Abstract
Purpose
Sorafenib, an oral multitargeted tyrosine kinase inhibitor, is highly bound to plasma proteins (>99.5%). Little is known about the influence of variations in sorafenib protein binding on its disposition. The aims of this study were to characterize in vitro sorafenib binding properties to albumin using the quenching fluorescence method and investigate the influence of albuminemia and bilirubinemia on sorafenib disposition in 54 adult cancer patients.
Results
In vitro estimate of sorafenib dissociation constant (Kd) for albumin was 0.22 μM [CI95 0.20–0.23]. In physiological conditions, sorafenib unbound fraction would increase 1.7-fold as albuminemia decreased from 45 g/L (680 μM) to 30 g/L (453 μM). In presence of bilirubin, apparent Kd of sorafenib was ~1.5-fold greater for bilirubin/albumin molar ratio of 1:4. In clinical settings, median sorafenib clearance (CL) was 1.42 L/h (0.75–2.13 L/h). In univariate analysis, sex, body mass index, and albuminemia were associated with CL (p = 0.04, 0.048, and 0.008, respectively). In multivariate analysis, albuminemia (p = 0.0036) was the single parameter independently associated with CL.
Conclusion
These findings highlight the major influence of albuminemia on sorafenib clearance and its disposition in cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sorafenib (Nexavar®), an oral multitargeted tyrosine kinase inhibitor, targets the kinase domains of vascular endothelial growth factor receptors (VEGFR-2 and VEGFR-3) and platelet-derived growth factor receptor family (PDGFR-ß and stem cell factor receptor [KIT]) (1). Additionally, it inhibits the kinase activity of both C-RAF and B-RAF. Sorafenib as a single-agent has demonstrated preclinical and clinical activity against several tumor types (2–6). In contrast with standard antineoplastics, sorafenib was also shown to be suitable for long-term administration because of its good safety profile (7). Currently, sorafenib is approved for the treatment of patients with advanced renal cell carcinoma and those with hepatocellular carcinoma.
A large interindividual variability in sorafenib disposition was observed in the different Phase I monotherapy trials (8). In contrast with other available tyrosine kinase inhibitors (9), little is known about the sources of pharmacokinetic variability for sorafenib. To date, only food has been identified as a factor that may contribute to this variability. However, conflicting data on this issue are published (10,11). Sorafenib is highly bound (>99.5%) to plasma proteins and has a low hepatic extraction yield (11). Therefore, its total clearance (CL) depends primarily on its plasma unbound fraction (fu), as long as the intrinsic clearance is unaffected. Hence, variations in sorafenib protein binding may contribute to the variability in sorafenib exposure.
Sorafenib is mainly bound to albumin, whose physiological role is also to serve as a transporter for fatty acids and bilirubin. In several pathological states, these endogenous ligands can accumulate to relatively high concentrations that can displace drugs highly bound to albumin, resulting in a significant increase in fu of these drugs (12). Patients with advanced solid tumors frequently exhibit denutrition, severe renal or hepatic impairment. Under those circumstances, hypoalbuminemia, hypertriglyceridemia or hyperbilirubinemia can occur; therefore, an increase in sorafenib fu resulting in an enhanced CL should be expected. In this context, characterizing the sorafenib binding to albumin is of critical pharmacological and clinical interest. Finally, Zsila et al. recently showed that sorafenib also binds to α1-acid glycoprotein (AAG) (13), although this result is in disagreement with the data provided by the manufacturer of sorafenib (11). As serum AAG concentration can be increased by 1.6–3.0 fold in several neoplasia, AAG may potentially be a parameter influencing sorafenib CL.
By using the quenching fluorescence method, we aimed to first characterize in vitro the binding properties of sorafenib to albumin and AAG, then to investigate the influence of bilirubin and fatty acids on sorafenib binding to albumin. Given that our in vitro data suggested that hypoalbuminemia and/or severe hyperbilirubinemia might modulate sorafenib albumin binding in vivo, we explored the influence of albuminemia and bilirubinemia on drug disposition in adult outpatients with advanced solid tumors receiving single-agent sorafenib.
