Abstract
Background The increasing prevalence of obesity and overweight adults creates a significant public health burden and there is great potential for pharmacists to be involved in the provision of weight management services, other than the mundane supply of commercial products. In order to provide optimal services that can be integrated into the healthcare system, a best practice model for weight management services in community pharmacy should be in place. We sought experts’ and key stakeholders’ opinions on this matter. Objectives (1) To identify components of a best practice model of a weight management service feasible in Australian community pharmacy. (2) To identify the role of pharmacists and the training requirements to up-skill pharmacists to competently provide weight management services. (3) To elicit any practical suggestions that would contribute to successful implementation of weight management services in pharmacy. Setting Australian primary care sector. Method Semi-structured interviews were conducted with a purposive sample of 12 participants including Australian experts in obesity and representatives of main Australian professional organisations in pharmacy. Interviews were digitally recorded, transcribed verbatim and thematically analysed using the framework approach. Main outcome measure Recommended components of pharmacy-based weight management services and training requirements. Results Participants perceived two potential roles for pharmacists involved in weight management: health promotion and individualised service. Multi-component interventions targeting all three areas: diet, physical activity and behaviour change were emphasised. Physical assessment (e.g. weight, waist circumference measurements), goal setting, referral to allied healthcare professionals and on-going support for weight maintenance were also proposed. Participants suggested pharmacists should undergo formal training and identified various training topics to improve pharmacists’ knowledge, attributes and skills to acquire competencies necessary for delivery of this service. Some physical and financial barriers in providing these services were also identified including infrastructure, pharmacists’ time and cost-effectiveness. Conclusion Pharmacists are well-positioned to promote healthy weight and/or implement weight management interventions. Furthering pharmacists’ role would involve training and up-skilling; and addressing key practice change facilitators such as pharmacy layout and remuneration. This study provides some insight into the design and implementation of a best practice model for pharmacy-based weight management services in Australia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Pharmacists can contribute to promoting healthy lifestyle in the community and provide weight management services that could be integrated into the Australian healthcare system.
-
Developing a formal training program for pharmacists in weight management is essential to maintain the quality and consistency of services.
Introduction
The increasing prevalence of obese and overweight adults worldwide is a significant public health burden [1]. In Australia, 61.4 % of the adult population were overweight or obese in 2007–2008 [2]. The total annual cost of obesity to Australia in 2008, including health system costs, loss of productivity costs and carers’ costs, was estimated to be AU $58 billion [3]. Obesity is associated with a number of diseases, as a result of metabolic consequences such as coronary artery disease, stroke and diabetes [4]. A modest reduction of 5–10 % in body weight can have positive effects on cardiovascular risk factors, reducing morbidity and improving quality of life [4].
The primary healthcare setting represents a valuable opportunity for managing Australia’s obesity problem [3]. Community pharmacists are considered to be one of the most accessible and trusted healthcare professionals [5]. The potential contribution of community pharmacy in disease management and dissemination of public health messages is increasingly recognised [5]. There is an extensive network of community pharmacies; with close to 5,000 pharmacies around Australia including rural and remote areas and each pharmacy serves on average 4,000 people [6].
A qualitative study conducted in 2009, with practising pharmacists in Australia, revealed they would like to play a more proactive role in increasing public awareness about obesity [7]. They also proposed that pharmacists should provide weight management services that are evidence-based, non-product based and involve a multi-disciplinary approach [7]. Currently, most weight management programs provided in pharmacies in Australia are product-related [8]. Lifestyle issues are addressed to some extent, but mainly to supplement the sale of products [8].
In the past consumers viewed pharmacists as medicines experts and did not often seek their advice on matters of general health [9]. More recently however, consumers in the United Kingdom (UK) have perceived pharmacists as providers of health advice and recipients of such advice were highly satisfied, although there were mixed perceptions about pharmacists’ capabilities [10]. Similarly, a study conducted in Australia in 2010, found consumers who had received a pharmacist’s advice about weight management in the past, were more supportive of pharmacy-based weight management services in the future [11].
