of 83 scenarios representing potential MDE situations and panelists were asked to indicate the extent to which they agree or disagree with each scenario to be considered or not considered a MDE on a nine-point scale. A score of 1 indicated total disagreement and the scenario should not be considered a MDE, while a score of 9 indicated total agreement and the scenario should be considered a MDE. Panelists were encouraged to include written comments to justify or qualify their scores.
Data analysis and definition of consensus
Descriptive statistics were calculated using Excel sheet (Microsoft Excel 2007). The first quartile (Q1), median (Q2), third quartile (Q3), and IQR of the scores were calculated for the definition and each scenario separately. The data were analyzed as previously described [5, 9]. Briefly, (1) when the median of scores fell within the range of 7–9 and the IQR was between 0 and 2, the definition or scenario was accepted; (2) when the median of scores fell within the range of 1–3 and the IQR was between 0 and 2, the definition or scenario was rejected; and (3) when the median of scores fell within the range 4–6 or the IQR was larger than 2, the definition or scenario was considered equivocal.
Third Delphi round
Scenarios that were considered equivocal in the second Delphi round were included in a revised questionnaire. The questionnaire was sent to panelists for a third Delphi round. Panelists were provided with median and IQR of the scores of each scenario considered equivocal in the second Delphi round. Additional comments made by panelists to justify or qualify their scores were also included. Inclusion of these details was previously shown to reduce the number of rounds needed to achieve consensus on issues in healthcare [24].
Scores of the third Delphi round were analyzed as previously described for the second Delphi round.
Results
Participant characteristics and response rate
The panel included community pharmacists practicing in different geographical locations, of both genders, belonged to different age groups, and graduated from different universities and pharmacy schools. The demographic details of the panelists are shown in Table 1. Of the fifty panelists, 25 (50 %) were females and 25 (50 %) were males. The median age was 32.5 (IQR 13.5) years.
In the second Delphi round, questionnaires were returned by all panelists and therefore, the response rate was 100 %. However, in the third Delphi round, questionnaires were returned by 46 (92 %) of the panelists.
Definition of MDEs
When asked to indicate the extent of their agreement or disagreement with the proposed definition, consensus was achieved to accept the proposed definition which stated that a MDE was “any unintended deviation from an interpretable written prescription or medication order in terms of content and labelling in addition to any unintended deviation from professional or regulatory references, or guidelines affecting dispensing procedures”. The median score was 7 and the IQR was 1.
Scenarios representing MDE situations
In the second Delphi round, consensus was achieved to consider 49 (59 %) of the 83 scenarios as MDEs. In the third Delphi round, consensus was achieved to consider further 13 (15.7 %) scenarios as MDEs. Scenarios considered as MDEs are shown in Table 2.
A total of 9 (10.8 %) scenarios were not considered as MDEs and the rest of 12 (14.5 %) scenarios were considered equivocal based on the opinions and comments of the panelists (Tables 3, 4). Considering the comments of the panelists following the third Delphi round, it was decided not to conduct further rounds as it would be unlikely to achieve consensus on the remaining scenarios. Equivocal scenarios might or might not be considered as MDEs depending on the individual situation.
At the end of the third Delphi round, the 83 scenarios were either considered as MDE situations, non-error situations or remained equivocal, i.e. to be considered as errors or not depending on the individual situation. In general, consensus was achieved to include scenarios representing MDE situations related to: (1) when the community pharmacist dispensed another item instead of the prescribed item, (2) when the community pharmacist dispensed a different dose, dosage form or count of the dispensed item, (3) when the community pharmacist failed to deliver or delivered incorrect essential information pertaining to the dispensed item, (4) when the community pharmacist failed to correctly pack or label the dispensed item, (5) when the community pharmacist failed to document essential dispensing notes required by regulatory authorities, (6) when the community pharmacist failed to dispense appropriate tools for the administration of the dispensed item, (7) when the community pharmacist failed to verify the validity of the prescription, (8) when the community pharmacist failed to follow appropriate procedures in the preparation of the dispensed item, and (9) when the community pharmacist failed to dispense a medication or a dose of medication (Table 2).
Discussion
In this study we sought consensus on a definition and scenarios representing MDE situations in Palestinian community pharmacy practice by a panel of community pharmacists. A definition of MDEs previously developed for community pharmacy practice in the UK and a total of 83 potential MDE situations were used. Situations representing MDEs were previously investigated individually or collectively, but a comprehensive list of potential MDE scenarios was not approached in one study [1, 2, 7–9, 12, 13, 17–19, 28–31]. To our knowledge, this study is the most comprehensive investigation of MDE situations using formal consensus techniques.
