ABSTRACT
Purpose
In hematopoietic stem cell transplantation (HSCT), cyclosporin is used to prevent graft-versus-host disease (GVHD). However, cyclosporin distribution in tissues is not linear, resulting in uncertainty regarding optimal dosing and monitoring. The objective of this study was to link the probability and severity of acute GVHD to cyclosporin exposure in blood, GVHD target organs, and lymphoid organs.
Methods
A physiologically based pharmacokinetic model of cyclosporin disposition and logistic regression models were used. Sixty-one pediatric patients undergoing HSCT were studied. Cyclosporin was administered by intermittent (n = 31) or continuous infusion (n = 30).
Results
At steady state (1 day before acute GVHD), exposures in all organs were related with the probability and severity of acute GVHD. Average cyclosporin concentration or, equivalently, its area under the curve (AUC) was the pharmacokinetic index best correlated with the anti-GVHD effect. Cyclosporin AUC in interstitial fluid of lymphoid organs was a superior index than that in blood, but marginally.
Conclusion
Hence, AUC in blood maybe used as an index of cyclosporin efficacy. Using our model, target AUCs in blood could be defined for malignant and non-malignant diseases, as well as the equivalent target values for C2 and C0 concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Allogeneic hematopoietic stem cell transplantation (HSCT) may induce acute graft-versus-host disease (aGVHD), which mainly occurs in skin, liver, and intestines (1). Despite progress in prophylaxis, aGVHD is still responsible for significant morbidity and mortality in HSCT recipients (2). Cyclosporin, an immunosuppressant drug, is used to prevent aGVHD. This drug exhibits a relatively narrow therapeutic window (3) and large inter-individual pharmacokinetic variability. Therefore, in order to improve therapeutic efficacy and reduce aGVHD, it is critical to optimize the dose regimen of cyclosporin to achieve and maintain the concentration in the target range (4–6). Severe GVHD carries a poor prognosis, with 25% long-term survival for grade III and 5% for grade IV (7).
In HSCT, cyclosporin is usually administered by intravenous infusion during the first 2 or 3 weeks following transplantation, before switching to the oral route. Continuous infusion (CI) and 2-h intermittent infusions (II) are commonly used, but there is no consensus regarding the best mode of administration (8). Our previous study, using a physiologically based pharmacokinetic model, showed that the area under the receptor occupancy versus time curve in the interstitial fluid of aGVHD target organs was greater after CI than after II, suggesting that CI maybe more efficacious (9).
There is also no consensus on the best way to monitor cyclosporin concentrations. The indices commonly considered for cyclosporin monitoring include trough concentration (C0), 2-h concentration (C2, in case of administration by 2-h infusion or by the oral route), plateau concentration (in case of continuous infusion), and AUC. In solid organ transplantation, concentration sampling 2 h after administration is usually considered as the best single method to predict exposure and effect (side effects and rate of rejection) (10–13). Following renal transplantation, both C2 and C0 were shown to be useful in predicting cyclosporin side effects (14). However, abbreviated AUC monitoring identified patients at risk for acute rejection more accurately than C2 (15). In HSCT, C0 was found to be a better predictor of aGVHD than C2 (4,16). An inverse relationship also exists between the probability of severe aGVHD and the median cyclosporin concentration during the week before engraftment (17). Information regarding the possible association between aGVHD and cyclosporin AUC-12 h is not currently available (18).
The main objective of this study was to identify the pharmacokinetic index of cyclosporin exposure best correlated with aGVHD occurrence and severity. The second objective was to determine the target values of this index to maximize the probability of obtaining the desired grade of GVHD in malignant and non-malignant diseases.
MATERIALS AND METHODS
Clinical Study
This was a retrospective, monocentric study. We studied the records of pediatric patients (4 months to 17 years of age) that underwent allogeneic bone marrow transplantation and received cyclosporin for the prevention of graft-versus-host disease (GVHD). The patients gave a written consent to use their data at the time of admission. Cyclosporin treatment was started the day before transplantation. The patients comprised two groups. In the first group, 30 patients were treated with cyclosporin administered by continuous infusion (CI group). In the second group, 31 patients received cyclosporin by intermittent infusion, twice daily (for 2 h every 12 h, II group). The patients in the two groups were matched for age, sex, indication for transplantation (malignant vs. non-malignant disease), proportion of related donors, administration of anti-lymphocyte serum, and number of mismatches when the donor was unrelated. The stem cell source was unmanipulated bone marrow from all donors. No methotrexate was administered.
