Abstract
Background Type 2 diabetes is highly prevalent among people of Pakistani background. Studies show that adherence to medicines is complicated for people with type 2 diabetes in general. Also, studies indicate that many people with type 2 diabetes and Muslim background fast during the month of Ramadan without adequate counselling on how to adjust their medicines. Objective To explore patient perspectives on medicine use during Ramadan, reasons for fasting and experiences with counselling on medicine use during Ramadan among people of Pakistani background with type 2 diabetes and at least one other chronic condition. Setting Greater Copenhagen, Denmark. Method The analysis is based on a study exploring lived experiences with counselling on medicines using semi-structured interviews and medication reviews. The analysis presented here builds on the subset of patients with Pakistani background (six interviewers). Results All interviewees pointed out that Islam allows ill people to refrain from fasting during Ramadan. However, all had fasted during Ramadan despite being diagnosed with type 2 diabetes. While fasting, they adapted their use of medicines in different ways, e.g. by changing the time of intake or by skipping morning medicines. Fasting during Ramadan meant a feeling of improvement in well-being for all interviewees. Reasons for this improvement included physiological, social and religious aspects. Healthcare professionals were rarely included in the decision-making process on whether or not to fast. Instead, friends and relatives, especially those with type 2 diabetes, were considered important to the decision-making process. Conclusion For people with Muslim background and a chronic condition, fasting during Ramadan may mean changes in medicine use that are not always discussed with healthcare professionals. Healthcare professionals should acknowledge that Muslim patients may find fasting during Ramadan beneficial to their well-being and therefore choose to fast despite the Islamic rule of exemption. This patient-centred approach to counselling on medicines may facilitate better medicine use and thus better clinical health outcomes among patients that choose to fast.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Ramadan fasting may mean changes in use of medicines among people of Muslim background with type 2 diabetes.
-
Patients with Diabetes Type-2 may experience that fasting, including refraining from taking medicines, improves their well-being for physiological, social and religious reasons.
-
Healthcare professionals should bear in mind that fasting is the patient’s individual choice based on the physiological, social and religious aspects of fasting.
Introduction
The prevalence of type 2 diabetes among people of Pakistani background living in Western countries is high [1, 2]. In general, adherence to medicines is impeded for people with type 2 diabetes due to co-morbidity, complex treatment regimens, and long-term disease duration causing more drug-related problems and negative health outcomes [3, 4]. While adherence to medicine regimens may be impeded for people with type 2 diabetes in general, some ethnic groups with this condition may encounter additional challenges for optimal medicine use.
Fasting during the month of Ramadan is one aspect that may influence counselling on medicines to people of Muslim background with type 2 diabetes. Ramadan fasting, which means abstaining from the intake of all foods, beverages etc. that enter the intestinal system from dawn to sunset, is generally considered obligatory for every responsible, healthy Muslim [5]. Although the Quran can be interpreted in different ways, a number of categories of people are generally considered exempt from fasting, including people with chronic conditions (due to what can be called the ‘rule of exemption’) [5]. Abstaining from taking oral medicines is generally considered part of fasting, but it is debated whether or not medicines entered directly into the blood stream (e.g. insulin injections) break the fast [5]. Little is known about how people with type 2 diabetes with Pakistani background relate to such theological debates on fasting in their everyday lives [6], specifically whether they consider themselves exempt from fasting and whether and why they choose to fast.
Several studies have explored the biomedical health effects of Ramadan fasting for people with type 2 diabetes. Some studies show no health effects, some show negative effects (mainly hypoglycaemia) and some show positive effects (weight loss and reduced waist circumference) [5, 7]. A literature review concludes that fasting is acceptable for people with well-balanced type 2 diabetes who are compliant regarding diet and medicines, and that fasting is possible for other categories of people with type 2 diabetes [7]. This is supported by more recent studies as well as recommendations for practice, which conclude that fasting is clinically acceptable for most people with type 2 diabetes who receive counselling on use of medicines and glucose monitoring while fasting [8–10].