In the present study, purposive sampling was used to construct the panel of community pharmacists. Purposive sampling was long considered biased in conservative views [26]. However, other randomized sampling techniques are not suitable for this study. The sampling technique used in this study permitted the inclusion of panelists who were expert in the topic being investigated. In this study we decided to recruit a panel of expert community pharmacists. This decision was because dispensing medications and patient counseling in community pharmacy practice are the sole responsibility of community pharmacists. Therefore, MDEs in community pharmacy practice are committed by community pharmacists or occur under their responsibility. Pharmacists who commit MDEs may be subjected to blame, disciplinary action, litigation and/or job loss [32, 33]. Furthermore, to change the behavior leading to errors among community pharmacists, obviously, it would be better to use definitions that community pharmacists would agree with instead of using definitions that pharmacists would not agree with [5, 22, 23, 34, 35].
Many definitions were previously developed and used to investigate MDEs in previous studies [7, 9, 12, 18]. The definition used in this study was adopted from the study of Franklin and O’Grady [9]. The decision was made to adopt this definition because it was developed using the Delphi technique. In the study of Franklin and O’Grady, consensus on the definition was achieved using a panel composed of 16 panelists from the UK. Although the exact composition of the panel used was not provided in detail, amendments were made to the definition based on feedback from the panel adds to its validity. Amendments were made to include content and labeling errors. Inclusion of content and labeling errors was of particular importance as in previous studies a considerable portion of MDEs were content and labeling errors [9, 12].
Interestingly, all invited panelists accepted to participate, a strength which adds to the validity of the study. Panels used in the Delphi technique vary considerably in size and may range from 10 to over 1000 [26, 36]. However, the literature is inconclusive on the ideal size. Previous studies on other types of medication errors used fifty panelists or less [22–24]. The panel size used in this study was either comparable or larger than panel sizes used to achieve consensus on issues in healthcare [5, 9, 22–24]. Obviously, the panel used in this study was larger than the one used in the study of Franklin and O’Grady [9]. In this study, consensus on the definition was achieved with a larger panel of fifty community pharmacists with diverse geographical locations, gender, age group, experience and academic backgrounds (Table 1). Our results add to the validity and suitability of the definition to be used in Palestinian community pharmacy practice. In the absence of gold standards, using formal consensus methods may reduce bias, promote transparency and validation of judgmental methods in the development of certain criteria [37]. Hence, definitions approached using formal consensus techniques might be more appealing than other definitions.
Using a three round Delphi technique, consensus was achieved to consider 62 scenarios as MDEs (Table 2). These results are consistent with some scenarios used in previous studies investigating MDEs [1, 7–9, 12, 18, 28]. However, consensus was achieved to consider 9 scenarios as non-error situations (Table 3). These scenarios represented common practices in the community pharmacy settings. In general, panelists believed that some deviations made by community pharmacists in common practice are justified. Examples include generic substitutions, not dispensing a medication based on professional judgment or when the patient refuses to take the medication. In this study, generic substitutions were not considered as MDEs, even when the physician prescribed a brand-name medication or a branded generic version. Generic substitution continues to generate heated debates [38]. While evidence for similar safety and efficacy scientifically justifies substitution it is subjected to local legislations. Some legislations permit generic substitution without the prescriber’s permission while other legislations require prescriber’s authorization. In neighboring Jordan, for example, current regulations do not permit the pharmacist to make any change or substitution to prescriptions, unless authorized by the physician [39]. However, the ministry of health encourages generic substitution and physicians in public sector are encouraged to prescribe generically [39]. In this study, panelists did not consider dispensing a pack of medication missing the patient information leaflet as a MDE. Similar consensus was previously achieved by a panel from the UK [9]. Panelists commented not to include misspelling a medication name as a MDE when the misspelling was minor and the medication can be recognized without confusion.
Some labeling errors were divisive among panelists and after the third Delphi round remained equivocal (Table 4). These scenarios would be considered as MDEs or not depending on the individual situation. We did not execute a further Delphi round as based on the panelists’ comments, it is unlikely that consensus would be achieved on these scenarios. Moreover, conducting further rounds would lead to panel fatigue which is a known limitation of the Delphi process [22].
