Abstract
Objective To determine UK non-medical prescribers’ (NMPs) (supplementary or independent) current participation and self-reported competence in pharmacovigilance, and their perceptions of training and future needs. Setting Non-medical prescribers in health care in the United Kingdom. Awareness of and participation in the Yellow Card Scheme (YCS); attitudes towards ADR reporting; strategies to encourage reporting; pharmacovigilance training; and demographics. The sample comprised nurse (n = 912) and pharmacist (n = 2,439) NMPs in the UK. Main outcome measures Self-reported competence in pharmacovigilance, knowledge of and participation in the YCS, attitudes towards ADR reporting; strategies to encourage ADR reporting; pharmacovigilance training during NMP training. Results Six hundred and thirteen responses were received giving an overall response rate of 20.4 %. Response rates for nurse and pharmacist prescribers were 32.2 % (n = 293) and 13.1 % (n = 320) respectively. Three hundred and fifty-nine respondents (58.6 %) had submitted a Yellow Card. Although the majority of respondents (70.4 %) felt competent in pharmacovigilance, a third (34.2 %) said they needed further training. Respondents reported a positive attitude towards ADR reporting, yet only a minority (22.9 %) correctly answered factual questions about the YCS. Approximately a third of respondents (35.6 %) “couldn’t remember” if pharmacovigilance was covered in their prescribing training. Publicity and education were commonly suggested measures to enhance contribution to the YCS. Conclusion While NMPs report participation and competence in ADR reporting, there are several key issues to consider including the need for further training and support to optimise their role in pharmacovigilance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact of findings on practice
-
There appears to be a need for higher education providers of non-medical prescribing in the UK to review the pharmacovigilance content of their courses.
-
Health professionals need to be encouraged to report ADRs via the YCS.
Introduction
Pharmacovigilance, defined by the World Health Organisation as ‘the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug related problems’, plays a key role in defining the safety of modern healthcare practice [1].
In the UK the ‘Yellow Card Scheme’ (YCS) is the principal process for reporting spontaneous suspected adverse drug reactions (ADRs), and receives reports from health professionals, patients and members of the general public [2].
Under reporting of ADRs by healthcare professionals is a key limitation for all spontaneous ADR reporting schemes, with only 6–10 % of serious ADRs being reported in the UK [3, 4].
The last decade has seen a drive towards the implementation of non-medical prescribing in the UK, with supplementary and independent prescribing by nurses and pharmacists [5, 6]. While supplementary prescribers can manage any diagnosed condition and prescribe any drug as defined by a patient-specific clinical management plan, independent prescribers can prescribe any drug (with the exception of controlled drugs which NMPs other than nurses and pharmacists may not prescribe) for both diagnosed and undiagnosed medical conditions. At present there are approximately 20,000 nurse and 2,400 pharmacist supplementary/independent prescribers (non-medical prescribers, NMPs) in the UK. NMPs undertake a training programme which includes pharmacovigilance [7] and a potential outcome could be enhanced participation in the YCS.
There are only data on the participation of nurses and pharmacists in ADR detection, monitoring and reporting [8–12] none relating to other NMPs.
Aim of the study
The aim of this study was to determine current participation and competence of NMPs in pharmacovigilance, and their perceptions of training and future needs.
Methods
A draft questionnaire was developed based on information from UK Medicines and Healthcare products Regulatory Agency policies and processes relating to the YCS, and prescribing roles of NMPs. The draft questionnaire was reviewed for face and content validity by the research team and a panel of academics and practitioners. The questionnaire was piloted on a sample of 148 NMPs [68 nurse prescribers sampled from the Association for Nurse Prescribing (ANP) and 80 pharmacist prescribers in two geographical regions of Scotland]. No amendments were made to the questionnaire post piloting.
The final questionnaire contained items in five domains: (1) awareness of and participation in YCS processes (ADR reporting, drug withdrawals, changes in marketing authorisation etc. (15 items); (2) pharmacovigilance training received as NMPs and perceptions on the value of this training (10 items); (3) attitudes towards their role in pharmacovigilance (14 items); (4) methods of enhancing NMP contribution to pharmacovigilance (4 items); and (5) demographics (practice and personal, 12 items).
