Abstract
Purpose
To investigate, for the first time, the influence of pharmacist intervention and the use of a patient information leaflet on self-application of hydrogel-forming microneedle arrays by human volunteers without the aid of an applicator device.
Methods
A patient information leaflet was drafted and pharmacist counselling strategy devised. Twenty human volunteers applied 11 × 11 arrays of 400 μm hydrogel-forming microneedle arrays to their own skin following the instructions provided. Skin barrier function disruption was assessed using transepidermal water loss measurements and optical coherence tomography and results compared to those obtained when more experienced researchers applied the microneedles to the volunteers or themselves.
Results
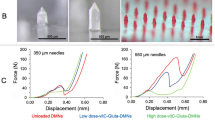
Volunteer self-application of the 400 μm microneedle design resulted in an approximately 30% increase in skin transepidermal water loss, which was not significantly different from that seen with self-application by the more experienced researchers or application to the volunteers. Use of optical coherence tomography showed that self-application of microneedles of the same density (400 μm, 600 μm and 900 μm) led to percentage penetration depths of approximately 75%, 70% and 60%, respectively, though the diameter of the micropores created remained quite constant at approximately 200 μm. Transepidermal water loss progressively increased with increasing height of the applied microneedles and this data, like that for penetration depth, was consistent, regardless of applicant.
Conclusion
We have shown that hydrogel-forming microneedle arrays can be successfully and reproducibly applied by human volunteers given appropriate instruction. If these outcomes were able to be extrapolated to the general patient population, then use of bespoke MN applicator devices may not be necessary, thus possibly enhancing patient compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microneedle arrays (MN) are minimally-invasive devices that painlessly by-pass the skin’s stratum corneum, which is the principal barrier to topically-applied drugs. MN (50–900 μm in height, up to 2000 MN cm-2) have been extensively investigated in recent years as a means to enhance transdermal drug and vaccine delivery (1,2). Indeed, MN arrays have already successfully delivered oligonucleotides, desmopressin, DNA, vaccines, insulin and human growth hormone in vivo in both animal models and in human clinical trials (1–4).
A 2012 report from Greystone Associates, Microneedles in Medicine: Technology, Devices, Markets and Prospects, puts the potential MN drug delivery market at just under $400 million globally (5). Since MN are frequently targeted not only to the $20 billion transdermal drug delivery and $25 billion global vaccine markets, but also to the $120 billion global biologics market, significant further growth is anticipated. While the first two MN-based products, just recently marketed, Soluvia® and Micronjet®, are based on metal and silicon MN, respectively, the current trend in MN-based research has involved recognition of the dubious biocompatibility of silicon and the potential for inappropriate reuse of silicon or metal microneedles, which remain fully intact after removal from a patient’s skin. Consequently, much recent effort has focussed on MN prepared from FDA-approved biocompatible polymers (1,4). Initially, such systems were prepared from hot polymer/carbohydrate melts. However, the high processing temperatures led to degradation of the biomolecular cargoes (6). Accordingly, an increasing emphasis has been placed on MN formulated from aqueous polymer gels (7–10). We have recently described novel hydrogel-forming MN arrays, prepared under ambient conditions that contain no drug themselves (10). Instead, they rapidly imbibe skin interstitial fluid upon insertion to form continuous, unblockable conduits between the dermal microcirculation and an attached patch-type drug reservoir. In so-doing, we have overcome one of the noted limitations of dissolving polymeric MN, in that delivered doses of biomolecules are no longer limited to what can be loaded into the needles themselves (8,10). Such hydrogel-forming MN initially act simply as a tool to pierce the stratum corneum barrier and then function as a rate-controlling membrane, allowing sustained delivery of high doses of biomolecules. Importantly, such MN are removed intact from skin, leaving no polymer residue behind, but are sufficiently softened, even after 1 min of skin insertion to preclude reinsertion, thus further reducing the risk of transmission of infection (10,11).
