ABSTRACT
Purpose
To quantify distribution of albuterol aerosol generated by a pneumatic nebulizer within the nose and lungs of a model of a 9-month-old child (SAINT) and aerosol loss to the environment, during simulated breathing at increasing tidal volumes (TVs).
Methods
99mtechnetium-labeled albuterol aerosol was generated by an IPI nebulizer with face-mask. Deposition was quantified as a percentage of emitted dose using gamma scintigraphy.
Results
Lung deposition was similar for all TVs, averaging 7.17 ± 0.01%, 9.34 ± 0.01% and 9.41 ± 0.02% at 50, 100 and 200 mL TV, respectively. In contrast, nose deposition increased significantly with TV, averaging 4.40 ± 0.02%, 11.39 ± 0.02% and 22.12 ± 0.02% at 50 mL, 100 mL and 200 mL TV, respectively (all p < 0.0167). Aerosol loss to the environment was significantly lower at 200 mL TV (53.81 ± 0.04%), compared to 50 mL (71.99 ± 0.02%) (p < 0.0167).
Conclusions
Our results suggest that nasal deposition of albuterol aerosol generated by a pneumatic nebulizer in 9-month-old infants may be significantly affected by changes in TV, ranging between 50 to 200 mL, whereas total lung deposition may not be affected. These results also predict that environmental losses would be highest when administering to a child breathing at 50 mL TV. These data should be useful to companies who are working to improve aerosol delivery systems to treat infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Nebulizers convert solutions and suspensions into small droplets that can be readily inhaled. The advantage to using nebulizers includes their ability to aerosolize high doses of drugs that are not available in dry powder inhalers (DPIs), or pressurized metered-dose inhalers (pMDIs). In addition, most nebulizers come with face-masks and can be used by patients less than 2 years old. When infants are treated with nebulizers, they frequently breathe through their noses using a face-mask.
Pneumatic or jet nebulizers use compressed gas flow to entrain liquid from a reservoir and break the liquid into small droplets by means of baffles. The particle size distribution of the aerosol leaving the device is determined by the design of the baffle and the flow through the device. These nebulizers are relatively inefficient, compared to newer devices.
Despite their inefficiency, pneumatic nebulizers are still widely used, especially in the hospital emergency room. Infants and toddlers who are experiencing shortness of breath, or bronchospasm, and come to the emergency room are often treated with the bronchodilator albuterol, which is generated as an aerosol by a pneumatic nebulizer and inhaled during continuous breathing using a face-mask. Nevertheless, little is known about the behavior of this aerosol in infant airways because ethical concerns make studies of deposition in infants and children using radiolabeled aerosols nearly impossible to perform. This lack of knowledge limits our understanding of the distribution of albuterol aerosol in particular, and liquid aerosols in general, within the upper and lower airways of this population and how the distribution could be altered to optimize deposition.
In vitro data regarding aerosol deposition is often obtained using inhalation flow rates that are typical for adults, who inhale aerosolized medications in a single breath. However, infants and young children inhale aerosolized medications during several breaths via tidal breathing. To accommodate this difference, some in vitro studies have incorporated pediatric tidal breathing into their experimental design and collected the emitted dose from the aerosol generator on a filter or in an impactor (1–5). This approach provides information about the amount of aerosol that is delivered to the mouth or nose, but tells us nothing about the distribution of the aerosol between the upper and lower airways. In addition, it is well known that infants breathe at different tidal volumes depending on their level of activity (6,7). However, little is known about how alterations in tidal volume affect deposition of a liquid aerosol in the nasal cavity and lungs of infants and young children.
Finally, it is unknown how much aerosol that is generated during typical nebulization is lost to the surrounding environment during administration. This information would be useful in designing delivery systems that minimize waste of the drug to the environment and reduce the care-giver’s exposure.
Since we could not address these issues in vivo, we designed a series of experiments that could answer these questions in a model of infant airways. The aim of this study was to quantify deposition of a liquid aerosol, generated by a pneumatic nebulizer with face-mask, during simulated breathing at 50, 100 and 200 mL tidal volumes in the nasal cavity and lower airways of an anatomically correct airway model of a 9-month-old infant. The amount of aerosol that was lost to the delivery system and the environment surrounding the model was also quantified.
