Abstract
Background Obesity is a growing problem in England with one quarter of the adult population being obese and around 60 % being overweight or obese. Given the high costs of treating obesity-related conditions such as coronary heart disease and type-2 diabetes the UK Government aims to reduce obesity through public health services including those provided by community pharmacists. Objective To evaluate the effectiveness of a community pharmacy weight management clinic in assisting obese patients to reduce their weight. Setting Community pharmacies across four Primary Care Trusts in England. Methods Retrospective analysis of data collected by pharmacies providing weight management programmes. The service involved measurement with provision of advice and support. Data analysis consisted of frequency counts, percentages and means with standard deviations (SD) for demographic and biometric variables. Paired t tests were used to compare weight, waist circumference and blood pressure at 3 and 6 months. Main outcome measure Weight change at 3 months. Results 281 patients attended the programme across four Primary Care Trusts. Three-quarters were female, mean age 52.8 years (SD ± 14.4) and mean baseline weight 96.3 kg (SD ± 15.7). At 3 months patients had lost weight (mean change = −3.07 kg) and waist circumference (mean change = −3.87 cm), but there was no difference in blood pressure. After 6 months weight and waist circumference were further reduced from baseline (mean change = −4.59 kg, −4.79 cm respectively) and there was a reduction in blood pressure (mean change systolic = −9.5 mmHg; diastolic = −4.7 mmHg). Conclusion The study has demonstrated that reductions in weight and waist circumference can be achieved in patients who participate in a community pharmacy weight management programme.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Pharmacists can contribute to tackling obesity through community pharmacy based clinics
-
Pharmacists can be successful in contributing to public health services other than those where medicines are supplied
Introduction
Obesity is a growing problem in England with one quarter of the adult population being obese and around 60 % of the population being overweight or obese [1]. Obesity is a risk factor for many diseases including coronary heart disease and type-2 diabetes [2]. Obese people are up to five times more likely to have hypertension compared with normal weight people [3] and the accumulation of abdominal fat has also been shown to increase the risk of hypertension [4]. The risk of diabetes shows a strong relationship with both increasing body mass index (BMI) and waist circumference [5]. Prognosis for obese patients is often poorer than for normal weight individuals with the same disease [2].
Many factors have contributed to the ‘obesity epidemic’ including changes in lifestyles resulting in increased food intake and reduced physical activity levels [2]. Whilst weight reduction programmes focus on these two modifiable factors, obesity is a complex interaction of environmental, genetic and psychosocial factors [6].
People find losing weight challenging and they frequently need support to help them achieve their aims. The National Institute for Health and Care Excellence (NICE) recommends that a combination of reduced calorie intake and increased physical activity levels should be the first line approach to managing obesity [7]. However, people may find this difficult without support and advice with evidence pertaining to the effectiveness of a number of factors alongside a diet and exercise programme [8]. These factors include: self-monitoring (e.g. using food diaries); social support from family and friends, or advisors, to provide motivation and encouragement; and an individual plan to develop techniques and strategies to adhere to new healthy behaviours and avoid relapsing into old habits [8].
The cost to the National Health Service (NHS) of obesity-related conditions has been estimated to be £4.2 billion each year and the 2010 public health white paper set out the government’s aim of improving diets and increasing activity in the population [9]. This white paper also recognised the success of providing public health services through community pharmacies for a range of conditions including smoking cessation and weight management [9].
Primary care based one-to-one interventions involving a structured advice programme have been shown to be effective in assisting people to lose weight over periods of up to 12 months [10, 11]. Recent evaluations of NHS commissioned pharmacy weight management services have reported that interventions based in community pharmacies can achieve weight loss for patients [12, 13]. However these reports only cover single geographical areas where the service was available.
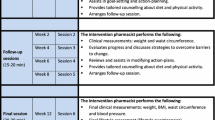
The Community Pharmacy Weight Management Programme was designed and managed on behalf of Primary Care Trusts (PCTs) by Alliance Healthcare. It was piloted in Coventry PCT in 2007 and extended to four other PCTs until 2010. The scheme was a measurement and structured advice programme provided by community pharmacies with up to 11 follow-up visits to monitor progress. The scheme was delivered by pharmacists and available to NHS patients with a BMI of 30 kg/m2 or more and at least one risk factor for coronary heart disease. The scheme aimed to assist patients in losing at least 5 % of their initial body weight.
Aim of the study
To evaluate the effectiveness of a community pharmacy weight management programme in assisting obese patients to reduce their weight using a retrospective analysis of data collected by pharmacies providing the service.
Ethical approval
Ethical approval for the study was obtained from the Proportionate Review Sub-committee of NRES Committee East Midlands—Nottingham 2. Each PCT gave their approval for the use of the anonymised data for this research.
