Abstract
Purpose
The pyrimidine analogue gemcitabine (dFdC) is frequently used in the treatment of patients with solid tumors. However, after i.v. application dFdC is rapidly inactivated by metabolization. Here, the potential of thermosensitive liposomes based on 1,2-dipalmitoyl-sn-glycero-3-phosphodiglycerol (DPPG2-TSL) were investigated as carrier and targeting system for delivery of dFdC in combination with local hyperthermia (HT).
Methods
DPPG2-TSL were prepared by the lipid film hydration and extrusion method and characterized by dynamic light scattering, thin layer chromatography, phosphate assay and HPLC. In vivo experiments were performed in Brown Norway rats with a syngeneic soft tissue sarcoma. Local HT treatment was performed by light exposure.
Results
DPPG2-TSL were stable at 37°C in serum and showed a temperature dependent dFdC release >40°C. Plasma half-life of dFdC was strongly increased from 0.07 h (non-liposomal) to 0.53 h (liposomal, vesicle size 105 nm) or 2.59 h (liposomal, 129 nm). Therapy of BN175 tumors with dFdC encapsulated in DPPG2-TSL + HT showed significant improvement in tumor growth delay compared to non-liposomal dFdC without HT (p < 0.05), non-liposomal dFdC with HT (p < 0.01), and liposomal dFdC without HT (p < 0.05), respectively.
Conclusions
Gemcitabine encapsulated in DPPG2-TSL in combination with local HT is a promising tool for the treatment of solid tumors. Therefore, these encouraging results ask for further investigation and evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pro-drug and pyrimidine analogue gemcitabine (2′, 2′-difluorodeoxycytidine, dFdC) has been approved for treatment of non-small lung, pancreatic, bladder and breast cancer (1,2), but showed also clinical activity in a variety of other solid tumors including soft tissue sarcomas (3–6). The pro-drug enters the cell via nucleoside transporters and is subsequently phosphorylated to gemcitabine triphosphate (dFdCTP) (7). The mechanism of action of dFdCTP is the competition with deoxycitidine triphosphate for incorporation into DNA, inhibition of DNA replication and subsequent induction of apoptosis. Furthermore, the drug is rapidly metabolized inside cells by deoxycytidine deaminase to inactive difluorodeoxyuridine and excreted into the bloodstream (7). Liposomal encapsulation of dFdC was used to protect the drug from rapid metabolization (8,9). This also increased the therapeutic efficacy of the drug in animal models by passive targeting of the vesicles to the tumor via the enhanced permeability and retention effect (10). Nevertheless, conventional liposomes like long-circulating PEGylated liposomal doxorubicin (Caelyx®/Doxil®) failed to show an improvement in clinical efficacy in humans compared to free drug (11). The proportion of accumulated liposomes in the tumor tissue was below 5% of the injected dose (12). PEGylated liposomes like Caelyx® are highly stable and the bioavailability of the drug is low (13). The carrier is taken up by cells via endocytosis, transferred to the lysosomal compartment and therefore the drug delivery to the nucleus was impaired (14). Therefore it would be of advantage to increase the local concentration of bioavailable drug in the diseased tissue by triggered drug release.
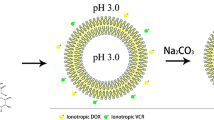
Thermosensitive liposomes (TSL) in combination with local hyperthermia (HT) or high intensity focused ultrasound (HIFU) are a promising tool to reach this goal (Fig. 1) (15–18). Recently a new paradigm for the clinical application of TSL was published (19). Intravascular doxorubicin (DOX) release from lysolipid-based TSL inside the heated tumor vasculature increased the concentration of bioavailable drug in the interstitial space, compared to conventional PEGylated liposomes. Moreover, the penetration depth of the drug inside tumors was significantly increased.
Principle of intravascular drug release from thermosensitive liposomes (TSL). Drug release occurs by passive transfer across the lipid membrane driven by the concentration gradient. The membrane bilayer forming phospholipids change from a solid gel (Lβ) to a liquid disordered (Lα) phase at their phase transition temperature (Tm). The Lα phase is characterized by a higher permeability compared to the Lβ phase because of higher disorder and movement in the phospholipid packing. Permeability is largest around Tm because of the coexistence of membrane areas in both phases and is further increased by disturbances in lipid packing, induced by lipid incorporation, lipid loss and interaction with blood components. Novel TSL are designed to release the drug into the blood stream when passing the heated tumor area. This approach requires a sufficient high drug release rate. The schema is not drawn to scale. HT, local hyperthermia; HIFU, high intensity focused ultrasound.
At present, most of the studies with TSL formulations used DOX for encapsulation. Only a small number of studies used other drugs such as neomycin (20), dacarbazin (21), melphalan (22), mitomycin C (23), miltefosine (24), and cisplatin (25). Objective of the present study was to encapsulate dFdC, a promising drug candidate, into a TSL formulation capable of intravascular drug release at mild hyperthermic conditions (41°C). We chose 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC)/1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC)/1,2-dipalmitoyl-sn-glycero-3-phosphodiglycerol (DPPG2) 50/20/30 (mol/mol) TSL (DPPG2-TSL) because of their fast release kinetics and high in vitro stability in serum (26,27), combined with superior in vivo half-life (28). A reversed phase high performance liquid chromatography (HPLC) method was established to quantify dFdC in aqueous samples. dFdC was passively encapsulated into preformed DPPG2-TSL and the resultant vesicles were characterized by HPLC and dynamic light scattering (DLS). Phospholipid composition, shelf life during preparation and storage were investigated by thin layer chromatography (TLC). The temperature dependent dFdC release was followed in vitro. The therapeutic effect of the resultant TSL was further investigated in a rat sarcoma model.
