Abstract
Objective To understand the types of services provided by Iranian clinical pharmacists in nephrology and infectious disease wards, the acceptance rate of clinical pharmacy services in these wards by physicians and the clinical significance of these services in the main teaching hospital in Iran. Setting: Nephrology and infectious disease departments of a university hospital in Iran. Methods During a 12-month prospective data gathering phase, details of all clinical pharmacy services in the nephrology and infectious disease wards of a large university hospital were recorded in the pharmacotherapy monitoring forms. Significance impact of clinical pharmacists’ services was assessed according to the guidelines of The Society of Hospital Pharmacists of Australia. Main outcome measure: Number and type of services provided. Results During 1 year, clinical pharmacists contributed to 1,386 services for 1,105 patients who were admitted in these two wards; of these services, about 95% were accepted by the physicians and about half of them were of moderate-to-life saving clinical significance. Also at least 32% of services were considered to reduce the cost of drug therapy. Conclusions These results support the importance of clinical pharmacists’ participation in health care team rounds to improve the overall quality of medication therapy, enhance patient care and outcome and reduce drug costs to patients and society.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Half of the interventions by clinical pharmacists in an Iranian University hospital are of moderate to life-saving significance.
-
From a financial and patient-care perspective it is good to involve a clinical pharmacist in the rounds of the medical teams in hospitals in Iran.
Introduction
Medication related problems such as adverse drug reactions (ADRs), medication errors and harmful drug interactions may result in negative clinical and economic outcomes. The cost-effectiveness of clinical pharmacy services have been shown in some healthcare settings [1–6]. Also there are reports regarding the effectiveness of clinical interventions by pharmacy students on internal medicine clerkship [7], clinical pharmacists in ambulatory clinics for high-risk patients [8], during the dispensing process [9] and in nursing homes [10]. Additionally, home-based post acute care interventions by pharmacists have been shown to reduce readmission rates, total hospital stay and hospital based costs [11]. In Iran clinical pharmacy residency was developed by few American-educated Iranian clinical pharmacists as an academic sub-specialty program for pharmacists and this program included 18-month academic courses, 18 months clinical practice in teaching hospitals and a clinical thesis. Till now, clinical pharmacy services have been provided for in-hospital patients in eight university hospitals. These clinical pharmacists participate actively in physician rounds. Their services include taking medication history on admission, providing recommendations to physicians regarding the best treatment regimen (based on drug and dosage form availability, efficacy, drug-interactions, ADRs and cost), pharmaceutical care provision to patients (including dose adjustment based on patients age, weight, kidney or liver function, ADRs prevention or management, drug–drug, drug–food or drug–disease interactions identification and management), patient education, therapeutic drug monitoring, provision of drug information to all medical team staff and patients, and preparing of drug administration guidelines. In Iran, most of the clinical pharmacists’ activities have been focused on specialized clinical areas such as infectious diseases, nephrology, oncology, psychiatry, intensive care, cardiovascular and endocrinologic diseases.
Aim of the study
This study was designed to understand (1) what types of services are provided by clinical pharmacists in nephrology and infectious disease wards? (2) Are clinical pharmacy services in nephrology and infectious disease wards accepted by physicians? (3) Is there any clinical benefit in what clinical pharmacists do in the main teaching hospital in Iran?
Methods
During a 12-month prospective data gathering phase, details of all clinical pharmacy services in the nephrology and infectious disease wards of a large university hospital affiliated to Tehran University of Medical Sciences were recorded in the pharmacotherapy monitoring forms. The nephrology and infectious disease wards contained a total of 80 beds. The monitoring forms had been previously developed for uniform documentation of all clinical pharmacy residents’ interventions in these wards and contained the demographic data of the patients (including the patients’ hospital number, age, sex, weight), past medical and drug history of the subjects, drug-therapy data (including name, dosage form and doses of drugs, their route and frequency of administrations), physical examination and disease-specific laboratory findings (including blood urea level, serum creatinine, electrolytes and uric acid concentrations, complete blood count, iron status parameters, parathyroid hormone level, serum liver enzymes concentrations, fasting and post-prandial blood glucose, urinalysis findings, blood/sputum/urine culture results). Most of the clinical pharmacy services and the basis for each service were recorded in these forms. Some of the clinical pharmacists’ activities such as educational lectures, drug utilization reviews, interventions for non-admitted patients were not recorded in these forms.
Clinical pharmacy service was defined as any recommendation by a clinical pharmacist that related to patient drug therapy whether or not it resulted in any pharmacotherapy changes by physicians. Clinical Pharmacy services were classified as: (a) improving clinical outcomes including dosage adjustment for organ dysfunction, adding necessary drug, identification and management of harmful drug–drug, drug–disease, drug–food, or drug–herbal interactions, prevention or management of ADRs, identification, prevention or management of medication errors, therapeutic drug monitoring, considering drugs’ compatibilities with parenteral solutions or other simultaneously administered injectable medications and stability of injectable drugs after opening or reconstitution, providing of drug information to patients and health-care staff and assisting patients’ adherence to drug therapy and (b) potential drug cost-saving change including reduction in drug dosage based on clinical indication, change in dosage form, frequency or route of administration (usually changing from parenteral to oral drugs), discontinuation of unnecessary medication, or switch to cheaper agent based on equal efficacy and probably less ADRs [12]. Significance impact of clinical pharmacy services were assessed according to guideline of Society of Hospital Pharmacy of Australia [13] and like other similar studies by an independent senior clinical pharmacist and a physician who did not practice in these wards to reduce bias [2].