Limitations
Results of this study can be interpreted considering the following limitations. First, our panel of experts included solely community pharmacists. Other healthcare professional were not included. It is important to note that other healthcare professionals like physicians and nurses might have different views and opinions. However, in this study we intentionally recruited community pharmacists because dispensing medications and patient counselling in community pharmacy practice are the responsibility of community pharmacists. Second, the developed scenarios represent situations that occur in community pharmacy practice. Despite that some scenarios might apply to hospital pharmacy settings, our results might not be generalized to hospital pharmacy settings. Lastly, our results might not be generalized to community pharmacy settings where legislations do not permit community pharmacists to perform some of the practices considered common practice in this study.
Conclusion
Consensus on a definition of MDEs and scenarios representing MDE situations in Palestinian community pharmacy practice was achieved using a formal consensus technique. In previous studies, researchers must have counted MDEs and calculated error rates based on different MDE scenarios. Some potential MDE situations were divisive among researchers. This should have affected the numbers or rates of the reported MDEs in their studies and therefore it is not possible to compare results from these different studies. The use of consensual definitions and scenarios representing MDE situations in community pharmacy practice might minimize methodological variations and their significant effects on the number and rate of MDEs reported in different studies. Furthermore, using consensual definitions and MDE situations can permit and promote direct comparison of different studies conducted in community pharmacy practice. A pilot study using the scenarios that were considered as MDEs by the community pharmacists might be needed to assess the applicability of the findings of this study.
References
South DA, Skelley JW, Dang M, Woolley T. Near-miss transcription errors: a comparison of reporting rates between a novel error-reporting mechanism and a current formal reporting system. Hosp Pharm. 2015;50(2):118–24.
Ashcroft DM, Quinlan P, Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf. 2005;14(5):327–32.
Shawahna R, Rahman NU, Ahmad M, Debray M, Yliperttula M, Decleves X. Electronic prescribing reduces prescribing error in public hospitals. J Clin Nurs. 2011;20(21–22):3233–45.
Shawahna R, Rahman NU, Ahmad M, Debray M, Yliperttula M, Decleves X. Impact of prescriber’s handwriting style and nurse’s duty duration on the prevalence of transcription errors in public hospitals. J Clin Nurs. 2013;22(3–4):550–8.
Shawahna R, Masri D, Al-Gharabeh R, Deek R, Al-Thayba L, Halaweh M. Medication administration errors from a nursing viewpoint: a formal consensus of definition and scenarios using a Delphi technique. J Clin Nurs. 2016;25(3–4):412–23.
Cheung KC, Bouvy ML, De Smet PA. Medication errors: the importance of safe dispensing. Br J Clin Pharmacol. 2009;67(6):676–80.
Beso A, Franklin BD, Barber N. The frequency and potential causes of dispensing errors in a hospital pharmacy. Pharm World Sci. 2005;27(3):182–90.
Cina JL, Gandhi TK, Churchill W, Fanikos J, McCrea M, Mitton P, et al. How many hospital pharmacy medication dispensing errors go undetected? Jt Comm J Qual Patient Saf. 2006;32(2):73–80.
Franklin BD, O’Grady K. Dispensing errors in community pharmacy: frequency, clinical significance and potential impact of authentication at the point of dispensing. Int J Pharm Pract. 2007;15(4):273–81.
Braund R, Furlan HM, George K, Havell MM, Murphy JL, West MK. Interventions performed by New Zealand community pharmacists while dispensing prescription medications. Pharm World Sci. 2010;32(1):22–5.
Ocampo CC, Garcia-Cardenas V, Martinez-Martinez F, Benrimoj SI, Amariles P, Gastelurrutia MA. Implementation of medication review with follow-up in a Spanish community pharmacy and its achieved outcomes. Int J Clin Pharm. 2015;37(5):931–40.
James KL, Barlow D, McArtney R, Hiom S, Roberts D, Whittlesea C. Incidence, type and causes of dispensing errors: a review of the literature. Int J Pharm Pract. 2009;17(1):9–30.
Al-Arifi MN. Community pharmacists’ attitudes toward dispensing errors at community pharmacy setting in Central Saudi Arabia. Saudi Pharm J. 2014;22(3):195–202.
Buurma H, de Smet PA, van den Hoff OP, Egberts AC. Nature, frequency and determinants of prescription modifications in Dutch community pharmacies. Br J Clin Pharmacol. 2001;52(1):85–91.