For each patient, periodic monitoring of whole-blood cyclosporin concentration was performed (EMIT, Dade Behring, Deerfield, Illinois, USA) on a Cobas Mira® analyzer automate. The dosing regimen was adjusted with a Bayesian method (USC*Pack® Software, version 10.0, Laboratory of Applied Pharmacokinetics, University of Southern California, USA) to achieve and maintain the target blood cyclosporin concentration. The target concentrations were defined as described in our previous studies (4,19). In the CI group, the target steady-state concentration was 200 μg/l (malignant disease) or 280 μg/l (non-malignant disease). In the II group, the target was a 12-h trough concentration of 110 μg/l (malignant disease) or 130 μg/l (non-malignant disease).
The aGVHD was graded according to the classification of Glucksberg modified by Armitage (20–22). This scale determines aGVHD severity (from grade 0 to IV, no aGVHD to maximum severity) by a combination of the scores of the three target organs (skin, intestines and liver) of aGVHD. These organs are graded independently from 0 to 4, corresponding to the extent of skin rash, diarrhea volume, and total bilirubin concentrations.
PBPK Model in Pediatric Patients and Predicted Exposure
The pediatric physiologically based pharmacokinetic (PBPK) model, including 11 organs validated in children (9), was fitted individually to the venous whole-blood cyclosporin concentrations of the 61 pediatric patients undergoing HSCT and receiving only cyclosporin as immunosuppressive treatment. For each patient, the data records included the dosing history, the first two concentration measurements, body weight, age, and hematocrit. The estimated parameters were the hepatic intrinsic clearance and the plasma unbound fraction of cyclosporin. A Bayesian estimator (Maximum a Posteriori) was used to estimate these parameters, as described in our previous study (9). The areas under the concentration vs. time curves (AUC D1, from 0 to 24 h after the onset of treatment, and AUC SS, at steady state) were estimated by numerical integration in several compartments (venous blood and interstitial compartments of bone including bone marrow, skin, liver, thymus, and intestines), using the dosing history of each child. The time corresponding to steady state was defined as the day before the occurrence of aGVHD, or day 13 when no aGVHD occurred (median time to aGVHD was 14 days). A three-compartment open model was fitted to the individual concentration profiles in blood, simulated thanks to the PBPK model. The kinetic profiles obtained with the three-compartment model were indistinguishable from the profiles generated by the PBPK model. The three-compartment model was coupled with the interface model (described below) and allowed to calculate Cb(t). Substituting the three-compartment model to the PBPK model was necessary for computational reasons, because the software used for subsequent analyses (NONMEM) could not easily handle a PBPK model involving a large system of ordinary differential equations.
Interface Model
In order to test the influence of the concentration profile (II versus CI) on the efficacy of cyclosporin (in terms of aGVHD), an interface model was constructed. This approach was introduced recently (23) for relating the drug concentration profile in the body and the pharmacodynamic (PD) response. This model is a nonlinear-effect compartment model that ensures the required sensitivity of the PD response with respect to drug dose and/or concentration variation. The concentration in the effect compartment, C e , varies according to the following equation:
where C b is the blood cyclosporin concentration calculated using the three-compartment model, C th is the threshold concentration, and H is a categorical variable equal to 1 if C b is greater than C th , and equal to zero otherwise. The parameter α is the elimination rate constant from the effect compartment; it controls the delay between the kinetics of concentration in blood and the kinetics of effect. The parameter β controls the saturation mechanism from the effect compartment. When C th = 0 and β = 0, this model reduces to the usual effect compartment model. A nonlinearity in the transduction process would result in C th or β greater than 0. The average concentration in the effect compartment over the preceding 24 h, C av , was calculated as the 0–24 h AUC of Ce(t), divided by 24. It was taken as a pharmacokinetic index to be related to the probability P of occurrence of aGVHD in a binary logistic regression model:
where a 0 and a 1 are regression parameters to be estimated. The parameter a 0 controls the probability of aGVHD when no drug is given, while a 1 controls the rate of reduction of this probability by cyclosporin concentration unit. Because the estimates of parameters α and a 1 were expected to be highly correlated, the parameter α was fixed to 1 so that at equilibrium, under the null hypothesis C th = 0 and β = 0, the concentrations C e and C b are equal. Hence, the parameters a 0 , a 1 , β, and C th were estimated by nonlinear regression, while the remaining parameters were fixed either to a common value (α = 1) or to their individual estimate (pharmacokinetic parameters). The likelihood ratio test was used to test the hypothesis C th = 0 and β = 0.