The prevalence of Ramadan fasting among people with Pakistani background and type 2 diabetes living in Europe is not well known. A Norwegian study among immigrants from Pakistan who used antihypertensives, cholesterol-lowering drugs and/or anti-diabetics showed that nearly half of them fasted [11]. A population-based study in countries with the majority population being Muslim found that 79 % of people with type 2 diabetes fasted [12]. Approximately 25–33 % of users of insulin or oral anti-diabetics changed their medication while fasting [12].
Few studies have explored why Muslims with type 2 diabetes decide to fast during Ramadan [6, 13, 14]. A British study of people of Pakistani background found that almost all respondents did fast, albeit to varying degrees [6]. Fasting was seen as a practice that is malleable to the potential of the individuals following it [6]. In a Swedish study among people of Somali background, the interviewees did not consider Ramadan fasting compulsory for people with type 2 diabetes, and some found fasting beneficial to health [14]. In a French study among Muslim inpatients with diabetes, the respondents consulted relatives much more frequently than their general practitioners regarding whether or not to fast [13]. Consulting the general practitioner did not have major impact on the final decision on fasting [13]. These studies suggest that from a patient perspective fasting can be considered beneficial, and that communication with healthcare professionals about how to use medicines while fasting could be improved. However, knowledge is still limited as to why fasting is sometimes experienced as beneficial, and why relatives might be consulted more often than healthcare professionals.
Over the last few decades, the ideal for counselling on medicines has shifted from compliance (the patient must take the medicines as prescribed) to adherence (the patient and the healthcare professional must reach a common agreement) and concordance (the relationship between the healthcare professional and the patient) [4, 15]. This shift means a change from a dictatorial, hegemonic relationship between patient and professional to a partnership where the two develop a treatment plan in which the patient’s values, perspectives and competencies are a central component [15]. A counselling setting with room for the patient to raise concerns about the treatment, including concerns about the implementation of the treatment plan, is considered more likely to improve patient health compared to a more dictatorial, one-way communication from the healthcare professional [4, 15]. The inclusion of patient perspectives on medicine use during Ramadan is an example of counselling conducted on the basis of concordance and adherence.
Theoretical background
The concepts of adherence and concordance illustrate the importance for healthcare professionals to know more about the rationales underlying patients’ use of medicines. In understanding this patient perspective, we have been inspired by the anthropologist Arthur Kleinman’s distinction between disease (the healthcare professional’s understanding) and illness (the patient’s understanding) [16, 17]. According to Kleinman, healthcare professionals may tend to refer to a biomedical paradigm with emphasis on clinically relevant measures and outcomes (e.g. blood sugar levels), which may lead to counselling sessions with little emphasis on why and how patients may choose to fast during Ramadan. The patient, on the other hand, understands his/her illness from an everyday perspective where the diagnosis is just one among many aspects of his/her identity, and where illness is situated in the context of everyday life [16, 18].
Aim of the study
The aim of this study is to explore patient perspectives on medicine use during Ramadan, reasons for fasting, and experiences with counselling on medicines among people of Pakistani background with type 2 diabetes and at least one other chronic condition.
Methods
Interview study
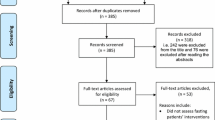
The analysis is based on a study exploring lived experiences regarding counselling on medicines among people of Danish and Pakistani background living in greater Copenhagen, Denmark, who have type 2 diabetes and at least one other chronic condition. The co-morbidity inclusion criteria was chosen in order to reflect the high prevalence of other chronic conditions among people with type 2 diabetes, which generally impedes adherence to medicines [3, 4]. Data included semi-structured, face-to-face interviews and medication reviews conducted in April–May 2010. Recruitment took place in a local community, a mosque and by snowballing in a purposive strategic sampling process.