A recent systematic review by Gordon et al. [12], evaluated ten studies of community pharmacy-based weight management interventions which were conducted in the United States of America (USA), UK, Switzerland, Spain and Denmark. The review demonstrated that pharmacy-based weight management interventions can produce modest weight loss, however, the authors concluded that larger, long-term studies, with rigorous study designs would be required in order to establish effectiveness and cost-effectiveness. Furthermore, due to the heterogeneous nature of the interventions, it was difficult to draw conclusions on what the optimal weight management services in community pharmacy should be.
The Community Pharmacy Weight Management Project [8], an Australian government funded investigation, evaluated weight management programs provided in Australia and developed a conceptual model for community pharmacy weight management. The proposed model was based on critical literature review findings, the National Health and Medical Research Council clinical practice guidelines and other Government policies for the management of overweight and obesity. Although the investigators identified the key components of the model, they concluded more preliminary work is required. They recommended collaborating and negotiating with stakeholders about the structure and content of the weight management program and the necessary training modules for pharmacists.
Following the above mentioned recommendations, it was considered important to consult a range of stakeholders, including those within the pharmacy profession and allied health, to gain further understanding about the program content and up-skilling required by pharmacists.
Aim
The aim of this study was to consult experts in the field of weight management and professional organisations in pharmacy, regarding initiation of weight management services in Australian community pharmacy.
Objectives
-
1.
To identify components of a best practice model of a weight management service that would be feasible in an Australian community pharmacy.
-
2.
To identify the role of the pharmacist and the training requirements to up-skill pharmacists to competently provide weight management services.
-
3.
To elicit any practical suggestions that would contribute to successful implementation of a weight management services model in pharmacy.
Method
This was an exploratory qualitative study that employed in-depth, semi-structured interviews. Ethics approval was obtained from The University of Sydney Ethics Committee (approval no. 14318), prior to commencement of the study.
Participants and recruitment
A purposive sample of Australian experts in weight management and representatives of the three main professional organisations in Australian community pharmacy were invited to participate in the study. The sample was obtained using a stratified purposive sampling strategy described by Liamputtong and Ezzy [13].
Experts were identified by peer recommendation or through authorship of published articles on obesity management, or leadership of relevant committees/societies. They were considered ‘experts’ based on their high profile in their field and extensive qualifications. The sample consisted of five dieticians, three psychiatrists, three exercise physiologists and five physicians. There was no pre-determined sample size and experts were recruited until data saturation [13].
The three major professional organisations relating to community pharmacy in Australia are: The Pharmacy Guild of Australia, The Pharmaceutical Society of Australia and the Australian Association of Consultant Pharmacy. Each organisation was contacted for a national representative to participate in the study.
Interviews
Semi-structured interviews were conducted between November 2011 and February 2012. Where face-to-face interviews were not possible, telephone interviews were alternatively performed.
An interview guide was developed to ensure standardised and systematic data collection [14]. The interview guide was developed based on the study objectives and the literature pertaining to this subject area.
There were four main open-ended questions:
-
1.
What role can pharmacists play in weight management in the community?
-
2.
What training components does a pharmacist need to complete to provide weight management services?
-
3.
What should be included in a pharmacy-based weight management service model?
-
4.
Any other suggestions to help with implementation or barriers that need to be considered?
To establish face and content validity [14] the interview guide was piloted with a dietitian and a pharmacist. With minor amendments, the research team agreed the interview guide would accomplish the objectives of the study.
