Abstract
Purpose
The development of particle-based carriers for transepidermal drug delivery has become a field of major interest in dermatology. In this study, we investigated the suitability of biodegradable poly-lactic acid (PLA) particles loaded with fluorescent dyes as carriers for transepidermal drug delivery.
Methods
The penetration profiles of PLA particles (228 and 365 nm) and the release of dye from the particles were investigated in human skin explants using fluorescence microscopy, confocal laser scanning microscopy and flow cytometry.
Results
PLA particles penetrated into 50% of the vellus hair follicles, reaching a maximal depth corresponding to the entry of the sebaceous gland in 12–15% of all observed follicles. The accumulation of particles in the follicular ducts was accompanied by the release of dye to the viable epidermis and its retention in the sebaceous glands for up to 24 h. Kinetic studies in vitro as well as in skin explants revealed, that, although stable in aqueous solution, destabilization of the particles and significant release of incorporated dye occurred upon contact with organic solvents and the skin surface.
Conclusions
These results suggest that particles based on PLA polymers may be ideal carriers for hair follicle and sebaceous gland targeting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Drug delivery systems have gained great attention in the last years because of their bio-distribution and loading-release features that allow to deliver drugs selectively and over a prolonged time course to the specific site of action. In the fields of dermatology and cosmetics, micro- and nanoparticles (NPs) have been studied since decades and some formulations are already commercially available. Several kinds of particles are actually investigated as drug delivery systems for topical applications, including modified liposomes, solid lipid nanoparticles (SLN) and biodegradable polyesters NPs like poly-lactic acid (PLA), poly-lactic-co-glycolic acid (PLGA) and poly-ε-caprolactone (PCL). One of the features that make NPs interesting for dermatological applications is their tendency to penetrate and accumulate preferentially in the hair follicle orifices (1–5). For this reason, NPs have been proposed for the site-specific drug delivery to pilosebaceous structures (6–8). Drugs applied on skin in classical galenic preparations may enter the skin through both the stratum corneum and the hair follicles indistinctively. On the contrary, the loading of drugs on particles allows reducing the trans-epidermal pathway and increases the drug concentration in the hair follicles (9). This preferential accumulation allows an improvement of the therapeutic index for drugs in dermatotherapy and specifically in the therapy of hair-follicle-associated diseases. In fact, in vitro and in vivo studies demonstrated that topically applied substances permeate faster and reach higher concentrations in skin with follicles compared to skin without follicles or with selectively blocked follicles (10,11). The interfollicular epidermis and the epithelium of the acroinfundibulum form a relatively tight barrier, but the horny layer in the lower follicular tract is incomplete since the corneocytes in this region are smaller and not completely differentiated (12). Therefore, NPs carrying drugs in the follicular duct can ensure a better and faster drug penetration into the viable epidermis. Microspheres and NPs penetrate down to different depths depending on their size (13,14). The use of the adequate particle size would therefore allow the selective targeting of specific structures and cell populations within the follicles (5). Moreover, hair follicles represent a reservoir where particles can accumulate and create high local concentrations of drugs (15). The particle depot in the follicular duct also ensures a prolonged drug release, which enables the reduction of the applied dose and the frequency of applications (16). The majority of the studies in this field focus on particles as carriers, which release their load after penetration into the hair follicle openings. This approach minimizes the risk of particle translocation into the viable tissue and potential hazardous effects. In fact, there is little evidence that particles at a size exceeding 100 nm translocate to the viable epidermis of intact skin (17). The translocation capacity of smaller particles across intact skin is still a matter of discussion (18,19). However, safety concerns have been raised based on reports of nanoparticle translocation across the hair follicle epithelium especially in barrier-disrupted or otherwise pre-damaged skin (14,20–22). In the light of these results, careful considerations of the toxicological profile of particles and their constituents as well as their biodegradability are instrumental in the design of innovative therapeutic systems.
In this study, we investigated the suitability of poly-lactic acid (PLA) NPs as carriers for transepidermal drug delivery. PLA is a linear, lipophilic, biodegradable polymer. Lactic acid, the constituting monomer, is easily derived from renewable resources like corn starch or sugarcane. The fact that lactic acid is the only degradation product following the polymer hydrolysis makes PLA polymer of interest for several applications. In medicine, it is used to produce bioabsorbable implants for orthopaedic surgery (23), for the treatment of facial lipoatrophy in HIV patients (24) as well as for treatment of scars and for esthetic rejuvenation (25). PLA micro- and nano-particles have widely been studied as delivery systems for systemic and topical applications (26). However, to our knowledge there are no articles reporting on PLA NPs as delivery systems for topical application on human skin. Two PLA NPs were used: 228 nm particles loaded with nile red (shortened NR_PLA_228) and 365 nm particles loaded with coumarin-6 (shortened Coum-6_PLA_365). Nile red was chosen because of its emission in the red region of the light spectrum, where skin has a low auto-fluorescence. Coumarin-6 was chosen because of its high fluorescence quantum yield. This allowed us to obtain Coum-6-PLA particles with fluorescence intensity similar to that of NR-PLA particles but with a lower dye load. The comparison of the two particle types should also provide insights on the effect of different dye loads on particle stability.
The penetration profile of transcutaneously applied PLA NPs into human vellus hair follicles, the release of loaded dye and the dye permeation to the viable epidermis and pilosebaceous structures were investigated.