Binary Analysis of aGVHD Occurrence
In this analysis, patients were quoted as 0 (no aGVHD) when their Glucksberg’s score was equal to 0, and quoted as 1 otherwise. First, the mean predicted AUC D1 and AUC SS in blood, and interstitial fluid of bone, thymus, and intestines were compared according to the occurrence of aGVHD. In the same way, AUC D1 and AUC SS in blood and skin were compared according to the occurrence of cutaneous aGVHD. Second, the influence of cyclosporin exposure and other covariates on the probabilities of aGVHD and aGVHD in skin was assessed by binary logistic regression with SPSS package (version 17, SPSS, Chicago, Illinois, USA). The covariates considered were AUC, age, body weight, sex, and infusion type. The logit probability of aGVHD was modeled as a linear function of these covariates. Significance of the relationship was assessed by comparing the slope of the linear function to zero by a t-test.
Categorical Analysis of aGVHD Occurrence
In this analysis, the five-grade aGVHD classification of Glucksberg (20–22) was used. In order to visualize the relationship between exposure and aGVHD grades, an exploratory graphical analysis was first performed by plotting the cumulative probabilities of Glucksberg’s grades as a function of cyclosporin AUC tertiles. Second, the mean AUCs in blood and organs by aGVHD grade (grades 0, 1, and ≥ 2) were compared by analysis of variance (ANOVA). Third, the links between cyclosporin exposure and total aGVHD grade or cutaneous aGVHD score were assessed by multinomial logistic regression. The logit of the cumulated probability of having a grade lower than a given value was modeled as a linear or nonlinear (Emax) function of exposure.
The linear model was defined by the following equation:
where A m and B were regression parameters to be estimated. The Emax model was defined by the following equation:
where Emax and AUC 50 represent the maximum effect and the AUC producing 50% of the maximum effect, respectively. γ is the coefficient of sigmoidicity.
No random effect was considered. Parameter estimation was performed using the Laplacian method for likelihood computation in NONMEM (version VI, NONMEM Project Group, University of California, San Francisco, CA). In order to test the model’s ability to predict the probability of observing a grade, qualification of the PD model was based on a visual predictive check. The distribution of predicted probabilities of aGVHD grades (0, 1, or ≥ 2) as a function of AUC SS tertiles in blood and intestines, calculated according to the logistic multinomial model, were compared with the observed probabilities. The distribution of the predicted probabilities was obtained by Monte-Carlo simulation, using the posterior distribution of the regression parameters of the multinomial model. The posterior distribution was assumed normal, with mean equal to the point estimate, and standard deviation equal to the standard error of the estimate.
Statistical and Pharmacokinetic Methods
Statistical analyses, including binary logistic regression, were performed using the SPSS package. Student’s t-test was used to compare means, and the chi-square test was performed to compare proportions, with an alpha risk fixed at 5%. Pharmacokinetic and other non-linear regression analyses were carried out using the program NONMEM. For hypothesis testing during model building, the likelihood ratio test was used in case of nested models, based on the difference between the objective function values of the full and the reduced model, with alpha = 5%. The Akaike’s Information Criterion (AIC) was also calculated for model selection.