Data analysis
The digitally recorded interviews were transcribed verbatim and de-identified. The framework approach was chosen to analyse the data [15]. This involved five stages: familiarisation, identifying a thematic framework, indexing, charting, mapping and interpretation [15]. The transcripts were coded by one of the researchers, using an iterative process with the assistance of QSR NVivo 8 software (QSR International Pty Ltd). Emerging themes were then independently identified from the transcripts by another researcher. These were compared and discussed to develop a thematic framework. A consensus meeting was undertaken by the research team to finalise concepts and wording of the themes. Exemplar quotes were extracted to illustrate themes.
Results
In total 12 participants were interviewed. Each of the three pharmacy professional organisations nominated a national representative [Pharm]. Of the 16 experts in the sample pool, 9 experts were interviewed. The experts consisted of three dieticians (Diet), one psychiatrist (Psyc), two exercise physiologists (EP) and three physicians (Phys). After analysis of the transcripts six key themes emerged from the data.
-
Theme 1: The pharmacist is well positioned to address weight issues
All participants expressed the view that pharmacists play an integral and unique role in the community and that they conduct health-related interventions at an individual level and/or population level. They felt pharmacists can make a positive contribution to weight management and should become more involved. Several facilitators for the provision of weight management services in the community pharmacy setting were identified, including: accessibility, established rapport with individuals and scientific knowledge.
Pharmacists are underutilised… they are important players and they ought to be involved in these types of lifestyle related interventions [Psyc]
-
Theme 2: The pharmacist can provide both generic and personalised advice on weight control
The participants perceived two potential service models/roles for the pharmacist: targeted health promotion and individualised service.
Some participants considered that it would be beneficial for pharmacists to play a health promotion and education role in weight management due to their high exposure to the population. Furthermore, they recognised that a pharmacist’s position in the community allows for opportunistic encounters enabling the capture of individuals who may otherwise not be willing to seek weight management services.
Rather than non-specific public health campaigns such as poster displays and handing out of brochures, participants suggested pharmacists should target individuals and provide tailored advice around managing a healthy weight.
Pharmacists can target certain people and promote general healthy eating advice and physical activity. [Diet 1]
The use of a screening tool or a questionnaire was also suggested as an effective and practical way to engage individuals. Pharmacists could use this to help make specific recommendations and direct individuals to appropriate services.
Most participants perceived pharmacists could play a more pro-active and organised role in the individualised care of the person, provided that the pharmacist had been trained.
Pharmacists can provide a professional and formalised weight management service and give appropriate advice around dietetics and exercise requirements for individuals. [Phys 3]
-
Theme 3: The pharmacist should be involved in assessment, goal setting and ongoing support
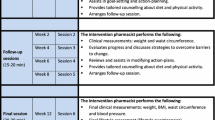
Many suggestions were made regarding what would be expected of the pharmacist conducting a weight management service. A general description is presented below, but a detailed summary of components suggested to be included in pharmacy-based weight management services in Australia is provided in Table 1.
All participants considered pharmacists could be involved in some assessment, which would help to identify individuals who may benefit from the intervention and also be an appropriate way of measuring outcomes.
With the appropriate equipment, pharmacists could take all necessary measurements like height, weight, waist… can also check blood glucose levels, medication list [Diet 2]
Participants also perceived pharmacists could have a role in developing realistic goals specific to the individual’s needs.
The best way is to form a partnership with the individual and help them to set goals and help to achieve them [Pharm 1]
Due to the chronic nature of obesity and the high probability of relapse after weight loss, participants recognised that pharmacists are ideally positioned to provide ongoing motivational support and follow-up sessions, which would help establish weight stability or maintenance.
Weight loss is not something that is short-term and there needs to be a maintenance phase… managing weight is life-long. [Phys 2]
-
Theme 4: The pharmacist should engage with other healthcare professionals on this issue
Participants identified the importance of pharmacists operating within a multi-disciplinary team in the community.