MATERIALS AND METHODS
Aerosol Generation
Albuterol aerosol was generated by an IPI nebulizer (IPI Medical Products, Inc., Chicago, IL) that was connected to a 3/4 HP air compressor (Thomas Model 1020; Sheboygan, WI). Airflow from the compressor to the nebulizer was regulated at 10.5 L/min. Aerosol was delivered through a corrugated tube that was 15 cm long, plus a plastic funnel-shaped face-mask. The nebulizer volume consisted of 9.75 mL of chilled albuterol (0.625 mg/ml) plus 0.25 mL of the gamma-emitting radioisotope 99mtechnetium (Cardinal Health, Dublin, OH).
We chose albuterol for nebulization in these experiments for the reasons discussed above. We chose the IPI nebulizer for these experiments because it is representative of the many pneumatic nebulizers available for liquid aerosol delivery in the hospital emergency department. The facemask was chosen as a generic version of face-masks that are available. The face-mask was placed lightly against the face, but was not sealed to the face.
Model of Infant Airways
We quantified deposition of the aerosol in four copies of the Sophia Anatomical Infant Nose-Throat (SAINT) model during simulated breathing at tidal volume. The SAINT model was reproduced from CT scans of the upper airways of a 9-month-old baby as reported previously by Janssens and colleagues (8). The lips, nasal cavity, nasopharynx and larynx are included in the model, but there is no oral passage, since 9-month-old babies are typically obligate nose breathers. Sinuses are not developed in the 9-month-old infant and are not included in the model. Our experimental set-up is shown in Fig. 1.
Delivery of the Aerosol
Aerosol was delivered continuously over a 30-second period to each copy of the SAINT model during tidal breathing. Parafilm covered the exhalation port of the nebulizer, so there would be no losses of radioactivity during the exhalation period.
Inhalation began at the same time as generation of the aerosol. The funnel-shaped face-mask was held against the face of the model, surrounding the nose and mouth, but the seal was not airtight. The model was surrounded with a plastic bag to capture aerosol that escaped into the environment. Losses in the bag represented possible exposure to the caregiver. Aerosol that passed through the model was captured on a filter. Radioactivity detected on the filter represented activity from droplets that could deposit in the lungs.
No attempt was made to coat the airways of the model for several reasons. First, we were uncertain as to what compound(s) was/were suitable to use to mimic naturally occurring mucus in the nasal cavity. To date, there is no agreed-upon formula. Second, we were concerned that application of any mucus substitute might not be homogeneous and could be thick in some areas of the nasal cavity and thin in others, and this could affect aerosol deposition in ways that are not representative of the natural mucous distribution. We were also concerned that the application would not be reproducible between model copies. Other investigators clearly share these concerns and have performed studies of aerosol deposition in nasal cast models without coating the airways (9,10).
Tidal Volume Breathing
A computer-operated breathing simulator (PARI Breath Simulator, PARI GmbH, Starnberg, Germany) controlled inhalations and exhalations through the model at pre-set times and tidal volumes. Respiratory rate was set at 15 breaths/30 seconds. The duration of inhalation was set at 0.9 sec. The duration of exhalation was 1.1 sec. The respiratory duty cycle (inspiratory time/total respiratory cycle time) was 0.45. Tidal volumes included 50 mL, 100 mL and 200 mL. Each of the four model copies was tested at all three tidal volumes for a total of 12 runs.
We chose these tidal volumes and respiratory rate based on results reported in a study by Janssens and colleagues (11), who recorded the breathing patterns of 18 children during sleep and while awake. Children had a mean age of 11 ± 5.1 months. During sleep, respiratory rate averaged 32 breaths/min and ranged between 22 and 53 breaths/min. Tidal volume averaged 97 mL and ranged between 39 and 138 mL. When awake, respiratory rate averaged 49 breaths/min and ranged between 33 and 83 breaths/min. Tidal volume averaged 83 mL and ranged between 20 and 141 mL. Tidal volumes of 50 mL and 100 mL and a respiratory rate of 15 breaths/30 seconds are well within the range of actual values measured in these infants. In addition, tidal volumes are usually expressed as 8–10 mL per kg weight. Since the 9-month-old baby that the SAINT model was based upon was 10 kg, the tidal volume for this baby would be 80–100 mL. A tidal volume of 200 mL was included as an upper range comparison.