Materials and Methods
Chemicals and Apparatus
Human serum albumin (HSA, fraction V fatty acid free), AAG from human plasma (purity 99%), myristic acid (MYR), dimethyl sulfoxide (DMSO) and Tris-HCl were purchased from Sigma (St. Louis, MO, USA). Sorafenib was purchased in LC Laboratories (Woburn, USA). A 2 μM protein solution (HSA or AAG) was prepared in Tris-HCl buffer solution (0.5 M, pH 7.4). Stock solution of sorafenib (1 g/L) was prepared in methanol, then stored at −20°C in the dark. Stock solution of MYR (5,000 μM) was prepared in methanol, then stored at 4°C in the dark up to 1 week. Stock solution of bilirubin (250 μM) was daily prepared in 0.5 M NaOH.
A Shimadzu RF-1501 fluorescence spectrophotometer (Champs sur Marne, France) equipped with a 10 mm quartz cell was used to measure the fluorescence spectra and the fluorescence intensity. The maximum excitation wavelength (λexc) and maximum emission wavelength (λmax) for HSA and AAG were 280 nm and 354 nm, respectively. Sorafenib, bilirubin and MYR had negligible fluorescence at λexc of 280 nm.
The chromatography system used to assay plasma sorafenib concentration consisted of Dionex Ultimate 300 equipped with a gradient pump with degas option and gradient mixer, a UV-visible detector, an autosampler, and a Chromeleon® chromatography workstation (Dionex Corporation, Sunnyvale, CA, USA). Chromatographic separation was achieved on a C8+ Satisfaction® (250 mm × 3 mm, 5 μm; Cluzeau Info Labo, Courbevoie, France) associated with a guard column packed with the same bonded phase.
Sorafenib Binding to Albumin or α1-Acid Glycoprotein
Appropriate amounts of sorafenib were transferred in 5 ml glass tube and evaporated to dryness under a gentle stream of nitrogen gas. Then, the dry residues were reconstituted with 50 μl of DMSO and completed to 1 ml with 2 μM protein solution (HSA or AAG). The final concentrations of sorafenib were in the range 0.05–50 μM. The resultant mixture was incubated 1 h at 37°C. A blank system containing 50 μl DMSO and 950 μl of 2 μM protein solution was similarly prepared. After 1 h incubation, fluorescence intensity was measured. Each experiment was performed in triplicate.
Influence of MYR and Bilirubin on Sorafenib Binding to Albumin
Appropriate amounts of sorafenib were transferred in 5 ml glass tube and evaporated to dryness under a gentle stream of nitrogen gas. Dry residues were reconstituted in 1 ml of 2 μM HSA solution including either MYR or bilirubin solution 2% (v/v). MYR or bilirubin was added in HSA solution during sorafenib dry residue reconstitution. The incubation time for MYR and bilirubin was 60 min. In presence of bilirubin, the mixture was incubated in the dark to avoid photodegradation of bilirubin (14). The final concentrations of sorafenib were in the range 0.05–10 μM. The final concentrations of MYR were 10, 20, 100 and 250 μM, and those of bilirubin were 0.1, 0.5, 1 and 5 μM. These concentrations of MYR and bilirubin were far from those observed in physiological conditions, but the ratios MYR/HSA or bilirubin/HSA were in the physiological range.