MATERIAL AND METHODS
Nanoparticles Synthesis
PLA NPs were synthesized as described in Lamalle-Bernard et al. (27). Briefly, the polymer was dissolved in acetone at a concentration of 2% w/w, and this solution was added to an aqueous solution under moderate stirring. The solvents were then evaporated under reduced pressure at room temperature. No residual solvent was detected by proton NMR spectra from dissolved particle samples. The final PLA concentration was between 60 to 70 mg/ml depending on the batch and was precisely measured by weighing the wet and dried materials. Fluorescent particles were obtained as above, the fluorescent dyes being dissolved in acetone with PLA. Care was taken to protect solution from light throughout the experimental procedure. Poly (D,L-lactic acid) 30,000g/mol−1was purchased from Phusis (Grenoble, France). Green fluorescent polystyrene particles (FluoSpheres ®, 200 nm) were purchased from Molecular Probes (Oregon, USA).
Tissue Samples
Human skin (retroauricular region, breast, and abdomen) was obtained, within 24 h after surgical excision, from healthy volunteers undergoing plastic surgery. Volunteers had signed an informative consent approved by the Institutional Ethics Committee of the Medical Faculty of the Charité-Universitätsmedizin Berlin and in accordance with the ethical rules stated in the Declaration of Helsinki Principles.
Particle Application on Skin Explants
Skin samples were examined macroscopically and microscopically for tissue damage. Subcutaneous fat was removed and skin was cut into 1 or 16 cm² samples, leaving safety margins of 0.5 cm to the border of the tissue in order to avoid sideways non-specific penetration of tested particles into the tissue. Prior to the application of particles, cyanoacrylate skin surface stripping (CSSS) was performed once as described previously (13) using superglue (UHU GmbH, Buehl/Baden, Germany). Two different types of PLA NPs, 365 nm nanoparticles loaded with Coum-6 (Coum-6_PLA_365) and 228 nm NPs loaded with NR (NR_PLA_228) were applied. The particles suspensions were sonificated for 3 min (Sonorex Super RK102H, Bandelin, Berlin, Germany) and a volume of 20 µl/cm2 of a 0.5% (w/v) suspension in PBS (pH = 7.4) was applied on the sample skin area. Tissue samples were then incubated at 37°C in a humidified chamber for 2, 4, 8, 16 and 24 h. Skin from three different donors was used for both follicular penetration studies and dye-release kinetics.
Cryosections and Fluorescence Microscopy
The penetration profile of studied PLA NPs in vellus hair follicles and the time dependent release of NR from PLA NPs applied on skin samples were investigated by fluorescence microscopy on cryosections. After skin incubation, adhesive tape stripping was performed five times to remove the NPs that had not penetrated in the hair follicles and to reduce the amount of free NPs on the tissue section. A skin area of 1 cm2 was excised and split into four blocks which were frozen in liquid nitrogen. Cryosections of 5 µm thickness were prepared from each block using a microtome (2800 Frigocut-N, Reichert-Jung, Heidelberg, Germany). As in previous studies by our group (13), cutting was performed with fresh blades from the dermis side towards the epidermis in order to avoid dislocation of NPs from the skin surface on the section. Cryosections (150–300 sections per donor, three different donors) were screened by fluorescence microscopy (BX60F3, Olympus, Hamburg, Germany). Coum-6 fluorescence was detected using 470–490 nm BP and 550 nm LP filters, while NR was detected using 545–580 nm BP and 610 nm LP filters. Longitudinal sections of vellus hair follicles were selected for confocal laser scan microscopy analyses (FluoViewTM FV1000, Olympus, Germany). Probes were excited with an Helium–Neon Laser (543 nm) and fluorescence was detected in the region of 600–700 nm. Digital image overlay was used to localize the fluorescent signal on the tissue sections.
Estimation of Particles Penetration Depth
A semi-quantitative analysis of the follicles allowed the evaluation of the average depth reached by the NPs (Fig. 1a). In all, 150–300 sections from skin samples treated with PLA NPs were analyzed, and at least 50–60 hair follicles were identified. Only the best section of each hair follicle was chosen, subsequent sections of the same hair follicle were excluded from the study. The vellus hair follicles were analyzed for the presence of fluorescent NPs and, accordingly to the maximal depth reached by the fluorescent NPs, were classified in four types: negative, middle of epidermis, complete epidermis and deep penetration. The percentages of follicle types was calculated and plotted in Fig. 1b.
Penetration profile of PLA NPs into hair follicles. The penetration depth of the studied PLA NPs (Coum-6_PLA_365 and NR_PLA_228) in vellus hair follicles after 4 h incubation was evaluated on cryosections of human skin explants. VHF were classified into four types in accordance to the NPs penetration depth as represented in a. The penetration depth is reported as percentage of VHF type and was determined on a total number of at least 60 follicles per sample using skin from three different donors b. We found that PLA NPs penetrated into 50% of all observed VHFs and in 12–15% of VHFs reached the entry level of the sebaceous duct
Isolation of Epidermis Cells
Epidermal cell suspensions were generated as described elsewhere (28), with slight modifications. Briefly, dispase digestion (2.4 U/ml Dispase I, Roche, Germany) was performed on chopped skin samples for 2.5 h at 37°C. The epidermis was then detached from the dermis and treated with 0.025% trypsin and 1.5 mM CaCl2 in PBS (pH 7.4) for 15 min at 37°C. The digested epidermis was filtered (Cell Strainer, BD FalconTM, Germany) and cells were collected by centrifugation.
Flow Cytometry
Epidermis cells isolated from skin explants treated with the studied PLA NPs (0.5%, 16 h) and epidermis cells incubated in vitro with the same PLA NPs articles (50 µg/ml) were analyzed by flow cytometry using a FACS Calibur and the CellQuests software (Becton Dickinson, Heidelberg, Germany). A total number of 20,000 events were recorded. The software FCS-Express 3.1 (De Novo Software, USA) was used to analyse the collected data.