The interviews were based on a hermeneutic approach that explored the interviewees’ understandings and life worlds by asking questions related to concrete practices and their perspectives on these practices, and thereby inviting answers about concrete behaviour and perceptions but also about related themes that each interviewee find important to raise in a discussion on counselling on medicines [19]. Since interviews explored the lived experiences situated in the context of everyday life, the theme of experiences related to Ramadan emerged from data during analysis. The analysis is conducted as a secondary analysis of a subset of patients. Because of the topic of Ramadan, only people of Pakistani background, all of whom were Muslims, were included is this analysis (Table 1). The analysis centred on exploring responses to questions about concrete practices regarding medicines during Ramadan. Four out of the six interviews included data on Ramadan.
Living with type 2 diabetes varied from 3 to 20 years, and current anti-diabetics being used included metformin, insulin and/or sitagliptin. Hypertension and hypercholesterolaemia were frequent complementary diagnoses, but all interviewees had other somatic and/or psychiatric conditions as well (Table 1). All six interviewees were retired, most of them through early retirement due to health problems. Five of them had no formal education from Denmark and had worked as unskilled workers whereas one was trained in early childhood education and had worked in the field most of her working life.
Interpreting
A pharmacy master’s student conducted the medication reviews. She was fluent in Danish, Urdu and Punjabi and also attended all interviews as interpreter. Each interviewee chose the language(s) used during interviews. Prior to the field work, the interpreter received basic interpreter training. Interviews were recorded and transcribed. Translations from Urdu and Punjabi were validated by a third person, not the interpreter, but also fluent in Danish, Urdu, and Punjabi. Data consisted of interview transcripts and field notes reflecting the life circumstances of each interviewee and the researcher’s impressions from the interview situation. Data were analysed throughout the study to allow emerging themes to be fed back into subsequent interviews.
Ethics
During recruitment, patients were given a verbal explanation of the study by the trilingual master’s student. Written consent was obtained. Interviewees were informed that interviews would be audiotaped and transcribed and that all identifying information would be deleted. No approval from ethical committees is needed for interview studies according to official Danish research guidelines. The study was approved by the Danish Data Protection Agency and complies with ethical principles for medical research as set out in the Helsinki Declaration [20]. In Table 1 and in the result section, interviewees are given a number each in order to protect the interviewees’ anonymity.
Results
Five themes emerged from the analysis: exemption from fasting; medicine use during Ramadan; feeling of improved well-being when fasting; explanations for improved well-being; and talking with others about fasting.
Exemption from fasting
Though not asked directly, all interviewees talked about the option of not fasting during Ramadan. One interviewee said:
When I start feeling very ill, then it’s permitted not to fast, so I don’t do it (Participant 2)
One interviewee suggested that Islam was sometimes perceived as a religion that did not exempt ill people from fasting:
You know that they say that sugar patients [diabetics], they are not allowed to [fast during] Ramadan. There are many that don’t do it, but Allah says okay […]. For Allah it’s not wrong if there is a diabetes patient who doesn’t celebrate [fast during] Ramadan. (Participant 3)
Another interviewee stated:
So our Islam is not so strict […]. We also have solutions. (Participant 5)
Thus, the interviewees expressed that Islam exempts ill people from fasting during Ramadan.
However, having a chronic condition may present a different challenge to fasting than temporary conditions, where postponing fasting can be an option:
If someone is ill, then they are permitted to have a break [from fasting]. But some illnesses, they are – not for example one that has a cold or one that has a fever or something you recover from in two days, three days – but some illnesses, they are part of your life. They don’t [go away] in two days or three days, they are there the whole time. (Participant 3)
Thus, temporarily postponing the fast is not an option for people with a chronic condition such as type 2 diabetes. Instead the ‘rule of exemption’ was raised as being relevant for people with chronic conditions.
Medicine use during Ramadan
Although all interviewees stated that Islam exempts ill people from fasting during Ramadan, all had fasted during Ramadan while having type 2 diabetes, and three still did so. The fourth interviewee had fasted for 15 years after receiving her diagnosis, but chose to stop due to heart problems and a change in her diabetic medication to insulin. Another interviewee stated that although she intends to fast, if she starts feeling very ill while fasting, she will stop. This suggests that although patients may initially choose to fast, physical ‘signals’ during Ramadan may cause them to stop (thus, resorting to the rule of exemption).
