Abstract
Objective: To undertake a cost-utility analysis (CUA) of a pharmacy-led self-management programme for Chronic Obstructive Pulmonary Disease (COPD). Setting: A single outpatient COPD clinic at the Mater Hospital, Belfast, Northern Ireland between. Method: CUA alongside a randomised control trial. The economic analysis used data from 127 COPD patients aged over 45 years, with an FEV1 of 30–80% of the predicted normal value. Participants received either a pharmacy-led education and self-management programme, or usual care. One year costs were estimated from the perspective of the National Health Service and Personal Social Services and quality-adjusted life years (QALYs) were calculated based on responses to the EQ-5D at baseline, 6 and 12 months. Main outcome measure: Cost per QALY gained. Results: The mean differences in costs and effects between the self-management and education programme and usual care were −£671.59 (95 CI%: −£1,584.73 to −£68.14) and 0.065 (95% CI; 0.000–0.128). Thus the intervention was the dominant strategy as it was both less costly and more effective than usual care. The probability of the intervention being cost-effective was 95% at a threshold of £20,000/QALY gained. Sensitivity analyses indicated that conclusions were robust to variations in most of the key parameters. Conclusion: The self-management and education programme was found to be highly cost-effective compared to usual care. Further research is required to establish what aspects of self-management and education programmes have the greatest impact on cost-effectiveness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact of findings on practice
-
A structured education and self-management programme led by clinical pharmacists for patients with COPD can bring about a reduction in healthcare resource utilisation and an improvement in health-related quality of life.
-
Education and self-management for patients with COPD was found to be highly cost-effective compared with usual care.
Introduction
Chronic obstructive pulmonary disease (COPD) is an umbrella term for a number of chronic lung conditions including chronic bronchitis and emphysema. The disease is typically characterised by airflow obstruction which is usually progressive and not fully reversible. The airflow obstruction is generally the result of damage to the airways brought about by a chronic inflammatory response to (most typically) tobacco smoke [1, 2]. Symptoms most commonly include cough, phlegm production and shortness of breath. In severe cases the patient may suffer from frequent episodes of acute exacerbations or ‘flare-ups’, which contribute towards the overall deterioration of health status and quality of life [3–5]. COPD is a major cause of morbidity and mortality in adults with 210 million people diagnosed worldwide [6]. In the UK, an estimated 900,000 patients have been diagnosed with the condition, although the actual number of patients with COPD is believed to be around 1.5 million [2]. It is expected to be the third leading cause of death worldwide by 2020 (exceeded only by heart disease and stroke) [7]. It is difficult to ascertain the true mortality rate due to COPD, however, it is estimated to cause approximately 30,000 deaths per year in the UK [1, 2].
A large-scale international survey “Confronting COPD in North America and Europe” resulted in comprehensive information about the impact of COPD on patients, healthcare and society [8]. Economic analysis of patient responses to the survey highlighted the substantial economic impact of COPD on both the UK healthcare system and the economy [1]. The average cost per patient per annum was estimated to be £819.42, with 60% of this cost (£494.67) attributable to unscheduled care [hospital inpatient stay, accident and emergency visits and unscheduled visits to a general practitioner (GP) or specialist]. The authors suggested that the relatively high use of unscheduled healthcare resources reported in the survey may reflect poor disease control with inadequate management of symptoms and exacerbations.
Self-management is a term applied to any formalised patient education programme aimed at: teaching the skills needed to carry out medical regimens specific to the disease, guide health behaviour change, and provide emotional support for patients in the control of their disease so that they may live functional lives [9]. There is increasing awareness that self-management may be an effective method of managing a range of chronic illnesses [10–13] including COPD [9, 14]. By providing patients with information on their condition and how to prevent or manage exacerbations, their health status may improve and healthcare resource utilisation decrease. Indeed, the most recent NICE (National Institute for Health and Clinical Excellence) clinical guidelines for the management of COPD recommend that further research be carried out into the efficacy of such patient focused programmes [2]. The most recent Cochrane review of self-management education interventions of patients with COPD [15] showed that in general self-management education programmes of COPD had a positive effect on health care utilisation. A reduction was observed in hospital admissions and in doctor and nurse visits, however, an increase in use of steroid and/or antibiotic courses was observed. The authors hypothesised that the latter may be due to the educated patients recognising the symptoms of an exacerbation more readily and responding to them by the self-initiation of medication. A small but significant improvement was seen in health-related quality of life, however, the difference was not large enough to be considered clinically relevant. The authors of the review, however, felt that the diversity of the outcome measures, follow-up periods, COPD-population and interventions used in the studies made it impossible to draw any firm conclusions regarding the effectiveness of self-management education for patients with COPD.