Data that was extracted from the pharmacotherapy monitoring forms was used to feed into an Excel® spreadsheet for presentation and analysis.
Results
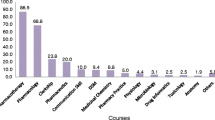
During this 1 year study, 1,105 patients with the mean age plus or minus standard deviation of 52.5 ± 14.1 years old were admitted in nephrology and infectious disease wards. A total number of 1,386 clinical pharmacy services were recorded during these 12 months in these wards; of them 1,310 (94.5%) were accepted to be prescribed by physicians. So, the rate of accepted clinical pharmacy services was 1.2 per patient. The percentage of each type of clinical pharmacy services and the clinical significance of these services has been presented in Tables 1 and 2 respectively. As seen, about half of the clinical pharmacy services consisted of discontinuation of unnecessary drugs and changing in dose or frequency of prescribed drugs and treatment duration and almost half of the services were of moderate to major clinical significance. Those clinical pharmacy services that aimed to reduce drug costs and consisted about 32% of all of interventions are summarized in Table 3.
Discussion
For the first time in Iran, this study analyzed documented services by Iranian clinical pharmacists in nephrology and infectious disease wards of a main teaching hospital and illustrated the value of those services in patient care.
Most of the clinical pharmacy services (66.2% of services) in these wards were recommendations to clarify or correct the physicians’ prescription including changes in frequency, duration or dose of prescribed drugs, discontinuation of unnecessary drugs or addition of a the missed drug to the patient’s treatment regimen, which is somewhat similar to the findings of French clinical pharmacists [14]. French pharmacists reported 66% of their interventions as a drug switch (22.2%), drug discontinuation (16.3%), addition of a new drug (3.7%) and dose adjustment (23.8%). Adding a new drug to the treatment regimen accounted for 20.8% of Iranian clinical pharmacists compared with 3.7% in the French study and this shows more missing treatment in our hospital. As mentioned by other investigators, the major cause of prescribing errors may be the result of the physicians’ lack of essential drug and patient information at the time of prescribing [15]. One method of providing such information is computerized physician order entry [16]; however, computerized ordering systems have not been provided in Iranian hospitals yet. This shows that how important the role of clinical pharmacist is in our hospitals and suggests that clinical pharmacists in hospitals can intervene as experts to select an appropriate drug treatment plan for patients. The clinical pharmacy service is much more available than computerized physician order entry. The intervention requires better utilization of pharmacists’ time rather than additional resources. Most of the pharmacists in Iranian hospitals work in the drug dispensary and are free at times in the morning when patients are visited by physicians, as drugs are not distributed to the wards then Pharmacists’ participation in medical team rounds at these times, at least in some specialized wards such as nephrology, infectious disease and intensive care, may provide pharmacy services to these complicated patients with several co-morbidities that need polypharmacy and sometimes treatment with low therapeutic index drugs.
Determining the significance of the impact of clinical pharmacy services may have been a potential source of bias however we tried to reduce it by including a senior clinical pharmacist and a physician who did not work in these wards, as evaluators. The main limitation of this study was the lack of control group. Since there was no matched control group in this study to compare the clinical outcome of patients in the intervention and control groups, the exact cost effectiveness analysis of clinical pharmacists’ activities was impossible; however, according to raw data, we partially see the pharmacoeconomically beneficial role of the clinical pharmacist in the hospital setting.
As seen in Table 3, at least 32% of clinical pharmacy services have the potential to reduce the cost of pharmacotherapy and the estimation is just based on changing the drug administration route from parenteral to oral, discontinuing of unnecessary drugs or reducing the dose based on clinical indication. If dose reductions based on organ function, changes to cheaper alternative treatment regimens, prevention of adverse events and the cost of their management, or better outcomes and shortening of hospitalization were added to this estimation, we would be able to show the real economic-justified role of clinical pharmacists in hospitals. It shows that cost saving is one of the important roles of clinical pharmacists; therefore, government and insurance systems should support clinical pharmacy services in hospitals and the health system.
In the present study clinical pharmacists provided 1.2 accepted services per patient which is less than that what reported by English pharmacists; about three interventions per patient [17]. We evaluated the clinical significance of clinical pharmacy services according to Australian standards [13] which differ from those used in European studies. Based on both consultant and clinical pharmacist opinions respectively, about half of the Iranian clinical pharmacy services were of moderate to life-saving clinical significance. In the English study 26.6 or 44.2% of the clinical pharmacists’ interventions had significant impact according to consultant or pharmacist opinion respectively [17]. In the first study in the Netherlands, 52 and 83 of 173 clinical pharmacists’ interventions (30 and 48% respectively) were evaluated as having an extremely significant to significant impact by physicians and pharmacists respectively [18]. As seen, the clinical significance of Iranian clinical pharmacists’ services is comparable to those of their European colleagues.