Methods
The study was a retrospective analysis of data collected by pharmacies as part of providing the weight management programme. Data to be used were originally collected for collation and feedback to the PCTs about the service in their area. Four of the five PCTs who provided the service gave permission to use their data for this analysis.
Weight management programme
The weight management programme was designed and managed by Alliance Healthcare on behalf of the commissioning PCTs. Alliance Healthcare, a member of Alliance Boots supports pharmacies to improve patient outcomes through pharmacy-led services. This is funded by manufacturers as well as the NHS through local commissioning or a combination of both. The commissioned weight management programme also received partial funding from the Department of Health.
Individual pharmacies within the PCT decided whether or not to participate in the service. The service was provided to patients by pharmacists who received training from Alliance Healthcare about the programme including the service structure, taking patient measurements and methods to motivate patients to change their behaviour. Patients were recruited to the service by the pharmacy staff or pharmacists based on their use of current therapies for conditions associated with obesity or following a discussion about their weight; referral to the service by their GP practice; or by self referral.
Patients attended an initial assessment with the pharmacist, to ensure they met the inclusion criteria for the programme and to provide the first structured advice session; the programme inclusion criteria are fully detailed below. Patients consented to the service after it had been explained to them and prior to any measurements being taken. Patients were then invited to follow-ups initially at 2 weekly and then approximately monthly intervals for up to a total of 12 visits. Measurements recorded included age, gender, height, weight, BMI, blood pressure (BP), waist and hip circumference and clinical measurements such as cholesterol levels and random blood glucose. Details of the advice provided at baseline and each visit were not included in the data provided by the pharmacies. The service was provided on an individualised basis with calorie restricted diet plans and increased physical activity targets which were reviewed at each visit, together with other health advice as appropriate, such as smoking cessation.
The service was provided in four PCTs but differed slightly across these PCTs. The timing of the follow-ups varied across the PCTs, as did the measurements taken and, in particular, the visits at which these measurements were taken. The programme was provided in a range of pharmacies—independents, small chains and large multiples.
Inclusion criteria for the service were being aged 18 years or over, having a BMI 30–38 kg/m2 and at least one risk factor for coronary heart disease (hypertension, hyperlipidaemia, type-II diabetes, increased waist circumference (defined as ≥102 cm in males and ≥88 cm in females; for Asian males ≥90 cm and Asian females ≥80 cm)). There were some variations in the programme across the PCTs with one having no upper BMI limit for inclusion and another not including hyperlipidaemia as a risk factor. Pregnant or breast-feeding women and any patients considered by the pharmacist to be in too poor a state of health were not eligible for the programme.
Evaluation of the service
Alliance Healthcare checked the collected data for completeness, and queried with the reporting pharmacy where data were missing, illegible or seemingly incorrect. The database was subsequently supplied to the researchers. Data were cleaned on arrival at the University, converted to enable comparison across time and transferred to PASW version 17 for analysis.
Data analysis
Data analysis consisted of frequency counts and percentages for the demographic and biometric variables. The proportion of people achieving 5 % weight loss was calculated at 3, 6 months and for their last recorded visit together with the 95 % confidence interval (CI) for each proportion. Paired t tests were used to compare weight and waist circumference at 3 months and approximately 6 months (either 26 or 28 weeks as visits across the PCTs did not coincide at this time point). Additionally the analysis was repeated using last observation carried forward (LOCF) to determine the impact of drop-out from the programme on the results. Those patients who did not remain in the programme until the time point were assigned their last recorded weight and a paired t test was done to determine the effect on the result for 3 and 6 months follow-up.
The programmes had variable upper limits for BMI for entry to the programme (one PCT had no upper limit and the other PCTs a maximum BMI of 38), we did not apply these upper limits for BMI in our main analysis as the pharmacies had recruited patients above the BMI maximum but we conducted a sensitivity analysis to determine whether or not this would affect the interpretation of the results. The sensitivity analysis excluded 43 patients with a BMI >38 kg/m2 at baseline. As with the main analysis paired t tests were used to compare baseline with 3 and 6 months follow-up for weight, waist circumference and blood pressure.
Results
Records were received for a total of 332 patients from four PCTs. Nine patients were excluded from the analysis as there was no baseline weight or BMI recorded. BMI was re-calculated based on the height and weight records. The inclusion criteria that patients must have a BMI of at least 30 were then applied to these re-calculated values and 42 patients were excluded from the analysis, see Fig. 1.