Materials and Methods
Chemicals
The synthetic phospholipid DPPG2 was synthesized as described previously (29). DPPC and DSPC were purchased from Corden Pharma Switzerland LLC (Liestal, Switzerland). Gemzar® (38 mg/ml dFdC) was obtained from Lilly Deutschland GmbH (Bad Homburg, Germany). 5-fluorouridine was from Sigma Aldrich GmbH (Munich, Germany). All other chemicals were either from Carl Roth GmbH (Karlsruhe Germany) or Sigma Aldrich GmbH (Munich, Germany). All solutions were exclusively prepared with deionized and purified water from the ultrapure water system (Milli Q Advantage, Millipore).
Preparation of DPPG2-TSL
TSL were prepared by the lipid film hydration and extrusion method (26,27). The phospholipids were dissolved in chloroform in a round-bottom flask in a molar ratio of DPPC/DSPC/DPPG2 50/20/30. Thereafter the solvent was removed in a rotary evaporator to obtain a homogeneous dry lipid film. The film was hydrated in 20 mM HEPES, 150 mM NaCl (HN buffer), pH 7.4 at 60°C. Unilamellar vesicles were formed after a tenfold high pressure extrusion (LIPEXTM thermobarrel extruder, Northern Lipids Inc. Burnaby, BC, Canada) through polycarbonate membranes of a defined pore size (100 or 200 nm).
Passive Loading of dFdC to DPPG2-TSL
The drug was passively loaded to pre-formed DPPG2-TSL. This was previously shown for other liposomal formulations (8) and drugs (25). In the present study DPPG2-TSL were diluted 1/1 (vol/vol) with Gemzar® at 4°C to a final dFdC concentration of 18 mg/ml (68.4 mM) and the dispersion was subsequently transferred to a thermoshaker (Eppendorf, Hamburg, Germany) and incubated for 30 min at 60°C under shaking (750 rpm). The dispersion was concentrated by centrifugation with an Avanti J-26XP centrifuge (rotor JA 25.50, 75,600×g, 60 min, 15°C). The supernatant was discarded and the pellet was suspended with one third of the initial TSL volume using HN buffer pH 7.4. TSL were further purified by size exclusion chromatography with PD-10 columns (GE Healthcare, Munich, Germany) using HN buffer pH 7.4 as eluent to remove non-encapsulated dFdC.
Characterization of DPPG2-TSL
TSL preparations have been characterized as previously described in detail (26,27). The hydrodynamic diameter (z average), size intensity distribution plot and zeta potential were determined by DLS (Zetasizer Nano ZS, Malvern Instruments, Worcestershire, United Kingdom). The instrument was calibrated with a NanosphereTM size standard (125 nm, Thermo Fisher Scientific, Waltham, MA, USA). Phospholipid composition and shelf life was quantitatively measured with TLC. TLC plates were developed with chloroform/methanol/acetic acid (97.5%)/water 100/60/10/5 (vol/vol) to achieve the separation of phosphatidylcholines (DPPC, DSPC) from DPPG2, lyso-phosphatidylcholine (Lyso-PC) and lyso-phosphatidyldigylcerol (Lyso-PG2). A lipid standard containing DPPG2, DPPC and 1-palmitoyl-sn-glycero-3-phosphocholine (P-Lyso-PC) was applied in every TLC run to check the separation quality. Phospholipid concentration was measured by phosphate analysis (30) using a 1 g/l phosphate solution (Merck KGaA, Darmstadt, Germany) as reference standard.
Temperature and Time Dependent dFdC Release
DPPG2-TSL with encapsulated dFdC were diluted 1/12 (vol/vol) in HN buffer pH 7.4 or fetal calf serum (FCS) at room temperature. 120 μl of this solution was incubated in a pre-heated thermoshaker. The sample reached the desired incubation temperature within a few seconds. Please refer to the Results section for the particular conditions. After incubation, each sample was diluted with 200 μl ice cold HN buffer pH 7.4 to stop the experiment and was immediately transferred to Millipore Amicon® Ultra-0.5 ultrafiltration tubes (30 kDa MWCO, Merck KGaA, Darmstadt, Germany) and centrifuged (14,000×g, 10 min). The filtrate contained non-liposomal dFdC and the drug concentration was measured with HPLC. Drug release was calculated as:
cT is the concentration of non-liposomal dFdC after incubation of the sample for the time period t at the temperature T, c0% is the baseline concentration of non-liposomal dFdC without any incubation, and c100% is obtained after disrupting the TSL by addition of 10% Triton X-100 instead of HN buffer pH 7.4 and subsequent incubation at 45°C for 15 min.
High Performance Liquid Chromatography
Quantification of dFdC from aqueous samples was performed with HPLC using a previously published method (31), which was modified as described below. Samples (30 μl) were diluted with 10 μl internal standard (IS, 250 mg/ml 5-fluorouridine in 10 mM KH2PO4 pH 7), 170 μl phosphate buffered saline and 400 μl acetonitrile. After vigorous mixing, the sample was centrifuged (19,000×g, 6 min) and 500 μl of the supernatant was transferred to a fresh glass tube. The solvent was removed (40°C, steady stream of nitrogen) and the dry sediment was dissolved in 400 μl 10 mM KH2PO4 pH 7. The sample was transferred to HPLC injection tubes after centrifugation (19,000×g, 10 min). Runs were performed with a Waters HPLC system (Waters 515 HPLC pumps, Waters 717plus autosampler, and Waters 490E multiwavelength detector) with a C18 column (Kinetex®, 100 mm × 3 mm, 2.6 μm particle size; 100 Å pore size, Phenomenex Ltd., Aschaffenburg, Germany) together with a μBondapakTM C18 pre-column (Waters GmbH, Eschborn, Germany). 50 μl per sample was injected and eluted with an isocratic flow of 0.5 ml/min using 10 mM KH2PO4 pH 7 as mobile phase. The column was heated to 40°C. The wavelength for detection was 275 nm. Gemzar® was used for the preparation of the calibration samples. Pooled human plasma (blood bank of the University hospital of Munich) was spiked with 0, 20, 50 and 100 ng/μl dFdC to obtain calibration samples. Please refer to the Supplementary Material for further information on recovery, linearity, specifity and precision of the method.