The interviewees had different practices regarding when and how much diabetic medicine to take during Ramadan. One took her usual doses, but took her morning medicines earlier and evening medicines later so she could fast between sunrise and sunset. Another interviewee explained why he does not take his morning medicines during Ramadan:
If I eat my morning medicine and I don’t eat anything for lunch or anything, my sugar numbers, they go down already, and then if I eat medicine, then they go down even further, and then I am finished. So I don’t eat [medicine in the] morning, I only eat evening, that’s enough. (Participant 3)
Some interviewees speculated about Ramadan fasting in the year ahead (2011), since the time of year would increase the number of daily fasting hours to 18–19 in Denmark. They hoped to be able to fast but were nevertheless aware that the number of fasting hours would make it more difficult.
Feeling of improved well-being when fasting
All interviewees had experienced an improvement in their well-being during Ramadan fasting, and the interviewees who still fasted all stated that fasting made them feel better. One interviewee said:
I enjoy Ramadan like everyone else. It’s true, I don’t notice it, [although] I don’t eat lunch or I don’t eat morning medicines and such, [I don’t notice it], not at all, all normal. (Participant 3)
Thus, it was a general experience that Ramadan fasting meant improvement in the feeling of well-being.
Explanations for improved well-being
Some of the interviewees elaborated on the reasons underlying the increased feeling of well-being while fasting, which included physiological, social and religious aspects.
Physiological aspects
One explanation presented was physiological, using the rationale that intake of sugary foods would not cause high blood sugar levels because the basic blood sugar level was lower due to fasting. One interviewee said about eating dates when breaking the fast during Ramadan:
In spite of eating dates which are so sweet, I am still completely normal […]. At that point, your sugar level is very low because you haven’t eaten all day, but since you eat the dates which are so sweet, then your sugar level reaches normal again, right? (Participant 3)
One of the interviewees explained that the healthy food intake contributed to the feeling of well-being:
I felt very well, because I think that we ate many healthy foods, and often at the appropriate time. So therefore I felt very well during that period. (Participant 6)
Another physiological explanation was that the body gets used to fasting:
The first three-four [days during] Ramadan, then I had a little headache at the end, right, because you are dehydrated and so on. That also passed after five-six days, then your body gets more used to it. (Participant 6)
Thus, physiological aspects partly related to dietary changes during Ramadan were felt to contribute to improved well-being.
Social aspects
One interviewee also gave a social explanation for the increased feeling of well-being:
But I do it [fast during Ramadan] because my whole life I have celebrated Ramadan, and I think it’s the best month in our lives, Ramadan. It is the best month, a cosy month. (Participant 3)
Thus, the concept of Ramadan as a continual and pleasant time makes taking part in it by fasting increase well-being.
Religious aspects
Some of the interviewees also had religious explanations for their improved well-being during fasting. A man explained:
It’s a blessing that in the month of Ramadan that a person who is sick gets, you know, gets better and feels well, while you are fasting, right, and that’s a blessing, that’s the blessing of the Ramadan month. (Participant 3)
A woman elaborated:
So, it’s something about being in contact with your God, so it helps a lot, that is, when you believe in it. (Participant 6)
Fasting as a religious practice may also imply a feeling of empowerment and control regarding health. One interviewee elaborated on how despite his diagnoses, he was confident about being able to fast during next Ramadan, although the number of fasting hours will increase:
It’s a question of having that will power […]. There are people, if you have will power, it’s okay, all right, even if you are sick, conscious [that] some things are part of you. If your thoughts don’t want to, then you cannot. If you say will power, I can manage, you can manage, and you will manage anyway. Alhamdullah [praise be to God], I am ready now. (Participant 3)
Talking with others about fasting
Some interviewees had friends or relatives with type 2 diabetes. One interviewee explained how she talked with relatives with and without diabetes as part of her decision making regarding Ramadan fasting:
My children told me not to fast because, ‘mom you have diabetes, so don’t do it’. But then I called my big sister [who has type 2 diabetes] and she asked me if I fasted, and then I said no, I didn’t, and then my sister said ‘you should start, you will feel much better’. And it’s true, I do feel better when I fast. (Participant 2)
Another interviewee related that although she knew many people with type 2 diabetes who did not fast, she also knew people with more severe type 2 diabetes who still fasted:
I also know many who are worse off than me, that is, those who also take insulin. […] They also celebrate it [fast during Ramadan]. […] They say it works well. (Participant 6)
Thus, having people in their social networks with the same condition was a source of support and inspiration for interviewees regarding Ramadan fasting.