The remaining 281 patients were recruited by 34 pharmacies with a mean of 9 patients per pharmacy, range 1–21. The mean age of patients was 52.8 years (SD ± 14.4) and three-quarters were female, see Table 1 for baseline characteristics. Fifty-four patients (19 %) attended only the initial visit and did not return for any follow-up appointments. Measurements of cholesterol, random blood glucose and HbA1C are not reported due to low numbers (74, 58 and 14 patients had these tests recorded respectively had results from each test recorded). Patient retention in the programme was 39 % (n = 110) at 2 months and 21 % (n = 59) at 6 months.
The primary aim of the weight management programme was to assist patients in losing 5 % of their body weight. This was achieved at 3 months for 26 patients, 24 % (95 % CI 16–32 %) of the 110 remaining in the programme, and at 6 months for 27 patients, 46 % (95 % CI 33–59 %) of the 59 remaining in the programme. Overall 15 % (n = 42, 95 % CI 11–19 %) of those who had a baseline assessment were known to have achieved the 5 % reduction in weight before leaving the programme.
There was a statistically significant reduction in weight at 3 months for those patients remaining in the programme (Table 2, n = 110, t = 9.209, p < 0.001). At 3 months seventy-two patients (66 %) lost less than 5 kg, with 23 (21 %) losing more than 5 kg, and 15 (14 %) gained weight or their weight was unchanged since baseline. The LOCF analysis, which included the last recorded weight of patients who dropped out from the programme, showed a statistically significant reduction in weight at 3 months although the effect size was reduced (n = 281; mean weight change since baseline = −1.692 kg (SD ± 3.14), t = 9.020, p < 0.001). Waist circumference was also reduced after 3 months in the programme (t = 7.720, p < 0.001). There was no statistically significant change in blood pressure.
At 6 months for those patients remaining in the programme there were statistically significant reductions in weight and waist circumference compared with baseline (Table 2; n = 59; mean weight change since baseline = −4.59 kg, t = 7.440, p < 0.001; mean change in waist circumference since baseline = −4.79 cm, t = 6.629, p < 0.001), although 11 patients (19 %) gained weight or their weight was unchanged since baseline. The LOCF analysis showed a statistically significant reduction in weight at 6 months although similar to 3 months the effect size was reduced (n = 281; mean weight change since baseline = −1.931 kg (SD ± 3.70), t = 8.738, p < 0.001). By 6 months statistically significant reductions in blood pressure were observed with two-thirds (n = 22) having blood pressure reduced at 6 months compared with baseline [mean change in systolic BP = −9.5 mmHg (SD ± 20.1); mean change in diastolic = −4.7 mmHg (SD ± 9.0)]. However, only just over half of patients had a record of blood pressure measurement at 6 months.
The sensitivity analysis which included only those patients meeting both lower and any upper BMI criteria showed similar changes compared with baseline to the main analysis—Table 3.
Discussion
Patients achieved a reduction in weight and waist circumference at 3 months in the programme; around a quarter achieved the goal of reducing their body weight by 5 % at 3 months. These effects were also seen at 6 months and additionally there was a reduction in blood pressure, which was not seen at 3 months.
This paper reports a weight management programme in a real life situation, not a part of a trial. An advantage of which is being able to demonstrate that the programme was successful in achieving weight loss for those remaining in the programme at 3 months in everyday practice. However using a before and after study method limits the usefulness of the results in that there is no control group for comparison. The absence of a control group means we cannot be confident that it was the intervention which caused the weight loss or whether the size of the reduction in weight could be achieved with a smaller and less costly intervention. There was also a high loss to follow-up in this study (61 % at 3 months). Reasons for the high loss to follow-up are unknown however the LOCF analysis including all patients with their last recorded weight up to 3 months showed a statistically significant reduction in weight after 3 months but effect size was reduced, −1.69 kg (SD ± 3.14) compared with −3.07 kg (±3.49) in the completers analysis.
It has been suggested that a reduction of 5 % from initial weight for overweight and obese people is sufficient to gain some health benefit [14] and this level of weight loss was achieved for nearly one quarter of those remaining in the programme at 3 months and almost half at 6 months. Of those who commenced the programme 15 % were known to have achieved at least a 5 % reduction in weight by their last visit to the programme.
The size of the mean change in weight (−3.07 kg) at 3 months was similar to a number of other studies reporting UK pharmacy based weight management interventions where no medicine or weight loss product was supplied [12, 13, 15], as was the percentage change, although this was not reported for all studies. Only one of these studies had a control arm, which was 12 vouchers for free exercise sessions at a local leisure centre [15]. The proportion of participants achieving a weight loss of 5 % or more after 3 months in our study (24 % of those remaining in the programme) was similar to other one-to-one NHS weight management programmes [12, 16]. Retention of patients in the weight management programme (39 % at 3 months) was comparable with other one-to-one pharmacy based programmes [12, 13], but lower than that seen in group based programmes [15].