Considering the economic burden of COPD and the current climate of limited healthcare resources, it is essential that cost-effective management programmes are implemented. To date, only a few studies have attempted to assess the cost-effectiveness of self-management education in COPD [14, 16, 17]. These studies have differed in the methodological approach used, the perspective on costs and outcomes adopted for the analysis and the primary clinical outcome of interest.
Aim of the study
The aim of the study was to undertake a cost-utility analysis to establish the cost-effectiveness of a pharmacy-led education and self-management programme for COPD compared with usual care.
Methods
The economic evaluation took place alongside a randomised control trial (RCT). Ethical approval was obtained from the Office of Research Ethical Committees for Northern Ireland (ORECNI: 06/NIR02/23). The full details of the RCT are presented elsewhere [18], however, in brief, 173 patients were recruited from an outpatient COPD clinic at the Mater Hospital, Belfast, Northern Ireland between October 2006 and May 2008 and randomly allocated to receive either the self-management education programme or usual care. The randomisation was carried out using the minimisation method [19]. Patients were included if they were aged over 45 years with a confirmed diagnosis of COPD for at least 1 year and an FEV1 of between 30 and 80% of the predicted normal value. Patients with Congestive Heart Failure (CHF), moderate to severe learning difficulties, severe mobility problems, a terminal illness or who had attended a pulmonary rehabilitation programme in the last 6 months were excluded.
The goal of the self-management education programme was to increase the patients’ self-efficacy to manage or avoid breathing difficulty while participating in certain activities. Intervention patients received a 60 min consultation with a hospital pharmacist at baseline during in which they were educated individually on COPD, their prescribed medication, the importance of adherence, inhaler technique, and the management of COPD symptoms including exercise and breathing techniques. A customized action plan for acute exacerbations was developed for each patient which included advice to GPs to provide a prescription for an antibiotic (amoxicillin/clavulanic acid) and an oral corticosteroid to be initiated promptly by patients in the event of acute exacerbations. This was followed by a 20 min telephone call at 3 and 9 months, and a 30 min outpatient visit at 6 and 12 months. Control patients attended the hospital outpatient clinic at 6 and 12 months where they received usual care from medical and nursing staff which included symptom assessment, spirometry where necessary and the prescription of inhalers and medication when needed.
Health outcomes
For the economic evaluation, the impact of the intervention on health-related quality of life (HRQoL) was measured using both the EQ-5D [20] administered at baseline, 6 and 12 months. The EQ-5D is a generic preference-based measure of health which provides a description of health using five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) each with 3 levels of severity and has been shown to be appropriate for use in patients with COPD [21]. It is recommended by NICE [22] for use in economic evaluation. The UK social preference weights for EQ-5D health states were used to obtain single utility values from the responses at each time point. These preference weights were derived using the time-trade off (TTO) technique in a representative sample of the general population [23]. The area-under-the-curve (AUC) method [24] was used to estimate patient-specific QALYs accrued over the 12 month period. This method involves multiplying the utility of the patients’ health state at each time point by the duration of the health state, and then summing these over the study period. It was assumed that changes in utility over the time points were linear.
Measuring and valuing costs
In line with guidance from NICE [22] a National Health Service (NHS) and Personal Social Service (PSS) perspective was adopted for the analysis. Only costs relevant to this perspective were considered. Patient-specific healthcare resource utilisation was collected prospectively during the study. This was not COPD specific, unless otherwise stated. Information on general practitioner (GP) visits (both scheduled and unscheduled, i.e. emergency) were obtained via patient completed questionnaires administered at 6 and 12 months. Information on emergency department (ED) visits, hospital bed days and exacerbation medication usage (oral steroid and antibiotic courses) was collected using active follow-up of the patients’ medical records. Resource use was quantified and valued in monetary terms by multiplying these units by unit costs (Table 1) which were obtained from national sources whenever possible [25, 26] and based on the financial year 2006/2007 in UK Sterling (£). The intervention costs included the cost of steroid and antibiotic courses provided to patients to be taken in the event of an exacerbation (irrespective of whether they were administered), the costs of a clinical pharmacist’s time input (including training), costs of an administrator’s time input, printing costs and overhead costs. Discounting of costs and health outcomes was not required as the study did not exceed 12 months.