One interviewee mentioned having talked to her doctor about fasting:
The doctor told me, if you celebrate [fast during] Ramadan, then your disease will get worse, so you must take care, and I did. (Participant 5)
Conversely, another interviewee said that she had not talked to her doctor about fasting. Still another explained that the issue of Ramadan was ‘a secret’, indicating that he considered his medicine behaviour during Ramadan to be a private issue.
Discussion
This study shows that people with type 2 diabetes and Pakistani background may choose to fast during Ramadan, and this may mean changes in their medicine use. They do not always discuss these changes with healthcare professionals. Rather, changes are based on the patient’s own reflexions and discussion with family or friends, especially those with type 2 diabetes. The participants in the study represent a rather vulnerable patient group with co-morbidity and low social position, and the results might reflect this.
For all interviewees, Ramadan fasting meant a feeling of improved well-being, which is supported by a Swedish study among people of Somali background [14]. This current study provides further exploration of the reasons behind this improvement, namely, the social and religious aspects in addition to the physiological. For example, Ramadan may mean an increased focus on health and healthy living as part of religious practice. As a religious practice, fasting may also simultaneously reinforce spirituality for the individual Muslim and invoke social interaction in the religious community. By choosing to fast, patients may experience bodily discomfort (e.g. decreased blood sugar levels), but from a patient perspective (illness), this may not equal the spiritual and social gains of fasting. In a biomedical paradigm with emphasis on clinical measures such as blood sugar levels, fasting may make no sense at all and may be even harmful. However, from a patient perspective, where the concept of illness [16] is embedded in an everyday life consisting of practices, values, identity and social interaction, fasting—despite religious ‘rules of exemption’—may not be all that irrational.
Studies are rare on the attitudes of healthcare professionals about counselling people with type 2 diabetes on Ramadan fasting. However, a French study found that when counselling Muslims with diabetes, general practitioners often told patients not to fast with the argument that they are exempt from fasting according to the Quran [13]. Their advice was grounded in the assumption that patients were not able to self-manage their diabetes during the fast. The same study also found that consultation with general practitioners on Ramadan issues did not have major impact on fasting behaviour [13]. A Canadian study questions the advice about not fasting by finding that the healthy Bangladeshi and Somali women interviewed agreed that healthcare professionals should not simply advise against fasting, but rather provide guidance on health maintenance while fasting [22]. In this current study, all interviewees emphasised that the flexibility of Islamic rules allows for ill people to refrain from fasting. This finding was surprising, since the interviewees were only asked about their actual behaviour regarding medicines. That they all chose to highlight the flexibility of their religion could be influenced by encounters in the healthcare sector where they were told that they are not supposed to fast according to Islam.
This current study also explored who people with type 2 diabetes and Pakistani background talk to about Ramadan fasting. Friends and family were more often consulted than healthcare professionals. This finding is supported by the above-mentioned French study [13] and a British study of Pakistani patients with long-term illnesses, which found that patients and healthcare professionals are often unwilling to engage in dialogue about religious influences on health issues [23]. Patients lack confidence in raising the issue, and professionals lack awareness of its importance. Consequently, patients receive little or no support on these issues, despite their clinical relevance [23].