Cell Culture
The rat tumor cell line BN175 (soft tissue sarcoma, Brown Norway rat; kindly provided by Timo ten Hagen, Erasmus MC, Rotterdam) was grown in RPMI 1640 medium supplemented with 10% FCS (vol/vol), 100 U/ml penicillin and 100 μg/ml streptomycin, respectively. Medium and supplements were obtained from Biochrom AG (Berlin, Germany). Cells were cultured at 37°C in a humidified atmosphere of 95% air and 5% CO2.
In Vitro Toxicity Assay
The cells were seeded in 96 well plates in 100 μL culture medium (BN175 5,000 cells per well). The medium was removed after 24 h and distinct concentrations of dFdC (0.4 nM to 2,486 nM) in 100 μL RPMI 1640 medium with 20 mM HEPES supplemented with 10% FCS (vol/vol) (Biochrom AG, Berlin, Germany) were added. The plates were closed by taping and submerged in a water bath at either 37°C or 41°C for 60 min. Afterwards 100 μl of standard cell culture medium was added and the cells were incubated for another 48 h under standard condition. For analysis 20 μL WST-1 reagent (Roche Diagnostics, Mannheim, Germany) was added to each well. Absorption was measured after 1 h with an ELISA reader at 450 nm (MRX, Dynex Technologies, Chantilly, USA). The results were fitted with OriginPro 8.1.5 (OriginLab Corp., Northhampton, MA, USA) to Eq. 2:
S(c) is the percentage of surviving cells that were treated with a concentration c of dFdC compared to cells receiving no drug. The median lethal dose (LD50) value was directly obtained from the point of inflection (c0) based on 50% of dead cells.
Animals
All animal studies were performed in accordance to protocols approved by the responsible authority (Regierung of Oberbayern, Az. 55.2-1-54-2532-144-11). Male inbreed Brown Norway rats weighing 250 to 350 g where obtained from Charles River GmbH (Sulzfeld, Germany). The animals were housed in cages in groups of three, in a temperature controlled environment with a 12-h light/dark cycle and with free access to standard chow (ssniff Spezialdiäten GmbH, Soest, Germany) and water. All experimental procedures were performed under anesthesia (isofluran 2–5% and oxygen 1.5 l/min).
Pharmacokinetic Study
Free dFdC and DPPG2-TSL with encapsulated dFdC, at a dose of 6 mg dFdC per kg, were injected intravenous (i.v.). Blood samples were collected at different time points (please refer to the Results section for the particular time points) in lithium heparin microvettes (Sarstedt, Nümbrecht, Germany), centrifuged and the resulting plasma was stored at −20°C until quantification with HPLC. The plasma concentration of dFdC was fitted with OriginPro 8.1.5 to a two compartment pharmacokinetic model:
where c(t) is the dFdC concentration at time t after i.v. application, kα and kβ are the rate constants of elimination and the initial dFdC concentration at t = 0 h is given by c(0) = Aα + Aβ. The plasma half-lives of both phases were calculated with Eq. 4:
The area under the curve (AUC0-6h) was calculated by integration of Eq. (3) from t = 0 to 6 h.
Therapeutic Study
Fragments (2–2.5 mm) of soft tissue sarcoma BN175 were transplanted subcutaneously on the left hind leg of the rats. Tumor growth was recorded by caliper measurements every second day and the volume was calculated using an ellipsoid approximation V = π/6(abc). Treatment was initiated when one diameter was over 0.5 cm. The tumor was locally heated with a cold-light source (Photonic PL2000, Photonic Optics, Vienna, Austria) (Fig. 2). For groups treated with HT, intratumoral temperature and rectal body temperature were monitored with probes. When tumor temperature reached 41°C the animals were injected with 6 mg per kg dFdC formulations i.v. and the 60 min heating period started.
Setup for small animal local hyperthermia (HT) with light exposure: (1) device for inhalation anesthesia, (2) cold light source, (3) tumor bearing hind leg, (4) swab with hole to protect healthy tissue from light exposure, (5) hyperthermia treatment, (6) rectal temperature probe, (7) catheter for venous access, (8) measured body temperature, (9) measured tumor temperature.
Statistical Analysis
Data were shown as the mean value ± standard deviation of at least three independent experiments. Two-sample t-tests (OriginPro 8.1.5) were used to determine whether the mean values of two samples were statistically different or not.
Results
Passive Encapsulation of dFdC into DPPG2-TSL
To avoid a contamination of the high-pressure extruder device with dFdC and to ensure a safe handling during preparation the drug was loaded passively into preformed vesicles. In initial experiments HN buffer pH 7.4 was identified as optimal buffer for passive loading (data not shown). Moreover, an incubation temperature of 60°C yielded the fastest uptake rates compared to 40°C (data not shown). Next, the optimal loading time was determined to be 30 min, indicated by the highest molar dFdC to phospholipid ratio without any change in zeta potential, z average, and polydispersity index (PDI) over time (Fig. 3). The phospholipid concentration of the dispersion affected the encapsulation efficacy of dFdC. Encapsulation efficacy after 30 min at 60°C increased from 2.6% to 5.5% when the phospholipid concentration was increased from 10 mM to 50 mM. In contrast, molar dFdC to phospholipid ratio was hardly affected by the phospholipid concentration in the dispersion. Nevertheless, the occurrence of larger aggregates after 60 min of incubation was more prominent in samples with a lipid concentration above 25 mM, whereas for samples below 25 mM vesicle size slightly increased without observable aggregate formation (Fig. 3e). This indicated a superior stability of vesicles at lower phospholipid concentrations. No Lyso-PC formation was detectable during the first 20 min of loading, but content increased with time to 1.1% ± 1.2% after 60 min.
