ABSTRACT
Purpose
Dosing of the anticoagulant enoxaparin may result in bleeding following excessive doses or thrombosis if dose is too low. Rarely, anti-Xa activity is used to assess the dose for enoxaparin, but its utility to predict clotting or bleeding remains uncertain. We aimed to develop a clotting time test to monitor enoxaparin therapy.
Methods
A previously developed mathematical model of the coagulation network was used to identify suitable targets for monitoring enoxaparin therapy. In vitro experiments were then carried out to demonstrate proof of mechanism of the clotting time test activated by the new target activator.
Results
Using the mathematical model, we identified Xa as a plausible activating agent for a clotting time test for enoxaparin. In vitro experiments showed a prolongation of the Xa clotting time of 4.6-fold in the presence of enoxaparin (0.5 IU/ml) where 10 nM Xa was used to activate clotting.
Conclusions
Using both simulations and in vitro experiments, we provide a proof of mechanism for the Xa clotting time (XaCT) test, which can be considered for further development to provide a biomarker of the effect of enoxaparin on the clotting system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Thrombosis is the pathological activation of the haemostatic system within the vasculature and results in formation of a solid mass of platelets, fibrin and trapped blood cells inside blood vessels. Inappropriate activation of the coagulation process or inappropriate formation of platelet aggregates in blood vessels is treated with anticoagulants or, in a few situations, with medicines that activate fibrinolysis. Careful control of the action of therapeutic anticoagulants is required to prevent the adverse effects of bleeding from excessive anticoagulation or thrombosis and thromboembolism where anticoagulation is inadequate (1).
Enoxaparin is a low molecular weight heparin (LMWH) anticoagulant that is widely used to minimise the risk for thrombosis in patients with acute coronary syndromes, pulmonary embolism or deep vein thrombosis (2–5). Its activity is mediated by increasing the activity of a physiological inhibitor, antithrombin (AT). The outcome is enhanced inactivation of Xa and several other activated factors, resulting in inhibition of the coagulation network (6). Despite claims that LMWHs have more predictable dosing requirements than unfractionated heparins, the rates of bleeding and thrombus formation are similar (7–9). Sequelae from bleeding or thrombosis arising as adverse effects from inadequately controlled anticoagulation may be severe and in some cases life threatening.
In contrast to the older anticoagulants, unfractionated heparin (UFH) and warfarin, there is no currently accepted method for monitoring the effect of enoxaparin on coagulation. The need to monitor has been the subject of debate, with some studies suggesting that LMWHs are no safer than UFH and require monitoring (10). This begs the question, could safety and efficacy be improved with appropriate laboratory monitoring of LMWH, either universally or in selected patients? For warfarin and UFH, it is usual to measure the time for a blood sample to clot after stimulation with activating agent(s). The tests used are the standardised prothrombin time (PT), i.e., the international normalised ratio (INR) for warfarin (11) and the activated partial thromboplastin time (aPTT) for UFH (12). Both the PT and the aPTT assess multiple steps in the clotting system and measure the time to form a fibrin clot. These tests identify deficiencies in any of the clotting factors or pathways that may arise and affect the final clot formation. Both PT and aPTT have been found to provide a good prediction of the risk for bleeding, or clotting and thrombosis, when used with warfarin and UFH, respectively.
Currently, there is no multi-step clotting time test for LMWHs such as enoxaparin, and assessment of dose effect is seldom performed. It is possible to measure anti-Xa activity (one of the critical activated precursors for coagulation), but there is no well-accepted target activity value, and dose adjustments are difficult to make (5,13). Neither the PT/INR nor aPTT produce significant dose-response changes with enoxaparin and so do not provide meaningful evaluation of bleeding or thrombotic risks (5,6,12–15). Measurement of anti-Xa activity assesses the activation of only a single component of the clotting system and is not a widely available test. We consider there is a need for an alternative, simple, stable, diagnostic clotting time-based test to monitor treatment with enoxaparin.
There have been various attempts at developing tests to monitor LMWH therapy. The activated clotting time (ACT) is a less sensitive global test of coagulation and is used to monitor the level of anticoagulation in patients undergoing percutaneous coronary interventions or aorto-cardiac bypass surgery who receive bolus doses of UFH (16). Four studies have shown that the ACT is sensitive to LMWH and may be of value in monitoring patients, particularly in relation to percutaneous coronary angioplasty (17–20). Other studies have shown little or no effect of LMWH on the ACT (21–24). A study involving UFH, enoxaparin and fondaparinux, a synthetic penta-saccharide Xa inhibitor, and their effects on the ACT and aPTT in healthy volunteers found that enoxaparin produced significantly less prolongation of both the ACT and the aPTT than UFH, whereas fondaparinux had no effect on either of these tests (23). Finally, the addition of enoxaparin or fondaparinux to blood containing UFH produced no significant prolongation of the ACT beyond that produced by UFH alone. It was concluded that the ACT and aPTT cannot be used to monitor enoxaparin or fondaparinux (23).