A mix of open and closed question types were used with 5-point Likert scales for attitudinal statements. The questionnaire was developed following best practice [13, 14] using Snap 10 Professional® (software for web and email questionnaire design, publication, data entry and analysis) and presented as a web-based survey hosted online.
The full study sample was: all supplementary and independent pharmacist prescribers (n = 2,439, January 2011); and all supplementary and independent nurse prescribers registered with the ANP (n = 912, January 2011). Emails were sent directly by the ANP and other continuing education organisations/centres to pharmacist and nurse prescribers using text provided by the research team. Two reminder emails were sent, a week apart. The survey was live from January to May 2011.
The survey instrument generated anonymised emails of online submissions to the research team. These were imported into Snap before direct export to SPSS (SPSS Inc., Cary, NC version 17.0). Quantitative data were analysed using descriptive statistics to fully describe participants, their current pharmacovigilance training, prescribing setting, process and participation in pharmacovigilance etc. Chi squared was used to test for any association between nurse/pharmacist and pharmacovigilance training; prescribing setting/perceptions of competence and Yellow Card reporting. p values ≤0.05 were considered significant.
Open comments were analysed thematically. After familiarisation with the data, emerging themes were identified and data coded. Two researchers (VP and KM) independently verified the themes with any disagreement being reviewed by other members of the research team. Illustrative quotes are provided for each theme with respondents (nurse prescriber, NP and pharmacist prescriber, PP) allocated a consecutive number.
The North of Scotland Research Ethics Committee advised that the project did not require formal ethics committee review.
Results
Six hundred and thirteen responses were received giving an overall response rate of 20.4 %. Response rates for nurse and pharmacist prescribers were 32.2 % (n = 293) and 13.1 % (n = 320) respectively. Three hundred and eighty-seven responses (63.1 %) were from England, 167 (27.2 %) from Scotland, 31 (5.1 %) from Wales and 28 (4.6 %) from Northern Ireland.
The majority were female (81.9 %, 502) and aged over 35 years (86.4 %, 530). Three quarters had been registered as supplementary prescribers for more than 4 years (75.9 %, 465) with almost half as independent prescribers for the same period (48.1 %, 295). There was equal representation of those practising in primary (29.7 %, 182) and secondary care settings (29.2 %, 179).
To establish the homogeneity of respondents, the demographic characteristics of the first and last 50 respondents were compared. These two sub-groups were similar in terms of gender, years of experience as health professionals and time since registration as NMPs.
When asked about NMP course content, just over half of respondents (57.2 %, 351) recalled specific pharmacovigilance training. Perceptions of aspects of training are reported in Table 1.
While the levels of difficulty and course duration were reported as ‘appropriate’, 32 (9.1 %) gave an ‘inappropriate’ rating for the emphasis on the legal implications of pharmacovigilance. Forty-nine respondents (13.9 %) rated the relevance to prescribing practice as ‘irrelevant’. The duration of pharmacovigilance training throughout the NMP course varied from 1 to 6 hours.
Of note 7.2 % (44) of respondents did not receive training in pharmacovigilance and 35.6 % (218) were unable to remember. A greater proportion of nurse prescribers than pharmacist prescribers recalled training in pharmacovigilance (p < 0.001).
When asked about competence and training needs in pharmacovigilance (Table 2), 70.3 % (431) disagreed that they were competent in all aspects of pharmacovigilance and 34.2 % (210) agreed that they required further training.
A common theme highlighted by the majority of respondents in relation to lack of competence was the need for continuous training and regular updates.
As one pharmacist prescriber noted,
I think that it is very important to have ongoing pharmacovigilance training for prescribers and all health care professionals to improve reporting and awareness [PP 266],
while one nurse prescriber commented,
the medical world moves on. I have been offered very little relevant training since gaining my prescribing qualification and have been offered no specific training in this area. [NP 342]
Almost a third of respondents (28.5 %, 175) stated that ‘experience as a health professional’ had provided them with all the pharmacovigilance training they required.
When given a series of statements to rate their knowledge of the YCS (Table 3) only one-fifth (22.8 %, 140) answered all questions correctly. More than half of respondents (52.4 %, 321) incorrectly stated that all suspected ADRs in adults should be reported. 13.4 % (82) incorrectly stated the requirement to determine causality prior to reporting. Those respondents agreeing that they were competent in pharmacovigilance were more likely to answer all questions correctly (p < 0.005).