Influence of gemcitabine (dFdC) loading time at 60°C on biophysical parameters of DPPG2-TSL. (a) Loading was optimal after 30 min, indicated by the highest molar dFdC to phospholipid ratio (n = 4). (b) Zeta potential of the resultant DPPG2-TSL did not change during 60 min of loading (n = 4). (c) Z average (n = 4), and (d) polydispersitiy index (PDI) remained constant during 45 min of incubation but markedly increased at 60 min (n = 4). (e) Representative intensity distribution plots obtained from dynamic light scattering measurements of DPPG2-TSL incubated for either 10 or 60 min in presence of dFdC. The occurrence of larger aggregates after 60 min was more prominent for dispersions with higher phospholipid concentrations.
In Vitro Characterization of DPPG2-TSL Encapsulating dFdC
dFdC was passively loaded to pre-formed DPPG2-TSL containing HN buffer pH 7.4 by 30 min incubation at 60°C. Up to 13 independent batches were prepared and characterized to investigate the reproducibility of the preparation method (Table I). The method was feasible to prepare DPPG2-TSL batches with a satisfying batch-to-batch reproducibility in vesicle size, PDI, zeta potential, molar dFdC to phospholipid ratio and DPPG2 content. The intensity plots measured with DLS revealed narrow size distributions without any larger aggregates present (data not shown). Both, the lipid concentration and dFdC to phospholipid ratio were high enough to allow an i.v. bolus injection in rats with a dFdC dosage of 6 mg drug per kg body weight.
Phospholipid stability during preparation was investigated by TLC to quantify hydrolysis products of DPPC, DSPC and DPPG2. Lyso-PG2 and Lyso-PC contents were low and reached 0.6 ± 1.1% and 1.3 ± 1.1%, respectively. In 6 of 16 batches no lysolipids were detectable. Batches with a Lyso-PC content > 1.5 mol% (n = 5) were excluded from the experiments. Batches are immediately stored at −20°C after preparation to avoid the formation of additional lysolipids during storage.
The in vitro dFdC release from DPPG2-TSL could be triggered by mild hyperthermic temperatures (Fig. 4). In HN buffer pH 7.4, less than 6% dFdC was released during 5 min of incubation at temperatures ≤41°C. Above 41°C the dFdC release was increased and reached 25.7 ± 12.8% and 41.5 ± 14.0% at 42 and 43°C, respectively. Presence of serum components further increased the dFdC release to 66.1 ± 18.8% and 81.8 ± 15.0% at 42 and 43°C, respectively. The effect of serum on drug release is described for a wide range of TSL formulations (26,27,32). Moreover, a tendency to faster dFdC release at temperatures above 40°C was observed when decreasing the vesicle size from 143 nm to 109 nm (Fig. 4, inset).
In vitro gemcitabine (dFdC) release from DPPG2-TSL. Vesicle size (z average) was 138 nm. Temperature dependent release profile was measured either in 20 mM HEPES, 150 mM NaCl pH 7.4 (buffer, n = 5) or fetal calf serum (FCS, n = 9). Inset: Representative measurements with DPPG2-TSL of different vesicle size in FCS.
Stability in FCS at 37°C was good with less than 20% release after 6 h of incubation. Leakage of dFdC was 4.2 ± 1.0%, 7.7 ± 10.6% 15.8 ± 11.6%, and 15.3 ± 10.7% after 1, 2, 4, and 6 h of incubation (n = 5), respectively.
The mean measured baseline concentration of non-encapsulated dFdC (c0%) was 15.6 ± 9.2%. Assuming that non-encapsulated dFdC was completely removed by size exclusion chromatography during TSL preparation, c0% is the amount of dFdC leaking from DPPG2-TSL during rapid dilution.
In Vitro Cytotoxicity of dFdC
The cytotoxic effect of dFdC in the BN175 cells is shown in Fig. 5. LD50 of dFdC obtained for BN175 at 37°C (-HT) and 41°C (+HT) was 24.0 nM ± 2.8 nM and 24.9 nM ± 2.6 nM, respectively. Furthermore, cytotoxicity was similar, if HT was applied after a 24 h-exposure to dFdC (data not shown).
Pharmacokinetic Study
Figure 6 shows the stability of DPPG2-TSL with encapsulated dFdC compared to free dFdC after i.v. administration of 6 mg dFdC per kg body weight. The data was exponentially fitted to a two compartment PK model as described in Materials and Methods. The results are presented in Table II. Free dFdC was rapidly cleared from blood with an initial plasma half-life (tα) of 0.07 h. Liposomal encapsulation significantly increased tα of dFdC in blood to 0.53 h and 2.59 h for vesicles with a size of 105 nm and 129 nm, respectively. Even 24 h after TSL administration there was still dFdC detectable in the plasma samples (0.5 ± 0.8 μg/ml for the smaller and 2.2 ± 0.2 μg/ml for the larger TSL, respectively). The AUC0-6h was doubled when vesicle size was increased from 109 to 129 nm (Table II).