Other clotting tests such as the HepTest and prothrombinase-induced clotting time test were designed as surrogate measures of plasma heparin concentrations and employ excess Xa (25,26). However, they are not specific for measuring heparin effect because the addition of hirudin (which produces an anti-IIa (anti-thrombin) effect) will prolong the clotting time (27). In some clinical conditions, the changes in the concentration of specific markers of blood clotting activation during LMWH administration have been investigated, but assays of prothrombin fragment F1 + 2, thrombin-antithrombin complexes, and D-dimers have not been found to be sufficiently sensitive and useful in the assessment of antithrombotic efficacy of the anticoagulant therapy (28).
A mechanistic and quantitative model of the coagulation network has been developed (Fig. 1). The model has been shown to accurately describe the time course for activation of coagulation factors both in vivo and also in vitro in PT and aPTT tests. The model has also been used to predict the concentration-time and effect-time profiles of warfarin, heparins and vitamin K in humans (29), as well as venom-induced consumptive coagulopathy arising from some snake bites (30).
Schematic of the coagulation network model. The bold solid lines represent activation process, complex formation, reduction or oxidization; the broken lines represent stimulation of reaction or production; the dot-bar lines represent stimulation of degradation; the solid lines represent inhibition of reduction. APC, activated protein C; AT, antithrombin; CA, activator for the contact system; DP, degradation product; F, fibrin; Fg, fibrinogen; II, prothrombin; IIa, thrombin; K, kallikrein; LMWH, low molecular weight heparin; P, plasmin; PC, protein C; Pg, plasminogen; Pk, prekallikrein; PS, protein S; TF, tissue factor; TFPI, tissue factor pathway inhibitor; Tmod, thrombomodulin; VK, vitamin K; VKH2, vitamin K hydroquinone; VKO, vitamin K epoxide; XF, cross-linked fibrin. (Adapted from Wajima et al. (29)—the one error has been removed, modifications have been made to clarify details, and new subsystems have been added).
The overarching aim of this study was to identify and evaluate plausible activating agent(s) for a clotting time test to assess the anticoagulant effect of enoxaparin. Four specific objectives were identified: 1) in silico assessment of standard clotting time tests (aPTT and PT/INR) when applied to enoxaparin, 2) in silico identification of new targets for activating a clotting time test, 3) in vitro assessment of Xa as a new target for activating a clotting time test, and 4) in silico predictions of the kinetics of activation in the test. These specific objectives were designed to provide a proof-of-mechanism of the clotting time test and to assess whether the test appears to work by a mechanism that we understand and predict. The in silico experiments in the study provide the mechanistic framework, and the in vitro experiments show a realisation of the mechanism. This study was aimed at exploring a mechanism, and future work will assess the utility of any test identified in this work along the lines of a proof-of-concept.
MATERIALS AND METHODS
In Silico Assessment of Activation of Standard Clotting Time Tests When Applied to Enoxaparin
A mathematical model of the coagulation system (Fig. 1) published earlier (29) was used to assess current clotting time tests. Simulations using the model were carried out to address why warfarin but not enoxaparin prolongs PT and also why UFH but not enoxaparin prolongs aPTT. All simulations were performed in MATLAB® version 7.10.0 (R2010a), a product of the MathWorksTM Inc. (Natick, USA). Clotting time was defined as the time it takes for a fibrin clot to start to form in plasma after addition of an activating agent to a plasma sample. The criterion for formation of a clot using the mathematical model was based on the integral of fibrin, which determines the area under the fibrin concentration-time curve (fibrin AUC). Using this measure the criterion for clot formation was a fibrin AUC of 1500 nM.sec (29). This is approximately equivalent to a 30% consumption of fibrinogen in a standard PT/INR test (31).
The PT is the time for plasma to clot after addition of a thromboplastin reagent (tissue factor, calcium and phospholipid). The in silico PT test was performed by simulating the clotting time after adding tissue factor (TF) to a plasma sample with the initial TF concentration of 300 nM, which is in excess of VII (10 nM). The TF concentration of 300 nM in the model was chosen arbitrarily and was based on a calibration to a clinically observed PT of 12-15 s in the absence of any anticoagulant. The value used here should not be construed to be necessarily representative of TF concentrations used in actual PT tests. The influences of various lower concentrations of TF were also investigated. The effect of enoxaparin was simulated at a therapeutic concentration of enoxaparin (taken as 0.5 IU/ml of anti-Xa activity). Time courses of X and Xa in the absence as well as presence of enoxaparin (0.5 IU/ml) were also simulated using the model.
The aPTT is the time for plasma to clot after the addition of calcium following pre-incubation with phospholipid and an activator for the contact system (e.g., kaolin). The in silico aPTT test was performed by setting the initial XIa and XI concentrations to \( 0.148*{\text{XI}}(0) \) and \( 0.339*{\text{XI}}(0) \), respectively, where XI(0) is the concentration of XI in a plasma sample (29). The influences of various initial conditions for the aPTT test were also investigated. Finally, the effect of enoxaparin was simulated in a similar way to the in silico PT test.