MN devices are not equivalent to conventional transdermal patches, in that they are not simply applied to the skin surface. Rather MN function principally by breaching the skin’s protective stratum corneum barrier and often penetrate into the viable epidermis and dermis (1,12). It is now well known that the depth of MN penetration is influenced not only by the force applied, but also MN geometry (height, shape, interspacing) and speed of application (12–15). A plethora of MN applicator devices have been described and evaluated (16). However, in our experience as pharmacists, even the most simple devices, such as inhalers and pessary applicators, can be improperly used by patients and, very often, patients are discouraged from using a medicinal product if they perceive its use to be overly complex. It is our view that MN-based products would be most successful commercially, and in terms of patient acceptance, if they can be applied by a patient to their own skin without an additional applicator device or the need for assistance from a skilled medical practitioner. Accordingly, in this study, we describe, for the first time, the influence of pharmacist intervention and the use of a patient information leaflet on self-application of hydrogel-forming MN arrays by human volunteers.
Materials and Methods
Chemicals
Gantrez® AN-139, a copolymer of methyl vinyl ether and maleic anhydride (PMVE/MAH, Mw = 1,080,000) was a gift from Ashland (Kidderminster, UK). Poly(ethylene glycol) (PEG, molecular weight 10,000 Da) was purchased from Sigma-Aldrich (Steinheim, Germany). Millipore water was used throughout the study, while all other chemicals used were of analytical reagent grade. Moisture-impermeable, heat-sealable poly(ester) foils were purchased from Transparent Film Products Ltd (Newtownards, UK).
Fabrication of Hydrogel-Forming MN Arrays
Aqueous blends containing 15% w/w poly(methylvinylether/maelic acid) (PMVE/MA) and 7.5% w/w poly(ethyleneglycol) 10,000 (PEG) were utilized to fabricate MN by using laser-engineered silicone micromould templates (7,8,10). MN were prepared of three heights; 400 μm, 600 μm and 900 μm, each arranged in 11 × 11 configurations on a 0.5 cm2 area, with a MN-free border to give a final patch area of 1.0 cm2. Optimum polymeric composition was previously determined in our previous hydrogel work (10,17,18). MN were crosslinked (esterification reaction) by heating at 80°C for 24 h (10,17,18), and the sidewalls formed by the moulding process removed using a heated blade.
MN packages were produced from moisture-impermeable, heat-sealable poly(ester) foil, measuring 4.0 cm × 5.0 cm (Transparent Film Products Ltd, Newtownards, UK). MN produced were placed in the foil packaging and sealed using a heat sealer (P400/L Impulse Heat Sensor Heat Press, Polybags Ltd, Middlesex, UK). The arrays were then stored individually in these packages under ambient conditions until required for application.
Volunteer Recruitment
Twenty healthy Volunteers (8 men and 12 women) aged between 21 and 23 years old from the final year student population at the School of Pharmacy, Queen’s University Belfast, with no pre-existing skin conditions were recruited to the study by means of an email circular. Individuals conducting research projects on microneedles were excluded from the study to reduce subject bias. Volunteers were asked not to apply cosmetic formulations to their ventral forearm 24 prior to the study and to avoid hot showers/baths or exercise immediately before the study. Volunteers were provided with information on the study, the risks associated and the confidentiality of the results obtained upon recruitment. The School of Pharmacy Ethical Committee, Queen’s University Belfast, approved this study. All Volunteers provided fully-informed consent prior to beginning the study.
Patient Information Leaflet and Counselling
Patient information leaflets (PILs) are normally supplied with medicinal products and medical devices where the patient is expected to use them by themselves at home. Upon dispensing such items for the first time to a patient, it is normal practice for the pharmacist to provide expert counselling.
The PIL used in this study (Fig. 1) was designed on the basis of existing PILs for transdermal patches and devices that require a more descriptive protocol, such as inhalers for treatment of asthma. The views of MN researchers, pharmacy practice researchers and also of those with no clinical background were considered in the design of the PIL. The PIL was then checked for best practice against the criteria laid out in “Quality Criteria for PILs” published by the MHRA (19) to ensure it was of an appropriate standard.