Data analysis
The economic analyses were carried out on a per protocol basis therefore they were based only on patients for whom there was complete resource use and health outcomes data. Demographic and clinical data were analysed using IBM SPSS Statistics version 19 to perform Chi-square tests for categorical data and independent t tests for continuous data. Resource data is typically skewed and so the underlying assumptions of parametric tests of the mean are frequently violated. Since the arithmetic mean is the statistic of interest for decision making, both parametric t tests and nonparametric bootstrapping were used as recommended [27]. STATA version 10 was used to calculate 95% non-parametric confidence intervals for differential mean costs and QALYs based on 1,000 bias-corrected, accelerated bootstrap replications. Imbalance in the mean baseline utilities between the intervention and control groups was controlled for by using multiple regression to estimate the differential QALYs [28].
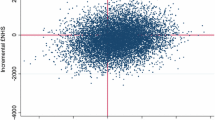
Economic evaluation involves an incremental analysis of the costs and consequences of alternative courses of action, thus the incremental cost-effective ratio (ICER) was calculated by dividing the mean cost difference between the intervention and control patients by the mean QALY difference to establish the cost per QALY gained. To account for sampling uncertainty in the cost and effect data used to calculate the ICER, non-parametric bootstrapping was also performed to generate 1,000 bootstrap replicates of the ICERs which were then plotted on the cost-effectiveness plane. The resulting scatterplot was used to derive the cost-effectiveness acceptability curve (CEAC) by calculating the proportion of the replicates which would be considered cost-effective at various thresholds of willingness-to-pay for an additional QALY.
A series of univariate sensitivity analyses were performed to explore how robust the results were to changes in the assumptions upon which they were based. We explored the impact on the cost-effectiveness of the intervention of variations in; the number of bed days used in each group, the cost of the self-management and education programme and the effectiveness of the programme. Finally, multiple imputation was used to impute missing QALY and cost data with treatment group, age, gender and COPD severity incorporated into the multiple linear regression models as covariates.
Results
The analysis was based only on patients for whom there was complete resource use and outcomes data for the intervention period (127 patients: intervention, n = 64; control, n = 63) were included in the economic analysis (see Fig. 1). Baseline characteristics were similar across sociodemographic, clinical and functional variables (Table 2).
The mean EQ-5D utility scores for the intervention and usual care group patients at baseline, 6 and 12 months, and the mean QALYs gained over the study period are presented in Table 3. A mean differential QALY (controlled for baseline utility) of 0.065 in favour of the self-management education programme group was found, but this was not statistically significant (P = 0.051).
The mean health resource usage per patient over the study period is presented in Table 4. Statistically significantly lower unscheduled GP visits, ED visits, hospital bed days and oral steroid and antibiotic courses were observed in the intervention group compared to usual care over the 12 month study period. The main difference related to the number of hospital bed days with there being 60% fewer hospital bed days associated with the intervention group. The mean cost of healthcare resource usage per patient over the study period is presented in Table 5. This value in the intervention group was £859.00 compared with £1,911.77 in the control group. The cost of the intervention-related resources was £381.18 per patient, bringing the total per-patient cost for the intervention group to £1,240.18, which is still lower than the total per-patient cost for the usual care group. Thus a mean differential cost of −£671.59 was found, indicating a cost saving in the intervention group. However, this difference was not statistically significant (P = 0.065).
Cost-utility analysis
Self-management and education was found to be both more effective and less costly than usual care thus it is the dominant strategy. In this situation the ICER is not calculated as self-management is clearly good value for money and furthermore it is inappropriate to interpret the magnitude of negative ICERs [29]. Uncertainty surrounding the estimates of costs and effects is represented on the cost-effectiveness plane (Fig. 2). The joint density of incremental costs and effects straddles all four quadrants of the cost-effectiveness plane, with the majority of the points lying in the south-east quadrant. This indicates that there is some degree of uncertainty surrounding both the presence and the magnitude of cost-savings and effectiveness. The CEAC summarises this uncertainty. The CEAC (not presented here) illustrates the probability of the self-management education programme being more cost-effective than usual care at different thresholds of decision makers’ willingness-to-pay (WTP) for a QALY. According to NICE [30] interventions with an ICER of less than £20,000 per QALY gained are likely to be considered to be cost-effective. The probability of the self-management education programme being cost-effective at this threshold was 95%. As the threshold increases, a proportion of the bootstrap re-samples falling into the south-east quadrant are no longer considered cost-effective, thus the probability is observed to decrease slightly.