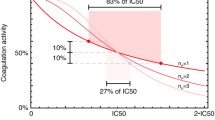
In Silico Identification of New Targets for Activating a Clotting Time Test
The mathematical model was used to identify new targets for monitoring enoxaparin therapy. To identify an activating agent for a clotting time test with enoxaparin, the in silico clotting system was activated using a range of activated clotting factors or complexes, including IIa, Va, VIIa, TF, VII-TF, VIIa-TF, VIIIa, IXa, IXaVIIIa, Xa, XaVa, XIa, XIIa, over a range of concentrations, individually and in combination with each other. The simulations assumed that calcium and phospholipid were available in excess. The aim of the simulations was to identify an activating agent, in the form of a clotting factor that
-
provides a reasonable clotting time (<60 s) and
-
is prolonged by at least two-fold to a reasonable clotting time (<60 s) in the presence of a therapeutic concentration of enoxaparin (0.5 IU/ml).
This would result in clotting times similar to those observed in a PT test.
In Vitro Assessment of Xa as a New Target for Activating a Clotting Time Test
Xa was identified in silico (method 2) as the best option as an activating agent for a clotting time test to detect enoxaparin effect. Plasma from a single donor was used for the in vitro experiments and was prepared by double centrifugation at 2000 g for 20 min at 20°C to ensure the sample was platelet-free. Xa (100 μL, 0.005-10 nM) was mixed in equal proportion with calcium chloride (100 μL of 25 mM) and kept in a heating block maintained at 37°C for 2–3 min. Plasma (100 μL), pre-warmed at 37°C, was then added to the mixture and the clotting time determined using a digital timer and visual inspection to identify the appearance of fibrin (apparent as a sudden increase in turbidity) (32). The effect of enoxaparin was determined by adding a 1:10 ratio of enoxaparin to plasma at concentrations of 0.1-1.0 IU/ml anti-Xa activity; controls (0 IU/ml activity) had a similar volume of saline buffer added. Clotting times were measured in three different sets of experiments: (I) where the concentration of Xa was varied in the absence of enoxaparin, (II) where the concentration of Xa was varied in the presence of a therapeutic concentration of enoxaparin (0.5 IU/ml), and (III) where the concentration of enoxaparin was varied in the presence of a specific Xa concentration. Each set of conditions was assessed in triplicate and the mean ± standard deviation determined.
In Silico Predictions of the Kinetics of Activation in the Test
After evaluating various activating agents and choosing Xa as a possible biomarker for enoxaparin activity, it was critical to modify the coagulation network model, as this study aimed to evaluate the influence of AT-Xa-enoxaparin relationship. Due to the behaviour of specific components of the model being tested, further equations were added to the model to account for the influence of variable AT concentrations. The original model (29) of the coagulation network, however, was built with different aims in mind, and at that time it was not necessary to include these equations. The simulated clotting times obtained using the modified mathematical model of the clotting network with Xa as the activating agent were compared to the clotting times obtained with the in vitro experiments. Equation (1) describes the concentration of Xa bound with AT in the absence or presence of enoxaparin:
The parameter \( {B_{\max }}(t) \) describes the maximum binding possible between Xa and AT and was assumed to be time-varying and equal to the concentration of AT in plasma, mean [AT] = 2.57 μM (33). The parameter \( {K_{{D_{Xa}}}} \) describes the affinity of AT for Xa in the absence of enoxaparin. Because enoxaparin produces its major anticoagulant effect by increasing the activity of AT against Xa (13), a coefficient that describes the increase in the affinity of AT for Xa in the presence of enoxaparin was included in equation (1). The coefficient, \( {f_{{K_D}}} \), was described by equation (2) below:
The parameter \( {K_{{D_E}}} \) in equation (2) describes the overall affinity of enoxaparin for AT. The model was then used to predict the clotting times for the three sets of in vitro experiments to provide a comparison of in silico predictions with in vitro observations. The in silico predictions were carried out at a range of values for the parameters \( {K_{{D_{Xa}}}} \) and \( {K_{{D_E}}} \). The final values set in the model were based on the similarity of model predictions to the results from the in vitro experiments.
RESULTS
In Silico Assessment of Activation of Standard Clotting Time Tests When Applied to Enoxaparin
PT Test
The in silico PT test was performed by simulating the clotting time after adding 300 nM of TF to a plasma sample. At this concentration of TF, a clotting time of 11.8 s was observed which was prolonged to 13.6 s in the presence of 0.5 IU/ml enoxaparin. Simulations of the time course of Xa in the PT test suggested that at a TF concentration of 300 nM and in the absence of enoxaparin, the concentration of Xa present at the time the clot formed (11.8 s) was 0.98 nM (Fig. 2a). In the presence of 0.5 IU/ml enoxaparin, the concentration of Xa present after 11.8 s was 0.37 nM. Although enoxaparin reduced the Xa concentration by 60% at this time, sufficient unbound Xa remained to continue activation of coagulation. This simulation suggests that the concentration of TF used to activate the system is sufficiently high that it results in excess concentrations of Xa that overcome the enoxaparin concentration of 0.5 IU/ml, and hence therapeutic enoxaparin causes only a very slight (15%) prolongation in PT to 13.6 s.