Quantification of Emitted Dose
The emitted dose from the IPI nebulizer was quantified by measuring the number of microcuries of technetium that exited the outport of the T-connector of the IPI nebulizer during 30 seconds of continuous nebulization. Radioactivity was captured on an absolute filter attached to the outport of the nebulizer and was quantified in a deposition calibrator (Capintec, Inc., Ramsey, NJ). Parafilm covered the exhalation port of the nebulizer, so no radioactivity was lost during the exhalation period.
Quantification of Aerosol Deposition
Deposition of the aerosol was quantified on the filter, which represented lung deposition, within the nasal cavity of the model, on the model face and in the tube/face-mask by a large-field-of-view gamma camera (ZLC, Siemens, Gammasonics, Des Plains, IL). The dose calibrator was used to quantify aerosol that deposited within the bag, which represented exposure to the surrounding environment and caregiver. Each of the gamma camera images was acquired over a 7-minute period and was analyzed with a Sopha computer (SMV, Twinsburg, OH). Counts detected within the various regions of interest were converted to microcuries using a camera sensitivity factor. Microcuries within each region were expressed as a percentage of the emitted deposition (i.e. microcuries of technetium emitted from the nebulizer).
Deposition within the nasal cavity was quantified by analyzing the gamma camera images as follows. A small volume of saline admixed with 99mtechnetium was poured into each model on a day that was different from the experimental day. The model was then turned upside down and sideways to encourage circulation of the liquid throughout the nasal cavity. Then, the model was imaged with the gamma camera. This process outlined the borders of the nasal cavity, and the image became the reference image.
Aerosol deposition within the nasal cavity was quantified as both total deposition and regional deposition. Total deposition was determined by superimposing the reference image for a given model on the aerosol image for that model and quantifying the number of counts detected within the reference border of the aerosol image. Counts were converted to microcuries using a camera sensitivity value. In this way, we ensured that we would be analyzing the same nasal cavity field for each image obtained for each copy of the model at the different TVs.
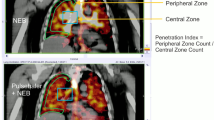
Regional deposition within the nasal cavity was quantified by dividing the width of the reference image into three vertical regions. These three regions were then superimposed onto the radioaerosol image as shown in Fig. 2. Regional deposition was quantified in terms of radioactivity deposited in inner and outer zones of the nasal cavity. We developed a similar method of analysis for quantifying aerosol distribution within human lungs (12,13). Mean counts per picture element in the inner and outer regions of the radioaerosol scan were calculated, and an inner:outer zone (I:O) ratio was derived. The outer zone was selected such that it represented the most anterior third of the nasal cavity, whereas the inner region represented the most posterior third.
Method for quantifying total and regional aerosol deposition in the nasal cavity of the model. Total deposition was determined by superimposing the reference image for a given model on the aerosol image for that model and quantifying the number of counts detected within the reference border of the aerosol image. Regional deposition was quantified by dividing the width of the reference image into three vertical regions. These three regions were then superimposed onto the radioaerosol image. Regional deposition was quantified in terms of radioactivity deposited in inner and outer zones of the nasal cavity.
Aerosol Particle Size Measurements
We quantified the particle size distribution of 99mtechnetium-albuterol aerosol generated by two IPI nebulizers and a 3/4 HP air compressor (Sears Craftsman Compact Model 919.150270) using a laser diffraction system (Sympatec Helos; Sympatec GmbH, Clausthal-Zellerfeld, Germany). A different compressor was used for the particle-sizing experiments, because they occurred at a site that was different from where the deposition studies were performed, and the Thomas compressor was not available at the second site. There is no reason to think the change in compressor-affected particle size, since both the Sears and Thomas air compressors had the same nominal horsepower and equivalent performance specifications for air delivery output (L/min) vs. pressure (psig), as stated by their respective manufacturers. During experiments at both sites, airflow from the compressor to the IPA nebulizer was regulated at 10.5 L/min. The test liquid was 10 ml of chilled albuterol (0.625 mg/ml) solution with decayed 99mtechnetium.