Data Analysis from the Quenching Method
The fluorescence intensity versus drug concentration data were analyzed by non-linear regression. The fluorescence intensity was calculated as the mean of the three experiments. The exact mathematical expression for describing competitive binding of two different ligands (sorafenib and bilirubin) to a protein molecule (15) was fitted to the data by weighted least-squares. The coefficient of variation (CV) of the residual error model used for weighting fluorescence intensity measurements was assumed to be constant and equal to 3%. This model involves the dissociation constant (Kddrug, KdL) of each ligand, the common binding capacity (Bmax) of the drug, the fixed total concentration of the interacting ligand (Lt), as well as parameters related to the quenching ability of both ligands. From these parameters, the bound drug concentration (Cb) could be calculated from the unbound protein concentration (Pu) and the total concentration of drug (Ct) as \( {{\text{C}}_{\text{b}}} = {{\text{C}}_{\text{t}}} \times {{\text{P}}_{\text{u}}}/\left( {{\text{K}}{{\text{d}}_{\text{drug}}} + {{\text{P}}_{\text{u}}}} \right) \). The unbound concentration of drug (Cu) was calculated from the formula Cu = Ct−Cb, and the unbound fraction (fu) as fu = Cu/Ct. In presence of a competitive ligand (L), the apparent Kd of the drug was calculated as \( {\text{K}}{{\text{d}}_{\text{app}}} = {\text{K}}{{\text{d}}_{\text{drug}}} \times \left[ {1 + \left( {{{\text{L}}_{\text{u}}}/{\text{Ki}}} \right)} \right] \), where Lu is the unbound concentration of the competitive ligand and Ki is equal to KdL in most instances. By using the quenching fluorescence method, we recently investigated the binding properties of bilirubin to albumin and documented a Kd value of 1.06 μM for bilirubin (16). This value was thus used as Ki for bilirubin. Finally, sorafenib unbound fraction in in vivo conditions was extrapolated from the formula: \( {\text{fu}} = {\text{Kd}}/\left( {{\text{Kd}} + {\text{n}} * {{\text{P}}_{\text{t}}} - {{\text{C}}_{\text{t}}}} \right) \), where Pt and n are protein concentration and the number of binding sites on protein for sorafenib, respectively. Given that the total plasma sorafenib concentration ranges from 2 to 10 mg/L in clinical settings, the total sorafenib concentration (Ct) was fixed at 5 mg/L (=10.8 μM). The results are expressed as point estimates [95% confidence interval].
Clinical Study
From April 2008 to July 2010, consecutive unselected patients with advanced solid tumors were prospectively included in a study cohort regardless of the type of tumor. To be eligible, cancer patients (>18 years old) had to be treated by single agent sorafenib. This study was approved by the local Review Board for Oncology, and all patients provided written informed consent, in compliance with the ethical principle of the revised Declaration of Helsinki (Edimburg, 2000) and according to French regulations.
According to their general status, patients were started on sorafenib at a daily dose of 200 or 400 mg twice daily. At the time of the first follow-up visit (at least 8 days after treatment initiation), plasma samples were collected to assess plasma sorafenib concentrations at steady state. Sorafenib concentration determinations were conducted in our laboratory using a previously published method (17). The accuracy, within-assay and between-assay precision of this method were 96.9–104.0%, 3.4–6.2% and 7.6–9.9%, respectively. Finally, a specific bayesian estimator developed in our institution (18) allowed estimating individual sorafenib CL. A one-compartment model with saturated absorption, first-order intestinal loss and linear elimination was implemented in the ADAPT II software package (19), then used to estimate individual sorafenib clearance. For the residual error model, the coefficient of variation (CV) of the residual error was assumed to be constant, with CV fixed to 40%, in agreement with a previous unpublished population study.
Statistical Analyses for the Clinical Study
Results are expressed as median (range) or [interquartile range]. Categorical data were summarized by frequency counts and percentages. Associations between CL and baseline parameters (age, sex, body mass index (BMI), AST, ALT, GGT, ALP, bilirubinemia, albuminemia and C-reactive protein (CRP) level) were inferred using the Spearman correlation test or the Mann-Whitney U-test when appropriate. In order to identify the independent factors influencing sorafenib CL, multivariate analysis was done using a multiple regression with both forward and backward selection methods. Variables that showed a significance of p < 0.05 in the univariate analysis were selected for inclusion in the multivariate analysis. All the results from the multivariate analysis with p < 0.05 were considered significant. The 95% confidence interval (CI95%) of parameter estimates was obtained by bootstrapping (3,000 replications). Calculations were done with NCSS 2007 software (NCSS, Kaysville, UT).