Simulated time course of Xa in the PT test. (a) Time course of Xa in the PT test when activated by 300 nM of TF in silico in the absence (solid line) or presence (dash-dotted line) of 0.5 IU/ml enoxaparin. (b) Time course of Xa in the PT test when activated by 0.003 nM of TF in silico in the absence (solid line) or presence (dash-dotted line) of 0.5 IU/ml enoxaparin.
In contrast, changing the TF concentration by a factor of 100,000 to 0.003 nM predicted a clotting time of 2.6 min which was prolonged to 5.9 min in the presence of 0.5 IU/ml enoxaparin. Simulations of the time course of Xa production, at the TF concentration of 0.003 nM and in the absence of enoxaparin, predicted a concentration of Xa of 1.3 pM at the time the clot formed (2.6 min), which was around 700-fold lower than that formed with 300 nM TF (Fig. 2b). In the presence of 0.5 IU/ml enoxaparin, the concentration of Xa present after 2.6 min was 96% lower (0.05 pM) and resulted in a 2.3-fold prolongation of PT to 5.9 min.
In vitro experiments were carried out at a TF concentration of 1.5 nM, and clotting times greater than 10 min were obtained. Investigation of the effects of the addition of phospholipids appeared to be influential, and further experiments with TF were not continued. Please note that the actual concentration of TF is not able to be determined in these experiments, but rather all predictions are based on the relative concentration (relative to 300 nM).
aPTT Test
The in silico aPTT test was performed by setting the initial XIa and XI concentrations to \( 0.148*{\text{XI}}(0) \) and \( 0.339*{\text{XI}}(0) \), respectively, where XI(0) is the concentration of XI in the plasma sample (29). At an XIa concentration of 1.5 nM, a clotting time of 34.4 s was observed, which was prolonged to 49.3 s in the presence of 0.5 IU/ml enoxaparin. Simulations of the time course of Xa in the aPTT test suggested that at an XIa concentration of 1.5 nM in the absence of enoxaparin, the concentration of Xa at the time the clot formed (34.4 s) was 0.06 nM (Fig. 3a). In the presence of 0.5 IU/ml enoxaparin, the concentration of Xa present after 34.4 s was 85% lower (0.0093 nM) and was associated with clot formation at 49.3 s. As with the PT test, the activation condition (concentration of XIa in the case of the aPTT) resulted in concentrations of Xa that largely overcame the enoxaparin concentration of 0.5 IU/ml.
Simulated time course of Xa in the aPTT test. (a) Time course of Xa in the aPTT test when activated by 1.5 nM of XIa in silico in the absence (solid line) or presence (dash-dotted line) of 0.5 IU/ml enoxaparin. (b) Time course of Xa in the aPTT test when activated by 0.015 nM of XIa in silico in the absence (solid line) or presence (dash-dotted line) of 0.5 IU/ml enoxaparin.
In contrast, at a 100-fold lower XIa concentration of 0.015 nM, a clotting time of 77 s was observed, which was prolonged to 167 s in the presence of 0.5 IU/ml enoxaparin. Simulations of the time course of Xa production at this lower XIa concentration of 0.015 nM and in the absence of enoxaparin predicted that the Xa concentration present at the time the clot formed (77 s) was 0.0063 nM, which was 10-fold lower compared to that formed with 1.5 nM of XIa (Fig. 3b). In the presence of 0.5 IU/ml enoxaparin, the concentration of Xa present after 77 s was 0.0004 nM (94% lower), which resulted in a 2.2-fold prolongation of aPTT to 167 s.
In Silico Identification of New Targets for Activating a Clotting Time Test
Simulations using the mathematical model of the coagulation system identified Xa as a plausible activating agent for a clotting time test to measure the dose effect of enoxaparin (see Table I). A Xa concentration of 0.05 nM gave a clotting time of 13.8 s, which was prolonged 2-fold to 27.2 s in the presence of 0.5 IU/ml enoxaparin. Activation with Va, VIIa, VII-TF or VIIIa did not result in the formation of a clot, whereas activation with XIIa did not result in a two-fold prolongation in the presence of 0.5 IU/mL enoxaparin. Clotting times on activation with a combination of clotting factors were similar to those with individual factors; individual factors were therefore preferred over combination of factors.
In Vitro Assessment of Xa as a New Target for Activating a Clotting Time Test
Xa was assessed in vitro as a plausible activating agent for a clotting time test to measure enoxaparin effect (Xa clotting time (XaCT) test).
Effect of Varying Xa Concentrations on Clotting times in the Absence of Enoxaparin
Concentrations of Xa from 0.005 to 10 nM produced clotting times that ranged from 473 ± 11 to 15.3 ± 0.6 s respectively (Fig. 4).