A strategy for counselling was then developed, again following discussion with MN researchers and pharmacy practice researchers. This counselling consisted of details about MN technology, removal of the MN array from the impermeable packaging, how to hold and apply the MN (force required was described as “pressing an elevator button firmly”) and finally how to remove and dispose of the array (Table I).
Volunteer Application Protocol
The study was conducted at a controlled room temperature of 20°C and a relative humidity of 45 ± 5%. The subjects were acclimatised in this room for 15 min prior to the start of the experiment. During this time, subjects were presented with the PIL and allowed to read the application technique of MN arrays alongside counselling from the Researcher (KM, a newly-qualified pharmacist with 1 month experience of MN application). Each application used a new MN array. Two circular areas were then marked on the right ventral forearm and one on the left ventral forearm and numbered 1, 2 and 3 respectively (in ball-point pen measuring approximately 1.5 cm2). The circular areas were located at similar positions on each forearm. Before the Volunteers applied the MN arrays, baseline transepidermal water loss (TEWL) values were recorded to give an indication of skin barrier function (VapoMeter®, Delfin Technologies Ltd, Kuopio, Finland). TEWL measures the outward diffusion of water through the skin and, as such, provides information on the barrier status (20). Measurement of TEWL by evaporimeter is often used as an alternative to invasive measures of skin barrier obtained by local excision or biopsy. Indeed, the technique has been frequently used in MN-based studies, due to its patient-friendly non-invasive nature and capability for rapid data generation (21–24). TEWL measurements were taken by carefully resting the TEWL probe horizontally on the application site, with the probe head vertical and perpendicular to the skin, the TEWL values were recorded for a period of 10–15 s and the values expressed in g m−2 h−1.
Each subject was then presented with the 400 μm MN array design within its package, and asked to apply the MN to circle 1 on their right ventral forearm for 30 s following the steps detailed in the PIL. Once the subject had immediately removed the MN array from their forearm, the TEWL was again measured. This circle of skin was then left untouched for 30 min before another TEWL reading was taken.
The second MN application was performed on circle 2 on the right ventral forearm, this time by the Researcher. A baseline TEWL was taken again before application of the array and then immediately after removal of the array and at 30 min post-removal. The third microneedle application was performed on circle 3 on the left ventral forearm by the Volunteer again. This time the subject was given no PIL or Researcher counselling, but relied on experience from their former application and that of the Researcher. A baseline and immediate post-removal TEWL reading were measured. Volunteers were revisited after 24 h to check for any adverse skin sensations or reactions during that period.
Control experiments investigating variability in TEWL values were conducted with 4 additional Volunteers, whose skin was not punctured using MN. TEWL values for these Volunteers were measured on each arm on four occasions over two separate 30 min periods on the same day.
Researcher Application Protocol
Self-application by the Researcher was conducted in the same environment as that detailed in 2.5 above. Five circular areas were marked on the researcher’s left and right ventral forearms (10 in total), at approximately the same location on each forearm (marked in ball-point pen, approximately 1.5 cm2). There was, obviously, no requirement for a PIL or counselling in this application protocol. The Researcher acclimatised to the environment for 15 min prior to application. Prior to application, baseline TEWL values were again recorded for each of the circles. The Researcher then applied a 400 μm design MN array for 30 s to the circular areas on the ventral forearm and, upon removal, a second TEWL reading was taken. This was repeated for each of the 10 circles. Each circular area was left untouched for 30 min before the final TEWL reading was measured.
Experienced Operator Protocol
Self-application by an “Experienced Operator” (AZA, A Lecturer in Pharmaceutics with 2 years’ experience of application of MN to human Volunteers in vivo) was conducted in the same environment as that detailed in 2.5 above. Five circular areas were marked on the operator’s right ventral forearm (marked in ball-point pen, approximately 1.5 cm2). There was again no requirement for a PIL or counselling in this application protocol. The Experienced Operator acclimatised to the environment for 15 min prior to application.