Cell Extracts
After overnight incubation of skin with the studied PLA NPs, adhesive tape stripping was performed five times and epidermis cells were isolated as described above. From 16 cm2 skin, approximately 5×107 cell/ml were isolated. Dichloromethane (1 ml) was added and the cell pellet was vortexed (MSI Minishaker, IKA® Labortechnik, Germany) for 1–2 min. After 30 min the cell extracts were centrifuged and their fluorescence intensity was measured with a fluorescence spectrophotometer (LS 50B, Perkin Elmer, Germany). The concentration of NR and Coum-6 in the cell extracts was determined by use of calibration curves of the respective dye in dichloromethane. The reported values are the averages of three experiments with skin from three different donors.
In Vitro Release Studies
The in vitro release of NR and Coum-6 from PLA NPs was carried out in triplicate in a two-phase (hydrophilic/lipophilic) system using phosphate buffer (PBS) as hydrophilic phase and isopropyl mirystate (IPM) or hexane as lipophilic phase. PLA particle suspensions (1 ml, 610 µg/ml) in PBS were prepared and added with the same volume of lipophilic solvent. Hexane was chosen because of its high lipophilicity, while IPM was chosen because of its similarity with sebum and to simulate the lipophilic nature of the stratum corneum (29). The NPs suspension in PBS was constantly stirred and small aliquots (10 µl) of the lipophilic solvent were removed and replaced with the same volume of fresh solvent at time 0, 1, 2, 3, 4, 5, 16 and 24 h. The aliquot was diluted with the adequate solvent and the fluorescence intensity was measured spectrophotometrically (LS 50B, Perkin Elmer, Germany). The concentration of dye in the receptor lipophilic solvent was determined by comparing the fluorescence intensity of the unknown samples to that of standard samples (calibration curves).
RESULTS
Follicular Penetration of 228 and 365 nm PLA Particles in Human Skin Explants
In order to determine the extent of follicular penetration of topically applied PLA NPs with a diameter of 228 and 365 nm, fluorescence microscopy on cryosections of human excised skin was performed. 150–300 sections per skin samples were analyzed. A minimum of 50–60 hair follicle sections were identified, and the average penetration depth along the follicular duct was analyzed semi-quantitatively (Fig. 1a). The analyzed vellus hair follicles (VHF) were classified into four types: negative, middle epidermis, complete epidermis and deep penetration (as described in materials and methods). According to our own measurements on retroauricular vellus hair follicles, the thickness of the interfollicular epidermis ranges between a minimum of 64 ± 12 µm and a maximum of 99 ± 18 µm in VHF-bearing skin and the length of the infundibulum in VHF was measured to be 225 ± 34 µm (30). The amounts of classified follicles were expressed as percentages of all analyzed VHFs. The graphic in Fig. 1b reports the penetration profile of PLA NPs as averages of data obtained from three different donors. Similar results were found for the two studied PLA NPs. Both PLA NPs, loaded with nile red (228 nm) or with coumarin-6 (365 nm), penetrated in approximately 50% of all investigated VHF. 12–24% of these positive follicles presented a pattern of NPs superficial agglomeration with particles deepened to the middle of the epidermis. In 14–20% of follicles, particles were visible in all the epidermis length while in 10–22% of follicles particles penetrated down to the entry level of the sebaceous gland. For both particle sizes no penetration in the interfollicular skin or in the perifollicular epithelium was observed. These results show that 228 and 365 nm PLA particles applied on excised human skin accumulate in 50% of follicles with a maximum penetration depth corresponding to the deepest region of the infundibulum.
Release of NR from PLA NPs Applied on Skin Explants
Beside the granular pattern typical of mono-dispersed NPs and aggregates, a diffuse fluorescence was visible in epidermis and sebaceous glands after transcutaneous application of dye-loaded PLA NPs. Preparing cryosections of skin treated with NR_PLA_228 after different incubation times allowed us to follow the dye release kinetic on skin explants. Fig. 2 is a summary of the pictures taken at different incubation times. After 2 h of incubation (Fig. 2), nanoparticle clusters were visible on the skin surface, in the hair follicle openings and in the upper part of the infundibulum. We detected a diffuse red fluorescence in the stratum corneum while the rest of the epidermis was only slightly stained. No fluorescence was detectable in the sebaceous gland after 2 h of incubation. After 4 h incubation, the fluorescence signal in the epidermis and in the follicular duct increased and was detectable also in the sebaceous glands. In fact, the fluorescence reached a maximum in the epidermis 8 h after incubation and after 16 h in the sebaceous gland and it persisted for up to 24 h. Within the hair follicle ducts, we identified both, particle clusters as well as a diffuse intense fluorescence. To further analyze this process, we performed confocal scan microscopy on cryosections of excised skin treated with NR_PLA_228 particles (Fig. 3). The possibility to excite the sample at a defined wavelength where NR has its maximal absorption (543 nm) and to detect the emitted light in the spectrum range of 600–700 nm allowed us to distinguish between the fluorescence of NR and the skin auto-fluorescence. A diffuse dye fluorescence was found in the stratum corneum, in the interfollicular epidermis, in the follicular epithelium as well as in the hair follicle duct (Fig. 3a-c). Particle clusters were visible in the follicular duct, predominantly in the infundibulum. The closer observation of the epidermis (Fig. 3 a’-c’) revealed the presence of NR in the cell cytoplasm but not in the cell nuclei, that imposed themselves as dark, circular areas approximately in the middle of the cells. After an initial burst, with a maximum release of NR, the fluorescence intensity decreased but persisted for up to 24 h. The released lipophilic dye permeated into the viable epidermis and diffused to the sebaceous gland, where it accumulated in the sebum filled areas.