Effect of varying Xa concentrations on clotting times in the absence or presence of 0.5 IU/ml enoxaparin: In vitro clotting times (seconds) after activation by varying Xa concentrations (0.005 to 10 nM) in the absence (‘○’) or presence (‘●’) of 0.5 IU/ml enoxaparin using plasma from a single donor. Data are shown as error bars of mean values of triplicate measurements ±3SD. In silico clotting times (seconds) after activation by varying Xa concentrations (0.05 pM to 0.1 nM) in the absence (‘∆’) or presence (‘▲’) of 0.5 IU/ml enoxaparin. Clotting time for a Xa concentration of 0.05 pM could not be obtained due to the insensitivity of the model for very low Xa concentrations.
Effect of Varying Xa Concentrations on Clotting times in the Presence of 0.5 IU/ml Enoxaparin
Using Xa at concentrations of 0.005 to 10 nM with 0.5 IU/ml enoxaparin, produced clotting times that ranged from 2148 ± 49 to 70 ± 5 s. This ranged from 4.5- to 6.8-fold lengthening of the clotting time (Fig. 4).
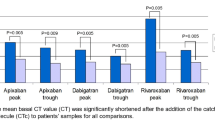
Effect of Varying Enoxaparin Concentrations on Clotting Times in the Presence of a Specific Xa Concentration
A clotting time of 15 s, similar to the upper end of the physiological range for the PT, was obtained with a Xa concentration of 10 nM, and this concentration was used to activate the clotting system to assess the effect of varying enoxaparin concentrations (0.1-1.0 IU/ml). In the presence of 1.0 IU/ml enoxaparin, the clotting time was prolonged 10-fold to 153 s; in contrast, 0.1 IU/ml enoxaparin caused only a 1.7-fold prolongation to 26 s, compared to the control with no enoxaparin (see Table II).
In Silico Predictions of the Kinetics of Activation in the Test
After the modification of the mathematical model to include the binding of Xa and AT, as described in equation (1), the model was used to predict the clotting times for the three sets of in vitro experiments to provide a comparison of in silico to in vitro observations. Based on the similarity of model predictions to the results obtained in the in vitro experiments, the parameters \( {K_{{D_{Xa}}}} \) and \( {K_{{D_E}}} \) were set to 0.56 nM and 16.5 nM, respectively. In addition, since the in silico system assumes phospholipids and calcium are always in excess, it was found necessary to adjust to a standard concentration of exogenous Xa. The purpose of this in silico evaluation was to assess whether the mathematical model supports the findings from the experimental observations on clotting in the presence of varying concentrations of Xa and enoxaparin, i.e., in the in vitro testing that were undertaken as a proof-of-mechanism study in method 3 for the “XaCT test.”
Effect of Varying Xa Concentrations on Clotting times in the Absence of Enoxaparin
When the in silico clotting system was activated using 0.05 pM to 0.1 nM Xa, a concentration-dependent decrease in simulated clotting times from 3255 s to 15 s was observed (Fig. 4). Similar trends between the in vitro and in silico experiments were seen, although the in silico predictions diverged at lower Xa concentrations. The in silico Xa activating concentration in Fig. 4 was adjusted by a factor of 100 for comparison with the in vitro experiments.
Effect of Varying Xa Concentrations on Clotting times in the Presence of 0.5 IU/ml Enoxaparin
Clotting times ranged from 37 h to 70 s in the presence of 0.25 pM to 0.1 nM Xa, giving a 4.6- to 193-fold prolongation in silico, compared to their respective controls (Fig. 4), in the presence of 0.5 IU/ml enoxaparin. Clotting time for a Xa concentration of 0.05 pM could not be obtained due to the insensitivity of the model for very low Xa concentrations. Similar to experiment (I), the in silico results showed an agreement at 0.1 nM but diverged at lower concentrations of Xa. The model over-predicted the influence of enoxaparin at declining concentrations of Xa.
Effect of Varying Enoxaparin Concentrations on Clotting Times in the Presence of a Specific Xa Concentration
A Xa concentration of 0.1 nM was chosen to activate the system in silico, as this concentration gave the same clotting time of 15 s, as was observed with the in vitro results. Presence of 0.1 to 1 IU/ml of enoxaparin in silico resulted in a prolongation of clotting time from 26 s to 145 s, i.e. 1.7- to 9.5-fold (see Table II). The model and in vitro results agree closely.
DISCUSSION
Using both simulations from an in silico model and in vitro experiments, we show that a Xa clotting time test has the potential to be used to assess the effect of enoxaparin on the clotting system. The in silico simulations showed that only clotting tests activated by low concentrations of Xa were sensitive to the effects of enoxaparin and produced clotting times which are likely to be manageable in the clinic. We then used in vitro experiments to demonstrate proof-of-mechanism of the Xa clotting time test and compared clotting times from these experiments to in silico simulated clotting times. These provide the basis for the Xa clotting time test being useful for monitoring enoxaparin.