Prior to application, baseline TEWL values were recorded for each of the circles. The Experienced Operator then applied a 400 μm design MN array for 30 s to the circular areas on the ventral forearm and upon removal a second TEWL reading was taken. This was repeated for each of the 5 circles. Each circular area was left untouched for 30 min before the final TEWL reading was measured.
Questionnaire
A structured questionnaire, consisting of 7 fixed questions, was devised to consider the subjects’ thoughts and opinions of MN technology, and the application process. Questionnaires were designed in consultation with MN and pharmacy practice researchers and piloted with staff and postgraduate students in the School of Pharmacy. Following agreed amendments, and with full ethical approval, the questionnaires were administered to the Volunteers once the application protocol was complete. The questionnaire was used to discover the Volunteers’ thoughts about MN self-application and also their overall opinion about the technology (scale strongly positive to strongly negative 1–5). Data obtained was analysed by Microsoft Excel® (Microsoft Corporation, Redmond, USA). Where Volunteers provided additional opinions outside the structured questionnaire, their responses were recorded and considered in detail in order to identify trends and opportunities to enhance the patient experience when using microneedle-based products.
Penetration Depth Investigation
Since TEWL indicates the degree of skin barrier disruption rather than MN penetration depth or the diameter of the created micropores, and since penetration depth and micropore diameter upon application are likely to be important determinants of interstitial fluid uptake by, and subsequent drug delivery from, hydrogel-forming MN arrays, additional studies were conducted using the minimally-invasive skin imaging technique optical coherence tomography (OCT). Five additional Volunteers were recruited according to the protocol detailed above. Following pharmacist counselling, and having read the PIL during acclimatisation to the study environment, the Volunteers applied an array of the 400 μm, 600 μm and 900 μm MN to each of the three circles marked on their forearms. The Researcher and Experienced Operator both did the same. In addition to TEWL measurements, taken as before, OCT (VivoSight™ Topical Multi-Beam OCT Handheld Probe, Michelson Diagnostics Ltd, Kent, UK) was used, as described previously (10–12), to study MN penetration depth and micropore diameter. Data was presented as means (± S.D.) of 10 replicate measurements of MN penetration depth and the diameter of the corresponding micropore for MN of the same array, where the MN penetration depth/micropore diameters were selected at random from the 121 penetrating MN in each array. Quantification was performed using the imaging software ImageJ® (National Institute of Health, USA). The scale of the image files obtained was 1.0 pixel = 4.2 μm, thus allowing accurate measurements of the depth of MN penetration and the diameter of micropores created.
Statistical Analysis
Statistical analysis was performed using Prism 4® for Windows (Graphpad, San Diego, USA). Analysis was performed using the Mann–Whitney U-Test. In all cases, p < 0.05 denoted significance.
Results
Table II shows the influence of Volunteer self-application of MN following pharmacist counselling and Volunteer reading of a PIL. TEWL values were significantly increased (p < 0.001) following immediate MN removal in both cases, with an approximate increase of TEWL of 30% from baseline values. Application to the left arm was performed following application of MN to the right arm of Volunteers by the Researcher (Table III). Researcher application again led to a significant increase in TEWL values, though the increase was again in the order of 30% and was not significantly different to the results obtained from either of the Volunteer self-applications (p = 0.8392 and 0.6073 for right arm and left arm, respectively). In all cases, TEWL values had returned to almost baseline values 30 min post-MN removal, indicating restoration of skin barrier function. A similar pattern of TEWL increase was seen when the MN were self-applied by the Researcher (Table IV). No significant difference was found between the increase in TEWL immediately post-MN removal when comparing the pooled Volunteer data (self-application to right and left arm) with the Researcher self-application data (p = 0.0708). Data obtained for self-application by the Experienced Operator again followed a familiar pattern, with no significant difference in the increase in TEWL as compared to the pooled Volunteer self-application data (p = 0.0832). When MN were not applied to skin, TEWL values changed little. For the 4 Volunteers studied in this control experiment, their initial mean TEWL was 9.1 g m−2 h−1 (Range: 7.2–12.0). When measured 30 min later, the mean TEWL was again 9.1 g m−2 h−1 (Range: 5.3–10.7). When measured again later the same day, their initial mean TEWL was 8.6 g m−2 h−1 (Range: 7.0–10.8). When measured 30 min later, the mean TEWL was 8.5 g m−2 h−1 (Range: 7.2–9.8) (Table V).