RESULTS
Clinical Study
Patient characteristics are summarized in Table I. An episode of aGVHD occurred in 34 patients (56%). In most cases, the disease was limited to skin; digestive and hepatic disease occurred only in approximately 10% of the patients. Therefore, only the grade of GVHD and the score of skin GVHD were considered in the analysis. The mean dose at day 1 was not significantly different in patients, whether aGVHD occurred or not (3.40 ± 0.80 vs. 3.93 ± 1.01 mg/kg, p-value = 0.10).
Interface Model
In the context of the interface model, the average concentration of cyclosporin in the effect compartment was significantly related to the probability of aGVHD occurrence, when C th and β were set to zero (p < 0.001 compared to a model with a 1 = 0). Relaxing each assumption (C th > 0 or β > 0) did not improve the fit; the difference in objective function values was less than 1. Hence, there was no evidence of nonlinearity in the effect compartment (at least those types of nonlinearities), and the transduction (in a broad sense, the link between receptor occupancy and anti-GVHD effect) could be regarded as a linear process. The probability of aGVHD was related to the average concentration, or equivalently, to the AUC over 24 h. Therefore, cyclosporin AUC was retained as a pharmacokinetic index in the pharmacodynamic analysis.
Cyclosporin AUC and Probability of aGVHD
The PBPK model, fitted to the individual data of each child, allowed the estimation of cyclosporin AUCs in blood and in the interstitial fluid of the target organs. At day 1, mean AUCs were significantly different between patients with and without aGVHD, in bone and lymphoid organs (p-value < 0.05), but not in blood. At steady state, mean AUC in the same tissues was significantly greater when there was no aGVHD (p < 0.05 in each case, Table II). Regarding cutaneous aGVHD, at day 1 and at steady state, the mean AUC in skin was significantly lower for patients who suffered cutaneous aGVHD, compared to those with no cutaneous aGVHD (p-value < 0.05). In contrast, no significant difference was found for the mean AUC in blood between these two groups at day 1 (Table II).
These results prompted us to characterize quantitatively the link between the probability of GVHD and cyclosporin exposure. At day 1, no link between blood cyclosporin AUC and the occurrence of aGVHD was found by binary logistic regression (Table III). Conversely, there were significant links between interstitial AUCs in lymphoid organs at the beginning of the treatment (AUC D1) and the occurrence of aGVHD (p-value < 0.05). In the same way, AUC in skin was significantly related to the probability of cutaneous aGVHD (p-value < 0.05). At steady state, there were significant links between AUCs in blood and lymphoid organs and the occurrence of aGVHD (p < 0.01 in each case, Table III).
Sex, body weight, type of donor (related or unrelated), number of cells in the graft, and type of infusion were also tested as covariates. However, no covariate was found to be related to the outcome (data not shown). Cyclosporin infusion duration was not a significant covariate of aGVHD occurrence once AUCs were taken into account. When binary logistic regression took into account both AUC SS and AUC D1, only AUC SS remained a significant covariate (p-value < 0.05, data not shown). A 3D representation of the probability of aGVHD as a function of AUC D1 and AUC SS in intestines, the most influential organ, is shown in Fig. 1. The figure shows that AUC SS variations have a greater influence on aGVHD probability than AUC D1.
Cyclosporin AUC and aGVHD Grade
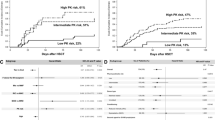
Graphical exploratory analysis revealed that total aGVHD grades and cutaneous aGVHD scores were apparently not related to cyclosporin exposure at day 1. On the contrary, at steady state, high cyclosporin exposure in blood and interstitial fluids seemed to be associated with higher probabilities of low-grade GVHD (Figs. 2 and 3). At the beginning of cyclosporin treatment, for all lymphoid organs but not for the blood, aGVHD grade increased when there was a lower mean AUC D1. At steady state, for blood and lymphoid organs, the same trend was observed, and the difference between the three grades of aGVHD was statistically significant (p < 0.01, Table IV).
