Abstract
Objective The objectives of this study were to determine the reasons for returning medications unused and the types of unused medications returned based on therapeutic class. Setting: This study was conducted in a region of New Zealand covered by the Hutt Valley District Health Board. This region has approximately 51,000 households. Methods A ‘Disposal of Unwanted Medication Properly (DUMP)’ campaign was conducted for a four week period in November 2007 in the Hutt Valley DHB region. A collection bag was delivered to every household for the collection and disposal of any unused medications. Participants were instructed to return the bags to a community pharmacy. Those returning medications were also asked to complete a questionnaire to determine why the medications were not used. A sample of the returned medications was identified and quantified and every completed questionnaire was analysed. Main outcome measures: The main outcome measures included: types and quantities of medications returned, calculated costs of these medications and reasons for returns. Results Over the four week period, 1,605 bags were returned for disposal. A total of 329 bags (20%) containing a total of 1,253 items were fully analysed. Only 653 questionnaires were completed (41%) all of which were analysed. The most commonly reported reason for not using the medication was that it had passed the expiry date (26%), the second was treatment change (24%), followed by condition resolved (15%). ‘Alimentary tract & metabolism’ and ‘respiratory systems & allergies’ accounted for 21 and 20% of cost respectively. Conclusions This study found that main reasons identified for patients having unwanted medications were ‘treatment changes’ and ‘expired’. Additionally respiratory medications contributed 20% of the costs associated with unused medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
In New Zealand, significant amounts of medications are unused
-
The major reasons for returning medicines in New Zealand are ‘expired’ and ‘treatment changes’.
-
Respiratory medications represent 20% of the cost of returned medicines in New Zealand, and this may be an area where pharmacists can play a key role.
Introduction
Medication wastage has a huge impact worldwide, especially in monetary terms and studies have estimated this cost to be as high as NZD $9–11 billion per annum [1]. Bereavement and change of medications were found to be the most common reasons why medicines are returned while other reasons include medicines no longer needed, expired and adverse drug reactions [2–4]. A study in Sweden identified the same reasons and also concluded that excess supply and unclear instructions on prescribed medicines could be additional reasons why huge volumes of medicines are unused [5]. If prescriber changes are indeed the most common reason for medications to be returned, then policies that increase the amount issued may add to this problem.
There has been debate as to whether dispensing policies exert an impact on the volume of medication wastage. A study in the United Kingdom showed that 66% of the returned items to a pharmacy were medications that had been dispensed for greater than a 1 month period [3]. Given that monthly dispensing will incur additional dispensing and professional fees studies have investigated the financial cost of these compared to reduction in medication wastage. An American study calculated that based on prior patterns of medication refill behaviour, moving from a 100 day supply to a 34 day supply may actually increase the cost due to increased dispensing fees and this would not be offset by the predicted savings from reduced medication wastage [6].
Pharmacy in New Zealand
In New Zealand, whilst each pharmacy is individually owned and operated by a pharmacist, a government agency (Pharmac) manages the pharmaceutical schedule. Items on the schedule are either fully or partly funded by the government and the pharmacy is paid a set dispensing fee per item. There is a co-payment system where depending on socioeconomic, health status, prescriber organisation and number of items collected in a year, the patient pays either $0, $2, $3 or $15 per item.
In New Zealand ‘stat’ or all-at-once dispensing was reintroduced on the 1 October 2003. With stat dispensing 3 months supply may be given to a patient rather than just a single month and two repeats. Pharmac intended that up to 50% of all subsidised medications dispensed be available under the stat dispensing proposal. Pharmac predicted that there would be an increase in the volume of medicines collected via stat dispensing since not all patients collected all three repeats in the past, but that this might only lead to a 6% increase in dispensed medications that may be wasted. Assuming an expenditure of $599 million for medications in 2007 [7] this 6% equates to $36 million dollars potentially wasted in New Zealand. This additional cost was believed to be more than outweighed by the reduction in dispensing and professional fees paid to pharmacists and would actually lead to overall savings [8].
This policy was intended as a cost-effective measure to off-load the long term cost burden of medications from patients via government funding. This has since led to large quantities of medicines being dispensed to the New Zealand patient population, particularly those suffering from chronic medical conditions [8].