There needs to be appropriate referral pathways… some of these cases will not be able to be solely managed by the community pharmacist and you may well need to refer people to more intensive therapy or further investigation. [Phys 3]
-
Theme 5: The pharmacist requires formalised training and skill development in weight management
All participants expressed the need for pharmacists to undergo formalised training in weight management. They indicated stakeholders of the pharmacy profession should develop relevant competency standards for pharmacists involved in weight management. Some suggested with training and accreditation, a pharmacist could gain “advanced practitioner status,” which could serve as a means for the public and other healthcare professionals to recognise their proficiency in weight management.
Several training topics/skills were identified by the participants and have been categorised under headings: theory and practical skills.
Theory
-
Aetiology of overweight and obesity
-
Principles of weight loss
-
Benefits of weight loss
-
Emotional and psychological issues
-
Treatment: energy intake
-
Treatment: behaviour change
-
Pharmacotherapy
-
Over-the-counter (OTC) products and supplements
-
Weight maintenance
Practical skills
-
Communication
-
Motivational interviewing
-
Goal setting
-
Assessment
-
History taking
-
Measurement
-
Knowing when to refer
-
Theme 6: Some physical and financial barriers to pharmacists’ involvement in weight management currently exist
Participants identified some important organisational barriers to delivering pharmacy-based weight management services, including: infrastructure, pharmacists’ time, and cost-effectiveness. Concerns stemmed from practical considerations—the need for privacy in particular, the impact of such a service on work flow and financial outcomes. Some participants suggested that any intervention should have a cost-effectiveness analysis that defines set up costs, running costs and the likely profit for business.
Some pharmacies don’t have the private areas to discuss confidential issues. [Diet 6]
There needs to be a strong business case and financial modelling for pharmacy owners to take this up. [Pharm 3]
Discussion
This study set out to examine the opinions of various stakeholders about the potential role of pharmacists in weight management, the components of an appropriate weight management service within pharmacies and the level and type of training required to enable the implementation of an effective weight management service within community pharmacy. This study complements previous work conducted by our group exploring the opinions of consumers [11] and pharmacists [7] about issues that align with those under study. Our overall aim is to inform development of a best practice model for weight management services in community pharmacy, and identify the training and up-skilling required to assist with its effective implementation.
The documented responses of a range of experts in the field of obesity, together with representatives of professional organisations in pharmacy, indicated unanimous support for pharmacists’ involvement in weight management in the community. All participants identified that pharmacy-based weight management requires multi-component interventions that address all three lifestyle areas including diet, physical activity and psychology, which is consistent with evidence-based national and international clinical guidelines [4, 16, 17].
Two potential service models/roles for pharmacists involved in weight management were identified in this study: health promotion and individualised service.
Health promotion
Pharmacists are ideally positioned in the community to contribute to health promotion as they see the healthy, as well as the ill and their families [18]. Thus, pharmacists can contribute to the education and improvement of the overall health of the population [18]. On this premise, in 2005 the UK Department of Health developed a public health ‘care pathway’ for pharmacists in dealing with obesity, which included options to raise awareness, provide advice, refer as appropriate to specialist services and review progress [19]. Similarly, these components could be adapted into the Australian community pharmacy setting.
Individualised service
A review by Kirk et al. [20] evaluated the evidence for effective weight management practice and concluded that interventions should be designed and targeted to meet the needs of the individual. The pharmacist is a suitable healthcare professional to provide individualised care and tailored counselling [21]. As demonstrated in a study carried out in Switzerland (2002–2003) [22], where pharmacists were involved in delivering intensive counselling that included individualised weight reduction advice and goal setting on nutrition habits and physical activity. Participants (n = 568) who received intensive counselling achieved a significant weight loss at 3 months and 74.1 % had displayed changes in their lifestyle behaviours [22].
Based on the findings of this study, components to be included in pharmacy-based weight management services summarised in Table 1, appeared to be comprehensive and in line with international literature. Elements found to be effective in international pharmacy-based weight management trials and relevant clinical practice recommendations were perceived to suit the Australian community pharmacy setting in this model.