NR release after transcutaneous application of PLA NPs on human excised skin. NR_PLA_228 were applied on fresh skin explants and incubated for 2, 4, 8, 16 and 24 h. Superficial, non-penetrated NPs were then removed by tape stripping and cryosections were prepared. Images are a selection of pictures showing the time-dependent permeation of released NR in the viable epidermis and its accumulation in sebum and in the sebaceous glands for up to 24 h
Confocal scanning microscope analysis of cryosections. Laser scan microscopy was performed on cryosections of human skin after transcutaneous application of NR loaded PLA NPs. Transmitted light a, red fluorescence b and digital overlayed c images of a representative sample are reported. Images a’, b’ and c’ were obtained by zooming in the marked region ( 3× magnification). We found that, upon being released from PLA NPs, NR localized in stratum corneum and in the cytoplasm of epidermis cells which is a hint to a dye trans-cellular diffusion pathway
In order to unequivocally prove that the fluorescence detected in the epidermis is generated exclusively by the released dye and not from translocated particles, we applied polystyrene particles which do not let dye leaching (Fluospheres, 200 nm) on excised human skin (Supplemental Material Fig. 1). We observed that PS particles accumulated deep in the follicle duct without leaking of the loaded fluorescent dye while most of PLA particles aggregated in the follicle ducts and the loaded dye diffused to the epidermis. These results confirmed our hypothesis that PLA NPs, when topically applied on skin explants, are able to release the carried drugs within hours.
The Lipophilic Dye Released by PLA NPs Permeate into the Epidermis Cells
The confocal scan microscope pictures showed a clear pattern of intracellular fluorescence in the interfollicular and follicular epidermis. To verify the internalization of the released dye by the cells and definitively exclude the uptake of whole particles, we isolated the epidermis cells from skin incubated overnight with NR_PLA_228 and Coum-6_PLA_365. The isolated cells were analyzed by flow cytometry, fluorescence microscopy and fluorescence spectrophotometry (Fig. 4). Epidermal cells incubated in vitro with PLA particles served as controls for particles internalization, while untreated isolated cells were used as negative control. The flow cytometry histograms of epidermis cells with in vitro internalized NPs were clearly shifted with respect to those of untreated cells. The same cells observed with the fluorescence microscope exhibited a spotted fluorescence pattern typical of internalized NPs (Fig. 4a,b). On the contrary, the flow cytometry analysis of epidermal cells isolated from PLA treated skin explants showed only a small shift with respect to cells isolated from untreated skin (Fig. 4c,d). Epidermis cells isolated from skin incubated with Coum-6_PLA_365 exhibited mean fluorescence intensity (MFI) values of 9.53 (± 2.37) while in vitro samples had MFI values of 48.14 (± 13.37). Similarly, cells isolated from skin treated with NR_PLA_228 particles had MFI values of 6.49 (± 0.67) while in vitro samples had an average MFI values of 32.60 (± 10.91). The fluorescence pictures put in evidence that cells isolated from PLA-treated skin had a diffuse, low-intensity fluorescence, which could not be associated to NPs. The spectrophotometry analysis, further confirmed the presence of Coum-6 and NR in the cell extracts. In fact, the typical fluorescence emission spectra of Coum-6 and NR (Fig. 4e,f) could be recorded. The dye concentrations in cell extracts have also been calculated by means of standard curves. The measurements proved to be reproducible and similar concentrations were found for Coum-6 and NR (1.96 ng/ml and 2.29 ng/ml, respectively). These data confirm that in our studies, PLA NPs did not translocate to the viable epidermis as already observed with the confocal microscope. Moreover, they confirm that both NR and Coum-6 permeate via an intracellular diffusion pathway and are detectable within the cells of the viable epidermis till 16 h after NPs application onto excised skin.