Regarding total aGVHD, AUC SS was a more significant covariate than AUC D1 (p-value < 0.01). The Emax model was not significantly better than the linear model. Grade of aGVHD was significantly related to AUC SS in blood and in bone, intestines, and thymus (p < 0.01). According to the criterion of Akaike, the best model was the linear model involving AUC SS in organs, although the difference with the model involving AUC SS in blood was almost as good (AIC = 126.4 vs. 124.2). No other potential covariate exerted a significant influence (data not shown). The parameter values of the best model are summarized in Table V. The predictive check revealed no invalidation of the model (Fig. 4). The probability of aGVHD grades (0, 1, or ≥ 2) as a function of AUC SS in blood, according to the logistic multinomial model, is shown in Fig. 5.
Probability of aGVHD grades (0, 1 or ≥ 2) as a function of AUC SS tertiles in blood (upper panel) and intestine (lower panel), according to the logistic multinomial model. Each box-plot represent the distribution of the predicted probability, obtained by Monte-carlo simulation of the posterior distribution of the regression parameters of the model. The observed probability is represented by the full circle (●).
DISCUSSION
The main objective of this statistical analysis, based on a modeling approach, was to identify the pharmacokinetic index of cyclosporin exposure best correlated with aGVHD severity. The indices commonly considered for cyclosporin include the trough concentration, 2-h concentration, plateau concentration, and AUC. For practical reasons, all these indices are measured in blood. In our study, patients received cyclosporin by CI or II. In this way, a similar average concentration or AUC could be achieved through very different concentration profiles (with different C2 and C12 concentrations). This design, coupled with the analysis by an interface model, allowed us to disentangle the influence of the concentration profile in blood, the hypothetical delay due to cyclosporin diffusion to the receptor, and hypothetical nonlinearity in the transduction process.
We found that average concentration was the pharmacokinetic index related to the anti-GVHD effect, irrespective of the concentration profile. As a consequence, administration of cyclosporin by II or CI may have equal efficacies, provided that the average blood concentration achieved is similar. The higher AUC of receptor occupancy in the interstitial fluid of aGVHD target organs yielded by CI, compared to II in our previous study (9), does not result in increased efficacy, probably because the difference in receptor occupancy is too small. As AUC is equal to the product of average concentration and dosing interval, AUC 0–24 h may also be used as a predictor of efficacy.
AUC D1 and AUC SS were both related to anti-GVHD efficacy in univariate analysis, but AUC D1 was no longer a predictor once AUC SS was taken into account in a multivariate analysis. This result may be explained by the high correlation between AUC D1 and AUC SS; it does not imply that the early achievement of adequate AUC is not important for prevention of aGVHD.
Cyclosporin AUC in interstitial fluid of lymphoid organs was a more significant index than that in blood, but only marginally, because AUCs in blood and interstitial fluids were correlated (data not shown). As a consequence, considering interstitial AUCs is not a beneficial strategy, and target AUCs in blood may be defined. Two cases should be considered.
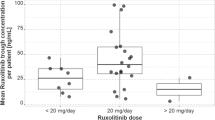
In the case of malignant disease, a grade 1 GVHD is desired for its anti-leukemia effect (24). A target AUC of approximately 10 h.mg/l may be chosen in order to maximize the probability of grade 1, but minimize the probability of grade ≥ 2 (Fig. 5). This target AUC is equivalent to an average cyclosporin concentration of 420 μg/l. According to our pharmacokinetic model, under 2-h intermittent infusion, the corresponding values for C2 and C12 are 1,000 μg/l and 80 μg/l, respectively. These predictions agree with the target concentrations used in several studies: plateau concentration of 450 to 520 μg/l (25), 150 to 400 μg/l (26), 250 to 400 μg/l (27), C2 observed by Hendriks (28) or Barkholt (16) and C12 observed by Martin (4). The agreement of our prediction with target values considered as relevant on clinical grounds is strongly supportive of our model. As a result, the model may be used to explore in silico, by simulation, the efficacy of different dosing strategies.
On the other hand, in the case of non-malignant disease, a grade 0 GVHD is desired. The target exposure is therefore different. An AUC of approximately 16 h.mg/l is associated with the absence of GVHD with a probability of 80% (Fig. 5). This value is equivalent to a plateau concentration of 660 μg/l, a C2 of 1,600 μg/l, and a C12 of 120 μg/l.