Results
Binding Properties to Albumin or α1-Acid Glycoprotein
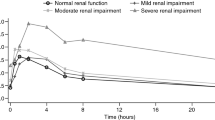
As shown in Fig. 1, sorafenib quenched both HSA (Fig. 1a) and AAG (Fig. 1b) fluorescence in a concentration-dependent manner. For HSA, the estimates of Kd and Bmax were 0.22 [0.20–0.23] μM and 0.66 [0.61–0.70] μM, respectively. For AAG, the estimates of Kd and Bmax were 0.90 [0.31–1.48] μM and 1.39 [0.45–2.34] μM, respectively. As a 2 μM protein solution was used for these analyses, we calculated that 0.33 mol of sorafenib can be bound by 1 mol of HSA and that 0.70 mol can be bound by 1 mol of AAG. Given that Ka = 1/Kd, the AAG/HSA nKa ratio would be 0.52. Fig. 2 presents a simulation of sorafenib fu at various physiological plasma concentrations of HSA (Fig. 2a) or AAG (Fig. 2b). Thus, sorafenib fu would be 0.1% and 0.17% at albumin concentration of 680 μM (45 g/L) and 453 μM (30 g/L), respectively. Regarding AAG, sorafenib fu would be 2.8% and 0.78% at physiological concentrations of 30 μM (1.3 g/L) and 90 μM (3.9 g/L).
Simulation of sorafenib unbound fraction to various plasma concentrations of (a) albumin or (b) α1-acid glycoprotein (AAG). The relation between drug unbound fraction (fu) and protein concentration (Cprot) was extrapolated from the formula \( {\text{fu}} = \left( {{\text{K}}{{\text{d}}_{\text{sorafenib}}}/\left( {{\text{K}}{{\text{d}}_{\text{sorafenib}}} + \left( {{\text{n}} * {{\text{C}}_{\text{prot}}}} \right) - {\text{C}}{{\text{t}}_{\text{drug}}}} \right)} \right) * 100 \). Total sorafenib concentration (Ctdrug) was fixed at 10.8 μM (=5 mg/L).
In Vitro Influence of Bilirubin and MYR on Sorafenib Binding to Albumin
In presence of bilirubin or MYR, the binding of sorafenib to albumin was disrupted (Fig. 3). For bilirubin concentrations ranging from 0.5 to 5 μM, Kdapp of sorafenib was approximately 1.4- to 5.5-fold greater than Kd previously determined without bilirubin (Table I). At MYR concentrations of 100 and 250 μM, Kdapp of sorafenib was approximately 4- and 10-fold greater than Kd previously determined without MYR, respectively (Table I).
Quenching curves of human serum albumin in presence of sorafenib and myristic acid (a) or bilirubin (b). RF0 is the relative fluorescence intensity of albumin in the presence of endogenous ligand (myristic acid or bilirubin) at respective concentration. RF is the relative fluorescence intensity in presence of sorafenib and endogenous ligand.
Clinical Study
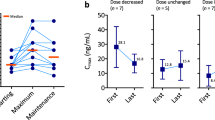
Fifty-four adult cancer patients with advanced solid tumors were enrolled in the study. Clinical and biological baseline characteristics are summarized in Table II. The most common primary tumor sites were melanoma (37%) and hepatocellular carcinoma (26%). The median sampling time after treatment initiation was 11 (7–28) days. The median dose of sorafenib was 800 mg/day (400–800). The median sorafenib clearance was 1.42 L/h (0.75–2.13 L/h) (Fig. 4). In the univariate analysis, sex (p = 0.04), BMI (p = 0.048) and albuminemia (p = 0.008) were the three parameters associated with sorafenib CL (Table III). In the multivariate analysis, albuminemia (p = 0.0036) was the single parameter independently associated with sorafenib CL. Overall, the relation was CL = 2.37 [CI95 1.73–3.0]–0.026 [CI95 −0.043– −0.009]*albuminemia (r = 0.39).