Analysis of epidermal cells isolated from skin explants incubated with PLA NPs. Epidermal cells isolated from skin treated with Coum-6_PLA_365 or NR_PLA_228, respectively, were compared to isolated epidermal cells incubated in vitro with the same NPs. The intracellular uptake of PLA NPs or released dye was estimated on single cells using flow cytometry and fluorescence microscopy (a-d, original magnification ×100). The uptake of released dye was also confirmed by spectrophotometrical measurements on epidermis cell extracts (e,f). The reported mean fluorescence intensity (MFI) and cell extract concentrations are the average of three independent experiments
In Vitro Release Kinetic of Nile Red and Coumarin-6 from PLA Nanoparticles
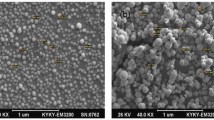
The studied PLA NPs were stable in aqueous suspensions and no release of the lipophilic dyes was observed for the particles kept in water or PBS. In order to understand the reasons for the dye release upon contact with skin, we decided to perform an in vitro release study in two-phase systems (PBS/hexane and PBS/IPM) mimicking the lipophilic environment of the skin. Hexane was chosen because it is a lipophilic solvent, not miscible with water and without polar groups which could interact with those of the PLA polymer. IPM was chosen because its chemical structure resembles that of sebum components (e.g. wax esters and triglycerides) and the lipophilic nature of the stratum corneum. In both organic solvents, a time dependent increase of the fluorescence intensity could be measured for both PLA NPs (Fig. 5). The emission spectra corresponded to those of NR and Coum-6. On the contrary, in the aqueous phase (after centrifugation and precipitation of the NPs) no significant increase of fluorescence intensity was detected even after 24 h. All kinetic curves showed an initial increase of released dye, followed by a plateau approximately after 16 h. The dye concentrations measured in hexane (Fig. 5a) were higher than those measured in IPM (Fig. 5b), e.g. after 24 h incubation 121.4 ng/ml (9.95%) and 84.05 ng/ml (6.89%) of NR were calculated in hexane and IPM respectively. Similarly, the amounts of released Coum-6 reached values of 46.34 ng/ml (37.98%) and 11.49 ng/ml (9.42%) in hexane and IPM, respectively. It has to be noticed that the dye loading percentages of the two PLA NPs were different: 0.2% for NR_PLA_228 and 0.02% for Coum-6_PLA_365. Therefore, it is not surprising that the amounts of dye released by NR-PLA_228 particles were higher than those released by Coum-6_PLA_365 particles while the cumulative percentages values of Coum-6 are higher than those of NR. During the kinetics experiments, we observed a coloured layer in the interface between water and IPM (or hexane). Therefore, the NPs suspension in PBS and the IPM solution were microscopically analyzed at the end of each kinetics (Fig. 5c-h). In the aqueous suspension (Fig. 5c,g) a spotted fluorescence pattern revealed the presence of single NPs and sporadically of small aggregates. On the contrary, in the interface PBS/IPM, as well as in the side areas, fluorescent clusters of micrometer size were observed (Fig. 5d-f,h). The fluorescence patterns of aggregated particles observed in the interface PBS/IPM were similar to those found on the skin surface and in the follicular ducts (Fig. 2, arrows) and differed from those formed by PLA NPs in aqueous suspensions. Polystyrene particles did not form clusters upon contact with IPM, even after 24 h incubation (Supplemental Materials, Fig. 2). These findings confirm that PLA NPs can rapidly release the loaded lipophilic dyes when coming in contact with a lipophilic environment and that the release process is due to the diffusion of dye out of the particles as a consequence of particles destabilisation.
In vitro release of nile red (NR) and coumarin-6 (Coum-6) from NR_PLA_228 and Coum-6_PLA-423 particles. The release of lipophilic dyes from PLA NPs was performed in hexan/PBS a and IPM/PBS b biphasic systems. The cumulative percentages of dye released from PLA NPs in the lipophilic phase are reported as a function of time. At the end of each kinetics experiment, aliquots were collected from the aqueous particle suspension as well as at the water/IPM interface and analyzed with a fluorescence microscope. We found that particles in the buffered aqueous suspension were almost monodispersed (e,g) while particle clusters were visible in the aliquots collected at the water/IPM interface (c,d) and in IPM (f,h)
DISCUSSION
In this study, we intended to test the suitability of PLA-particles as drug delivery systems for dermatotherapeutic applications, especially for hair follicle targeting. The fluorescent dyes were incorporated in the PLA particles in order to facilitate microscopic particle detection. They further served as lipophilic model compounds to study the release of incorporated substances, their diffusion out of the particles as well as retention in the different skin compartments. The finding that the PLA-particles accumulated preferentially in hair follicles is perfectly in line with previous studies on particle penetration in hair follicles (31). The PLA-particles were detected in approximately 50% of the analyzed VHF, which is in accordance with previous studies in our group using other particle types. These studies revealed that depending on the skin sample approximately 50–70% of the hair follicles are open for penetration (unpublished data). In fact, Lademann et al. introduced the concept of open and closed hair follicles suggesting that availability for penetration is dependent on the functional status of the hair follicle as well as on the presence of cellular debris and sebum, both of which may clog the infundibulum (31). The experimental findings on the excised human skin are still highly relevant. According to recent studies, penetration rates in vivo can be expected to be up to ten-fold higher (32), e.g. after skin excision, the hair follicles volume is reduced by the contraction of the surrounding elastic fibres so that the hair follicle is less receptive for the penetration of applied substances (33). In a significant percentage of VHF (12–15%) the PLA particles penetrated into the infundibulum and were also observed at the entrance level of the sebaceous duct. According to our own data obtained from human VHF of the retroauricular region, this corresponds to a maximal depth of 225 µm (30). Translocation of intact particles into or across the hair follicle epithelium was not detected, which is in accordance with the current opinion, that translocation of particles > 100 nm into the viable tissue is rather unlikely to occur. The particle accumulation in hair follicles was accompanied by a striking diffuse fluorescence signal visible in the epidermis as well as in the hair follicle duct. Confocal scan microscopy as well as flow cytometry and microscopy of single cell suspensions derived from particle-treated epidermis clearly confirmed diffusion of free dye into epidermal cells. Concomitantly, we detected clusters of particles in the hair follicle openings rather than scattered single particles, suggesting that aggregation occurred. The fact that in skin cryosections or in cells isolated from the epidermis no intracellular spotted fluorescence was observed allowed us to exclude translocation of intact PLA particles into the viable epidermis.