OCT experiments (Fig. 2) revealed no marked differences in the width of created micropores (Table VI), regardless of MN height or applicant (Volunteer, Researcher, Experienced Operator). However, as MN height was increased, progressive increases were seen in the depth of MN penetration beyond the stratum corneum for all applicants (Table VI). This was mirrored by progressive increases in TEWL values as MN height was increased (Table VII). Interestingly, the percentage of the needle shaft that penetrated beyond the stratum corneum decreased as MN height increased (Table VIII). This was consistent, regardless of the applicant, with no significant differences (p > 0.05 in each case) in percentage penetration between the Volunteers and the Researcher, the Researcher and the Experienced Operator or the Volunteers and the Experienced Operator at each of the MN heights.
The questionnaire was used to highlight the Volunteers’ views on MN, as it is now widely accepted that obtaining the opinions of the eventual users of medical technology is important and they should have a greater involvement (25). Volunteer’s views on MN are likely to help those involved in MN development towards producing an end product that is acceptable to the general patient population. Data was grouped according to identifiable themes and individual Volunteer statements summarised and categorised for the purposes of tabulation (Table IX). For example, “Would different people apply different amounts of pressure to the microneedle?” and “What about patients having different skin thickness?” became “Inter-patient variability in applying pressure or skin thickness”.
All 20 Volunteers stated that MN could be transferred and used by the public effortlessly, but only if an appropriate PIL and counselling by a pharmacist was available. Furthermore, subjects agreed that the use of a placebo would be good for the public to practice before application. Table IX also displays the Volunteers’ perceived advantages of the technology, with the main benefits stated being those over hypodermic injection with less painful administration, self-administration, reduced fear and needle-stick injuries being raised by all 20 Volunteers. Despite the Volunteers being able to recognise the key benefits of the technology, they were also wary about some perceived limitations, as 16 Volunteers were unsure if they had applied enough pressure to successfully insert the MN and also 9 Volunteers stated that if a drug was present they wouldn’t be confident that it would have entered the body. The majority of Volunteers questioned how much the technology would cost as compared to traditional injections and 14 volunteers wondered whether MN could be used as immediate release formulations. In spite of the possible disadvantages that were discussed by Volunteers, 80% stated that their overall view of MN technology was strongly positive, the remainder being positive, with no negative views expressed.
Discussion
MN technology is one of the most promising developments made in drug delivery over the past decades and possesses numerous advantages over conventional means of transdermal delivery. Drug substances with high molecular weight and/or water solubility can now be successfully delivered (1–5). Furthermore the rate of drug delivery can now almost be exclusively controlled by the delivery system as opposed to the stratum corneum (10,11). MN also have substantial benefits in that application is typically pain free and avoids bleeding (1–5). There is minimal microbial ingress into skin (11,26), meaning MN have never been associated with skin or systemic infection, avoidance of needle stick injuries and an ease of disposal for self-disabling polymeric MN. The benefits for patients and industry of MN-based products are, thus, very clear, with reduced vaccination risk in the developing world, controlled administration of a much greater range of drugs and extensive expansion of the transdermal drug delivery market the most immediately obvious.