The sensitivity analyses explored the impact of: reducing the difference observed in the bed days between groups by 50 and 100% (i.e. no difference), decreasing and increasing the cost of the intervention by 50%, decreasing the QALYs gained by 50% and multiply imputing the missing cost and QALY data instead of excluding patients with missing data from the analysis. For the latter, five replacement values (m = 5) were generated for each missing cell using multiple linear regression models containing the covariates treatment group, age, gender and COPD severity. The results showed that the self-management education programme for COPD patients remained the dominant strategy when most key parameters were varied. The one exception being that when there was no difference in the number of bed days used between groups, there was no longer a cost saving. The resulting ICER of £3,278 per QALY however still remains considerably lower than the NICE threshold of £20,000 per QALY.
Discussion
This study investigated the economic impact of a pharmacist-led self-management education programme for COPD patients compared with usual care. The intervention programme was associated with both a gain in QALYs (0.065) and a cost saving to the NHS of £671.59 per patient, thus it was the dominant strategy. Little can be concluded from the absence of statistically significant differences in cost and QALYs, since the main RCT was not powered to detect such differences. Furthermore, in economic evaluations more focus is now placed on how certain we can be of an intervention’s cost-effectiveness hence the use of cost-effectiveness acceptability curves [31]. Decisions no longer tend to be based on just the point estimates of cost and effect. The CEAC indicated that the probability of the intervention being cost-effective was 95% at a threshold of £20,000/QALY gained. Sensitivity analyses showed that this finding was robust to plausible variations in key parameters, thus the self-management programme for patients with COPD can be considered highly cost-effective. The current study is an important addition to the current evidence base as, despite the considerable financial burden of COPD, relatively few RCTs have been undertaken which explore the cost-effectiveness of self-management education programmes alongside the primary research question relating to clinical effectiveness [14, 16, 17, 32].
The results of the present study demonstrated that a pharmacy-led education and self-management programme reduced, on average, hospital bed days by 60% (which accounted for the majority of the cost difference), emergency department visits by 48% and unscheduled GP visits by 38%. These findings support those of Bourbeau and colleagues [9, 16] who reported a 42% reduction in all hospital days, a 35% reduction in all accident and department visits and a 59% reduction in unscheduled physician visits. Similarly, Gallefoss and Bakke [14] observed reduction in hospital admission costs, as did Tougaard and colleagues [32] in a study in the early 1990s. Despite the fact that the methodological approach differed between studies, it would appear that cost savings were achieved in the area of reduced hospitalisation. This is particularly appropriate as previous research has identified hospitalisation for exacerbations as a key cost driver in the management of COPD [32–37]. One economic evaluation undertaken alongside an RCT in this area (the COPE self-management education programme) has presented conflicting findings to those reported above. They determined that the COPE programme was twice as expensive as usual care, with no discernable benefit (as measured in QALYs) [17]. However, the COPE programme included a relatively expensive fitness programme and the economic evaluation took a societal perspective, thus included costs incurred by the patients whilst attending the programme.
This study highlights that one effective method of reducing the resource use of patients with COPD, in particular their hospital stay of patients, is to provide them with sufficient information so that they have the knowledge and ability to manage their own symptoms. Hospital pharmacists potentially play an important role in the delivery of such education programmes as they are in a primary position to be able to teach the skills needed to carry out medical regimens specific COPD, or indeed other diseases.
The health-related quality of life of COPD patients at baseline as measured by the EQ-5D was considerably lower than levels reported by Monninkhof et al. [17] (in patients with similar levels of COPD severity (intervention; 0.465, control; 0.485 vs. intervention; 0.81, control; 0.82). Furthermore, Rutten-van Mölken et al. [21] report individuals with a GOLD stage Very Severe average EQ-5D score of 0.647.
The reason for such low levels self-reported health status in our patients cannot be explained easily. The clinical characteristics of our patients appear to be comparable to those of the patients in Monninkhof et al.’s study. The low health status may be due, in part, to all patients being recruited from a single hospital in Belfast- an area which has been shown to have a significantly higher proportion of people reporting problems with health and a lower health status score than the rest of Northern Ireland [38] as measured by the EQ-5D. Similarly, findings from the Northern Ireland Census 2001 [39] showed that 14.3% of individuals in Belfast reported having poor health compared with 9.7% of people living in the rest of Northern Ireland. Furthermore the results of a comparative analysis of self-rated health and mortality in the UK [40] indicated that, after adjusting for age and gender those in Northern Ireland were 10% more likely to report not good or fairly good health (rather than good) than those in England and Wales. These differences highlight that our results cannot be readily generalised to other settings. The disparity between the self-reported health status scores of the COPD patients in the present study and those in other studies highlights the drawback of recruiting patients from a single site. A larger, multisite RCT is required to better understand the nature of self-reported health status in these patients and to facilitate the generalisability of our results.