Pharmacokinetic study in Brown Norway rats following an intravenous injection of free dFdC and encapsulated in DPPG2-TSL at a dose of 6 mg/kg dFdC (n = 3). The data was fitted to a two compartment pharmacokinetic model (solid lines, please refer to Table II for the calculated parameters).
Therapeutic Study
Treatment of BN175 tumors in rats was performed with a single i.v. injection of 6 mg dFdC per kg body weight. Five groups have been chosen: 0.9% saline with HT, non-liposomal dFdC without HT, non-liposomal dFdC with HT, dFdC encapsulated in DPPG2-TSL without HT and dFdC encapsulated in DPPG2-TSL with HT (mean vesicle size of 141 nm). HT treatment lasted 60 min and drugs were injected after the tumor reached a temperature of 41°C. Rats treated with all tested dFdC formulations showed a temporary decrease in tumor volume, which was not observed for the saline control (Fig. 7). HT had no additional therapeutic effect when non-liposomal dFdC was applied (Fig. 7, triangles). This correlated with the results from the cell culture study (Fig. 5). The treatment with liposomal dFdC with HT was most effective and differed significantly from non-liposomal dFdC with HT (p < 0.01), non-liposomal dFdC without HT (p < 0.05), and liposomal dFdC without HT (p < 0.05) (Fig. 7). Obvious regional or systemic toxicity was only observed in 2 rats treated with liposomal dFdC without HT by developing skin lesions on the tails 6 and 14 days after treatment (Fig. 7, inset).
Therapeutic study with gemcitabine (dFdC) encapsulated in DPPG2-based thermosensitive liposomes. A relative change of the tumor volumes (V/V0) of the s.c. implanted soft tissue sarcoma BN175 was observed after treatment with 6 mg per kg of non-liposomal dFdC with local hyperthermia (HT) (n = 6), dFdC without HT (n = 10), dFdC encapsulated in DPPG2-TSL without HT (n = 6), or dFdC encapsulated in DPPG2-TSL with HT (n = 6) compared to the untreated control: saline with HT (n = 9). Inset: skin lesions after treatment with DPPG2-TSL without HT.
Discussion
TSL offer the possibility of heat induced localized therapy with the advantage of reduced side effects. The lipid membrane shields healthy tissue from cytotoxicity of the encapsulated drug. Moreover, the drug is protected from metabolization before reaching target tissue. Because of the short in vivo half-life of dFdC after i.v. injection (Fig. 6) encapsulation in TSL might be a major opportunity to increase chemotherapeutic efficacy of this potent cytostatic drug. Objective of the present study was to investigate this assumption in a proof of concept study in the BN175 model, since dFdC is used in therapy of soft tissue sarcomas (3–5).
A passive loading method of dFdC to preformed DPPG2-TSL was applied, which allowed a safe handling without contamination of equipment during preparation. Biophysical properties like vesicle size, polydispersity index and zeta potential remained unaffected during 30 min loading time at 60°C (Fig. 3). Overall, the method yielded TSL with high batch-to-batch reproducibility (Table I). The drug encapsulation efficacy was as expected < 10%. This result is comparable to other passive lipid film hydration methods where phospholipid concentrations below 50 mM have been used (28). Nevertheless, encapsulation efficacy might be significantly increased by applying alternative preparation methods like the dual asymmetric centrifugation method (33). TLC analysis revealed the occurrence of lysolipids in 10 of 16 TSL batches, which could be attributed to the drug loading conditions. During the first 20 min of loading no lysolipids were detected, but the amount increased to 1.1% ± 1.2% after 60 min. The pH of the pre-formed DPPG2-TSL drops from 7.4 to ~3 after addition of the acidic drug stock solution. Together with the incubation temperature of 60°C, these are optimal conditions for phospholipid hydrolysis (34). All preparations were stored at −20°C immediately after preparation to avoid the generation of additional lysolipids, especially because dFdC promotes the hydrolysis of phospholipids in a concentration-dependent manner (35). Nevertheless, the total amount of lysolipids after preparations was acceptable low (< 1.5%) and had no negative effect on drug retention. DPPG2-TSL retained more than 80% of dFdC when incubated for 6 h at 37°C in FCS.
For the cell line SW1573 and R-1 it was previously shown, that the timing of dFdC and HT exposure is important. Results showed that a simultaneous application leads to a similar or decreased cell killing effect of dFdC, dependent on cell line and temperature (36,37). Our cell culture experiments with the BN175 cells did not show a difference if treated with dFdC alone or with simultaneous application of mild HT of 41°C (Fig. 5). This fact gave the opportunity to observe the cytotoxicity of the liposomal carrier and targeting system itself without biased results caused by hyperthermia damage.
In the therapeutic study (Fig. 7) we found a significant tumor growth delay with HT triggered dFdC release from TSL compared to all the other treatment groups. While the saline with HT treated control did not show a decrease in tumor volume in the days after treatment, all dFdC formulations induced an inhibition in tumor growth. The simultaneous application of non-liposomal dFdC and HT neither influenced the treatment significant synergistic nor in decreasing cytotoxicity of the drug. It was previously shown that the schedule for HT application was important for the efficacy of the treatment. Results of a rat R-1 rhabdomyosarcoma model showed a drug potentiating effect of HT (70 min, 43°C) with 20 mg dFdC per kg body weight when HT was applied 48 h after dFdC treatment (37). In this experiments the simultaneous addition of HT had no effect on tumor growth delay compared to dFdC alone. This nicely fits to our results. Since objective of the present study was to selectively deliver dFdC to the tumor and to show an improvement in tumor therapy with HT triggered drug release, we decided against a second HT treatment yet. However, in future experiments it would be worth to test whether further HT treatments before and/or after heat-triggered drug delivery could potentiate the anti-tumor effect. The advantage of a pre-HT treatment is that tumor vessels open up for improved extravasation and a second heat trigger would increase interstitial drug release (38). The improved tumor growth delay and the observed skin reactions in the group treated with dFdC encapsulated in DPPG2-TSL without HT compared to the non-liposomal treated groups (Fig. 7) are supporting evidences for the long circulation time of the used formulation. It was shown before, that liposomal dFdC and the resulting non-targeted sustained release of the drug causes a higher anti-tumoral activity accompanied by a significant decrease of the maximum tolerable dose compared to free dFdC (39). The triggered intratumoral release gives an opportunity of uniform high intravascular dFdC concentrations over the duration of 60 min HT treatment in the target tissue. A clinical pharmacokinetic study demonstrated the advantage in accumulation of dFdCTP in cells obtained with a fixed dose rate infusion (1,500 mg/m2 over 150 min) compared to a standard infusion therapy (2,200 mg/m2 over 30 min) (40). An explanation is the extended exposure duration of the cells to the drug. Thereby, the risk for saturation of the dFdC activating enzyme inside the cells (41–43) will be reduced.