Central to the future success of MN technology will be its correct use by patients, with reproducible insertion of MN into skin crucial. The recently-marketed Soluvia® and Micronjet® devices closely resemble a conventional hypodermic needle and syringe, the key differences being the much shorter shaft length for the single Soluvia® needle and the four needles for Micronjet®. Accordingly, such devices will be inserted into patients’ skin by skilled medical professionals in much the same way as a conventional needle, rather than by patients themselves. Therefore, the advantages of these systems are likely to be limited to enhanced reliability of intradermal vaccination, rather than facilitated at-home use by patients, which is where the major market driver is for MN-based delivery technologies. The MN devices that will have the greatest patient and commercial benefit are likely to be those that more closely resemble a traditional transdermal patch in terms of appearance and application/insertion than a traditional injection. The majority of MN insertion/penetration studies have to date been conducted using excised animal skin. Although this provides essential pre-clinical data, there are significant architectural and immunological differences between animal and human skin (27). Therefore, any micropores created in animal models are not completely accurate representations of human skin. More recent studies involving the use of ex vivo human skin have shown that, while it provides an anatomically relevant model for MN research, the excision of the skin from its natural environment results in considerable biomechanical changes to the tissue (28), with loss of skin tension and the support of underlying muscle and fat likely to be important. Recently, there has been an increase in the number of studies that have examined MN penetration in human volunteers (10,11,29), providing data that can be directly extrapolated to the clinical environment. However, the principal goal of such studies has been to evaluate the safety, sensation or drug delivery associated with MN insertion rather than the ability of human subjects to successfully insert the MN into their own skin (10,11,29,30). Indeed, it is notable that in all of these studies the research team have applied the MN to the volunteers, rather than the volunteers self-applying the MN. In an investigation of the opinion of both the public and healthcare professionals of MN technology (31), numerous points were raised about the advantages of self-administration; 88% of subjects agreed they would be happy to use MN on themselves, provided that there was clear instruction, and 84% of participants stated self-administration of MN was a significant benefit over hypodermic injection. As no studies have been conducted focusing on human subjects’ ability to successfully self-insert MN arrays into their own skin, it would seem prudent to tests this. Accordingly, this formed the basis of the present study.
Today, no medicinal product or medical device is provided without a PIL and it would be irresponsible of healthcare professionals, such as medical doctors and dispensing pharmacists, not to counsel their patients on a new medicine or device prescribed for them for the first time. Accordingly, a suitable PIL and pharmacist intervention strategy were designed and implemented here. These approaches were successful, in that application of 400 μm MN arrays comprised of 121 individual MN yielded comparable increases in TEWL values whether the arrays were self-applied by the novice Volunteers, the Researcher, who was relatively new to the field, or the Experienced Operator. Indeed, the Volunteers caused similar disruption to skin barrier function with their very first MN application as they did with their second, which also followed application to their skin by the Researcher. Since OCT studies indicated that increase in TEWL values was closely related to increasing depth of MN penetration into skin, it is likely that Volunteers inserted MN to reasonably similar depths to each other, the Researcher and the Experienced Operator following pharmacist counselling and having read the PIL.
In this study, we have shown for the first time that our hydrogel-forming MN arrays can be successfully and reproducibly applied by human volunteers given appropriate instruction. If these outcomes were extrapolated to the general patient population, then use of bespoke MN applicator devices, such as that employed for self-application in clinical trials of Zosano’s Macroflux® device (16), would not be necessary, thus possibly enhancing patient compliance. However, a number of factors must be considered in progression from here. The relatively small number of subjects participating in the present study were all final year Pharmacy students who, despite not having prior knowledge of the application of MN, are well-educated and have extensive clinical knowledge. The MN arrays used here had total patch areas of approximately 1.0 cm2. While patches this size are likely to be suitable for vaccination purposes, due to the small doses required, significantly larger patch sizes will be required for delivery of non-potent therapeutic agents. Finally, TEWL readings can be subject to inter-individual variation and can be affected by the anatomical region sampled, as well as ambient conditions. Accordingly, we are now moving forwards from this Pilot Study to carry out a much larger, fully-funded, investigation centred on members of the lay public and employing a variety of MN designs in terms of MN geometry and patch size, with OCT measurements being used to determine the penetration depth of every MN in each array. Since the volunteers here were concerned that patients would not know if they had applied sufficient pressure, we will be incorporating low-cost pressure-responsive feedback systems into a backing layer that will overly the MN patches. The outcomes of this new study will undoubtedly enhance industry and regulatory confidence in MN-based products, increasing investment and speeding translation to commercialisation and patient benefit.