An R1 lens measured particles in the range of 0.1 to 35 µm. The software was Windox 5.2.2. The nebulizer output was positioned perpendicular to and approximately 5" in front of the laser detection lens. The flow rate to the nebulizer was verified at 10.5 L/min. The Sympatec data recording was started, and it was verified that the laser was sampling the aerosol cloud. Nebulizer #1 was tested this way 19 times, and nebulizer #2 was tested 30 times.
Data Analysis
Data are presented as mean ± standard deviation for the four runs at each of three TVs. Paired t-tests were performed to test for differences in distribution of the aerosol in the various regions of interest during the three tidal breathing conditions. These included the filter (lung deposition), within the nasal cavity of the model, on the face, in the tube/face-mask and in the bag. This same approach was used to compare deposition within the nasal cavity in terms of I:O ratio at the three tidal volumes. Since there were three comparisons for each region of interest, we corrected the significance level to account for the multiple comparisons. P-values ≤ 0.0167 (i.e. 0.05/3) indicated a statistically significant difference between comparisons.
RESULTS
Particle Size of Chilled 99mTechnetium-Albuterol
The average mass median diameter (MMD) for multiple measurements of the chilled 99mtechnetium-albuterol was 4.65 µm for nebulizer #1 and 4.91 µm for nebulizer #2. The mean MMD for the two nebulizers was 4.78 ± 0.18 µm.
I:O Ratios in Nasal Cavity
I:O ratios varied with changes in tidal volume but were not statistically different. I:O ratio averaged 1.46 ± 0.38, 0.71 ± 0.26 and 0.79 ± 0.26, at 50, 100 and 200 mL TV, respectively. These data indicate that distribution of the aerosol within the nasal cavity of the models did not change significantly over this range of tidal volumes.
Summary of Aerosol Deposition for All Sites
Mean percent deposition of 99mtechnetium on the filter (lung deposition), in the nasal cavity, tube/face-mask, bag (environment) and on the model face for all of the four models at the three tidal volumes are summarized in Table I. Data are expressed as a percentage of the emitted dose. Average total deposition approximated 100% at each tidal volume condition, indicating that the emitted dose was accounted for as either deposited within the model, deposited on or within the components of the delivery device, or as lost to the surrounding environment.
Lung Deposition
Fig. 3 shows average deposition of aerosol on the filter (lung deposition) at the three tidal volumes. Total lung deposition averaged 7.17 ± 0.01%, 9.34 ± 0.01% and 9.41 ± 0.02% at 50, 100 and 200 mL TV, respectively. These values were not statistically different.
Nasal Cavity Deposition
Fig. 4 shows average deposition of aerosol in the nasal cavity at the three tidal volumes. Nasal cavity deposition increased significantly with increasing TV, averaging 4.40 ± 0.02% at 50 mL, 11.39 ± 0.02% at 100 mL and 22.12 ± 0.02% at 200 mL TV (all p < 0.0167).
Loss of Aerosol in Tube/Face-Mask
Fig. 5 shows the average loss of aerosol within the tube/face-mask at the three tidal volumes. Losses within the tube/face-mask were similar at all TV, averaging 11.42 ± 0.01%, 11.27 ± 0.01% and 13.58 ± 0.03% at 50, 100 and 200 mL TV, respectively.
Loss of Aerosol to the Environment
Fig. 6 shows the average loss of aerosol to the environment (i.e. activity measured in the bag) at the three tidal volumes. Losses to the environment were similar at 50 and 100 mL TV, averaging 71.99 ± 0.02% and 63.84 ± 0.05%, respectively. However, losses at 200 mL TV (53.81 ± 0.04%) were significantly reduced compared to 50 mL TV (71.99 ± 0.02%) (p < 0.0167).
Deposition on the Face
The average deposition of aerosol on the face was significantly less at 50 mL TV (0.08 ± 0.00%) compared to 100 mL TV (0.80 ± 0.00%) (p < 0.0167). Deposition on the face was not different at 100 mL and 200 mL TV (0.37 ± 0.01%), or for 50 mL, compared to 200 mL TV.