The released lipophilic dye diffused into the sebum, permeated to epidermal cells, and accumulated in sebaceous glands for up to 24 h. A rapid release of lipophilic compounds in the lipophilic environment of the skin has already been reported for other particle types, e.g. the release of NR from poly(caprolactone) NPs applied on porcine ear skin was studied by Alvarez-Roman and co-workers (29). Mordon et al. reported the release of the lipophilic dye methylen blue from highly porous nylon microspheres using ethanol to favour dye release (8). However, in these reports, neither denaturation of the NPs nor formation of clusters or aggregates was observed. The PLA particles used in our study were stable in aqueous solutions over several weeks after their preparation. No dye leaking was observed. Aggregation and a rapid dye release appeared to occur only upon skin contact. Based on these observations, we hypothesized, that PLA particles destabilize on the skin surface and in the follicular duct, form clusters, and release the incorporated lipophilic dye. To test this hypothesis, we decided to investigate the release of dye in an in vitro biphasic system consisting in an organic lipophilic solvent and a buffer solution. This allowed us to mimic the release process, probably occurring at the interface between the NPs aqueous suspension and the sebum on the skin surface and in the hair follicle ducts. The in vitro release kinetics of NR and Coum-6 from PLA particles showed a rapid and time-dependent dye release in the lipophilic phase followed by a plateau after approximately 16 h. Alvarez-Roman et al. reported similar results for NR encapsulated in poly((-caprolactone) NPs in an in vitro kinetic using an aqueous suspension of NPs and IPM as receptor medium (29). Similarly, in vitro release from PLGA particles of a lipophilic drug (adapalene) was also studied in artificial sebum (6), where a rapid release was found with a plateau after 4 h. Nevertheless, decomposition of pegylated PLA NPs and drug disassociation after intravenous injection has also been reported. The denaturation was found to occur predominantly as result of particle interactions with blood α- and β-globulins (34). A rapid release of lipophilic drugs from polyester NPs after contact with a lipophilic solvent may be due to the partition of the dye between the lipophilic cores of the particles and the lipophilic solvent as well as to the dissolution of the polymer in the lipophilic phase. On the contrary, the release of lipophilic drugs from particles in water suspensions is a slow process which occurs only upon polymer hydrolysis and particle erosion (35,36). In our study, the dye release from PLA NPs in contact with the lipophilic solvents was concomitant with particles destabilisation and formation of clusters similar to those observed in skin explants. Both NR_PLA_228 and Coum-6_PLA_365 particles destabilized in lipophilic environment, suggesting that the different dye loads had low influence on PLA particle stability on skin. The particle clusters at the interface between water and IPM probably result from the aggregation of the particle due to the low dielectric constant of IPM that drastically reduces the repulsive electrostatic forces responsible for the stabilisation of the colloid in the water phase. Moreover, the organic phase can penetrate within the lipophilic PLA matrix allowing the diffusion of the originally stranded dye in the close environment of the clusters. Because aggregate formation and a rapid dye release were observed in both our in vitro and ex-vivo kinetics, it is reasonable to think that they are the direct consequence of particle contact with a lipophilic environment and possibly the result of NPs denaturation. The lipophilic milieu of the skin would be responsible for the loss of the colloidal stability of topically applied PLA NPs and the rapid release of the carried lipophilic dye would result from the possible diffusion of the dye in the external lipophilic medium of the skin. The high local concentration reached by NPs accumulated in skin furrows and follicular ducts would then favor the aggregation of denaturated particles. In our studies with different particle types, we observed that not all particles underwent aggregation upon contact with lipophilic environments; e.g. neutravidin-coated PS NPs did not form clusters when mixed with IPM, but kept the same fluorescence spotted pattern typical of mono-disperse particles (Supplemental Material, Fig. 2). It is not clear yet if the stability of neutravidin-coated PS NPs is due to the nature of the polymer or to their coating and further investigations are ongoing in our group. Taken all together, these results show the need for a better understanding of nanoparticle interactions with different biological environments and of the factors influencing the release of NPs loads in in vivo systems.
CONCLUSIONS
Based on our findings, we hypothesize that PLA particles, after topical application on the skin surface, destabilize upon contact with sebum on the stratum corneum and in the hair follicle ducts. This destabilization leads to irreversible formation of clusters and aggregates, which we observed not only on the cryosections from human skin explants but also at the interface of our biphasic in vitro system. These results suggest that PLA particles, in contrast to stable solid particles such as polystyrene nanospheres, do not only accumulate, but also destabilize and release the loaded dye while forming aggregates within the hair follicle duct. The aggregation process could further prolong storage time within the duct and eventually cause the further release of incorporated compounds into the follicle, the sebaceous gland and the perifollicular tissue. Especially lipophilic compounds such as the fluorescent dyes used in our studies, preferentially diffuse via sebum and accumulate in the sebaceous glands for up to 24 h. Hence, PLA particles may represent ideal candidates for the design of drug delivery systems, which aim to target active compounds into hair follicles. In fact, our studies revealed that PLA particles meet all the criteria required to optimize current hair follicle targeting approaches: (i) preferential penetration via hair follicles, (ii) aggregation and cluster formation, which may cause prolonged retention in the hair follicle ducts, (iii) release of incorporated compounds which diffuse into the perifollicular region creating maximal concentration in and around the hair follicle (5).
The PLA particles are biodegradable, which minimizes hazardous effects. Particle production is easy and feasible also in larger batches. Both characteristics facilitate translation of our findings into clinical studies, and follow-up studies are currently performed by our group, which aim to improve the penetration profile and to modify the kinetics of drug release. A number of different drugs have already been successfully encapsulated in PLA NPs (37), including DNA, proteins and peptides. Possible applications range from dermatotherapy and treatment of hair follicle-associated disorders, such as acne vulgaris, to targeting of stem cells, i.e. gene therapy (38,39), or antigen-presenting cells, i.e. transcutaneous immunization approaches (14,40). Moreover, the particles and clusters accumulated in the follicular duct represent drug depots ensuring a prolonged drug release and could be utilized in dermal drug delivery systems and patch applications for systemic drug release (41,42).