Just over half (58.6 %, 359) of respondents had submitted a Yellow Card, 46.3 % (284) prior to NMP training and 28.7 % (176) since qualifying as an NMP. Pharmacist prescribers were significantly more likely than nurse prescribers to have reported an ADR via the YCS (p < 0.001), as were those working in primary care medical practices and secondary care when compared to those in community pharmacy/nursing practice.
Of those who could recall submitting a Yellow Card, the most common drug classes involved were cardiovascular (7.8 %, 28), vaccines (7.2 %, 26), anti-infectives (5.8 %, 21), smoking cessation treatments (5.3 %, 19) and non-steroidal anti-inflammatory drugs (4.2 %, 15).
Thirty-four respondents (9.5 %) reported that following their Yellow Card submission they subsequently avoided prescribing that particular drug.
Key reasons given by respondents for not submitting a Yellow Card, despite having recognised an ADR, were lack of time to report and uncertainty over who was responsible for reporting, as highlighted in the following quotes.
not a deliberate omission. Usually comes about in the consult and you are so busy doing everything else you don’t register that you need to report it. [PP 12]
my previous experiences of reporting have been time consuming - the information needed is not always readily available and easy to obtain. Also sometimes more information is requested and the process puts increased pressure on an already stressful and busy workload. [NP 484]
it was a clear ADR but I felt it was not my position to report it and felt not as capable as others to do so as I was less experienced and not prescribing at that time. [NP 269]
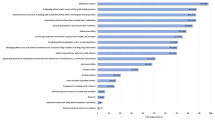
Three quarters of respondents (72.4 %, 444) commented on methods to encourage reporting, highlighting their perceived need to improve the reporting system, particularly the provision of feedback on reports submitted.
I would like to be clearer about which drugs to report on the Yellow Card system as I feel my uncertainty puts me off reporting. [PP 576]
clear information about when it is necessary to report ADRs. Clear feedback on the result of a report. Links within prescribing/pharmacy software. Incentives/encouragement from pharmaceutical company representatives. [PP 515]
I think ease of use on computer as most people and healthcare professionals have to use this, also maybe a monthly reminder sent by email with attachment to the appropriate form for the yellow card to report any ADRs as a memory jolt. [NP 293]
clearly defined responsibility by trust as to which member of a patient’s care team is responsible for this. Developing an iPhone App to enable easy, rapid bedside reporting. [PP 216]
The majority (62.8 %, 385) of respondents expressed the need to enhance health professional and patient awareness of patient reporting.
patients don’t have a clue and its about awareness - posters in pharmacies would be a start [PP 107]
I don’t believe that patients/general public are aware that they can report adverse effects. I have never known a health care professional (including myself) inform the patient that they can do this or how to access the reporting scheme. [PP 150]
Responses to attitudinal items on pharmacovigilance are given in Table 4. Of note, 22.1 % (135) agreed that they were reluctant to submit a Yellow Card without evidence of causality. Almost half (48.1 %, 295) agreed that responsibility for submitting Yellow Cards was enhanced with their prescribing status yet only 17.7 % (109) agreed that their ADR reporting activity had increased since qualifying as a prescriber. Under a fifth (16.2 %, 99) also agreed that they often forgot the need to report ADRs and 35.1 % (215) were concerned about the potential legal implications arising if a drug they had prescribed had caused an ADR.
When asked who should take responsibility for contacting a patient in the event of a drug which they had prescribed being withdrawn from the market, the majority (79.1 %, 485) acknowledged that it was their responsibility. Similarly, most respondents (75.2 %, 461) would take responsibility for switching the patient to another medication.
Discussion
This is the first study to determine NMP participation in pharmacovigilance, perceptions of training, competence and future needs.
Over one-third of respondents could not recall pharmacovigilance being covered during their NMP training. While almost half agreed that their responsibility for submitting Yellow Cards was enhanced with their prescribing status, less than one-fifth agreed that their ADR reporting activity had actually increased since qualifying as a prescriber. Around 10 % did not feel competent in all aspects of pharmacovigilance and more than a third were concerned about potential legal implications if a drug they prescribed caused an ADR. Key themes were identified from responses to open questions indicating a need for: constant reminders of the need to monitor and report ADRs using the YCS; the provision of feedback following a Yellow Card submission; and a heightened awareness of the YCS for health professionals and patients.