Discussion
The pharmacokinetics of sorafenib in cancer patients display a substantial interindividual variability (8). The knowledge of factors that contribute to its pharmacokinetic variability is warranted to better anticipate excessive toxicity and, conversely, lack of efficacy. As reported herein, our data offer the first evidence that albuminemia influences sorafenib CL and thus contributes to the interindividual variability in sorafenib disposition.
By using the induced circular dichroism (ICD) spectroscopy, Zsila et al. previously reported AAG and albumin values of sorafenib Kd which are approximately 2- and 100-fold higher than ours, respectively (13). Differing experimental conditions may account for the large discrepancy in albumin values of sorafenib Kd between the two investigations. Indeed, Zsila et al. used a physiological concentration of albumin, while we worked at a low, non-physiological concentration (2 μM) to avoid the non-linearities caused by the inner filter effect. However, Parikh et al. showed for several drugs that the quenching fluorescence method correlated well with equilibrium dialysis, a reference technique using physiological concentrations of albumin (20). Therefore, their work supports the idea that the low concentration of albumin does not affect the estimation of sorafenib Kd. In contrast, the fatty-acid composition of albumin may influence the affinity of sorafenib for albumin and therefore explain the discrepancy between the two studies, but Zsila et al. do not provide this specific information. Overall, the difference in albumin values of sorafenib Kd between the two studies remains unclear. From our Kd value and number of binding sites, we estimated a 99.9% binding of sorafenib to albumin at normal physiological concentration (45 g/L). However, based on an extrapolation, the estimate is greatly concordant with the results documented in vivo by the manufacturer and Miller et al. (99.9 and 99.5%, respectively) (11,21). Taken together, these different results support the reliability of the quenching fluorescence method to explore the protein binding characteristics of sorafenib. Additionally, they confirm that sorafenib binds to AAG, but to a greater extent to albumin. Despite the strong binding affinity of sorafenib to AAG, the AAG/HSA n.Ka.P ratio would not be large enough to compensate the higher concentration of albumin (~670 μM) over AAG (20–40 μM) in plasma. This would remain true even if the increased AAG and reduced HSA plasma levels in malignant diseases were taken into account. Therefore, these results confirm that sorafenib is primarily bound to albumin in human plasma.
This is the first report to investigate in vitro the influence of bilirubin and MYR on sorafenib binding to albumin. Of all the factors investigated, we found that the albumin concentration itself provided the most substantial effect. Thus, sorafenib fu would increase 1.7-fold if the HSA concentration decreased from its physiological concentration of 45 g/L to 30 g/L. Regarding the influence of endogenous ligands on sorafenib binding, our experiments suggest that in clinical settings, the risk of competition with sorafenib for albumin binding sites appears further likely with bilirubin than with fatty acids. Indeed, bilirubin significantly disrupts sorafenib binding to albumin for a bilirubin/albumin molar ratio of 1:4. Physicians should be aware that a patient with normal albumin concentration (~670 μM) may present this 1:4 ratio when his total bilirubin concentration is greater than 170 μM. Therefore, a significant competition between sorafenib and bilirubin for albumin binding sites should be expected in patients experiencing severe hyperbilirubinemia. In contrast, no significant effect of MYR on sorafenib albumin binding was observed up to a MYR/albumin molar ratio of 10:1. As the free fatty acids/albumin molar ratio rarely exceeds 8:1 in severe physiological states (12), the event of a competition between sorafenib and fatty acids for albumin binding sites seems to be unlikely in clinical settings. Overall, our in vitro data suggest that hypoalbuminemia and/or severe hyperbilirubinemia in cancer patients might cause wide variations in sorafenib fu.