CONCLUSION
In HSCT, the best pharmacokinetic index relating the anti-GVHD effect to cyclosporin exposure was its average concentration or, equivalently, its AUC. This finding is an indirect argument for equal efficacies of CI and II. Cyclosporin AUC in interstitial fluid of lymphoid organs was a better index than in blood, but only marginally. Because AUCs are much more easily measured in blood than in interstitial fluids, AUC in blood may be used as an index of cyclosporin efficacy. We employed a logistic model and a PBPK model to define target AUCs in blood, as well as the equivalent target values for C2 and C12 concentrations. These results may help to better design clinical studies aimed at comparing dosing strategies, rates of infusion and/or targets for therapeutic drug monitoring.
REFERENCES
Ferrara JL, Levine JE, Reddy P, Holler E. Graft-versus-host disease. Lancet. 2009;373:1550–61.
Appelbaum FR. Haematopoietic cell transplantation as immunotherapy. Nature. 2001;411:385–9.
Bowers LD. Therapeutic monitoring for cyclosporine: difficulties in establishing a therapeutic window. Clin Biochem. 1991;24:81–7.
Martin P, Bleyzac N, Souillet G, Galambrun C, Bertrand Y, Maire PH, et al. Relationship between CsA trough blood concentration and severity of acute graft-versus-host disease after paediatric stem cell transplantation from matched-sibling or unrelated donors. Bone Marrow Transplant. 2003;32:777–84.
Byrne JL, Stainer C, Hyde H, Miflin G, Haynes AP, Bessell EM, et al. Low incidence of acute graft-versus-host disease and recurrent leukaemia in patients undergoing allogeneic haemopoietic stem cell transplantation from sibling donors with methotrexate and dose-monitored cyclosporin A prophylaxis. Bone Marrow Transplant. 1998;22:541–5.
Carlens S, Aschan J, Remberger M, Dilber M, Ringden O. Low-dose cyclosporine of short duration increases the risk of mild and moderate GVHD and reduces the risk of relapse in HLA-identical sibling marrow transplant recipients with leukaemia. Bone Marrow Transplant. 1999;24:629–35.
Cahn JY, Klein JP, Lee SJ, Milpied N, Blaise D, Antin JH, et al. Prospective evaluation of 2 acute graft-versus-host (GVHD) grading systems: a joint Societe Francaise de Greffe de Moelle et Therapie Cellulaire (SFGM-TC), Dana Farber Cancer Institute (DFCI), and International Bone Marrow Transplant Registry (IBMTR) prospective study. Blood. 2005;106:1495–500.
Ruutu T, Niederwieser D, Gratwohl A, Apperley JF. A survey of the prophylaxis and treatment of acute GVHD in Europe: a report of the European Group for Blood and Marrow, Transplantation (EBMT). Chronic Leukaemia Working Party of the EBMT. Bone Marrow Transplant. 1997;19:759–64.
Gerard C, Bleyzac N, Girard P, Freyer G, Bertrand Y, Tod M. Influence of dosing schedule on organ exposure to cyclosporin in pediatric hematopoietic stem cell transplantation: analysis with a PBPK-PD model. Pharm Res. 2010. doi:10.1007/s11095-010-0252-1.
Morris RG, Russ GR, Cervelli MJ, Juneja R, McDonald SP, Mathew TH. Comparison of trough, 2-hour, and limited AUC blood sampling for monitoring cyclosporin (Neoral) at day 7 post-renal transplantation and incidence of rejection in the first month. Ther Drug Monit. 2002;24:479–86.
Pescovitzand MD, Barbeito R. Two-hour post-dose cyclosporine level is a better predictor than trough level of acute rejection of renal allografts. Clin Transplant. 2002;16:378–82.
Caforio AL, Tona F, Piaserico S, Gambino A, Feltrin G, Fortina AB, et al. C2 is superior to C0 as predictor of renal toxicity and rejection risk profile in stable heart transplant recipients. Transpl Int. 2005;18:116–24.