However, findings should be interpreted with caution as our response rate was low compared with previous surveys of NMPs where response rates have exceeded 70 % [15–17]. Several factors may have contributed to this low response rate including failure of regulatory bodies (Nursing and Midwifery Council and General Pharmaceutical Council) to assist with the study, citing data protection issues. Furthermore, previous surveys have identified a substantial number of NMPs who have never prescribed [15–17] and it is possible that those with no prescribing experience may have been less likely to participate in this survey. Response and recall biases may reduce the generalisability of our findings to the population of NMPs in the UK. However, while we were unable to compare respondents to non-respondents, there is some evidence to suggest that late respondents may be similar in key respects to the non-respondent population [18]. We identified little difference between ‘early’ and ‘late’ respondents suggesting that response bias may be less of be an issue. We are also aware of the potential for social desirability bias where respondents may have given expected, anticipated answers [19].
Many of the issues identified by NMPs in this study are similar to those previously reported for medical prescribers. These issues include ignorance (unaware that only serious ADRs need to be reported); diffidence (fear of appearing ridiculous for reporting merely suspected ADRs); lethargy (procrastination, lack of interest or time to report); indifference (making little contribution to medical knowledge) and insecurity (certainty of drug causing ADR) [20].
To ensure optimisation of their contribution to medicines safety, NMPs should have a complete understanding of pharmacovigilance and the YCS. Our results, however, indicate the need for providers of NMP training to review the coverage of pharmacovigilance within their courses. While respondents voiced the need for further education and training on legal aspects of pharmacovigilance, our findings indicate that areas of adverse drug reaction causality, potential for litigation and assurances of confidentiality require particular attention. As previously demonstrated by Bracchi et al. [12], focused education and training in pharmacovigilance can enhance ADR reporting participation. Similarly, Green et al. [9] highlighted that pharmacovigilance related education and training was the only predictor of reporting in their survey of hospital pharmacists.
Despite issues of pharmacovigilance training, almost half of the respondents had submitted a Yellow Card, although for many the last submission had pre-dated their NMP training. Pharmacists were more likely than nurses to have reported, a finding which may be explained by their training in clinical pharmacology and medicines usage.
Similarly, those in community practice (nursing and pharmacy) were less likely than those based in primary or secondary care medical practice to have reported an ADR, perhaps due to lone working and the lack of peer support networks. Professional experiences of an ADR appeared to impact significantly on subsequent prescribing practice with respondents commenting that they would refrain from prescribing that particular drug in future. Such observations are of interest given the accepted low ranking of personal experience within the hierarchy of evidence based practice [21].
Our findings are not unique to the UK, and are similar to those of Gavaza et al. [22], who recently reported on the attitudes of Texan pharmacists to serious ADR reporting to the Food and Drug Administration. While pharmacists believed that reporting would enhance patient safety, they also indicated that reporting was time consuming and disrupted normal workflow. Hospital pharmacists had more positive attitudes towards reporting compared to their community based counterparts.
Respondents in our study suggested that Yellow Card reporting would be enhanced by coverage in continuing professional development activities, reminders of the YCS being embedded within prescribing software or the application of other reporting systems using technologies such as mobile phones.
Greater NMP awareness of patient and public reporting appears warranted. A recently published report found that patient reporting of ADRs added value to those reported by healthcare professionals by providing information on different types of drugs and reactions [23].
There is a need for further research on NMPs in the field of pharmacovigilance using qualitative methodologies to explore key areas including: perceptions of competence; related medico-legal issues; potential to enhance the YCS; and perceptions of the usefulness and utility of patient reporting. A prospective audit of the completeness and nature of NMP Yellow Card reports is warranted. This would require a modification of the Yellow Card to allow recording of NMP status.
Conclusion
In conclusion, while NMPs report participation in ADR reporting, there are several key issues to consider including the need for further training and support to optimise their role in pharmacovigilance.
References
Meyboom RGB. Data assessment in pharmacovigilance. [cited Sept 2011] http://www.ikev.org/haber/farmakovijilans/Meyboom%20Data%20Assessment.pdf.
Medicines and Healthcare products Regulatory Agency. Yellow card, helping to make medicines safer. [cited Sept 2011] http://yellowcard.mhra.gov.uk/.