Nevertheless, the treatment with HT triggered dFdC from TSL is only resulting in a small retardation in tumor growth compared to the free drug or liposomal drug without HT (Fig. 7). This may be explained by the very fast growing tumor model, the single low dFdC dose (6 mg per kg) or related to the DPPG2-TSL formulation. In the pharmacokinetic study (Fig. 6, Table II) the initial plasma concentration at t = 0 h was calculated to be 112.7 μg/ml for DPPG2-TSL with a vesicle size of 129 nm. However, the expected theoretical c(0) calculated from dosage was 150 μg/ml assuming that 4% of the body weight is plasma. The difference might be explained by an initial drug leakage during bolus injection which was shown in vitro by a dFdC leakage of 15.6 ± 9.2% upon rapid dilution. The reason for the occurrence of this effect may be suddenly appearing pressure on the vesicle membrane (44) or interactions of the bilayer with serum compounds (32). The temperature dependent dFdC release in serum (Fig. 4) showed that marked dFdC release occurred at temperatures ≥42°C. In the therapeutic study, however, the tumor tissue was heated only to 41°C, which might be not sufficient to generate high dFdC concentration inside the tumor tissue. This could be improved by optimization of the TSL formulation to release dFdC at lower temperatures or by achieving higher temperatures in the target tissue. Light exposure is a simple HT technique but limits the intratumoral temperature to 41°C. Increasing tumor temperatures >41°C would cause skin damages by formation of crusts or oedemas in the surrounding tissue. However, higher intratumoral temperatures could be easily reached by alternative heating techniques as HIFU (17,45).
Our in vitro (Fig. 4, inset) and in vivo (Fig. 6, Table II) results showed a higher stability of DPPG2-TSL when increasing the vesicle size. This fits to previous in vitro observations with DPPG2-TSL encapsulating carboxyfluorescein or DOX (27). A decrease in vesicle size significantly increases the membrane curvature (46). This leads to packing defects and loser packing of the phospholipids and results in a higher membrane permeability causing an increase in release rates of hydrophilic compounds (27). The lower dFdC retention at 37°C for smaller vesicles results in a faster drug inactivation and clearance from blood. Therefore the more stable DPPG2-TSL with a vesicle size of 139 nm have been chosen for the therapeutic study, since a high plasma level during the HT treatment is a prerequisite for an effective drug targeting to the tumor tissue (19,47).
Conclusion
Thermosensitive liposomes are promising for gemcitabine targeting to solid tumors in combination with local hyperthermia. Selective gemcitabine release from phosphatidyldiglyerol-based thermosensitive liposomes by local hyperthermia showed a significant tumor growth delay in rats compared to free drug. As postulated from in vitro results (27), the pharmacokinetic profile of the encapsulated drug was influenced by vesicle size. In vivo half-life of gemcitabine was increased by increasing vesicle size from 105 to 129 nm. Nevertheless, further improvements are required to obtain optimal performance of gemcitabine encapsulated in phosphatidyldiglyerol-based thermosensitive liposomes.
Abbreviations
- dFdC:
-
gemcitabine
- dFdCTP:
-
gemcitabine triphosphate
- DLS:
-
dynamic light scattering
- DPPC:
-
1,2-dipalmitoyl-sn-glycero-3-phosphocholine
- DPPG2 :
-
1,2-dipalmitoyl-sn-glycero-3-phosphodiglycerol
- DPPG2-TSL:
-
liposomes composed of DPPC/DSPC/DPPG2 50/20/30 (mol/mol)
- DSPC:
-
1,2-distearoyl-sn-glycero-3-phosphocholine
- FCS:
-
fetal calf serum
- HPLC:
-
high performance liquid chromatography
- HT:
-
local hyperthermia
- i.v.:
-
intravenous
- IS:
-
internal standard
- Lyso-PC:
-
lyso-phosphatidylcholine
- Lyso-PG2 :
-
lyso-phosphatidyldiglycerol
- P-lyso-PC:
-
1-palmitoyl-sn-glycero-3-phosphocholine
- TLC:
-
thin layer chromatography
- Tm :
-
solid gel to liquid disordered phase transition temperature
- TSL:
-
thermosensitive liposomes
References
Heinemann V. Gemcitabine: progress in the treatment of pancreatic cancer. Oncology. 2001;60(1):8–18.
Toschi L, Finocchiaro G, Bartolini S, Gioia V, Cappuzzo F. Role of gemcitabine in cancer therapy. Future Oncol. 2005;1(1):7–17.
Hensley ML, Maki R, Venkatraman E, Geller G, Lovegren M, Aghajanian C, et al. Gemcitabine and docetaxel in patients with unresectable leiomyosarcoma: results of a phase II trial. J Clin Oncol. 2002;20(12):2824–31.