Furthermore, participants proposed that pharmacists should engage with other healthcare professionals when dealing with weight issues. Consumers in another study similarly expressed the need for a holistic and multi-disciplinary approach [11]. Pharmacists can positively contribute to a multi-disciplinary team, the effectiveness of which has been shown in The Lifestyle Challenge Program (USA) [23]. This program was co-directed by a pharmacist and also involved a physician specialising in nutrition, a behavioural psychologist and an exercise physiologist. Between April 2001 and April 2004, ninety participants entered into the program. Participants displayed reduction in weight and showed improvements in health-related quality of life, binge-eating behaviour and depressive symptoms.
All the experts interviewed in this study stressed the importance of up-skilling pharmacists and suggested they undergo a formal training program in weight management. Similarly, a systematic review of studies that had examined professionals’ experiences and perspectives of obesity, concluded that healthcare professionals may require additional support and training to ensure they provide good quality care [24].
The ten studies included in the systematic review by Gordon et al. [12] provided little information about the content of the weight management service providers’ training, except that the duration of training varied from 5 h to 2 days. Pharmacists involved in one study in the USA, underwent a 1-day training program that covered topics including: pathogenesis, non-pharmacologic interventions, drug therapy and physical assessments.
A postal survey to pharmacists in Grampian, Scotland (2009) [25] demonstrated that pharmacists’ perceived training needs included one-on-one consultation skills, counselling skills and advice on weight loss products and drugs, which is consistent with our findings. Another study in Texas, USA (2004) found obesity counselling by pharmacists was correlated with their comfort and confidence in achieving positive outcomes [26]. Therefore, training should focus on these communication skills and in increasing pharmacists’ comfort and confidence levels.
Some physical and financial barriers identified in this study such as infrastructure, pharmacists’ time, and cost-effectiveness were consistent with previous Australian studies that examined barriers to providing enhanced pharmacy services [21, 27]. Financial viability represents an additional but important layer in producing a sustainable model for community pharmacy. Roberts et al. [28] identified the key facilitators to practice change in Australian community pharmacies, including: relationship with physicians, remuneration, pharmacy layout, patient expectation, manpower/staff, communication and teamwork, and external support/assistance. For successful implementation of weight management services in pharmacy, these key facilitators need to be addressed in the future.
Limitations of the study
While participants provided rich data, this study presents some limitations. There was only one nominated national representative from each of the three main pharmacy professional organisations in Australia. However, these representatives were highly regarded members of their relative national boards and spoke on behalf of thousands of their constituencies. In addition, the experts in obesity were all from a single state in Australia (New South Wales), which may limit the generalisability of the data. Nevertheless, we purposefully selected these experts for their national and international reputations in their fields. Also, whilst it was considered that experts can comment on the required training competencies required by pharmacists, it is important to note that not all would be familiar with pharmacists’ skills and abilities. Therefore, we only reported those who were capable of answering the interview question. In addition, participants were uniform in their responses, hence no comparisons or distinctions between the groups were made between the experts’ and representatives’ feedback. As it was an exploratory study, the results were intended to inform future service development; therefore comparisons between the groups were not made.
Implications of research
Weight management services in community pharmacy already align with Australia’s future strategic directions for pharmacy. That is, the higher uptake of professional services [29, 30]. This study revealed the potential for pharmacists to be involved in two service roles/models: health promotion and individualised service. It is envisaged that findings of this study may inform the development of training for pharmacists providing weight management services, which may in turn provide basis for accreditation and remuneration. Future research is required to determine the feasibility and efficacy of the two potential service models in Australia, and further development of pharmacists’ training competencies.
Conclusion
Weight management is an increasingly pertinent issue that requires a multi-faceted approach. Pharmacists represent a valuable opportunity to promote healthy lifestyle and/or be involved in multi-disciplinary interventions. It is important for national health bodies and professional organisations to ensure weight management services provided by pharmacists are supported by current clinical evidence and best practice principles. Furthering pharmacists’ role would involve training and up-skilling; and addressing key practice change facilitators such as pharmacy layout and remuneration. Participants’ views expressed in this study may provide some insight into the design and implementation of a best practice model for pharmacy-based weight management programs in Australia.