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29(5):296–385.
Lindquist M. Data quality management in pharmacovigilance. Drug Saf. 2004;27(12):857–70.
Department of Health. Supplementary prescribing by nurses, pharmacists, chiropodists/podiatrists, physiotherapists and radiographers within the NHS in England: a guide for implementation 2005. Department of Health, London.
Department of Health. Improving patients’ access to medicines: a guide to implementing nurse and pharmacist independent prescribing within the NHS in England 2006. Department of Health, London.
Stewart D, MacLure K, George J. Educating non medical prescribers. Brit J Clin Pharm. 2012;74(4):662–7.
Sweis D, Wong IC. A survey on factors that could affect adverse drug reaction reporting according to hospital pharmacists in Great Britain. Drug Saf. 2000;23(2):165–72.
Green CF, Mottram DR, Rowe PH, Pirmohamed M. Attitudes and knowledge of hospital pharmacists to adverse drug reaction reporting. Brit J Clin Pharm. 2001;51:81–6.
Morrison-Griffiths S, Walley T, Park BK, Breckenridge AM, Pirmohamed M. Reporting of adverse drug reactions by nurses. Lancet. 2003;361:1347.
Sri Ranganathan S, Houghton JE, Davies DP, Routledge PA. The involvement of nurses in reporting suspected adverse drug reactions: experience with the meningococcal vaccination scheme. Brit J Clin Pharm. 2003;56:658–63.
Bracchi RCG, Houghton J, Woods FJ, Thomas S, Smail SA, Routledge PA. A distance-learning programme in pharmacovigilance linked to educational credits is associated with improved reporting of suspected adverse drug reactions via the UK yellow card scheme. Br J Clin Pharm. 2005;60(2):221–3.
McColl E, Jacoby A, Thomas LN, Soutter J, Bamford C, Steen N, et al. Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients. Health Technol Assess. 2001;5(31):1–256.
Edwards PJ, Roberts I, Clarke M, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst. Rev. 2009;Jul 8(3).
George J, McCaig D, Bond C, Cunningham ITS, Diack HL, Watson AM, et al. Supplementary prescribing: early experiences of pharmacists in Great Britain. Ann Pharmacother. 2006;40:1843–50.
George J, McCaig D, Bond C, Cunningham S, Diack L, Stewart D. Benefits and challenges of prescribing training and implementation: perceptions and early experiences of RPSGB prescribers. Int J Pharm Pract. 2007;15:23–30.
Courtenay M, Carey N, Burke J. Independent extended and supplementary nurse prescribing practice in the UK: a national questionnaire survey. Int J Nurs Stud. 2006;44(7):1093–101.
Bowling A. Methods in health research. Buckingham: Open University Press; 2002.
Fisher RJ. Social desirability bias and the validity of indirect questioning. J Consum Res. 1993;20(2):303–15.
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2009;32:19–31.
Thomas G, Pring R. Evidence-based practice in education. Berkshire: Open University Press; 2004.
Gavaza P, Brown CM, Lawson KA, Rascati KL, Wilson JP, Steinhardt M. Influence of attitudes on pharmacists’ intention to report serious adverse drug events to the Food and Drug Administration. Br J Clin Pharm. 2011;71(1):143–52.
Avery A, Anderson C, Bond C, Fortnum H, Gifford A, Hannaford PC, et al. Evaluation of patient reporting of adverse drug reactions to the UK ‘Yellow Card Scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess 2011;15(20):1–234.
Acknowledgments
We acknowledge the contribution of the following organisations to recruiting nurse and pharmacist prescribers: Association for Nurse Prescribing; NHS Education for Scotland; Centre for Postgraduate Pharmaceutical Education; Northern Ireland Centre for Pharmacy Learning and Development; Welsh Pharmacy Board; National Prescribing Centre; and Royal Pharmaceutical Society. We are also grateful to those nurse and pharmacist prescribers who participated in the research.
Funding
The UK Medicines and Healthcare products Regulatory Agency (MHRA) funded this research.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stewart, D., MacLure, K., Paudyal, V. et al. Non-medical prescribers and pharmacovigilance: participation, competence and future needs. Int J Clin Pharm 35, 268–274 (2013). https://doi.org/10.1007/s11096-012-9739-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9739-7