Our in silico model of the coagulation system was initially used to investigate the reason for enoxaparin not having a significant prolonging effect on the common clotting time tests, PT and aPTT. The in silico PT and aPTT experiments suggested that the extent of PT or aPTT prolongation in the presence of enoxaparin depends on the concentration of the activating agent used in the test (TF for the PT and XIa for the aPTT). Routine PT tests use much higher concentrations of thromboplastin than might be expected under physiological conditions (34) and achieve high concentrations of Xa that overcome the effect of enoxaparin. The simulations suggested that at lower TF concentration, an appreciable prolongation in PT is observed with a therapeutic concentration of enoxaparin (0.5 IU/ml) because there is a much larger reduction in Xa concentrations. Similarly, the use of a lower concentration of XIa in the in silico aPTT test caused an appreciable prolongation in aPTT in the presence of enoxaparin. This is because a higher concentration of the activating agent used to activate the system results in excess concentrations of Xa that overcome therapeutic enoxaparin concentrations of 0.5 IU/ml. Hence, therapeutic enoxaparin causes only a small prolongation in currently manufactured versions of the PT and aPTT. The use of lower TF concentrations in a PT test would result in therapeutic concentrations of enoxaparin to cause an appreciable prolongation in the PT that would provide a diagnostically useful quantitation. Similarly, the use of lower concentrations of the activator (silica or kaolin) in the aPTT test reagents would also result in an appreciable prolongation in aPTT by therapeutic enoxaparin (data not shown). However, these activating agents would result in longer clotting times in the order of minutes and so limit the clinical usefulness of a modified aPTT or PT to evaluate enoxaparin effect.
We believe our findings could be applied to other anticoagulants as well. Samama et al. used commercially available PT and aPTT kits and showed that fondaparinux did not prolong PT and aPTT (27). The authors related the response of the drug on this system to its mechanism of action by stating that fondaparinux inhibits Xa activity by acting on free Xa instead of the prothrombinase complex and is thus less efficient at inhibiting the activation of prothrombin to thrombin. We suggest that the reason for fondaparinux not prolonging the PT and aPTT to an appreciable extent was due to the high concentration of TF or silica/kaolin, respectively, present in the PT or aPTT kits used in the study.
Commercially available PT test kits contain a mixture of agents including TF, phospholipids and calcium. Because a PT test is primarily used to monitor warfarin therapy, the PT test kits also include a heparin neutralizer to minimise effects on the PT from any heparins in the patient plasma samples. For example, Innovin® (recombinant human TF) and Thromborel® S (human placental thromboplastin), products of Dade Behring, Liederbach, Germany are insensitive to heparin concentration up to approximately 2 IU/ml and 0.6 IU/ml, respectively (http://www.medcorp.com.br/medcorp/upload/downloads/Innovin_Thromborel_PT_2006317143540.pdf). Therefore, besides a high concentration of TF used in PT test reagents, a further reason that LMWHs do not produce appreciable prolongation with currently available PT test kits is the addition of heparin neutralizers.
Clotting times of the order of a few seconds permit efficient use of diagnostic laboratory facilities when testing large batches of patient samples and are a driver for the high concentrations of activators used in PT and aPTT test kits. Our study shows that using Xa as an activating agent for a test with enoxaparin results in a clotting time in the order of seconds, and this is prolonged with increasing amounts of enoxaparin. A Xa concentration of 10 nM gave a physiological clotting time of 15 s when used as an activating agent in the in vitro experiments involving plasma from a single healthy volunteer. An appreciable prolongation of this clotting time to 26 s was observed in the presence of 0.1 IU/ml of enoxaparin compared to 153 s when 1.0 IU/ml of enoxaparin was present. The clotting time prolongation of 1.7- to 10-fold in the presence of 0.1-1.0 IU/ml of enoxaparin now needs to be assessed for consistency of performance with normal and patient plasma samples and ultimately for overall clinical utility.
Current tests for enoxaparin (and fondaparinux) dose effect involve assessment of anti-Xa activities and may be poor measures of patient outcomes (5,13). We suggest that a new test, which we have called the XaCT test, which uses Xa to activate plasma clotting, will ultimately provide an effective and simple means for assessing enoxaparin concentration in plasma and provide greater certainty around clinical treatment where this is appropriate.
We have provided a proof-of-mechanism study which has shown that our mathematical model of the coagulation system can be used to predict targets for blood coagulation tests and the general behaviour of these targets when used in an in vitro clotting time test. There was good agreement between the in silico and in vitro results for parts I and III of the fourth experiment after scaling for Xa concentration. Although scaling of Xa concentrations between in silico and in vitro was an important issue, we believe the main results are represented in the time course and concentration-response of activity rather than the specific factor concentrations. The clotting network model does not account for calcium and phospholipids, which are assumed to be in excess during all in silico versions of both in vivo and in vitro simulations. Hence, we would expect the in silico model should provide the lower bound of the likely in vitro concentrations. We also note that the model over-predicted the clotting time due to activation by variable concentrations of Xa under conditions of fixed enoxaparin concentration, while providing accurate predictions of the effect of variable enoxaparin-induced clotting time prolongation for a fixed Xa concentration. Again, we believe this discrepancy for variable Xa concentrations may in part arise from assumptions about phospholipids and calcium, which becomes more evident for longer clotting time values when the concentrations of Xa are low and hence the system is more sensitive to phospholipid and calcium concentrations.