Overall, this current study illustrates the need to take patient perspectives as a starting point in encounters with patients regarding medicines, since it may lead to knowledge that can inform clinical practice. Healthcare professionals may tend to focus on individual, non-contextual aspects of biomedical disease [17], e.g. by informing patients that they are exempt from the rule of fasting [13]. However, in order for medical treatment to be acceptable to patients, it must make sense to them in terms of their understanding of illness. Furthermore, counselling must take into account the additional priorities patients consider important in everyday life [4]. Religious practices that provide perceived physiological, spiritual and social gains may well be such a priority. A patient-centred dialogue will therefore provide healthcare professionals with important information about the patient’s understandings, which the professional will be able to incorporate into his counselling and vice versa [16]. Such dialogue would make improved medicine use with positive impact on treatment outcomes more likely.
Because exploring practices regarding medicine use during Ramadan was not a key objective of the overall study, the theme was not fully explored in all interviews with interviewees of Pakistani background, and some interviewees were not explicitly asked about the subject. However, because the study was on universal experiences with medicines for people with type 2 diabetes including interviewees of majority as well as minority background, presumably interviewees of Pakistani background felt more included and less stereotyped than if the purpose of the study had been to explore primarily Ramadan practices. This may have provided a setting where interviewees of Pakistani background were more open about sensitive issues such as Ramadan fasting. Additionally, since interviewees themselves raised and elaborated on the topic of reconciling medicine use with Ramadan fasting, it emphasises the value of researchers keeping an open-mind during analysis, in order to understand medicine use as it is perceived and lived by lay people.
Validity rests on the researcher’s ability to continually reflect upon, question and discuss pre-understandings during the entire research process [21]. Reflexivity regarding interviewing style was sought by discussing each interview with the master’s student/interpreter, reading field notes and listening to recordings of the interviews followed by adjusting questions between interviews. During analysis, emerging themes were discussed within the research group and in cross-disciplinary research groups. Validity was additionally sought by seeking to provide sufficient evidence from accounts in the dissemination of findings for others to critically judge the process of analysis and presentation.
Recommendations for practice
Scientific guidelines for healthcare professionals regarding management of type 2 diabetes during Ramadan exist, including summaries of important knowledge about what advice to give and the admonition that this advice should be given in a patient-centred manner [8, 9]. However, since the research literature is only in the making, these recommendations are only to a lesser extent based on scientific knowledge about patient perspectives on medicine use during Ramadan.
This current study points to the importance for healthcare professionals to bear in mind that people with type 2 diabetes and Muslim background may choose to fast and that fasting may mean changes in medicine use. Fasting may be understood as something that provides a feeling of improvement in people’s well-being, an improvement that has physiological, social and religious aspects. It is therefore important for healthcare professionals to avoid arguing for non-fasting based on theological arguments, e.g. that the patient is exempt from fasting according to Islam. Rather, counselling should be based on clinical knowledge of the options for adjusting medicines while fasting, providing the patient with a biomedical knowledge that can be used as part of the decision-making process regarding medicine use during Ramadan.
Conclusion
Fasting during Ramadan may mean changes in medicine use for people with Muslim background and a chronic medical condition. Healthcare professionals do not always discuss these changes with their patients. The study calls for healthcare professionals to acknowledge that Muslim patients may find fasting during Ramadan beneficial to their well-being and therefore choose to fast despite the Islamic ‘rule of exemption’. This knowledge is essential for healthcare professionals if they are to provide patient-centred counselling on medicines based on the ideas of concordance and adherence, and thus considered useful and relevant to the patient involved, in order to improve clinical health outcomes among patients that choose to fast.
References
Garduño-Diaz SD, Khokhar S. Prevalence, risk factors and complications associated with type 2 diabetes in migrant South Asians. Diabetes Metab Res Rev. 2012;28(1):6–24.
Wändell PE, Carlsson A, Steiner KH. Prevalence of diabetes among immigrants in the Nordic countries. Curr Diabetes Rev. 2010;6(2):126–33.
Haugbølle LS, Sørensen EW. Drug-related problems in patients with angina pectoris, type 2 diabetes and asthma - interviewing patients at home. Pharm World Sci. 2006;28:239–47.
WHO. Adherence to long-term therapies. Switzerland: WHO; 2003. ISBN:9241545992.