Many studies have demonstrated considerable interindividual variability in sorafenib exposure in cancer patients treated with single-agent sorafenib (9). In agreement with these studies, we observed a large variability in sorafenib disposition at steady state in our cohort. Herein, we present the first report of an inverse correlation between sorafenib CL and albuminemia. Additionally, in the multivariate analysis, albuminemia was the sole factor that was significantly associated with sorafenib CL. These results suggest that albuminemia may contribute to the interindividual variability in sorafenib disposition. Sorafenib CL primarily depends on fu, as long as the intrinsic clearance is unaffected. In this context, the variability in CL could result from fluctuations in fu related to variations in albuminemia. Our in vivo simulation supports this hypothesis. However, the determination of the plasma sorafenib fu, which would allow adequate demonstration, could not be performed because of a lack of sensitivity in our analytical method. To our knowledge, only Miller et al. explored the variations in sorafenib fu in cohorts of cancer patients with varying degrees of hepatic or renal impairment (21). Sorafenib fu was assessed after a single 400 mg-dose of sorafenib in patients with solid tumors or hematologic malignancies (multiple myeloma, non-Hodgkin’s lymphoma). The work of Miller et al. points out the high variability in sorafenib fu regardless of albuminemia and bilirubinemia. Furthermore, the authors have failed to identify a relationship between sorafenib fu and albuminemia or bilirubinemia (21). As we could not directly measure fu in the present work, the comparison between our results and those of Miller et al. should be interpreted with caution. Further studies are needed to clarify the variations in sorafenib fu in patients experiencing hypoalbuminemia and/or hyperbilirubinemia.
Inflammation, a common feature in cancer disease, is known to down-regulate both CYP3A4 expression and metabolic activities in liver and extra-hepatic tissues (22). Alexandre et al. recently reported a relationship between CYP3A4 activity and inflammatory status in cancer patients under docetaxel (23). Sorafenib is subjected to CYP3A4-mediated oxidation and UGT1A9-mediated glucuronidation; thereby, inflammatory status could influence sorafenib clearance. In the present study, the CRP level is not associated with sorafenib clearance in the multivariate analysis. As CYP3A4 pathway may account for a small fraction of the total elimination of sorafenib (24), the influence of the inflammatory status on sorafenib clearance could be limited. Further investigations are required to confirm this result.
Finally, it is important to realize that an increase in sorafenib fu would increase its clearance, thereby lowering its total concentration in plasma, while the average free active concentration would remain unchanged because both variations compensate each other exactly. This phenomenon has been well documented in transplant recipients treated with mycophenolic acid, another restrictively cleared drug which is highly bound to albumin (25,26). In this context, the pharmacokinetic/pharmacodynamic relationships for antitumor activity or toxicity based on sorafenib total exposure can be biased or confounded in clinical trials including hypoalbuminemic patients. Besides, the therapeutic drug monitoring for sorafenib is not currently recommended, but the large interindividual variability in sorafenib disposition (9) and the risk of pharmacokinetic drug-drug interactions (27) support its use. Patients treated with sorafenib frequently exhibit hypoalbuminemia related to denutrition, hepatic impairment or proteinuria, a common sorafenib-induced adverse event. Under those circumstances, a low total sorafenib exposure may be falsely interpreted as a low exposure to free active sorafenib, leading to the unnecessary recommendation of a higher dose and therefore to overexposure that might result in severe toxicity. This suggests that hypoalbuminemia should be taken into account in association with clinical end-points to rationalize sorafenib dosing regimens in cancer patients with low total sorafenib exposure.
In conclusion, the present findings shed light on the major influence of albuminemia on sorafenib CL and therefore on its disposition in adult cancer patients with advanced solid tumors. According to our in vitro experiments, severe hyperbilirubinemia should also affect CL. Overall, the present study paves the way for monitoring of albuminemia in a context of an individualized dosing regimen of sorafenib in cancer patients. Further studies are warranted to confirm this hypothesis.