DISCUSSION
We quantified deposition of albuterol aerosol, generated by an IPI nebulizer with face-mask, in the nasal cavity and lower airways of four copies of an anatomically correct airway model of a 9-month-old infant (SAINT). As part of these studies, we also examined the effect of alterations in tidal volume on aerosol deposition in the infant model and quantified loss of the aerosol to the delivery system and the environment surrounding the model. Total lung deposition was similar for all TVs, averaging 7.17 ± 0.01%, 9.34 ± 0.01% and 9.41 ± 0.02% at 50, 100 and 200 mL TV, respectively. In contrast, nose deposition increased significantly with TV, averaging 4.40 ± 0.02%, 11.39 ± 0.02% and 22.12 ± 0.02% at 50 mL, 100 mL and 200 mL TV, respectively (all p < 0.0167). Aerosol loss to the environment was significantly lower at 200 mL TV (53.81 ± 0.04%), compared to 50 mL (71.99 ± 0.02%) (p < 0.0167).
We believe that deposition of the 99mtechnetium-albuterol aerosol in the SAINT model reflects deposition in the in vivo condition. This is because Janssens and colleagues have shown that the upper airway dimensions on the CT scan of the SAINT model closely match those of the CT scan of the infant upon which the model was based (8). They also showed that airway resistance of the upper airways of the model is within the physiological range (8).
The respiratory duty cycle (inspiratory time/total respiratory cycle time) of 0.45, tidal volume of 100 mL and respiratory rate of 15 breaths/30 seconds were also in accordance with reference values appropriate for the 9-month-old subject used to construct the SAINT model (14). Because it is known that young children have variable breathing patterns (7), we included a lower (50 mL) and higher (200 mL) TV to bracket the range.
Janssens et al. (8) previously quantified lung deposition of budesonide aerosol generated by pMDI (Pulmicort® 200 µg, Astrazeneca, Zoetermeer, The Netherlands) and delivered by the Nebuchamber® holding chamber (AstraZeneca, Lund, Sweden) in the SAINT model at tidal volumes that was equivalent to ours. They present their data as percent of nominal dose. However, since aerosol was generated by a pMDI, the emitted dose and nominal dose should not be significantly different. In their study, they used a sealed face-mask protocol, and a mucus substitute was introduced into the nasal cavity. At 50 mL TV, lung deposition as a percent of nominal dose was 13.9%, and this decreased significantly to 8.8% at 100 mL TV and to 3.2% at 200 mL TV. They did not quantify nasal deposition in that study.
Our lung deposition is close to that observed in Janssens’s study for 50 and 100 mL TV, with 7.17 ± 0.01% and 9.34 ± 0.01%, respectively. However, we did not see a significant decrease in deposition at 100 mL, or 200 mL TV, compared to deposition at 50 mL, as reported by Janssens and colleagues with the budesonide aerosol (8). Lung deposition at 200 mL TV was 9.41 ± 0.022%, which was no different than deposition quantified at 50 or 100 mL TV.
In a second study by Janssens et al. (11), they repeated their quantification of lung deposition at different tidal volumes in the SAINT model with other pMDI drug formulations and holding chambers, using the sealed face-mask protocol. Their results showed an overall decrease in lung deposition at increasing TV. As part of that study, they quantified nasal deposition for the different formulations and chambers and found that overall nasal deposition increased with increasing TV. Nasal deposition varied between spacer devices and drug formulations, but ranged from approximately 1% to 25% at 50 mL TV, from approximately 5% to 30% at 100 mL TV and from approximately 15% to 40% at 200 mL TV. We observed the same relationship between nasal cavity deposition and increasing TV in our study. Nasal cavity deposition increased significantly from 50 to 200 mL TV, averaging 4.40 ± 0.02% at 50 mL, 11.39 ± 0.02% at 100 mL and 22.12 ± 0.02% at 200 mL TV (all p < 0.0167). These values fall within the range reported by Janssens et al. for drug delivery with a pMDI (11). Although nasal deposition increased with increasing TV in our study, it appears that more aerosol penetrated beyond the nasal cavity to the lung filter than in the Janssens study.
Our study and the two studies of Janssens and colleagues differed in terms of aerosol formulation, the use of a small volume holding chamber versus a corrugated tube, a loosely fitting face-mask versus a tightly sealed face-mask, the use or non-use of a mucus substitute, and continuous aerosol delivery by nebulizer versus single actuations from a pMDI into the holding chamber. All of these factors could have contributed to the observed differences in lung deposition for the two studies.