Sadiq A. Managing the fasting patient: sacred, ritual, modern challenges. In: Sheikh A, Gatrad AR, editors. Caring for muslim patients. Oxford: Radcliffe Publishing Ltd; 2000. p. 73–87. ISBN 1857753720.
Bissell P. Lay and professional accounts of non-compliance with treatment amongst people of Pakistani origin with type 2 diabetes. School of Pharmacy and Pharmaceutical Sciences: University of Manchester; 2000.
Benaji B, Mounib N, Roky R, Aadil N, Houti IE, Moussamih S, et al. Diabetes and Ramadan: review of the literature. Diabetes Res Clin Pract. 2006;73(2):117–25.
Ahmedani MY, Haque MS, Basil A, Fawwad A, Alvi SF. Ramadan Prospective Diabetes Study: the role of drug dosage and timing alteration, active glucose monitoring and patient education. Diabet Med. 2012;26(6):709–15.
Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2010;33(8):1895–902.
Sheikh A, Wallia S. Ramadan fasting and diabetes. BMJ. 2007;335(7620):613–4.
Håkonsen H, Toverud EL. Cultural influences on medicine use among first-generation Pakistani immigrants in Norway. Eur J Clin Pharmacol. 2012;68(2):171–8.
Salti I, Bénard E, Detournay B, Biachi-Biscay M, Le Brigand CL, Vionet C, et al. A population-based study of diabetes and its charachteristics during the fasting month of Ramadan in 13 countries. Diabetes Care. 2004;27(10):2306–11.
Gaborit B, Dutour O, Ronsin O, Atlan C, Darmon P, Gharsalli R, et al. Ramadan fasting with diabetes: an interview study of inpatients’ and general practitioners’ attitudes in the South of France. Diabetes Metab. 2011;37(5):395–402.
Wallin AM, Löfvander M, Ahlström G. Diabetes: a cross-cultural interview study of immigrants from Somalia. J Clin Nurs. 2007;16(11C):305–14.
Pollock K. Concordance in medical consultations—a critical review. Oxford and Seattle: Radcliffe Publishing; 2005. ISBN:101857758412.
Helman CG. Doctor-patient interactions. In: Culture, health and illness. 5th ed. London: Hodder Arnold; 2007. p. 121–55. ISBN:9780340914502.
Kleinman A. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. Berkeley: University of California Press; 1980. ISBN 9780520037069.
Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med. 2006;3(10):1673–6.
Dahlager L, Fredslund H. Hermeneutic analysis—understanding and pre-understanding. In: Vallgårda S, Koch L, editors. Research methods in public health. Copenhagen: Gyldendal Akademisk; 2008. p. 159–84. ISBN 9788762807945.
World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Helsinki: World Medical Association; 2008.
Stige B, Malterud K, Midtgarden T. Toward an agenda for evaluation of qualitative research. Qual Health Res. 2009;19:1504–16.
Pathy R, Mills KE, Gazeley S, Ridgley A, Kiran T. Health is a spiritual thing: perspectives of health care professionals and female Somali and Bangladeshi women on the health impacts of fasting during Ramadan. Ethn Health. 2011;16(1):43–56.
Mir G, Sheikh A. ‘Fasting and prayer don’t concern the doctors … they don’t even know what it is’: communication, decision-making and perceived social relations of Pakistani Muslim patients with long-term illnesses. Ethn Health. 2011;15(4):327–42.
Acknowledgments
We wish to thank all interviewees and Farhat Shaheen who assisted as interpreter and contact person for the patients.
Funding
The study is supported by the School of Pharmaceutical Sciences (former Faculty of Pharmaceutical Sciences), University of Copenhagen, Denmark, with supplementary funding from The 1991 Pharmacy Foundation (The Danish Pharmaceutical Association) and The Danish Actavis Grant.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mygind, A., Kristiansen, M., Wittrup, I. et al. Patient perspectives on type 2 diabetes and medicine use during Ramadan among Pakistanis in Denmark. Int J Clin Pharm 35, 281–288 (2013). https://doi.org/10.1007/s11096-012-9716-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9716-1