References
Obesity and Overweight Fact Sheet No 311. World Health Organization; (updated 2012 May; cited 2013 Jan 21); Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
4364.0—National Health Survey: Summary of Results, 2007–2008 (Reissue). Australian Bureau of Statistics; (updated 2009 Aug; cited 2013 Jan 21); Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4364.0Main+Features12007-2008 (Reissue)?OpenDocument.
Australia: The Healthiest Country by 2020. Technical Report No 1: Obesity in Australia: A Need For Urgent Action. Prepared for the National Preventative Health Taskforce by the obesity working group. Barton, ACT: Commonwealth of Australia; 2008 (cited 2013 Jan 21); Available from: http://www.health.gov.au/internet/preventativehealth/publishing.nsf/Content/E233F8695823F16CCA2574DD00818E64/$File/obesity-jul09.pdf.
Clinical Practice Guidelines For The Management Of Overweight And Obesity In Adults. Prepared by the National Health And Medical Research Council. Canberra, ACT: Commonwealth of Australia; 2003 (updated 2004 Mar; cited 2013 Jan 21); Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/7AF116AFD4E2EE3DCA256F190003B91D/$File/adults.pdf.
Parliament of Australia House of Representatives Standing Committee on Health and Ageing. Inquiry into Obesity in Australia. Submission No. 82. Submission by the Pharmaceutical Society of Australia. Curtin, ACT: Pharmaceutical Society of Australia; 2008 [cited 2013 Jan 21]; Available from: http://www.aph.gov.au/house/committee/haa/obesity/subs/sub082.pdf.
Annual Report 2005–2006. Prepared by the Department of Health and Ageing. Canberra, ACT: Commonwealth of Australia; 2006 (cited 2013 Jan 21); Available from: http://www.health.gov.au/internet/annrpt/publishing.nsf/Content/56552835C4A23BE7CA257210002452B2/$File/1 Annual Report.pdf.
Um IS, Armour C, Krass I, Gill T, Chaar BB. Managing obesity in pharmacy: the Australian experience. Pharm World Sci. 2010;32(6):711–20.
Rieck A, Clifford R, Everett A. Community pharmacy weight management project. Stages one and two. The University of Western Australia; 2005 (updated 2006 Apr; cited 2013 Jan 21); Available from: http://www.guild.org.au/iwov-resources/documents/The_Guild/PDFs/CPA and Programs/3CPA General/2005-522/2006-05-29 CPWMP Final.pdf.
Anderson C, Blenkinsopp A, Armstrong M. Feedback from community pharmacy users on the contribution of community pharmacy to improving the public’s health: a systematic review of the peer reviewed and non-peer reviewed literature 1990–2002. Health Expect. 2004;7:191–202.
Eades CE, Ferguson JS, O’Carroll RE. Public health in community pharmacy: a systematic review of pharmacist and consumer views. BMC Public Health. 2011;11:582–94.
Um IS, Armour C, Krass I, Gill T, Chaar BB. Consumer perspectives about weight management services in a community pharmacy setting in NSW, Australia. Health Expect. 2012. doi:10.1111/j.1369-7625.2012.00788.x
Gordon J, Watson M, Avenell A. Lightening the load? A systematic review of community pharmacy-based weight management interventions. Obes Rev. 2011;12:897–911.
Liamputtong P, Ezzy D. Qualitative research methods. 2nd ed. South Melbourne, VIC: Oxford University Press; 2005.
Patton MQ. Qualitative evaluation and research methods. 2nd ed. Newbury Park: Sage Publications; 1990.
Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. Br Med J. 2000;320:114–6.