Abbreviations
- Coum-6:
-
coumarin-6
- Coum-6_PLA_365:
-
coumarin-6-loaded 365 nm PLA particles
- CSSS:
-
cyanoacrylate skin surface stripping
- IPM:
-
isopropylmiristate
- MFI:
-
mean fluorescence intensity
- NPs:
-
nanoparticles
- NR:
-
nile red
- NR_PLA_228:
-
nile red-loaded 228 nm PLA particles
- PCL:
-
poly- ε-caprolactone
- PLA:
-
poly lactic-acid
- PLGA:
-
poly-lactic-co-glycolic acid
- SLN:
-
solid lipid nanoparticles
- VHF:
-
vellus hair follicle
References
Li L, Lishko V, Hoffman RM. Liposome targeting of high molecular weight DNA to the hair follicles of histocultured skin: a model for gene therapy of the hair growth processes. In Vitro Cell Dev Biol Anim. 1993;29:258–260.
Bernard E, Dubois JL, Wepierre J. Importance of sebaceous glands in cutaneous penetration of an antiandrogen: target effect of liposomes. J Pharm Sci. 1997;86:573–578.
Li L, Hoffman RM. Topical liposome delivery of molecules to hair follicles in mice. J Dermatol Sci. 1997;14:101–108.
Alvarez-Román R, Naik A, Kalia YN, Guy RH, Fessi H. Skin penetration and distribution of polymeric nanoparticles. J Controll Release. 2004;99:53–62.
Vogt A, Mandt N, Lademann J, Schaefer H, Blume-Peytavi U. Follicular targeting-A promising tool in selective dermatotherapy. J Invest Dermatol Symp Proc. 2005;10:252–255.
Rolland A, Wagner N, Chatelus A, Shroot B, Schaefer H. Site-specific drug delivery to pilosebaceous structures using polymeric microspheres. Pharm Res. 1993;10:1738–44.
Lauer AC, Ramachandran C, Lieb LM, Niemiec S, Weiner ND. Targeted delivery to the pilosebaceous unit via liposomes. Adv Drug Deliv Rev. 1996;18:311–324.
Mordon S, Sumian Ch, Devoisselle JM. Site-specific methylene blue delivery to pilosebaceous structures using highly porous nylon microspheres an experimental evaluation. Lasers Surg Med. 2004;33:119–125.
Lademann J, Knorr F, Richter H, Blume-Peytavi U, Vogt A, Antoniou C, et al. Hair follicles: an efficient storage and penetration pathway for topically applied substances. Skin Pharmacol Physiol. 2008;21:150–155.
Michel M, L’Heureux L, Pouliot R, Xu W, Auger FA, Germain L. Characterization of a new tissue-engineered human skin equivalent with hair. In Vitro Cell Dev Biol Anim. 1999;35:318–326.
Teichmann A, Otberg N, Jacobi U, Sterry W, Lademann J. Follicular penetration: development of a method to block the follicles selectively against the penetration of topically applied substances. Skin Pharmacol Physiol. 2006;19:216–223.
Vogt A, Blume-Peytavi U. Die Biologie des menschlichen Haarfollikels. Hautarzt. 2003;54:692–698.
Toll R, Jacobi U, Richter H, Lademann J, Schaefer H, Blume-Peytavi U. Penetration profile of microspheres in follicular targeting of terminal hair follicles. J Invest Dermatol. 2004;123:168–176.
Vogt A, Combadiere B, Hadam S, Stieler KM, Lademann J, Schaefer H, et al. 40 nm, but not 750 or 1, 500 nm, Nanoparticles enter epidermal CD1a+ cells after transcutaneous application on human skin. J Invest Dermatol. 2006;126:1316–1322.
Lademann J, Richter H, Schaefer H, Blume-Peytavi U, Teichmann A, Otberg N, et al. Hair follicles—a long-term reservoir for drug delivery. Skin Pharmacol Physiol. 2006;19:232–236.
Schäfer-Korting M, Mehnert W, Korting HC. Lipid nanoparticles for improved topical application of drugs for skin diseases. Adv Drug Deliv Rev. 2007;59:427–443.
Warheit DB, Borm PJ, Hennes C, Lademann J. Testing strategies to establish the safety of nanomaterials: conclusions of an ECETOC workshop. Inhal Toxicol. 2007;19:631–643.
Cross SE, Innes B, Roberts MS, Tsuzuki T, Robertson TA, McCormick P. Human skin penetration of sunscreen nanoparticles: in-vitro assessment of a novel micronized zinc oxide formulation. Skin Pharmacol Physiol. 2007;20:148–154.
Baroli B, Ennas MG, Loffredo F, Isola M, Pinna R, López-Quintela MA. Penetration of metallic nanoparticles in human full-thickness skin. J Invest Dermatol. 2007;127:1701–1712.
Zhang LW, Monteiro-Riviere NA. Assessment of quantum dot penetration into intact, tape-stripped, abraded and flexed rat skin. Skin Pharmacol Physiol. 2008;21:166–180.
Rouse JG, Yang J, Ryman-Rasmussen JP, Barron AR, Monteiro-Riviere NA. Effects of mechanical flexion on the penetration of fullerene amino acid-derivatized peptide nanoparticles through skin. Nano Lett. 2007;7:155–160.
Ryman-Rasmussen J, Riviere JE, Monteiro-Riviere NA. Surface coatings determine cytotoxicity and irritation potential of quantum dot nanoparticles in epidermal keratinocytes. J Invest Dermatol. 2007;127:143–153.
Maurus PB, Kaeding ChC. Bioabsorbable implant material review. Oper Tech in Sport Med. 2004;12:158–160.