Abbreviations
- AAG:
-
α1-acid glycoprotein
- ALP:
-
alkaline phosphatase
- ALT:
-
aspartate alaninetransferase
- AST:
-
aspartate aminotransferase
- Bmax :
-
common binding capacity
- BMI:
-
body mass index
- Cb :
-
bound drug concentration
- CL:
-
total clearance
- CRP:
-
protein C-reactive
- Ct :
-
total concentration of drug
- CU :
-
unbound concentration of drug
- CV:
-
coefficient of variation
- DMSO:
-
dimethyl sulfoxide
- fu:
-
unbound fraction
- GGT:
-
Gamma-glutamyl transpeptidase
- HSA:
-
human serum albumin
- ICD:
-
induced circular dichroism
- Kd:
-
dissociation constant
- Kdapp :
-
apparent dissociation constant
- Ki:
-
inhibitor constant
- Lt :
-
concentration of interacting ligand
- MYR:
-
myristic acid
- PDGFR:
-
platelet-derived growth factor receptor
- Pu :
-
unbound protein concentration
- VEGFR:
-
vascular endothelial growth factor receptor
- λexc:
-
maximum excitation wavelength
- λmax:
-
maximum emission wavelength
References
Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64(19):7099–109.
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Staehler M, et al. Sorafenib for treatment of renal cell carcinoma: final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol. 2009;27(20):3312–8.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Wilhelm SM, Adnane L, Newell P, Villanueva A, Llovet JM, Lynch M. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol Cancer Ther. 2008;7(10):3129–40.
Kloos RT, Ringel MD, Knopp MV, Hall NC, King M, Stevens R, et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol. 2009;27(10):1675–84.
Pecuchet N, Avril M, Kerob D, Billemont B, Blanchet B, Herait P, et al. Relationship between dose, exposure, and antitumoral activity of sorafenib in melanoma. J Clin Oncol. 2010;28(15):suppl (May 20), Abstract 8582.
Blanchet B, Billemont B, Barete S, Garrigue H, Cabanes L, Coriat R, et al. Toxicity of sorafenib: clinical and molecular aspects. Expert Opin Drug Saf. 2010;9(2):275–87.
Strumberg D, Clark JW, Awada A, Moore MJ, Richly H, Hendlisz A, et al. Safety, pharmacokinetics, and preliminary antitumor activity of sorafenib: a review of four phase I trials in patients with advanced refractory solid tumors. Oncologist. 2007;12(4):426–37.
van Erp NP, Gelderblom H, Guchelaar HJ. Clinical pharmacokinetics of tyrosine kinase inhibitors. Cancer Treat Rev. 2009;35(8):692–706.
Strumberg D, Richly H, Hilger RA, Schleucher N, Korfee S, Tewes M, et al. Phase I clinical and pharmacokinetic study of the Novel Raf kinase and vascular endothelial growth factor receptor inhibitor BAY 43-9006 in patients with advanced refractory solid tumors. J Clin Oncol. 2005;23(5):965–72.
European Medicines Agency. Sorafenib (Nexavar): summary of product characteristics [online]. Available from URL: http://www.ema.europa.eu/humandocs/PDFs/EPAR/nexavar/H-690-en6.pdf.
Tesseromatisand C, Alevizou A. The role of the protein-binding on the mode of drug action as well the interactions with other drugs. Eur J Drug Metab Pharmacokinet. 2008;33(4):225–30.
Zsila F, Fitos I, Bencze G, Keri G, Orfi L. Determination of human serum alpha1-acid glycoprotein and albumin binding of various marketed and preclinical kinase inhibitors. Curr Med Chem. 2009;16(16):1964–77.
Weisiger RA, Ostrow JD, Koehler RK, Webster CC, Mukerjee P, Pascolo L, et al. Affinity of human serum albumin for bilirubin varies with albumin concentration and buffer composition: results of a novel ultrafiltration method. J Biol Chem. 2001;276(32):29953–60.