We also believe that the choice of the criteria for clot formation may not be reflective of slow-forming clots. In the in silico experiments, a fibrin AUC of 1500 nM.sec was used as a criterion for clot formation. Formation of a clot, however, is likely to be much more complex than this criterion suggests, since a very slow production of fibrin to achieve the same AUC may result in clot formation at a different critical value. Therefore, this critical value of the fibrin AUC to cause clot formation only relates to rapid formation of fibrin and we do not know how time will affect interpretation of this value. We believe this may have affected the model predictions at lower Xa concentrations when clotting times were in the order of minutes. In addition, the model neither accounts for binding of AT with clotting factors other than Xa nor for non-specific binding of Xa that may be involved. The value of 100 as a scaling factor was therefore chosen empirically so that the in vitro predictions at 10 nM match with the in silico predictions obtained at 0.1 nM. In all cases, we expect the model to predict the lower bound of any concentration range for activation of the system, since the model does not include non-specific binding nor does it account for a lack of phospholipids, both of which may occur in in vitro experiments. Also, the current coagulation network model was based on literature parameter values (29), and it is likely that some of these values may need to be modelled to get estimates that better reflect observed data. Despite these discrepancies, the model provided acceptable estimates of clotting times for the clinically important outcomes presented in Table II.
Xa is used extensively all over the world for anti-Xa measurements to get enoxaparin concentrations. The concentrations of Xa used in our study are similar to those in standard anti-Xa kits, and we do not perceive an issue with using Xa as an activating agent for clot formation. Therefore, the next stage of the development of the prototype “XaCT Test” will be a proof-of-concept study that aims to explore the clinical utility of the test. Validation studies will use plasma from a wide range of healthy volunteers to evaluate the reproducibility of the test. A successful proof-of-concept study would mean that this XaCT test could then be evaluated in patients receiving therapeutic LMWH to assess the amount of variance in anticoagulation achieved and the potential for reduced risk of thrombotic and bleeding events where control is optimised. We suggest that the XaCT test will provide a missing direct link for dose optimisation of drugs like LMWHs and fondaparinux. However, we would point out that there are other factors that need to be considered as well, which would not necessarily benefit from multiple subjects such as non-specific binding and assumption in the model that a clot forms at 1500 nM.sec for all values of time.
Abbreviations
- ACT:
-
activated clotting time
- aPTT:
-
activated partial thromboplastin time
- AT:
-
antithrombin
- INR:
-
international normalised ratio
- LMWH:
-
low-molecular-weight heparin
- PT:
-
prothrombin time
- TF:
-
tissue factor
- UFH:
-
unfractionated heparin
- XaCT:
-
Xa clotting time
REFERENCES
Eastham RD, Slade RR. Bleeding, clotting and transfusion. Oxford: Clinical Haematology, Butterworth Heinemann; 1992.
Antman EM, McCabe CH, Gurfinkel EP, Turpie AG, Bernink PJ, Salein D, et al. Enoxaparin prevents death and cardiac ischemic events in unstable angina/non-Q-wave myocardial infarction. Results of the thrombolysis in myocardial infarction (TIMI) 11B trial. Circulation. 1999;100:1593–601.
Cohen M, Demers C, Gurfinkel EP, Turpie AG, Fromell GJ, Goodman S, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease. Efficacy and safety of subcutaneous enoxaparin in non-Q-wave coronary events study group. N Engl J Med. 1997;337:447–52.
Eriksson BI, Kalebo P, Anthymyr BA, Wadenvik H, Tengborn L, Risberg B. Prevention of deep-vein thrombosis and pulmonary embolism after total hip replacement. Comparison of low-molecular-weight heparin and unfractionated heparin. J Bone Joint Surg Am. 1991;73:484–93.
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, et al. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest. 2001;119:64S–94S.
Hirsh J, Levine MN. Low molecular weight heparin. Blood. 1992;79:1–17.
Jorgensen LN, Wille-Jorgensen P, Hauch O. Prophylaxis of postoperative thromboembolism with low molecular weight heparins. Br J Surg. 1993;80:689–704.
Leizorovicz A, Haugh MC, Chapuis FR, Samama MM, Boissel JP. Low molecular weight heparin in prevention of perioperative thrombosis. BMJ. 1992;305:913–20.
Nurmohamed MT, Rosendaal FR, Buller HR, Dekker E, Hommes DW, Vandenbroucke JP, et al. Low-molecular-weight heparin versus standard heparin in general and orthopaedic surgery: a meta-analysis. Lancet. 1992;340:152–6.
Al-Sallami HS, Barras MA, Green B, Duffull SB. Routine plasma anti-Xa monitoring is required for low-molecular-weight heparins. Clin Pharmacokinet. 2010;49:567–71.
Hirsh J, Dalen JE, Deykin D, Poller L. Oral anticoagulants. Mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 1992;102:312S–26S.