The decision to collect only exacerbation related drug data was influenced by the previous cost-effectiveness analyses performed in this area. Bourbeau et al. [16] did not report the cost of pharmaceuticals at all, simply stating that no differences were observed. Gallefoss and Bakke [14] report the costs associated with the use of anti-asthmatics only and Monninkhof et al. [17] reported the cost of medications for exacerbations only. A pragmatic approach was therefore applied to this study to reduce the burden of data collection and yet maintain comparability with previous studies. We acknowledge however that a change in health status brought about by the intervention may cause changes in the medications prescribed outside of the study (and out of our control).
We performed a complete case analysis of the cost and QALY data for the primary economic analysis. This is a naïve method of dealing with censored data and leads to loss of information and statistical power [29]. Furthermore, we did not directly compare those patients with complete data with those who dropped out or had missing data. We did however perform multiple imputation of this missing data in the sensitivity analysis found that the intervention still remained highly cost-effective.
Further studies should attempt to confirm whether our findings are reproducible in other settings considering the issues surrounding the low health status of patients. These studies should also attempt to identify which aspects of the education and self-management programme were central to its overall effectiveness by varying, for example, the frequency of outpatient visits, the follow up period, the educational material provided and the healthcare professional delivering the programme.
Conclusion
Self-management and education in patients with COPD can potentially reduce the economic burden of the disease on the NHS and bring about positive gains in HRQoL, despite the progressive nature of the disease. The study also highlighted the important role hospital pharmacists have in educating patients about medication use. Considering the wide variety of self-management programmes for patients with COPD [15], further research is required to establish which aspects of self-management and education have the greatest impact on its overall cost-effectiveness.
References
Britton M. The burden of COPD in the UK. Results from confronting COPD survey. Respir Med. 2003;97(Suppl C):S71–9.
National Collaborating Centre for Chronic Conditions. Chronic obstructive pulmonary disease: national clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax. 2004;59(Suppl 1):1–232.
Miravitlles M, Ferrer M, Pont A, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004;59:387–95.
Seemugal TA, Donaldson GC, Paul EA, et al. Effects of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med. 1998;157:1418–22.
Spencer S, Jones P. Annual rate of health status decline in COPD patients is significantly related to the frequency of acute exacerbations. Eur Respir J. 1999;14(Suppl 30):19S.
The World Health Organisation. 2007. Available from: http://www.who.int/respiratory/copd/en/. Cited 8 Feb 2011 [Internet].
European Respiratory Society. European white lung book. Brussels; 2003. ISBN: 978-1904097303.
Rennard S, Decramer M, Calverley PMS, et al. Impact of COPD in North America and Europe in 2000: subjects’ perspective of confronting COPD international survey. Eur Respir J. 2002;20:799–805.
Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163(5):585–91.
Guevera JP, Wolf FM, Crum CM, et al. Effects of educational interventions for self management of asthma in children and adolescents: systematic review and meta analysis. BMJ. 2003;326:1308–9.
Taylor SJ, Milanova T, Hourihan F, et al. A cost-effectiveness of a community pharmacist-initiated disease state management service for type 2 diabetes mellitus. Int J Pharm Pract. 2005;13:33–40.
Kennedy AP, Nelson E, Reeves D, et al. A randomised controlled trial to assess the effectiveness and cost of a patient orientated self management approach to chronic inflammatory bowel disease. Gut. 2004;53:1639–45.
Robinson A, Wilkson D, Thompson DG, et al. Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. Lancet. 2001;358:976–81.
Gallefoss F, Bakke PS. Cost-benefit and cost-effectiveness analysis of self-management in patients with COPD—a 1-year follow-up randomized, controlled trial. Respir Med. 2002;96(6):424–31.
Effing TW, Monninkhof EM, van der Valk PDLPM, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007; Issue 4. Art. No.: CD002990. doi:10.1002/14651858.CD002990.pub2.