In general, loss of aerosol to the environment surrounding the SAINT models was high, suggesting a caregiver would be exposed to significant amounts of aerosol at all tidal volumes with this delivery system. However, aerosol loss was greatest at 50 mL TV, averaging 72%, whereas the loss was significantly less at 200 mL TV, averaging 53%. These data suggest that exposure to a caregiver with this delivery system would be greatest when administering to children who are breathing at low tidal volumes. These losses are probably similar to the in vivo condition, with the caregiver holding the funnel-shaped face-mask lightly against the face of the infant and aerosol escaping past the face of the child.
There are few in vivo studies with which to compare our findings, and the design or patient population for those studies differ significantly from our own. Nevertheless, we have compared our data with those reported by Chua et al. (15) and Wildhaber et al. (16). In experiments reported by Chua et al. (15), 12 infants who were 0.3–1.4 years old inhaled normal saline admixed with 99mtechnetium bound to diethylene pentaacetic acid (DTPA). Aerosol was generated by a Turret nebulizer (Medic-Aid LTD, UK) (MMAD = 2.3 μm) into a face-mask with a good seal. The authors reported that lung deposition averaged only 1% of the emitted dose from the nebulizer.
There are a number of differences between the two studies that could account for the lower lung deposition percentage reported by Chua et al. First, infants were sedated and may have been breathing at tidal volumes below 50 mL. This could have resulted in a significant reduction in lung deposition compared to our study where TV was 50 mL, or above. In addition, infants were diagnosed with cystic fibrosis, and, although not reported, it is likely that they had nasal infections and increased mucus production. The presence of large amounts of mucus would probably decrease delivery of aerosol beyond the nasal cavity. As mentioned earlier, we did not coat the models with a mucus substitute. Clearly, we quantified deposition in the SAINT model under ideal circumstances. More studies are needed to determine how deposition within the model varies with simulations of nasal infections.
Our lung deposition data is closer to what has been reported by Wildhaber et al. (16). In that study, the authors radiolabeled salbutamol and delivered it to 9 children who were 2–4 years old. The aerosol was generated by a Pari Baby nebulizer (PARI GmbH, Starnberg, Germany), driven by a Pari Proneb Turbo compressor, and was inhaled through a face-mask while breathing tidally for 5 minutes. The authors report that 5.4% of the nominal dose deposited in the lungs. Because they accounted for the total amount of radioactivity that was either deposited, or remained in the nebulizer, it is possible to calculate deposition in the lungs in terms of emitted dose. That calculation indicates that 14.5% of the emitted dose deposited in the lungs of the children under the reported breathing conditions. This deposition to the lung is somewhat higher than what we observed. However, the difference may be due to the fact that these children were older than the infant represented by our model and could breathe through their mouths. The particle size was also significantly smaller (MMAD = 3.21 µm), compared to the current study (MMD = 4.78 µm), and this may have resulted in higher deposition in the lungs.
CONCLUSION
Results from this study show how albuterol aerosol that is generated by the IPI nebulizer is distributed between the nasal and lower airways of an infant model under simulated breathing conditions and increasing TVs. These data indicate that deposition of nebulized albuterol aerosol in the nasal cavity of the infant model is significantly altered by changes in TV, ranging between 50 to 200 mL. This is similar to what has been reported with aerosol delivered by pMDI through a spacer to the same infant model. These results suggest that aerosol deposition in the 9-month-old infant nose may not be significantly affected by changes in formulation or type of delivery, but may be significantly affected by changes in tidal volume. In contrast, deposition to the lower airways of the model was unaffected by changes in TV when albuterol aerosol was administered during continuous delivery with the IPI nebulizer and face-mask in the current study. This differs from what has been reported for aerosol delivered by pMDI through a spacer to the same infant model, suggesting that aerosol delivery to the lower airways of these infants may vary with formulation and delivery system. Since it is very difficult, if not impossible, to conduct these studies in children, experiments such as these provide important information about the distribution of aerosolized medications between the upper and lower airways of infants and what factors alter that distribution. These data should be useful to companies who are working to improve aerosol delivery systems to treat infants.
REFERENCES
Berg E, Madsen J, Bisgaard H. In vitro performance of three combinations of spacers and pressurized metered dose inhalers for treatment in children. Eur Respir J. 1998;12:472–6.