NICE clinical guideline 43. Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. Prepared by the National Collaborating Centre for Primary Care and the Centre for Public Health Excellence at NICE. London, UK: National Institute of Health and Clinical Excellence; 2006 (updated 2012 May; cited 2013 Jan 21); Available from: http://www.nice.org.uk/nicemedia/pdf/CG43NICEGuideline.pdf.
SIGN Guideline 115: Management of Obesity. A national clinical guideline. Edinburgh, Scotland: Scottish Intercollegiate Guidelines Network; 2010 (cited 2013 Jan 21); Available from: http://www.sign.ac.uk/pdf/sign115.pdf.
Anderson C. Health promotion in community pharmacy: the UK situation. Patient Educ Couns. 2000;39:285–91.
Choosing health through pharmacy—a programme for pharmaceutical public health 2005–2015. Prepared by the Department of Health. London, UK: Crown; 2005 (cited 2013 Jan 21); Available from: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4107496.pdf.
Kirk SFL, Penney TL, McHugh T-LF, Sharma AM. Effective weight management practice: a review of the lifestyle intervention evidence. Int J Obes. 2012;37:178–85.
McMillan SS, Wheeler AJ, Sav A, King MA, Whitty JA, Kendall E, et al. Community pharmacy in Australia: a health hub destination of the future. Res Social Adm Pharm. 2012. doi:10.1016/j.sapharm.2012.11.003
Botomino A, Bruppacher R, Krahenbuhl S, Hersberger K. Change of body weight and lifestyle of persons at risk for diabetes after screening and counselling in pharmacies. Pharm World Sci. 2008;30:222–6.
Malone M, Alger-Mayer S, Anderson D. The lifestyle challenge program: a multidisciplinary approach to weight management. Ann Pharmacother. 2005;39:2015–20.
Mold F, Forbes A. Patients’ and professionals’ experiences and perspectives of obesity in health-care settings: a synthesis of current research. Health Expect. 2011. doi:10.1111/j.1369-7625.2011.00699.x
Newlands RS, Watson MC, Lee AJ. The provision of current and future Healthy Weight Management (HWM) services from community pharmacies: a survey of community pharmacists’ attitudes, practice and future possibilities. Int J Pharm Pract. 2011;19:106–14.
Dastani HB, Brown CM, O’Donnell DC. Combating the obesity epidemic: community pharmacists’ counseling on obesity management. Ann Pharmacother. 2004;38:1800–4.
Berbatis CG, Sunderland VB, Joyce A, Bulsara M, Mills C. Enhanced pharmacy services, barriers and facilitators in Australia’s community pharmacies: Australia’s National Pharmacy Database Project. Int J Pharm Pract. 2007;15:185–91.
Roberts AS, Benrimoj SI, Chen TF, Williams KA, Aslani P. Practice change in community pharmacy: quantification of facilitators. Ann Pharmacother. 2008;42:861–8.
Pharmaceutical Society of Australia. Issues paper on the future of pharmacy in Australia. 2010 (cited 2013 Jan 21); Available from: http://careers.curtin.edu.au/data/shared/documents/faculty_specific_resources/health_sciences/psa_future_of_pharmacy2010.pdf.
The Pharmacy Guild of Australia. The roadmap: the strategic direction for community pharmacy. 2010 (cited 2013 Jan 21); Available from: http://www.guild.org.au/iwov-resources/documents/The_Guild/PDFs/News and Events/Publications/The Roadmap/Roadmap.pdf.
Acknowledgments
The Author(s) would like to thank the participants who took part in this study.
Funding
The Authors declare that no external funding has been obtained for the study.
Conflicts of interest
The Author(s) declare(s) that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Um, I.S., Armour, C., Krass, I. et al. Weight management in community pharmacy: what do the experts think?. Int J Clin Pharm 35, 447–454 (2013). https://doi.org/10.1007/s11096-013-9761-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-013-9761-4