With only a population of just over 4 million people, New Zealand has 21 District Health Boards (DHB). These DHBs are geographically determined and manage health services including pharmaceutical budget for the people living in the defined DHB area. Many DHBs are investigating medication wastage to determine potential savings if this was wastage was minimised. Our group has previously conducted two smaller pilot studies in the Otago DHB region [9, 10] and found that the top 20 returned tablets had been dispensed in 3 month lots, and that the main reason for having unused medications was ‘changed to other therapy’. This current research was to investigate the situation in the Hutt Valley DHB (HVDHB) region and to determine the types and reasons why medications are unused.
Aim of the study
The aims of this study were to determine the reasons for returning medications unused and the types of unused medications based on therapeutic classification.
Method
A ‘Disposal of Unwanted Medication Properly (DUMP)’ campaign was conducted for a 4 week period in November 2007 in the Hutt Valley DHB region.
Posters explaining the campaign, the dates and process for disposal were displayed in each of the 31 community pharmacies in the Hutt Valley DHB region and pamphlets were distributed with dispensed medications in the 10 days before the collection phase began.
Plastic DUMP bags with instructions were distributed with community newspapers (Hutt News in Lower Hutt and The Leader in Upper Hutt). These newspapers go to all households in their respective communities (approx. 51,500 households). Bags were also provided to sheltered homes for mental health consumers and additional bags were provided to the pharmacies.
Participants were instructed to place all unwanted medication into the provided bags and then to return the bags to their local community pharmacy for appropriate disposal. When the bags were brought into the pharmacy, the pharmacy staff encouraged those returning the medications to complete a brief questionnaire in the pharmacy, based on one used previously [10]. As recognition of the time involved by the pharmacies, each pharmacy was given NZD $200 and an additional NZD $5 per bag returned to a maximum of NZD $300.
The questionnaire had five sections:
-
1.
Age group of owner(s) of medications
-
2.
Reason for medications not being used (a list of 10 options was provided, and an ‘other’ option)
-
3.
A question about medication subsidy status
-
4.
An estimation of the value of the returned medications
-
5.
The usual storage location of the medications
All completed questionnaires were collated and analysed.
Due to the volume of returns a sample was analysed. For convenience and to ensure that no individual pharmacy was over represented, every fifth bag was placed aside for detailed analysis. The content of each bag was collated and the following information recorded: generic name, trade name, strength, form, quantity, subsidy amount, full subsidy status and therapeutic classification (based on Anatomical Therapeutic Category (ATC)).
Only prescribed medication was included in the analysis, any over the counter medications or other items such as contact lens solution was recorded in the miscellaneous group but excluded from cost analysis.
All individual tablets and capsules were counted. Liquid medications were quantified by the amount left in the original container, semisolid preparations were estimated as a proportion of original container. Inhalers were recorded as either full, half-full or empty. Anything almost empty was excluded from the analysis.
The subsidy amount and cost per unit were taken from the New Zealand Pharmaceutical Schedule April 2007. This schedule dictates the amount that pharmacies are reimbursed for the medications dispensed based upon the brand and the strength dispensed. This allowed the cost of each medication returned to be calculated.
The totals for each individual medication was calculated, both quantity and cost. The number of items based on each therapeutic category was also counted as was the calculated cost. All non-prescription medications and any prescription items where the patient pays the full cost (i.e. sildenafil) were counted but excluded from the cost analysis.
Results
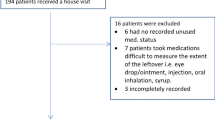
Over the 4 week period, 1,605 bags were returned for disposal. A total of 329 bags (20%) were fully analysed. Of the 1,605 returns, only 653 questionnaires were completed (41%) all of which were analysed.
The age distribution of the patients with unused medications was, <20 (8%), 21–40 (13%), 41–60 (28%), 61–80 (40%) and those over 81 years (11%). The reasons for not using the medications are listed in Table 1.
The 329 bags analysed contained 1,253 items. The items returned were identified and quantified by therapeutic group, number returned and cost.
All individual medications were counted and Table 2 shows the top 20 most returned generic item based on number and Table 3 based on cost. For comparison, the top 20 most prescribed items for the year ending June 2007 [7] are given in Table 4. For all items, differing strengths and brands are combined. Additionally items that are issued in three monthly lots are indicated by (*) and inhaled medications are indicated by (^).