Whilst we did observe changes in blood pressure for those patients remaining in the programme the number of patients in this analysis is small and only around half of patients had follow-up measurements. The changes in weight of those patients took time to be reflected in a change in blood pressure, with no difference at 3 months but a significant difference at 6 months. The size of the reduction in blood pressure seen in this study exceeds the reported reductions in blood pressure associated with weight loss in a meta-analysis (−1.1 mmHg for systolic and −0.9 mmHg per kg) [17]. The time for any reductions in weight to influence blood pressure is not known but 26 of the 34 randomized controlled trials included in the meta-analysis were at least 20 weeks duration. In the weight management programme blood pressure was measured using digital blood pressure monitors which should minimise errors in the measurement however not all patients had a blood pressure measurement taken at each time point. Reasons for not measuring blood pressure at each time point are unknown but it may be that patients refused, those without a raised BP at baseline may not have had a subsequent measurement or that familiarity with the situation resulted in lower readings.
This pharmacy based weight management programme has demonstrated a reduction in weight for patients. Retention of patients in the service, although similar to other one-to-one NHS programmes, is an issue that any future programme would want to try to improve. If we are to persuade people to enter a weight management programme it needs to be one that they can complete alongside their work and family commitments, thus pharmacies with their longer working hours may be an ideal place for some patients to obtain the support they need to assist them in losing weight. One advantage of basing weight management programmes in pharmacies for those patients who take regular prescription medicines would be that this on-going follow-up could be done when they attend the pharmacy to collect their dispensed medicines.
Although this evaluation has added to the evidence about pharmacy based weight management programmes, there is a need for controlled trials which include an economic evaluation to determine both the effectiveness and the cost-effectiveness of pharmacy based programmes.
Conclusion
The study has demonstrated that, in a real life situation, reductions in weight and waist circumference can be achieved by patients who participate in a community pharmacy weight management programme.
References
The NHS Information Centre. Lifestyles statistics: statistics on obesity, physical activity and diet: England, 2012. Published 23 February 2013, cited 7 June 2013. http://www.aso.org.uk/wp-content/uploads/downloads/2012/03/2012-Statistics-on-Obesity-Physical-Activity-and-Diet-England.pdf.
Haslam D, James W. Obesity. Lancet. 2005;366:1197–209.
Wolf H, Tuomilehto J, Kuulasmaa K, Domarkiene S, Cepaitis Z, Molarius A, et al. Blood pressure levels in the 41 populations of the WHO MONICA Project. J Hum Hypertens. 1997;11:733–42.
Cassano P, Segal M, Vokonas P, Weiss S. Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol. 1990;1:33–48.
Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ, et al. Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obesity. 2001;9:696–705.
Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007;8(Suppl 1):13–7.
National Institute for Health and Care Excellence. CG43 Obesity: quick reference guide 2 for the NHS. Published 29 January 2010, cited 7 June 2013. http://guidance.nice.org.uk/CG43/QuickRefGuide/NHS/pdf/English.
Lang A. Froelicher ES: Management of overweight and obesity in adults: behavioral intervention for long-term weight loss and maintenance. Eur J Cardiovasc Nurs. 2006;5:102–14.
Department of Health. Healthy lives, healthy people: our strategy for public health in England. Published 30 November 2010, cited 7 June 2013. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_121941.
Hardcastle S, Taylor A, Bailey M, Castle R. A randomised controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and CHD risk factors. Patient Educ Couns. 2008;70:31–9.
Counterweight Project Team. Evaluation of the counterweight programme for obesity management in primary care: a starting point for continuous improvement. Br J Gen Pract. 2008;58:548–54.
Bush J, Langley CA, Patel A, Harvey JE. Evaluation of the Heart of Birmingham teaching Primary Care Trust (HoBtPCT) my choice weight management programme. Published December 2011, cited 7 June 2013. http://eprints.aston.ac.uk/16563/.
Morrison D, McLoone P, Broshnahan N, McCombie L, Smith A, Gordon J. A community pharmacy weight management programme: an evaluation of effectiveness. BMC Public Health. 2013;13:282.
Blackburn G. Effect of degree of weight loss on health benefits. Obes Res. 1995;3(Suppl 2):211s–6s.
Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: lighten up randomised controlled trial. BMJ. 2011;343:d6500.
Counterweight Project Team. The implementation of the Counterweight Programme in Scotland, UK. Fam Pract. 2012;29:139–44.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Acknowledgments
Alliance Healthcare provided the service documentation, information about the service and the data for analysis to the authors, but had no influence on the study.
Funding
This study was funded by Alliance Healthcare.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boardman, H.F., Avery, A.J. Effectiveness of a community pharmacy weight management programme. Int J Clin Pharm 36, 800–806 (2014). https://doi.org/10.1007/s11096-014-9964-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-014-9964-3