Wang ZX. An exact mathematical expression for describing competitive binding of two different ligands to a protein molecule. FEBS Lett. 1995;360(2):111–4.
Vial Y, Tod M, Hornecker M, Urien S, Conti F, Dauphin A, et al. In vitro influence of fatty acids and bilirubin on binding of mycophenolic acid to human serum albumin. J Pharm Biomed Anal. 2011;54(3):607–9.
Blanchet B, Billemont B, Cramard J, Benichou AS, Chhun S, Harcouet L, et al. Validation of an HPLC-UV method for sorafenib determination in human plasma and application to cancer patients in routine clinical practice. J Pharm Biomed Anal. 2009;49(4):1109–14.
Boudou-Rouquette P, Blanchet B, Mir O, Billemont B, Ropert S, Barete S, et al. Proposal of a new population pharmacokinetics (PK) model of sorafenib and rationale for a three-daily schedule. J Clin Oncol. 2010;28:7s (abstr 3044).
D’Argenioand DZ, Schumitzky A. ADAPT II user’s guide: pharmacokinetic/pharmacodynamic systems analysis software. Los Angeles: Biomedical Simulations Resource; 1997.
Parikh HH, McElwain K, Balasubramanian V, Leung W, Wong D, Morris ME, et al. A rapid spectrofluorimetric technique for determining drug-serum protein binding suitable for high-throughput screening. Pharm Res. 2000;17(5):632–7.
Miller AA, Murry DJ, Owzar K, Hollis DR, Kennedy EB, Abou-Alfa G, et al. Phase I and pharmacokinetic study of sorafenib in patients with hepatic or renal dysfunction: CALGB 60301. J Clin Oncol. 2009;27(11):1800–5.
Morgan ET. Impact of infectious and inflammatory disease on cytochrome P450-mediated drug metabolism and pharmacokinetics. Clin Pharmacol Ther. 2009;85(4):434–8.
Alexandre J, Rey E, Girre V, Grabar S, Tran A, Montheil V, et al. Relationship between cytochrome 3A activity, inflammatory status and the risk of docetaxel-induced febrile neutropenia: a prospective study. Ann Oncol. 2007;18(1):168–72.
Lathia C, Lettieri J, Cihon F, Gallentine M, Radtke M, Sundaresan P. Lack of effect of ketoconazole-mediated CYP3A inhibition on sorafenib clinical pharmacokinetics. Cancer Chemother Pharmacol. 2006;57(5):685–92.
Benichou AS, Blanchet B, Conti F, Hornecker M, Bernard D, Taieb F, et al. Variability in free mycophenolic acid exposure in adult liver transplant recipients during the early posttransplantation period. J Clin Pharmacol. 2010;50(10):1202–10.
de Winter BC, van Gelder T, Sombogaard F, Shaw LM, van Hest RM, Mathot RA. Pharmacokinetic role of protein binding of mycophenolic acid and its glucuronide metabolite in renal transplant recipients. J Pharmacokinet Pharmacodyn. 2009;36(6):541–64.
Gomo C, Coriat R, Faivre L, Mir O, Ropert S, Billemont B, et al. Pharmacokinetic interaction involving sorafenib and the calcium-channel blocker felodipine in a patient with hepatocellular carcinoma. Invest New Drugs. 2010; 2Aug 13 [Epub ahead of print].
Acknowledgments & Disclosures
We acknowledge the help of J. Lecas (Centre de Langues de la Maison des Langues, Université Paris Descartes) in proofreading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tod, M., Mir, O., Bancelin, N. et al. Functional and Clinical Evidence of the Influence of Sorafenib Binding to Albumin on Sorafenib Disposition in Adult Cancer Patients. Pharm Res 28, 3199–3207 (2011). https://doi.org/10.1007/s11095-011-0499-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-011-0499-1