Maki RG, Wathen JK, Patel SR, Priebat DA, Okuno SH, Samuels B, et al. Randomized phase II study of gemcitabine and docetaxel compared with gemcitabine alone in patients with metastatic soft tissue sarcomas: results of sarcoma alliance for research through collaboration study 002. J Clin Oncol. 2007;25(19):2755–63.
Garcia-Del-Muro X, Lopez-Pousa A, Maurel J, Martin J, Martinez-Trufero J, Casado A, et al. Randomized phase II study comparing gemcitabine plus dacarbazine versus dacarbazine alone in patients with previously treated soft tissue sarcoma: a Spanish Group for Research on Sarcomas study. J Clin Oncol. 2011;29(18):2528–33.
Movva S, Verschraegen C. Systemic management strategies for metastatic soft tissue sarcoma. Drugs. 2011;71(16):2115–29.
Mini E, Nobili S, Caciagli B, Landini I, Mazzei T. Cellular pharmacology of gemcitabine. Ann Oncol. 2006;17 suppl 5:v7–12.
Bornmann C, Graeser R, Esser N, Ziroli V, Jantscheff P, Keck T, et al. A new liposomal formulation of Gemcitabine is active in an orthotopic mouse model of pancreatic cancer accessible to bioluminescence imaging. Cancer Chemother Pharmacol. 2008;61(3):395–405.
Jantscheff P, Esser N, Graeser R, Ziroli V, Kluth J, Unger C, et al. Liposomal gemcitabine (GemLip)-efficient drug against hormone-refractory Du145 and PC-3 prostate cancer xenografts. Prostate. 2009;69(11):1151–63.
Maeda H. The enhanced permeability and retention (EPR) effect in tumor vasculature: the key role of tumor-selective macromolecular drug targeting. Adv Enzyme Regul. 2001;41:189–207.
Judson I, Radford JA, Harris M, Blay JY, van Hoesel Q, Le Cesne A, et al. Randomised phase II trial of pegylated liposomal doxorubicin (DOXIL/CAELYX) versus doxorubicin in the treatment of advanced or metastatic soft tissue sarcoma: a study by the EORTC Soft Tissue and Bone Sarcoma Group. Eur J Cancer. 2001;37(7):870–7.
Harrington KJ, Mohammadtaghi S, Uster PS, Glass D, Peters AM, Vile RG, et al. Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Cancer Res. 2001;7(2):243–54.
Laginha KM, Verwoert S, Charrois GJ, Allen TM. Determination of doxorubicin levels in whole tumor and tumor nuclei in murine breast cancer tumors. Clin Cancer Res. 2005;11(19 Pt 1):6944–9.
Seynhaeve ALB, Dicheva BM, Hoving S, Koning GA, ten Hagen TLM. Intact Doxil is taken up intracellularly and released doxorubicin sequesters in the lysosome: Evaluated by in vitro/in vivo live cell imaging. J Control Release. 2013;172(1):330–40.
Lindner LH, Hossann M. Factors affecting drug release from liposomes. Curr Opin Drug Discov Devel. 2010;13(1):111–23.
Landon CD, Park J, Needham D, Dewhirst MW. Nanoscale drug delivery and hyperthermia: the materials design and preclinical and clinical testing of low temperature-sensitive liposomes used in combination with mild hyperthermia in the treatment of local cancer. Open Nanomed J. 2011;3:38–64.
Grüll H, Langereis S. Hyperthermia-triggered drug delivery from temperature-sensitive liposomes using MRI-guided high intensity focused ultrasound: drug delivery research in Europe. J Control Release. 2012;161(2):317–27.
May JP, Li S. Hyperthermia-induced drug targeting. Expert Opin Drug Deliv. 2013;10(4):511–27.
Manzoor AA, Lindner LH, Landon CD, Park J, Simnick AJ, Dreher MR, et al. Overcoming limitations in nanoparticle drug delivery: triggered, intravascular release to improve drug penetration into tumors. Cancer Res. 2012;72(21):5566–75.
Yatvin MB, Weinstein JN, Dennis WH, Blumenthal R. Design of liposomes for enhanced local release of drugs by hyperthermia. Science. 1978;202(4374):1290–3.
Chelvi TP, Ralhan R. Designing of thermosensitive liposomes from natural lipids for multimodality cancer therapy. Int J Hyperthermia. 1995;11(5):685–95.
Chelvi TP, Ralhan R. Hyperthermia potentiates antitumor effect of thermosensitive-liposome-encapsulated melphalan and radiation in murine melanoma. Tumour Biol. 1997;18(4):250–60.
Hosokawa T, Sami M, Kato Y, Hayakawa E. Alteration in the temperature-dependent content release property of thermosensitive liposomes in plasma. Chem Pharm Bull (Tokyo). 2003;51(11):1227–32.
Lindner LH, Hossann M, Vogeser M, Teichert N, Wachholz K, Eibl H, et al. Dual role of hexadecylphosphocholine (miltefosine) in thermosensitive liposomes: active ingredient and mediator of drug release. J Control Release. 2008;125(2):112–20.
Woo J, Chiu GN, Karlsson G, Wasan E, Ickenstein L, Edwards K, et al. Use of a passive equilibration methodology to encapsulate cisplatin into preformed thermosensitive liposomes. Int J Pharm. 2008;349(1–2):38–46.
Hossann M, Wiggenhorn M, Schwerdt A, Wachholz K, Teichert N, Eibl H, et al. In vitro stability and content release properties of phosphatidylglyceroglycerol containing thermosensitive liposomes. Biochim Biophys Acta. 2007;1768(10):2491–9.