References
Donnelly RF, Singh TRR, Morrow DIJ, Woolfson AD. Microneedle-mediated transdermal and intradermal drug delivery. Chichester: John Wiley & Sons, Ltd; 2012.
Kim YC, Park JH, Prausnitz MR. Microneedles for drug and vaccine delivery. Adv Drug Deliv Rev. 2012;64:1547–68.
Al-Zahrani S, Zaric, McCrudden MT, Scott C, Kissenpfennig A, Donnelly RF. Microneedle-mediated vaccine delivery: harnessing cutaneous immunobiology to improve efficacy. Expert Opin Drug Deliv. 2012;9:541–50.
Tuan-Mahmood TM, McCrudden MT, Torrisi BM, McAlister E, Garland MJ, Singh TR, Donnelly RF. Microneedles for intradermal and transdermal drug delivery. Eur J Pharm Sci. 2013 In Press.
Greystone Associates. Microneedles in medicine: technology, devices, markets and prospects. Amherst: Greystone Associates; 2012.
Donnelly RF, Morrow DIJ, Singh TRR, Migalska K, McCarron PA, O’Mahony C, et al. Processing difficulties and instability of carbohydrate microneedle arrays. Drug Dev Ind Pharm. 2009;35:1242–54.
Donnelly RF, Majithiya R, Singh TRR, Morrow DIJ, Garland MJ, Demir YK, et al. Design and physicochemical characterisation of optimised polymeric microneedle arrays prepared by a novel laser-based micromoulding technique. Pharm Res. 2011;28:41–57.
Migalska K, Morrow DIJ, Garland MJ, Thakur RRS, Woolfson AD, Donnelly RF. Laser-engineered dissolving microneedle arrays for transdermal macromolecular drug delivery. Pharm Res. 2011;28:1919–30.
Park JH, Allen MG, Prausnitz MR. Biodegradable polymer microneedles: fabrication, mechanics and transdermal drug delivery. J Control Release. 2005;104:51–66.
Donnelly RF, Singh TRR, Garland MJ, Migalska K, Majithiy R, McCrudden CM, et al. Hydrogel-forming microneedle arrays for enhanced transdermal drug delivery. Adv Funct Mater. 2012;22:4879–90.
Donnelly RF, Singh TR, Alkilani AZ, McCrudden MT, O’Neill S, O’Mahony C, et al. Hydrogel-forming microneedle arrays exhibit antimicrobial properties: potential for enhanced patient safety. Int J Pharm. 2013;451:76–91.
Donnelly RF, Garland MJ, Morrow DIJ, Migalska K, Thakur RRS, Majithiya R, et al. Optical coherence tomography is a valuable tool in the study of the effects of microneedle geometry on skin penetration characteristics and in-skin dissolution. J Control Release. 2010;147:333–41.
Olatunji O, Das DB, Garland MJ, Belaid L, Donnelly RF. Influence of array interspacing on the force required for successful microneedle skin penetration: theoretical and practical approaches. J Pharm Sci. 2013;102:1209–21.
Li WZ, Huo MR, Zhou JP, Zhou YQ, Hao BH, Liu T, et al. Super-short solid silicon microneedles for transdermal drug delivery applications. Int J Pharm. 2010;389:122–9.
Davis SP, Landis BJ, Adams ZH, Allen MG, Prausnitz MR. Insertion of microneedles into skin: measurement and prediction of insertion force and needle fracture force. J Biomech. 2004;37:1155–63.
Thakur RRS, Dunne NJ, Cunningham E, Donnelly RF. Review of patents on microneedle applicators. Recent Pat Drug Deliv Formul. 2011;5:11–23.