Of the top 20 items returned by number, 17 are issued as 3 months all-at-once (nine based on cost). With respect to cost inhalers represent a significant proportion (seven of the top 20). Only eight of the most returned items appear in the top 20 most prescribed (diclofenac sodium, aspirin, paracetamol, prednisone, simvastatin, calcium carbonate, omeprazole, cilazapril).
Table 5 shows the breakdown of returned items based on therapeutics grouping. Both the cost and number of returns are shown. The total cost of the returned medicines that were analysed was $17,100. This value is the manufacturer’s price and so does not include any professional fees such as dispensing fees.
Discussion
Reasons for medication not being used
The largest group of patients returning medications, were those in the 61–80 age range, this aligns with the New Zealand Ministry of Heath Annual Report [11] which shows increased spending on subsidised GP-prescribed medications with increasing age and may not necessarily indicate that this age group uses less of their prescribed medications. However there is some evidence that inappropriate prescribing may decrease adherence in elderly patients [12].
The two main reasons indicated for the medications not being used were ‘treatment changes’ (24%) and ‘passed expiry date’ (26%) (Table 1). This ‘treatment change’ and ‘expired medication’ is consistent with other published studies [2, 13, 14]. The finding of ‘treatment change’ is important as the most likely time for changes in prescribed medications for a patient’s condition is during the early phases of treatment [2] and so it may be prudent not to dispense an entire 3 months supply of medications when treatment is being initiated. ‘Trial’ prescriptions have been implemented in Canada, where a small amount of a new medication is dispensed and if tolerated then the remainder is collected. They found that these ‘trial’ prescriptions were well tolerated by patients and if focused on specific medications, could reduce the direct cost of medication wastage [15].
The large number of expired medication responses was unexpected as the majority of these medications had not expired. Respondents may have ticked this option for medications that had not been used for a period of time. The large number of ‘expired’ medications may also highlight the fact that patients are over supplied with medications for acute conditions and then store the rest in case needed later. This may be particularly true for ‘as required’ medications.
Types of medication returned
The therapeutic groups responsible for the most returns were ‘nervous system’, ‘alimentary tract & metabolism’ and cardiovascular (Table 5). This finding is consistent with other studies [2, 13, 16]. However when comparing based upon the cost of the returns, the ‘respiratory’ group represents only 8% of returns by number, but 20% of the cost. Looking at the high cost returned medications; seven of the 20 are inhaled medications.
Research has shown that accidental and intentional non-adherence is common [17] and that this as well as underuse of inhaled corticosteroids and overuse of short acting β-agonists consume significantly more health care resources [18]. The adherence to asthma treatment is important to maintain asthma control [19]. Appropriate and regular use of preventer medications may reduce reliever medication and result in clinical improvements [20] and reduce the financial waste. There is current evidence that pharmacists can play an important role in improving therapeutic outcomes for asthmatic patients by improving inhalation technique and adherence [20].
Patient adherence to prescribed therapy (especially with chronic illness) is often not ideal [21]. Approximately 50% of patients who have been prescribed chronic medication for the first time stop using them within a matter of months [22]. This may explain the high number of metformin and levodopa returned (Table 2).
Amount of medication supplied
Of the most returned items by number, eight of the top 20 are also on the top 20 for prescriptions written according to Pharmac’s data (Table 4) [7]. It follows that the more prescriptions written, the more that may be unused simply due to the amount issued. Many items in this list (nine) are ‘prn’ or ‘as required’ medications (i.e. analgesics, antiemetics and treatment for constipation). In New Zealand if a prescriber does not specify a quantity the pharmacist is obligated to dispense the maximum.
Limitations
There are some limitations to this study. Firstly the amount of returned medications may be a significant underestimate given the number of patients who dispose of unwanted medications with household rubbish [23]. This may have limited the number of returns possible there may be a loss of accuracy in our findings, and the returns may only represent a sub-section of the HVDHB population.
Secondly, by not analysing every bag we may have missed an opportunity to identify other areas to investigate and are relying on the fact that the sample chosen was representative. In particular, it has been reported that 50% of medications returned are from 10% of the patients [5] and in our smaller pilot study one individual returned over $14,000 worth of unused medications [10].
Conclusions
This study found that main reasons identified for patients having unwanted medications were ‘treatment changes’ and ‘expired’. Additionally respiratory medications contributed 20% of the costs associated with unused medications.
References
Daughton CG. Cradle-to-cradle stewardship of drugs for minimizing their environmental disposition while promoting human health. II. Drug disposal, waste reduction, and future directions. Environ Health Perspect. 2003;111(5):775–85.