Li J, Dahmen U, Beckebaum S, Cicinnati V, Valentin-Gamazo C, Frilling A, et al. Target range maximum of cyclosporine blood concentration two hours post dose in stable liver transplant patients. Eur J Med Res. 2006;11:139–45.
Rodrigo E, Ruiz JC, Angeles de Cos M, Ruiz J, Gago M, Pinera C, et al. Correlation of C0 and C2 levels with cyclosporine side effects in kidney transplantation. Transplant Proc. 2009;41:2328–31.
Troncoso P, Ortiz AM, Jara A, Vilches S. Abbreviated AUC monitoring of cyclosporine more adequately identified patients at risk for acute rejection during induction of immunosuppressive therapy after kidney transplantation than recommended C2 concentration values. Transplant Proc. 2009;41:127–30.
Barkholt L, Remberger M, Bodegard H, Ringden O, Bottiger Y. Cyclosporine A (CsA) 2-h concentrations vary between patients without correlation to graft-versus-host disease after allogeneic haematopoietic stem cell transplantation. Bone Marrow Transplant. 2007;40:683–9.
Punnett A, Sung L, Price V, Das P, Diezi M, Doyle J, et al. Achievement of target cyclosporine concentrations as a predictor of severe acute graft versus host disease in children undergoing hematopoietic stem cell transplantation and receiving cyclosporine and methotrexate prophylaxis. Ther Drug Monit. 2007;29:750–7.
Sibbald C, Seto W, Taylor T, Saunders EF, Doyle J, Dupuis LL. Determination of area under the whole blood concentration versus time curve after first intravenous cyclosporine dose in children undergoing hematopoietic stem cell transplant: limited sampling strategies. Ther Drug Monit. 2008;30:434–8.
Martin P, Bleyzac N, Souillet G, Galambrun C, Bertrand Y, Maire PH, et al. Clinical and pharmacological risk factors for acute graft-versus-host disease after paediatric bone marrow transplantation from matched-sibling or unrelated donors. Bone Marrow Transplant. 2003;32:881–7.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304.
Armitage JO. Bone marrow transplantation. N Engl J Med. 1994;330:827–38.
Michallet M, Dhedin N, Michallet AS. Allogeneic hematopoietic stem-cell transplantation for hematological malignancies. Bull Cancer. 2001;88:908–26.
Meille C, Iliadis A, Barbolosi D, Frances N, Freyer G. An interface model for dosage adjustment connects hematotoxicity to pharmacokinetics. J Pharmacokinet Pharmacodyn. 2008;35:619–33.
Neudorf S, Sanders J, Kobrinsky N, Alonzo TA, Buxton AB, Gold S, et al. Allogeneic bone marrow transplantation for children with acute myelocytic leukemia in first remission demonstrates a role for graft versus leukemia in the maintenance of disease-free survival. Blood. 2004;103:3655–61.
Miller KB, Schenkein DP, Comenzo R, Erban JK, Fogaren T, Hirsch CA, et al. Adjusted-dose continuous-infusion cyclosporin A to prevent graft-versus-host disease following allogeneic bone marrow transplantation. Ann Hematol. 1994;68:15–20.
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96:2062–8.
Ogawa N, Kanda Y, Matsubara M, Asano Y, Nakagawa M, Sakata-Yanagimoto M, et al. Increased incidence of acute graft-versus-host disease with the continuous infusion of cyclosporine A compared to twice-daily infusion. Bone Marrow Transplant. 2004;33:549–52.
Hendriks MP, Blijlevens NM, Schattenberg AV, Burger DM, Donnelly JP. Cyclosporine short infusion and C2 monitoring in haematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2006;38:521–5.
ACKNOWLEDGMENTS
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gérard, C., Bleyzac, N., Girard, P. et al. Links Between Cyclosporin Exposure in Tissues and Graft-Versus-Host Disease in Pediatric Bone Marrow Transplantation: Analysis by a PBPK Model. Pharm Res 28, 531–539 (2011). https://doi.org/10.1007/s11095-010-0299-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0299-z