Thakur RRS, Woolfson AD, Donnelly RF. Investigation of solute permeation across poly(ethylene glycol)-crosslinked poly (methyl vinyl ether-co-maleic acid) hydrogels. J Pharm Pharmacol. 2010;62:829–37.
Thakur RRS, Garland MJ, Migalska K, Caffarel-Salvador E, Shaikh R, Woolfson AD, et al. Influence of a pore-forming agent on swelling, network parameters and permeability of poly (ethylene glycol)-crosslinked poly(methyl vinyl ether-co-maleic acid) hydrogels: application in transdermal delivery systems. J Appl Polym Sci. 2012;125:2680–94.
Medicines & Healthcare products Regulatory Agency (2013) Quality Criteria for PILs http://www.mhra.gov.uk/Howweregulate/Medicines/Labelspatientinformationleafletsandpackaging. Accessed 21st April 2013.
Giudice EL, Campbell JD. Needle-free vaccine delivery. Adv Drug Deliv Rev. 2006;58:68–89.
Kalluri H, Kolli CS, Banga AK. Characterization of microchannels created by metal microneedles: formation and closure. AAPS J. 2011;13:473–81.
Kalluri H, Banga AK. Formation and closure of microchannels in skin following microporation. Pharm Res. 2011;28:82–94.
Haq MI, Smith E, John DN, Kalavala M, Edwards C, Anstey A, et al. Clinical administration of microneedles: skin puncture, pain and sensation. Biomed Microdevices. 2009;11:35–47.
Gomaa YA, Morrow DIJ, Garland MJ, Donnelly RF, El-Khordagui LK, Meidan VM. Effects of microneedle length, density, insertion time and multiple applications on human skin barrier function: assessments by transepidermal water loss. Toxicol in Vitro. 2010;24:1971–8.
Abelson J, Forest P-G, Eyles J, Smith P, Martin E, Gauvin FP. Deliberations about deliberative methods: issues in the design and evaluation of public participation processes. Soc Sci Med. 2003;57:239–51.
Donnelly RF, Singh TRR, Tunney MM, Morrow DIJ, McCarro PA, O’Mahony C, et al. Microneedle arrays allow lower microbial penetration than hypodermic needles in vitro. Pharm Res. 2009;26:2513–22.
Godin B, Touitou E. Transdermal skin delivery: predictions for humans from in vivo, ex vivo and animal models. Adv Drug Deliv Rev. 2007;59:1152–61.
Ng KW, Pearton M, Coulman S, Anstey A, Gateley C, Morrissey A, et al. Development of an ex vivo human skin model for intradermal vaccination: tissue viability and Langerhans cell behaviour. Vaccine. 2009;27:5948–55.
Gill HS, Denson DD, Burris BA, Prausnitz MR. Effect of microneedle design on pain in human volunteers. Clin J Pain. 2008;24:585–94.
Bal SM, Caussin J, Pavel S, Bouwstra JA. In vivo assessment of safety of microneedle arrays in human skin. Eur J Pharm Sci. 2008;35:193–202.
Birchall JC, Clemo R, Anstey A, John DN. Microneedles in clinical practice-an exploratory study into the opinions of healthcare professionals and the public. Pharm Res. 2011;28:95–106.
Acknowledgments and Disclosures
This work was supported by the Biotechnology and Biological Sciences Research Council (BB/K020234/1), the Engineering and Physical Sciences Research Council (EP/H021647/1) and the Wellcome Trust (WT094085MA). The authors report no conflict of interests, financial or otherwise.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donnelly, R.F., Moffatt, K., Alkilani, A.Z. et al. Hydrogel-Forming Microneedle Arrays Can Be Effectively Inserted in Skin by Self-Application: A Pilot Study Centred on Pharmacist Intervention and a Patient Information Leaflet. Pharm Res 31, 1989–1999 (2014). https://doi.org/10.1007/s11095-014-1301-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1301-y