Hossann M, Wang T, Wiggenhorn M, Schmidt R, Zengerle A, Winter G, et al. Size of thermosensitive liposomes influences content release. J Control Release. 2010;147(3):436–43.
Lindner LH, Eichhorn ME, Eibl H, Teichert N, Schmitt-Sody M, Issels RD, et al. Novel temperature-sensitive liposomes with prolonged circulation time. Clin Cancer Res. 2004;10(6):2168–78.
Eibl H. Synthesis of glycerophospholipids. Chem Phys Lipids. 1980;26(4):405–29.
Eibl H, Lands WE. A new, sensitive determination of phosphate. Anal Biochem. 1969;30(1):51–7.
Lanz C, Früh M, Thormann W, Cerny T, Lauterburg BH. Rapid determination of gemcitabine in plasma and serum using reversed-phase HPLC. J Sep Sci. 2007;30(12):1811–20.
Hossann M, Syunyaeva Z, Schmidt R, Zengerle A, Eibl H, Issels RD, et al. Proteins and cholesterol lipid vesicles are mediators of drug release from thermosensitive liposomes. J Control Release. 2012;162(2):400–6.
Massing U, Cicko S, Ziroli V. Dual asymmetric centrifugation (DAC)–a new technique for liposome preparation. J Control Release. 2008;125(1):16–24.
Grit M, Crommelin DJ. Chemical stability of liposomes: implications for their physical stability. Chem Phys Lipids. 1993;64(1–3):3–18.
Moog R, Brandl M, Schubert R, Unger C, Massing U. Effect of nucleoside analogues and oligonucleotides on hydrolysis of liposomal phospholipids. Int J Pharm. 2000;206(1–2):43–53.
Haveman J, Rietbroek RC, Geerdink A, van Rijn J, Bakker PJ. Effect of hyperthermia on the cytotoxicity of 2′,2′-difluorodeoxycytidine (gemcitabine) in cultured SW1573 cells. Int J Cancer. 1995;62(5):627–30.
van Bree C, Beumer C, Rodermond HM, Haveman J, Bakker PJ. Effectiveness of 2′,2′difluorodeoxycytidine (Gemcitabine) combined with hyperthermia in rat R-1 rhabdomyosarcoma in vitro and in vivo. Int J Hyperthermia. 1999;15(6):549–56.
Li L, ten Hagen TLM, Bolkestein M, Gasselhuber A, Yatvin J, van Rhoon GC, et al. Improved intratumoral nanoparticle extravasation and penetration by mild hyperthermia. J Control Release. 2013;167(2):130–7.
Moog R, Burger AM, Brandl M, Schuler J, Schubert R, Unger C, et al. Change in pharmacokinetic and pharmacodynamic behavior of gemcitabine in human tumor xenografts upon entrapment in vesicular phospholipid gels. Cancer Chemother Pharmacol. 2002;49(5):356–66.
Tempero M, Plunkett W, van Ruiz HV, Hainsworth J, Hochster H, Lenzi R, et al. Randomized phase II comparison of dose-intense gemcitabine: thirty-minute infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J Clin Oncol. 2003;21(18):3402–8.
Hughes TL, Hahn TM, Reynolds KK, Shewach DS. Kinetic analysis of human deoxycytidine kinase with the true phosphate donor uridine triphosphate. Biochemistry. 1997;36(24):7540–7.
Grunewald R, Kantarjian H, Keating MJ, Abbruzzese J, Tarassoff P, Plunkett W. Pharmacologically directed design of the dose rate and schedule of 2′,2′-difluorodeoxycytidine (Gemcitabine) administration in leukemia. Cancer Res. 1990;50(21):6823–6.
Abbruzzese JL, Grunewald R, Weeks EA, Gravel D, Adams T, Nowak B, et al. A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol. 1991;9(3):491–8.
Hallett FR, Marsh J, Nickel BG, Wood JM. Mechanical properties of vesicles. II. A model for osmotic swelling and lysis. Biophys J. 1993;64(2):435–42.
Hijnen NM, Heijman E, Kohler MO, Ylihautala M, Ehnholm GJ, Simonetti AW, et al. Tumour hyperthermia and ablation in rats using a clinical MR-HIFU system equipped with a dedicated small animal set-up. Int J Hyperthermia. 2012;28(2):141–55.
Hatzakis NS, Bhatia VK, Larsen J, Madsen KL, Bolinger P, Kunding AH, et al. How curved membranes recruit amphipathic helices and protein anchoring motifs. Nat Chem Biol. 2009;5(11):835–41.
Koning GA, Eggermont AMM, Lindner LH, ten Hagen TLM. Hyperthermia and thermosensitive liposomes for improved delivery of chemotherapeutic drugs to solid tumors. Pharm Res. 2010;27(8):1750–4.
Acknowledgments And Disclosures
The authors gratefully acknowledge the help of E. Wagner (Department of Pharmaceutical Biology-Biotechnology, Ludwig-Maximilians University, Munich, Germany) for providing facilities.
The research leading to these results has received funding from the European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 603028 (iPaCT project).
Chemical compounds studied in this study: DSPC (Pubmed CID 94190), DPPC (Pubmed CID 452110), DPPG2 (no Pubmed CID available, CAS 495403-05-9), dFdC (Pubmed CID: 60749).
The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 404 kb)
Rights and permissions
About this article
Cite this article
Limmer, S., Hahn, J., Schmidt, R. et al. Gemcitabine Treatment of Rat Soft Tissue Sarcoma with Phosphatidyldiglycerol-Based Thermosensitive Liposomes. Pharm Res 31, 2276–2286 (2014). https://doi.org/10.1007/s11095-014-1322-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1322-6