Langley C, Marriott J, Mackridge A, Daniszewski R. An analysis of returned medicines in primary care. Pharm World Sci. 2005;27(4):296–9.
Daniszewsi R, Langley C, Marriott J, Wilson K, Clewes P, Wilkinson M. An investigation of medicines returned to general practitioners and community pharmacies. Int J Pharm Pract. 2002;10(S):R42.
Braybrook S, John D, Leong K. A survey of why medicines are returned to pharmacies. Pharm J. 1999;263(7063):13–5.
Ekedahl AB. Reasons why medicines are returned to Swedish pharmacies unused. Pharm World Sci. 2006;28(6):352–8.
Domino ME, Olinick J, Sleath B, Leinwand S, Byrns PJ, Carey T. Restricting patients’ medication supply to one month: saving or wasting money? Am J Health Syst Pharm. 2004;61(13):1375–9.
Pharmaceutical Management Agency (Pharmac). Annual Review 2007. http://www.pharmac.govt.nz/2007/11/21/PHARMAC_AR_2007.pdf. Last accessed 7 Apr 2009.
Brady K. Pharmaceutical Management Agency: changes to the frequency of medicine dispensing. Office of the Auditor-General; 2005. http://www.oag.govt.nz/2005/pharmac/docs/pharmac.pdf. Accessed 4 Mar 2006.
Braund R, Yuen Y, Jung J. Identification and quantification of medication returned to Otago pharmacies. NZ Fam Physician. 2007;34:258–62.
Braund R, Chuah F, Gilbert R, Gn G, Soh A, Tan L, et al. Identification of the reasons for medication returns. NZ Fam Physician. 2008;35(4):248–52.
Ministry of Health Annual Report - Health and Independence. 2005. http://www.moh.govt.nz/moh.nsf/pagesmh/5315/$File/annual-report0506.pdf. Last accessed 7 Apr 2009.
Mansur N, Weiss A, Beloosesky Y. Is there an association between inappropriate prescription drug use and adherence in discharged elderly patients? Ann Pharmacother. 2009;43:177–84.
Coma A, Modamio P, Lastra CF, Bouvy ML, Marino EL. Returned medicines in community pharmacies of Barcelona, Spain. Pharm World Sci. 2008;30(3):272–7.
Cameron S. Study by Alberta pharmacists indicates drug wastage a “mammoth” problem. CMAJ. 1996;155(11):1596–8.
Paterson JM, Anderson GM. “Trial” prescriptions to reduce drug wastage: results from Canadian programs and a community demonstration project. Am J Manag Care. 2002;8(2):151–8.
Mackridge AJ, Marriott JF. Returned medicines: waste or a wasted opportunity? J Public Health (Oxf). 2007;29(3):258–62.
Ulrik CS, Backer V, Soes-Petersen U, Lange P, Harving H, Plaschke PP. The patient’s perspective: adherence or non-adherence to asthma controller therapy? J Asthma. 2006;43(9):701–4.
Anis AH, Lynd LD, Wang XH, King G, Spinelli JJ, Fitzgerald M, et al. Double trouble: impact of inappropriate use of asthma medication on the use of health care resources. CMAJ. 2001;164(5):625–31.
Molimard M, Le Gros V. Impact of patient-related factors on asthma control. J Asthma. 2008;45(2):109–13.
Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Annemans L, Remon JP, et al. Effectiveness of pharmacist intervention for asthma control improvement. Eur Respir J. 2008;31(4):790–9.
Osterberg L, Blaschke T. Adherence to medication. New Engl J Med. 2005;353(5):487–97.
Hugtenburg JG, Blom AT, Kisoensingh SU. Initial phase of chronic medication use; patients’ reasons for discontinuation. Br J Clin Pharmacol. 2006;61(3):352–4.
Braund R, Peake BM, Shieffelbien L. Disposal practices for unused medications in New Zealand. Environ Int. 2009;35:952–5.
Acknowledgements
Hutt Valley DHB and their local pharmacies for their participation.
Funding
New Zealand Pharmacy Education Research Fund for the funding of the summer studentship for GG.
Conflicts of interest statement
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braund, R., Gn, G. & Matthews, R. Investigating unused medications in New Zealand. Pharm World Sci 31, 664–669 (2009). https://doi.org/10.1007/s11096-009-9325-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-009-9325-9