Burgess CM, Quiroga RM. Assessment of the safety and efficacy of poly-L-lactic acid for the treatment of HIV-associated facial lipoatrophy. J Am Acad Dermatol. 2005;52:233–239.
Beer KR, Rendon MI. Use of Sculptra™ in esthetic rejuvenation. Semin Cutan Med Surg. 2006;25:127–131.
Mohamed F, Van der Walle CF. Engineering biodegradable polyester particles with specific drug targeting and drug release properties. J Pharm Sci. 2008;97:71–87.
Lamalle-Bernard D, Munier S, Compagnon C, Charles MH, Kalyanaraman KS, Delair T, et al. Co-adsorption of HIV-1 p24 and gp120 proteins to surfactant-free anionic PLA nanoparticles preserves antigenicity and immunogenicity. J Control Release. 2006;115:57–67.
Peiser M, Grutzkau A, Wanner R, Kolde G. CD1a and CD1c cell sorting yields a homogenous population of immature human Langerhans cells. J Immunol Methods. 2003;279:41–53.
Alvarez-Román R, Naik A, Kalia YN, Guy RH, Fessi H. Enhancement of topical delivery from biodegradable nanoparticles. Pharm Res. 2004;21:1818–1825.
Vogt A, Hadam S, Heiderhoff M, Audring H, Lademann J, Sterry W, et al. Morphometry of human terminal and vellus hair follicles. Exp Dermatol. 2007;16:946–950.
Lademann J, Otberg N, Richter H, Weigmann H-J, Lindemann U, Schaefer H, et al. Investigation of follicular penetration of topically applied substances. Skin Pharmacol Appl Skin Physiol. 2001;14:17–22.
Patzelt A, Richter H, Buettemeyer R, Roewert Huber HJ, Blume-Peytavi U, Sterry W, et al. Differential stripping demonstrate a significant reduction of the hair follicle reservoir in vitro compared to in vivo. Eur J Pharm Biopharm. 2008;70:234–238.
Starcher B, Aycock RL, Hill CH. Multiple roles for elastic fibers in the skin. J Histochem Cytochem. 2005;53:431–443.
Chen H, Kim S, He W, Wang H, Low PS, Park K, et al. Fast release of lipophilic agents from circulating PEG-PDLLA micelles revealed by in vivo Förster resonance energy transfer imaging. Langmuir. 2008;24:5213–5217.
Matsumoto A, Matsukawa Y, Suzuki T, Yoshino H. Drug release characteristic of multi-reservoir type microspheres, with poly(dl-lactide-co-glycolide) and poly(dl-lactide). J Control Rel. 2005;106:172–180.
Liu SQ, Yang YY, Liu XM, Tong YW. Preparation and characterization of temperature-sensitive poly(N-isopropylacrylamide)-b-poly(D, L-lactide) microspheres for protein delivery. Biomacromolecules. 2003;4:1784–1793.
Lassalle V, Ferreira ML. PLA nano- and microparticles for drug delivery: an overview of the methods of preparation. Macromol Biosci. 2007;7:767–783.
Sawicki JA, Anderson DG, Langer R. Nanoparticle delivery of suicide DNA for epithelial ovarian cancer therapy. Adv Exp Med Biol. 2008;622:209–219.
Sanvicens N, Marco MP. Multifunctional nanoparticles–properties and prospects for their use in human medicine. Trends in Biotechnol. 2008;26:425–33.
Vogt A, Mahé B, Costagliola D, Bonduelle O, Hadam S, Schaefer G, et al. Transcutaneous anti-influenza vaccination promotes both CD4 and CD8 T cell immune responses in humans. J Immunol. 2008;180:1482–1489.
Prausnitz MR. Microneedles for transdermal drug delivery. Adv Drug Del Rev. 2004;56:581–587.
Almeida AJ, Souto E. Solid lipid nanoparticles as a drug delivery system for peptides and proteins. Adv Drug Del Rev. 2007;59:478–490.
Acknowledgements
This work was partially supported by European funding to B. Verrier through the FP6 STREP Munanovac programme. C. Primard was supported by a fellowship from the Region Rhone-Alpes (France).
Author information
Authors and Affiliations
Corresponding author
Additional information
Fiorenza Rancan and Dimitrios Papakosta have contributed equally to this work
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig S1
Cryosections of human skin after topical application of NR_PLA_228 (a-c), Coum-6_PLA_365 (d-f) and 200 nm polystyrene (PS, g-i,) particles and 16 h incubation at 37°C. Images c,f and i show the 4 time magnified image of the marked region in the corresponding sample. Most PLA particles aggregate on the follicle openings while the fluorescent dye diffused into the epidermis. On the contrary, PS particles accumulated in the follicle duct without leaking of the loaded fluorescent dye. (PPT 4160 kb)
Fig S2
NR_PLA_228 (a), Coum-6_PLA_365 (b) and polystyrene particles (c,d, Fluospheres, 200 nm) suspended in PBS were incubated 24 h with IPM. Aliquots were then collected at the PBS/IPM interface and observed with a fluorescence microscope. PLA particles form clusters at the water/IPM interface (a,b) while no clusters of PS particles were visible at the interfaces between the two phases. PS particles, in contrast, remained in dispersion in the aqueous buffer phase (c,d). (PPT 755 kb)
Rights and permissions
About this article
Cite this article
Rancan, F., Papakostas, D., Hadam, S. et al. Investigation of Polylactic Acid (PLA) Nanoparticles as Drug Delivery Systems for Local Dermatotherapy. Pharm Res 26, 2027–2036 (2009). https://doi.org/10.1007/s11095-009-9919-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-009-9919-x