Bourbeau J, Collet JP, Schwartzman K, Ducruet T, et al. Economic benefits of self-management education in COPD. Chest. 2006;130:1704–11.
Monninkhof E, van der Valk P, Schermer T, et al. Economic evaluation of a comprehensive self-management programme in patients with moderate to severe chronic obstructive pulmonary disease. Chronic Respir Dis. 2004;1(1):7–16.
Khdour M, Kidney J, Smyth B, McElnay J. Clinical pharmacy led disease and medicine management programme for patients with COPD. Br J Clin Pharmacol. 2009;68(4):588–98.
Evans S, Royston P, Day S. Minim: allocation by minimisation in clinical trials. Available from: http://www-users.york.ac.uk/~mb55/guide/minim.htm. Updated 29 June 2004; cited 8 Feb 2011 [Internet].
EuroQol Group. Euroqol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Rutten-van Mölken MP, Oostenbrink JB, Tashkin DP, et al. Does quality of life of COPD patients as measured by the generic EuroQol five-dimension questionnaire differentiate between COPD severity stages? Chest. 2006;130(4):1117–8.
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: NICE. 2008. Available from: http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf. Updated 2 Jan 2009; cited 8 Feb 2011 [Internet].
Dolan P. Modelling valuations for EuroQol health states. Med Care. 1997;35:1095–108.
Mathews JNS, Altman D, Campbell MJ. Analysis of serial measurements in medical research. BMJ. 1990;300:230–5.
Curtis L, Netten A. Unit costs of health and social care. Canterbury: PSSRU, University of Kent; 2006.
British National Formulary. 51. British Medical Association and the Royal Pharmaceutical Society of Great Britain. London; 2006.
Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–200.
Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in a trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–96.
Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. Oxford: Oxford University Press; 2007. ISBN 978-0-19852997-2.
National Institute for Health and Clinical Excellence. Social value judgements: principles for the development of NICE guidance. 2nd ed. London: NICE; 2008. Available from http://www.nice.org.uk/aboutnice/howwework/socialvaluejudgements/socialvaluejudgements.jsp. Updated 20 Aug 2008; cited 8 Feb 2011 [internet].
Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
Tougaard L, Krone T, Sorknaes et al. Economic benefits of teaching patients with chronic obstructive pulmonary disease about their illness: the PASTMA Group. Lancet. 1992;339:1517–20.
Hilleman DE, Dewan N, Malesker M, et al. Pharmacoeconomic evaluation of COPD. Chest. 2000;118(5):1278–85.
Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest. 2000;117(2 suppl):5S–9S.
Jacobson L, Hertzman P, Lofdahl CG, et al. The economic impact of asthma and chronic obstructive pulmonary disease (COPD) in Sweden in 1980 and 1991. Resp Med. 2000;94(3):247–55.
Strassels SA, Smith DH, Sullivan SD, et al. The cost of treating COPD in the United States. Chest. 2001;119(2):344–52.
Foster TS, Miller, JD, Marton, JP, et al. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006;3:211–8.
Appleby J. Independent Review of Health and Social Care Services in Northern Ireland. Belfast: Department of Health, Social Services and Public Safety; 2005. Available from: http://www.dhsspsni.gov.uk/appleby-report.pdf. Updated 15 Dec 2006; cited 8 Feb 2011 [Internet].
Northern Ireland Statistics Research and Agency. 2001 census: Northern Ireland census area statistics: NUTS level regions. Table CAS315. Available from: http://www.nisranew.nisra.gov.uk/census/Census2001Output/CASTables/cas_tables_nuts.html#Health%20And%20Care. Updated 14 April 2005, cited 8 April 2011.
Young H, Grundy E, O’Reilly D, Boyle P. Self-rated health and mortality in the UK: results from the first comparative analysis of the England and Wales, Scotland, and Northern Ireland longitudinal studies. Popul Trends. 2010;139:11–36.
Acknowledgments
We are very grateful for the advice and feedback provided by the anonymous reviewers of this paper during its revision.
Funding
The authors wish to thank Chest Heart and Stroke (Northern Ireland) for financial support.
Conflicts of interests
None to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s11096-011-9598-7.
Rights and permissions
About this article
Cite this article
Khdour, M.R., Agus, A.M., Kidney, J.C. et al. Cost-utility analysis of a pharmacy-led self-management programme for patients with COPD. Int J Clin Pharm 33, 665–673 (2011). https://doi.org/10.1007/s11096-011-9524-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-011-9524-z