Everard ML, Clark AR, Milner AD. Drug delivery from holding chambers with attached facemask. Arch Dis Child. 1992;67:580–5.
Finlay WH, Zuberbuhler P. In vitro comparison of beclomethasone and salbutamol metered dose inhaler aerosols inhaled during pediatric tidal breathing from four valved holding chambers. Chest. 1998;114:1676–80.
Mitchell JP, Nagel MW. In vitro performance testing of three small volume-holding chambers under conditions that correspond with use by infants and small children. J Aerosol Med. 1997;10:341–9.
Barry PW, O’Callaghan C. The output of budesonide from spacer devices assessed under simulated breathing conditions. J Allergy Clin Immunol. 1999;104:1205–10.
Janssens HM, Van der Wiel EC, Verbraak AFM, de Jongste JC, Merkus PJFM, Tiddens HAWM. Aerosol therapy and the fighting toddler: Is administration during sleep an alternative? J Aerosol Med. 2003;16:395–400.
Bisgaard H. Patient-related factors in nebulized drug delivery to children. Eur Respir Rev. 1997;7:376–7.
Janssens HM, de Jongste JC, Fokkens WJ, Robben SGF, Wouters K, Tiddens HAWM. The Sophia Anatomical Infant Nose-Throat (SAINT) Model: A valuable tool to study aerosol deposition in infants. J Aerosol Med. 2001;14:433–41.
Minocchieri S, Burren JM, Bachmann MA, Stern G, Wildhaber J, Buob S, et al. Development of the premature infant nose throat-model (PrINT-Model)- an upper airway replica of a premature neonate for the study of aerosol delivery. Pediatr Res. 2008;64:141–6.
Foo MY. Y-S. Cheng, W-C. Su and M.D. Donovan. The influence of spray properties on intranasal deposition. J Aerosol Med. 2007;20:495–508.
Janssens HM, Krijgsman A, Verbraak TFM, Hop WCJ, de Jongste JC, Tiddens HAWM. Determining factors of aerosol deposition for four pMDI-spacer combinations in an infant upper airway model. J Aerosol Med. 2004;17:51–61.
Laube BL, Edwards AM, Dalby RN, Creticos PS, Norman PS. The efficacy of slow versus faster inhalation of cromolyn sodium in protecting against allergen challenge in patients with asthma. J Allergy Clin Immunol. 1998;101:475–83.
Laube BL, Benedict GW, Dobs AS. Time to peak insulin level, relative bioavailability and effect of site of deposition of nebulized insulin in patients with non-insulin dependent diabetes mellitus. J Aerosol Med. 1998;11:153–73.
Stick S. Measurements during tidal breathing. In: Sly P, Tepper R, Morgan W, editors. Infant respiratory function testing. New York: Wiley-Liss; 1996. p. 134.
Chua HL, Collis GG, Newbury AM, Chan K, Bower GD, Sly PD, et al. The influence of age on aerosol deposition in children with cystic fibrosis. Eur Respir J. 1994;7:2185–91.
Wildhaber JH, Dore ND, Wilson JM, Devadason SG, Le Souef PN. Inhalation therapy in asthma: nebulizer or pressurized metered-deposition inhaler with holding chamber? In vivo comparison of lung deposition in children. J Pediatr. 1999;135:28–33.
ACKNOWLEDGEMENTS
The authors wish to thank Robert Sievers, Ph.D. and his colleagues at Aktiv-Dry, LLC for their support of this study and Becton Dickinson for providing the PARI Breath Simulator used in these experiments. The authors also wish to thank Drs. H. M. Janssens and H. Tiddens of Erasmus Medical Center Rotterdam/Sophia Children’s Hospital (Rotterdam, The Netherlands), Dr. Johannes Wildhaber of the Department of Pediatrics, Kantonsspital (Fribourg, France) and Professor Lars Borgstroem of AstraZeneca Research and Development (Lund, Sweden) for providing the copies of the SAINT model used in these experiments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laube, B.L., Sharpless, G., Shermer, C. et al. Deposition of Albuterol Aerosol Generated by Pneumatic Nebulizer in the Sophia Anatomical Infant Nose-Throat (SAINT) Model. Pharm Res 27, 1722–1729 (2010). https://doi.org/10.1007/s11095-010-0171-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0171-1