In the present study, the acceptance rate of clinical pharmacists’ services by physicians was about 95%. The acceptance rate of pharmacist’s recommendations differs from 36 to 38% in Australian reports [10] to 73–89% in European [14, 17, 18] and 85–99% in American reports [15, 19]. This finding shows the appreciation of Iranian physicians of clinical pharmacy services.
Conclusion
Findings of the study support the importance of clinical pharmacists’ position in improvement of the overall quality of medication therapy, enhance patient care and outcome and reduce drug costs to patients and society.
References
Schumock GT, Butter MG, Meek PD, Vermeulen LC, Arondekar BV, Bauman JL, et al. Evidence of the economic benefit of clinical pharmacy services: 1996–2000. Pharmacotherapy. 2003;23(1):113–32.
Dooley MJ, Allen KM, Doecke CJ, Galbraith KJ, Taylor GR, Bright J, et al. A prospective multicentre study of pharmacist initiated changes to drug therapy and patient management in acute care government funded hospitals. Br J Clin Pharmacol. 2003;57(4):513–21.
Clavert RT. Clinical pharmacy—a hospital perspective. Br J Clin Pharmacol. 1999;47(3):231–8.
Plumridge RJ, Wojnar-Horton RE. A review of the pharmacoeconomics of pharmaceutical care. Pharmacoeconomics. 1998;14(2):175–89.
George B, Silcock J. Economic evaluation of pharmacy services—fact or fiction? Pharm World Sci. 1999;21(4):147–51.
Bond CA, Raehl CL, Franke T. Clinical pharmacy services, pharmacy staffing, and the total costs of care in United States hospitals. Pharmacotherapy. 2000;20(6):609–21.
Plam DQ. Evaluating the impact of clinical interventions by Pharm D students on internal medicine clerkships: the results of a 3 year study. Ann Pharmacother. 2006;40:1541–5.
Malone DC, Carter BL, Billups SJ, Valuck RJ, Barnette DJ, Sintek CD, et al. An economic analysis of a randomized, controlled, multicentre study on clinical pharmacist interventions for high-risk veterans: the IMPROVE study. Pharmacotherapy. 2000;20(10):1149–58.
Hawksworth GM, Corlett AJ, Wright DJ, Chrystyn H. Clinical pharmacy interventions by community pharmacists during the dispensing process. Br J Clin Pharmacol. 1999;47(6):659–700.
Roberts MS, Stockes JA, King MA, Lynne TA, Purdie DM, Glasziou PP, et al. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. Br J Clin Pharmacol. 2001;51(3):257–65.
Stewart S, Pearson S, Luke CG, Horowitz JD. Effects of home-based intervention on unplanned readmissions and out-of-hospital death. J Am Geriatr Soc. 1998;46(2):174–80.
McMullin ST, Hennenfent JA, Ritchie DJ, Huey WY, Lonergan TP, Schaiff RA, et al. A prospective, randomized trial to assess the cost impact of pharmacist-initiated interventions. Arch Intern Med. 1999;159(19):2306–9.
Dooley MJ, Bogovic A, Carroll M, Cuell S, Galbraith K, Matthews H. SHPA standards of practice for clinical pharmacy: SHPA committee of specialty practice in clinical pharmacy. J Pharm Pract Res. 2005;35(2):122–46.
Charpiat B, Conort O, Rose FX, Escofier L, Juste M, Roubille R, et al. Assessment of clinical pharmacists’ interventions in French hospitals: results of a multicenter study. Ann Pharmacother. 2008;42(7):1095–103.
Leape LL, Cullen D, Clapp MD, Burdick E, Demonaco HJ, Erickson JI, et al. Pharmacist participation in physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;281(3):267–70.
Bates DW, Leape LL, Cullen DJ, Larid N, Petersen LA, Teich JM. Effects of computerized physician order entry and a team intervention on prevention of serous medication errors. JAMA. 1998;280:1311–6.
Dale A, Copeland R, Barton R. Prescribing errors on medical wards and the impact of clinical pharmacists. Int J Pharm Pract. 2003;11:19–24.
Bosma L, Jansman FGA, Franken AM, Harting JW, Van Den Bemt PMLA. Evaluation of pharmacist clinical interventions in a Dutch hospital setting. Pharm World Sci. 2008;30(1):31–8.
Brown C. Physicians acceptance of drug-therapy recommendations using a written data and communications form. Consult Pharm. 1991;6:729–34.
Acknowledgements
The Authors appreciate the helpful comments of Professor Michael Dooley from Monash University, Australia.
Funding
No special funding was obtained for this research.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dashti-Khavidaki, S., Khalili, H., Hamishekar, H. et al. Clinical pharmacy services in an Iranian teaching hospital: a descriptive study. Pharm World Sci 31, 696–700 (2009). https://doi.org/10.1007/s11096-009-9336-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-009-9336-6