Chamba G, Bauguil G, Galiezot J. The role of the French community pharmacist in drug dispensing. Pharm World Sci. 1999;21(3):142–3.
Khdour MR, Hallak HO, Hejaz H, Shaeen M, Dweib M. Patterns of NSAIDs use in Palestinian mid-territories: a prospective study of ambulatory patients in outpatient pharmacies. Curr Clin Pharmacol. 2014;9(1):10–6.
Chua SS, Wong IC, Edmondson H, Allen C, Chow J, Peacham J, et al. A feasibility study for recording of dispensing errors and near misses’ in four UK primary care pharmacies. Drug Saf. 2003;26(11):803–13.
Allan EL, Barker KN, Malloy MJ, Heller WM. Dispensing errors and counseling in community practice. Am Pharm. 1995;NS35(12):25–33.
Flynn EA, Barker KN, Carnahan BJ. National observational study of prescription dispensing accuracy and safety in 50 pharmacies. J Am Pharm Assoc. 2003;43(2):191–200.
McLeod MC, Barber N, Franklin BD. Methodological variations and their effects on reported medication administration error rates. BMJ Qual Saf. 2013;22(4):278–89.
Hartley G, Dhillon S. An observational study of the prescribing and administration of intravenous drugs in a general hospital. Int J Pharm Pract. 1998;6(1):38–45.
Ghaleb M, Barber N, Franklin BD, Wong I. What constitutes a prescribing error in paediatrics? Qual Saf Health Care. 2005;14(5):352–7.
Dean B, Barber N, Schachter M. What is a prescribing error? Qual Health Care. 2000;9(4):232–7.
Duffield C. The Delphi technique: a comparison of results obtained using two expert panels. Int J Nurs Stud. 1993;30(3):227–37.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
Page A, Potter K, Clifford R, McLachlan A, Etherton-Beer C. Prescribing for Australians living with dementia: study protocol using the Delphi technique. BMJ Open. 2015;5(8):e008048.
McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs. 1994;19(6):1221–5.
Seifert SA, Jacobitz K. Pharmacy prescription dispensing errors reported to a regional poison control center. J Toxicol Clin Toxicol. 2002;40(7):919–23.
Bond CA, Raehl CL. Pharmacists’ assessment of dispensing errors: risk factors, practice sites, professional functions, and satisfaction. Pharmacotherapy. 2001;21(5):614–26.
Flynn EA, Barker KN, Gibson JT, Pearson RE, Berger BA, Smith LA. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. Am J Health Syst Pharm. 1999;56(13):1319–25.
Peterson GM, Wu MS, Bergin JK. Pharmacist’s attitudes towards dispensing errors: their causes and prevention. J Clin Pharm Ther. 1999;24(1):57–71.
Asbury RP. Pharmacist liability: the doors of litigation are opening. Santa Clara Law Rev. 1999;40:907.
Shah RK, Kentala E, Healy GB, Roberson DW. Classification and consequences of errors in otolaryngology. Laryngoscope. 2004;114(8):1322–35.
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–20.
Ross L, Wallace J, Paton J. Medication errors in a paediatric teaching hospital in the UK: five years operational experience. Arch Dis Child. 2000;83(6):492–7.
Akins RB, Tolson H, Cole BR. Stability of response characteristics of a Delphi panel: application of bootstrap data expansion. BMC Med Res Methodol. 2005;5:37.
Ferguson ND, Davis AM, Slutsky AS, Stewart TE. Development of a clinical definition for acute respiratory distress syndrome using the Delphi technique. J Crit Care. 2005;20(2):147–54.
Duerden MG, Hughes DA. Generic and therapeutic substitutions in the UK: are they a good thing? Br J Clin Pharmacol. 2010;70(3):335–41.
El-Dahiyat F, Kayyali R. Evaluating patients’ perceptions regarding generic medicines in Jordan. J Pharm Policy Pract. 2013;6:3.
Acknowledgments
Authors would like to thank all expert community pharmacists who participated in this study.
Funding
This study did not receive any specific funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shawahna, R., Haddad, A., Khawaja, B. et al. Medication dispensing errors in Palestinian community pharmacy practice: a formal consensus using the Delphi technique. Int J Clin Pharm 38, 1112–1123 (2016). https://doi.org/10.1007/s11096-016-0338-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0338-x