Hirsh J, Dalen JE, Deykin D, Poller L. Heparin: mechanism of action, pharmacokinetics, dosing considerations, monitoring, efficacy, and safety. Chest. 1992;102:337S–51S.
Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:188S–203S.
Boneu B. Low molecular weight heparin therapy: is monitoring needed? Thromb Haemost. 1994;72:330–4.
Hirsh J. Heparin. N Engl J Med. 1991;324:1565–74.
Dougherty KG, Gaos CM, Bush HS, Leachman DR, Ferguson JJ. Activated clotting times and activated partial thromboplastin times in patients undergoing coronary angioplasty who receive bolus doses of heparin. Cathet Cardiovasc Diagn. 1992;26:260–3.
Frank RD, Brandenburg VM, Lanzmich R, Floege J. Factor Xa-activated whole blood clotting time (Xa-ACT) for bedside monitoring of dalteparin anticoagulation during haemodialysis. Nephrol Dial Transplant. 2004;19:1552–8.
Lawrence M, Mixon TA, Cross D, Gantt DS, Dehmer GJ. Assessment of anticoagulation using activated clotting times in patients receiving intravenous enoxaparin during percutaneous coronary intervention. Catheter Cardiovasc Interv. 2004;61:52–5.
Marmur JD, Anand SX, Bagga RS, Fareed J, Pan CM, Sharma SK, et al. The activated clotting time can be used to monitor the low molecular weight heparin dalteparin after intravenous administration. J Am Coll Cardiol. 2003;41:394–402.
Wilson JM, Gilbert J, Harlan M, Bracey A, Allison P, Schooley C, et al. High-dose intravenous dalteparin can be monitored effectively using standard coagulation times. Clin Appl Thromb Hemost. 2005;11:127–38.
Greiber S, Weber U, Galle J, Bramer P, Schollmeyer P. Activated clotting time is not a sensitive parameter to monitor anticoagulation with low molecular weight heparin in hemodialysis. Nephron. 1997;76:15–9.
Henry TD, Satran D, Knox LL, Iacarella CL, Laxson DD, Antman EM. Are activated clotting times helpful in the management of anticoagulation with subcutaneous low-molecular-weight heparin? Am Heart J. 2001;142:590–3.
Linkins LA, Julian JA, Rischke J, Hirsh J, Weitz JI. In vitro comparison of the effect of heparin, enoxaparin and fondaparinux on tests of coagulation. Thromb Res. 2002;107:241–4.
Rabah MM, Premmereur J, Graham M, Fareed J, Hoppensteadt DA, Grines LL, et al. Usefulness of intravenous enoxaparin for percutaneous coronary intervention in stable angina pectoris. Am J Cardiol. 1999;84:1391–5.
Briggs C, Guthrie D, Hyde K, Mackie I, Parker N, Popek M, et al. Guidelines for point-of-care testing: haematology. Br J Haematol. 2008;142:904–15.
Perry DJ, Fitzmaurice DA, Kitchen S, Mackie IJ, Mallett S. Point-of-care testing in haemostasis. Br J Haematol. 2010;150:501–14.
Samama MM, Martinoli JL, LeFlem L, Guinet C, Plu-Bureau G, Depasse F, et al. Assessment of laboratory assays to measure rivaroxaban–an oral, direct factor Xa inhibitor. Thromb Haemost. 2010;103:815–25.
Vukovich T, Proidl S, Teufelsbauer H, Kautzky A, Erlacher L, Luger A, et al. Laboratory monitoring of thromboprophylaxis with low molecular weight and standard heparin. Thromb Res. 1992;66:735–43.
Wajima T, Isbister GK, Duffull SB. A comprehensive model for the humoral coagulation network in humans. Clin Pharmacol Ther. 2009;86:290–8.
Tanos PP, Isbister GK, Lalloo DG, Kirkpatrick CM, Duffull SB. A model for venom-induced consumptive coagulopathy in snake bite. Toxicon. 2008;52:769–80.
Kogan AE, Kardakov DV, Khanin MA. Analysis of the activated partial thromboplastin time test using mathematical modeling. Thromb Res. 2001;101:299–310.
O’Leary MA, Isbister GK. A turbidimetric assay for the measurement of clotting times of procoagulant venoms in plasma. J Pharmacol Toxicol Methods. 2010;61:27–31.
Conard J, Brosstad F, Lie Larsen M, Samama M, Abildgaard U. Molar antithrombin concentration in normal human plasma. Haemostasis. 1983;13:363–8.
Lindhoff-Last E, Samama MM, Ortel TL, Weitz JI, Spiro TE. Assays for measuring rivaroxaban: their suitability and limitations. Ther Drug Monit. 2010;32:673–9.
ACKNOWLEDGMENTS & DISCLOSURES
The authors acknowledge the support of University of Otago Postgraduate Scholarship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gulati, A., Faed, J.M., Isbister, G.K. et al. Development and Evaluation of a Prototype of a Novel Clotting Time Test to Monitor Enoxaparin. Pharm Res 29, 225–235 (2012). https://doi.org/10.1007/s11095-011-0537-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-011-0537-z